Abstract
Disturbances in serotonin neuroregulation and in hypothalamic-pituitary-adrenal axis activity are both likely, and possibly independent, factors in the genesis of suicidal behavior. This analysis considers whether clinically accessible measures of these two disturbances have additive value in the estimation of risk for suicide. Seventy-four inpatients with RDC major or schizoaffective depressive disorders entered a prospective follow-up study from 1978–1981, underwent a dexamethasone suppression test (DST) and had fasting serum cholesterol levels available in the medical record. As reported earlier, patients who had had an abnormal DST result were significantly more likely to commit suicide during follow-up. Serum cholesterol concentrations did not differ by DST result and low cholesterol values were associated with subsequent suicide when age and sex were included as covariates. These results indicate that, with the use of age-appropriate thresholds, serum cholesterol concentrations may be combined with DST results to provide a clinically useful estimate of suicide risk.
Keywords: Dexamethasone suppression test, cholesterol, cortisol, depressive disorder
1. Introduction
Suicide is a leading cause of death in the United States and is preceded by major depressive disorder (MDD) in the majority of cases (Barraclough et al., 1974). Accordingly, concerns over risks for suicide account for most psychiatric admissions of patients with MDD and thus the considerable expense and psychosocial disruptions that are associated with hospitalization. Such concerns are typically driven by suicidal tendencies as revealed in thoughts, plans, or behaviors but risk assessment is more complex and clinicians must weigh additional factors. These judgments have considerable importance. They underlie recommendations ranging from closer surveillance at home to involuntary psychiatric admission and they are important, as well, in determining inpatient activity levels and discharge timing. The relevant literature, though, yields little consistent evidence on which to base these estimations (Goldstein et al., 1991; Coryell and Young, in press).
Under the circumstances, a biological measure that is both clinically practical and sufficiently sensitive and specific to suicide risk would have substantial value. The failure to fully suppress plasma cortisol after a 1mg. dose of dexamethasone is one of the most widely investigated of potential measures. Convergent findings show hypothalamic-pituitary-adrenal (HPA) axis hyperactivity to be a risk factor for suicide in MDD (Dorovini-Zis and Zis, 1987; Nemeroff et al., 1988; Rao et al., 1989; Szigethy et al., 1994) and thus support the test’s validity as a measure of suicidality. A recent meta-analysis of seven studies concluded that dexamethasone suppression test (DST) nonsuppression increases the risk for suicide by a factor of 4.6 (Mann et al – personal communication).
Total serum cholesterol concentration is another clinically accessible measure of potential value in that numerous reports have associated suicidality with low serum cholesterol levels. Some investigators sampled suicide attempters from consecutive psychiatric admissions and compared them to nonattempters (Kunugi et al., 1997; Papassotiropoulos et al., 1999; Garland et al., 2000; Guillem et al., 2002), or to well controls (Gallerani et al., 1995; Sarchiapone et al., 2000; Tripodianakis et al., 2002). Others have described samples comprised specifically of patients with MDD (Modai et al., 1994; Alvarez et al., 1999; Kim and Myint, 2004), bipolar disorder (Modai et al., 1994; Bocchetta et al., 2001), panic disorder (Modai et al., 1994; Bocchetta et al., 2001; Obrocea et al., 2002; Ozer et al., 2004), borderline personality disorder (Atmaca et al., 2003) or anorexia nervosa (Favaro et al., 2004) and these also noted significantly lower cholesterol concentrations in comparison to those of nonattempters or of controls. Thus, the relationship between serum cholesterol and suicidality does not seem to be limited to individuals with major depressive disorder. Findings that this relationship is particularly strong for violent suicide attempts (Alvarez et al., 2000; Bocchetta et al., 2001; Atmaca et al., 2003; Kim and Myint, 2004) suggest that a low plasma cholesterol concentration is a risk factor for completed suicide as well. Studies using community samples have, in fact, shown this (Lindberg et al., 1992; Zureik et al., 1996; Ellison and Morrison, 2001). One large study from Finland did not and, instead, found a significant relationship between suicide and high cholesterol concentrations (Tanskanen et al., 2000). Some have suggested that this result reflected a particularly high rate of alcohol in Finland and the tendency of excessive alcohol intake to increase both cholesterol levels and risks for suicide (Golomb et al., 2004).
Biological evidence linking cholesterol and suicidality derives from demonstrated relationships between cholesterol concentrations and serotonin measures. Serotonergic dysfunction is a well-established substrate for suicidal behavior (Mann et al., 1999; Mann et al., 2001), a relationship apparently mediated by increased aggressivity (Golomb, 1998; Oquendo et al., - In press.). Low plasma concentrations of cholesterol in turn, have been associated with low platelet 5-HT content (Delva et al., 1996), low plasma serotonin concentrations (Steegmans et al., 1996) and blunted neuroendocrine responses to MCPP (Terao et al., 1997) or fenfluramine (Muldoon et al., 1992).
Fawcett et al (Fawcett et al., 1997) has proposed that serotonergic function and HPA-axis hyperactivity comprise independent risk factors for suicide. The former is thought to result in impulsivity and the latter in psychic pain and agitation. Insofar as both processes are independent of the other, biological measures of them should be additive in their implication of risk.
2. Methods
2.1. Subjects
An earlier report described this sample in detail (Coryell and Schlesser, 2001). Briefly, 78 individuals with Research Diagnostic Criteria (Spitzer et al., 1978) unipolar (n = 59), bipolar I (n=10), bipolar II (n = 9) or schizoaffective (n = 2) depression entered the NIMH Collaborative Depression Study (CDS) as inpatients at the Iowa site between 1978 and 1981 and, during their hospitalization, underwent a 1 mg. DST. The DST was not included among CDS assessments but many of the subjects also participated in a concurrent study of the diagnostic correlates of dexamethasone suppression (Schlesser et al., 1980). In other cases attendings obtained the test for clinical purposes.
2.2. Procedures
All CDS participants underwent extensive baseline clinical assessments that included the schedule for affective disorders and schizophrenia (Endicott and Spitzer, 1978). The DST was typically obtained within three days of admission and post-dexamethasone cortisol samples drawn at 8 a.m., 4 p.m. and/or 11 p.m.
All subjects entered a follow-up study with direct interviews scheduled at six-month intervals for the first five years and annually thereafter.
Raters learned of completed suicides as they attempted to schedule further interviews with a given subject. In these instances, attempts were made to interview family members as to the circumstances. All identifying data for all subjects had been screened with the National Death Index at intervals so that the mortality status of subjects lost to follow-up has been ascertained. As reported previously (Coryell and Schlesser, 2001), seven (21.9%) of 32 patients with a post-dexamethasone cortisol greater than 5 μg/dl indicating nonsuppression, committed suicide in the ensuing 10 years while only one (2.2%) of the remaining 46 patients did so.
A fasting serum cholesterol determination was one of the routine admission tests obtained on the University of Iowa psychiatric units during the three years of CDS intake. A review of medical records identified values for 74 of these 78 patients.
2.3. Data analysis
Univariate comparisons of continuous variables used t-tests. Cox regression analyses were used to assess relationships between serum cholesterol concentration, DST result and the demographic variables age and sex. Survival analyses were also used to derive cumulative probabilities of suicide across groupings based on baseline cholesterol measures. All tests for significance were two-tailed with P set at 0.05.
3. Results
The eight patients who eventually committed suicide, and the remaining 66 patients, had mean (SD) fasting serum cholesterol concentrations of 185.4 (46.2) mg/dl and 213.6 (43.9) mg/dl, respectively (t = −1.709, df = 72, P = 0.092). Suicides and nonsuicides did not differ significantly by age. Mean (SD) values were 39.4 (16.7) and 35.4 (14.2), respectively. Cholesterol concentrations did increase significantly with age, however (r = 0.458, P < 0.0001) and, when age was entered as a covariate in a Cox regression analysis, the relationship between baseline cholesterol concentration and eventual suicide was significant (Wald X2 = 4.7, df = 1, P = 0.030). Five (62.5%) of the 8 suicides and 43 (65.2%) of the nonsuicides were female. Results were little changed when sex was added as well (Wald X2 = 4.6, df = 1, P = 0.032). An ROC analysis indicated that a threshold of 190 mg/dl yielded the best balance of sensitivity (0.56) and specificity (0.74).
Cholesterol concentrations did not differ by DST suppressor status; mean (SD) values were 204.1 (43.7) mg/dl and 215.2 (45.3) mg/dl for patients who were nonsuppressors and those who were suppressors, respectively. Within the latter group, the sole patient who suicided had a baseline cholesterol value of 166 while the remaining subjects had a mean (SD) value of 216.3 (45.2) (nonsignificant). Among those who had been DST nonsuppressors, the seven who suicided had a mean (SD) baseline cholesterol concentration of 188.1 (49.1) and the remaining nonsuppressors had a mean (SD) value of 210.7 (42.2) (nonsignificant).
Previous studies of serum cholesterol levels and subsequent suicide divided cholesterol values into either three (Partonen et al., 1999) or four (Lindberg et al., 1992; Ellison and Morrison, 2001) groups. Because of the limited size of the current sample, values were ranked into three equal groups and the third with values less than or equal to 190 mg/dl were designated as high risk. Four (17.4%) of these 23 subjects and 4 (7.8%) of the remaining 52, committed suicide. A Kaplan-Meier hazard function (Fig. 1) showed that the differential risk increased progressively over the fifteen-year follow-up. The cumulative survival estimations for those with low cholesterol concentrations and for the remaining subjects were 77.3% and 81.2%, respectively.
Figure 1.
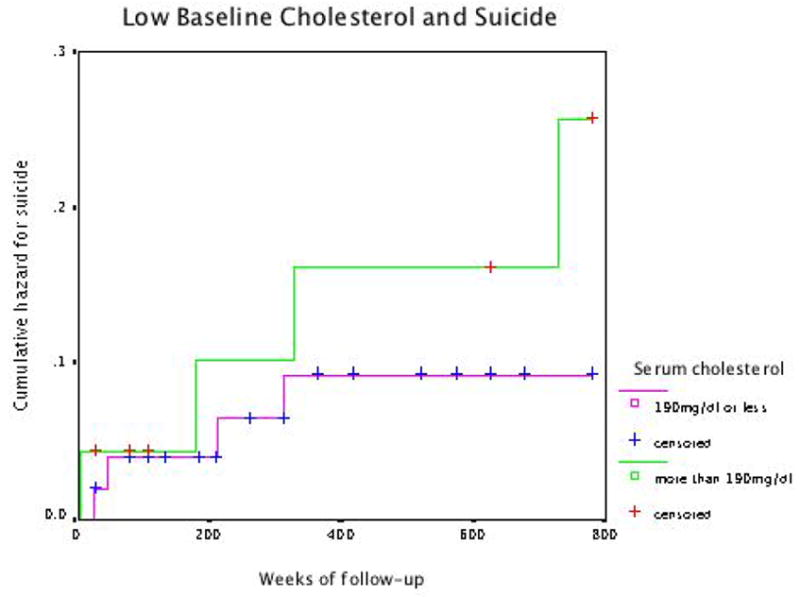
Low Baseline Cholesterol and Sucide
The proportion of patients who committed suicide increased in a stepwise fashion from those who had both a normal DST result and serum cholesterol values above the bottom third to those who had an abnormal DST result and cholesterol levels in the lowest third of the distribution (Table 1).
Table 1.
Risk Indicators and Suicide
| plasma cholesterol ≤190 mg/dl | DST nonsuppression | n | # (%) suicide | Survival analysis: cumulative probability, % |
|---|---|---|---|---|
| no | no | 30 | 0 | 0 |
| yes | no | 13 | 1 (7.7%) | 10.0 |
| no | yes | 21 | 4 (19.0) | 20.9 |
| yes | yes | 10 | 3 (30.0) | 40.9 |
4. Discussion
With control for age and sex, lower baseline serum cholesterol concentrations were clearly associated with eventual suicide in this group of inpatients with MDD. DST results were also predictive of eventual suicide yet bore little relationship to cholesterol concentrations. These findings are consistent with the hypothesis that HPA-axis hyperactivity and serotonergic deficits, here implied by low serum cholesterol levels, comprise orthogonal risk factors for suicide.
The clinical application of these two determinations presupposes appropriate thresholds to separate test results indicative of high risk from those that imply lower risk. A threshold of 5μg/dl for cortisol levels drawn at 0800 or 1400 following dexamethasone at 2300 is the most widely used to designate individuals as having HPA-axis hyperactivity but this was derived as being optimal for the separation of melancholia and nonmelancholic conditions rather than the prediction of eventual suicide. A different threshold appears to offer a better separation of psychotic and nonpsychotic MDD (Schatzberg et al., 1983) and the same may be true for the identification of eventually suicidal MDD patients. This possibility has not been explored. Unfortunately, our working data set lists each individual’s suppressor status but not their post-dexamethasone cortisol values.
Likewise, the four studies that have described associations between baseline cholesterol and subsequent suicide assigned subjects to three or four groups on the basis of these concentrations and found that the risk for suicide fell progressively across groups from low to high concentrations (Lindberg et al., 1992; Neaton et al., 1992; Zureik et al., 1996; Ellison and Morrison, 2001). Though none of these studies conducted ROC analyses to identify optimal thresholds, the step-wise increase in risk across groups of three and four suggest that a clear breakpoint may not have emerged.
As did Lindberg et al (Lindberg et al., 1992), we found that the relationship between serum cholesterol concentration and subsequent suicide was significant only with control for age. This renders more problematic the use of cholesterol concentrations as a clinical tool for estimating suicide risk in that thresholds appropriate for specific age cohorts will apparently be necessary. Because low cholesterol levels have been associated with suicide in large community-based studies, normal distributions from the ambient population may supply provisional thresholds.
Acknowledgments
Funded by NIMH grant MH 25416
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Citations
- Alvarez JC, Cremniter D, Gluck N, Quintin P, Leboyer M, Berlin I, Therond P, Spreux-Varoquaux O. Low serum cholesterol in violent but not in non-violent suicide attempters. Psychiatry Research. 2000;95:103–108. doi: 10.1016/s0165-1781(00)00171-2. [DOI] [PubMed] [Google Scholar]
- Alvarez JC, Cremniter D, Lesieur P, Gregoire A, Gilton A, Macquin-Mavier I, Jarreau C, Spreux-Varoquaux O. Low blood cholesterol and low platelet serotonin levels in violent suicide attempters. Biological Psychiatry. 1999;45:1066–1069. doi: 10.1016/s0006-3223(98)00160-7. [DOI] [PubMed] [Google Scholar]
- Atmaca M, Kuloglu M, Tezcan E, Ustundag B. Serum leptin and cholesterol levels in schizophrenic patients with and without suicide attempts. Acta Psychiatrica Scandinavica. 2003;108:208–214. doi: 10.1034/j.1600-0447.2003.00145.x. [DOI] [PubMed] [Google Scholar]
- Barraclough B, Bunch J, Nelson B, Sainsbury P. A hundred cases of suicide: clinical aspects. British Journal of Psychiatry. 1974;125:355–373. doi: 10.1192/bjp.125.4.355. [DOI] [PubMed] [Google Scholar]
- Bocchetta A, Chillotti C, Carboni G, Oi A, Ponti M, Del Zompo M. Association of personal and familial suicide risk with low serum cholesterol concentration in male lithium patients. Acta Psychiatrica Scandinavica. 2001;104:37–41. doi: 10.1034/j.1600-0447.2001.00374.x. [DOI] [PubMed] [Google Scholar]
- Coryell W, Schlesser M. The dexamethasone suppression test and suicide prediction. American Journal of Psychiatry. 2001;158:748–753. doi: 10.1176/appi.ajp.158.5.748. [DOI] [PubMed] [Google Scholar]
- Coryell W, Young E. Suicide in primary MDD: a twenty-one year follow-up. Journal of Clinical Psychiatry in press. [Google Scholar]
- Delva NJ, Matthews DR, Cowen PJ. Brain serotonin (5-HT) neuroendocrine function in patients taking cholesterol-lowering drugs. Biological Psychiatry. 1996;39:100–106. doi: 10.1016/0006-3223(95)00140-9. [DOI] [PubMed] [Google Scholar]
- Dorovini-Zis K, Zis AP. Increased adrenal weight in victims of violent suicide. American Journal of Psychiatry. 1987;144:1214–1215. doi: 10.1176/ajp.144.9.1214. [DOI] [PubMed] [Google Scholar]
- Ellison LF, Morrison HI. Low serum cholesterol concentration and risk of suicide. Epidemiology. 2001;12:168–172. doi: 10.1097/00001648-200103000-00007. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Favaro A, Caregaro L, Di Pascoli L, Brambilla F, Santonastaso P. Total serum cholesterol and suicidality in anorexia nervosa. Psychosomatic Medicine. 2004;66:548–552. doi: 10.1097/01.psy.0000127873.31062.80. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Busch KA, Jacobs D, Kravitz HM, Fogg L. Suicide: a four-pathway clinical-biochemical model. Annals of the New York Academy of Sciences. 1997;836:288–301. doi: 10.1111/j.1749-6632.1997.tb52366.x. [DOI] [PubMed] [Google Scholar]
- Gallerani M, Manfredini R, Caracciolo S, Scapoli C, Molinari S, Fersini C. Serum cholesterol concentrations in parasuicide. British Medical Journal. 1995;310:1632–1636. doi: 10.1136/bmj.310.6995.1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland M, Hickey D, Corvin A, Golden J, Fitzpatrick P, Cunningham S, Walsh N. Total serum cholesterol in relation to psychological correlates in parasuicide. British Journal of Psychiatry. 2000;177:77–83. doi: 10.1192/bjp.177.1.77. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Archives of General Psychiatry. 1991;48:418–422. doi: 10.1001/archpsyc.1991.01810290030004. [DOI] [PubMed] [Google Scholar]
- Golomb BA. Cholesterol and violence: is there a connection? Annals of Internal Medicine. 1998;128:478–487. doi: 10.7326/0003-4819-128-6-199803150-00009. [DOI] [PubMed] [Google Scholar]
- Golomb BA, Criqui MH, White H, Dimsdale JE. Conceptual foundations of the UCSD Statin Study: a randomized controlled trial assessing the impact of statins on cognition, behavior, and biochemistry. Archives of Internal Medicine. 2004;164:153–162. doi: 10.1001/archinte.164.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillem E, Pelissolo A, Notides C, Lepine JP. Relationship between attempted suicide, serum cholesterol level and novelty seeking in psychiatric in-patients. Psychiatry Research. 2002;112:83–88. doi: 10.1016/s0165-1781(02)00193-2. [DOI] [PubMed] [Google Scholar]
- Kim YK, Myint AM. Clinical application of low serum cholesterol as an indicator for suicide risk in major depression. Journal of Affective Disorders. 2004;81:161–166. doi: 10.1016/S0165-0327(03)00166-6. [DOI] [PubMed] [Google Scholar]
- Kunugi H, Takei N, Aoki H, Nanko S. Low serum cholesterol in suicide attempters. Biological Psychiatry. 1997;41:196–200. doi: 10.1016/S0006-3223(95)00672-9. [DOI] [PubMed] [Google Scholar]
- Lindberg G, Rastam L, Gullberg B, Eklund GA. Low serum cholesterol concentration and short term mortality from injuries in men and women. British Medical Journal. 1992;305:277–279. doi: 10.1136/bmj.305.6848.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann JJ, Brent DA, Arango V. The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology. 2001;24:467–477. doi: 10.1016/S0893-133X(00)00228-1. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. American Journal of Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Modai I, Valevski A, Dror S, Weizman A. Serum cholesterol levels and suicidal tendencies in psychiatric inpatients. Journal of Clinical Psychiatry. 1994;55:252–254. [PubMed] [Google Scholar]
- Muldoon MF, Kaplan JR, Manuck SB, Mann JJ. Effects of a low-fat diet on brain serotonergic responsivity in cynomolgus monkeys. Biological Psychiatry. 1992;31:739–742. doi: 10.1016/0006-3223(92)90285-8. [DOI] [PubMed] [Google Scholar]
- Neaton JD, Blackburn H, Jacobs D, Kuller L, Lee DJ, Sherwin R, Shih J, Stamler J, Wentworth D. Serum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Archives of Internal Medicine. 1992;152:1490–1500. [PubMed] [Google Scholar]
- Nemeroff CB, Owens MJ, Bissette G, Andorn AC, Stanley M. Reduced corticotropin releasing factor binding sites in the frontal cortex of suicide victims. Archives of General Psychiatry. 1988;45:577–579. doi: 10.1001/archpsyc.1988.01800300075009. [DOI] [PubMed] [Google Scholar]
- Obrocea GV, Dunn RM, Frye MA, Ketter TA, Luckenbaugh DA, Leverich GS, Speer AM, Osuch EA, Jajodia K, Post RM. Clinical predictors of response to lamotrigine and gabapentin monotherapy in refractory affective disorders. Biological Psychiatry. 2002;51:253–260. doi: 10.1016/s0006-3223(01)01206-9. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Russo SA, Underwood MD, Kassir SA, Ellis SP, Mann JJ, Arango V. Higher Postmortem Prefrontal 5-HT(2A) Receptor Binding Correlates with Lifetime Aggression in Suicide. Biological Psychiatry. doi: 10.1016/j.biopsych.2005.06.037. In press. [DOI] [PubMed] [Google Scholar]
- Ozer OA, Kutanis R, Agargun MY, Besiroglu L, Bal AC, Selvi Y, Kara H. Serum lipid levels, suicidality, and panic disorder. Comprehensive Psychiatry. 2004;45:95–98. doi: 10.1016/j.comppsych.2003.12.004. [DOI] [PubMed] [Google Scholar]
- Papassotiropoulos A, Hawellek B, Frahnert C, Rao GS, Rao ML. The risk of acute suicidality in psychiatric inpatients increases with low plasma cholesterol. Pharmacopsychiatry. 1999;32:1–4. doi: 10.1055/s-2007-979181. [DOI] [PubMed] [Google Scholar]
- Partonen T, Haukka J, Virtamo J, Taylor PR, Lonnqvist J. Association of low serum total cholesterol with major depression and suicide. British Journal of Psychiatry. 1999;175:259–262. doi: 10.1192/bjp.175.3.259. [DOI] [PubMed] [Google Scholar]
- Rao VP, Krishnan KR, Goli V, Saunders WB, Ellinwood EH, Jr, Blazer DG, Nemeroff CB. Neuroanatomical changes and hypothalamo-pituitary-adrenal axis abnormalities. Biological Psychiatry. 1989;26:729–732. doi: 10.1016/0006-3223(89)90108-x. [DOI] [PubMed] [Google Scholar]
- Sarchiapone M, Roy A, Camardese G, De Risio S. Further evidence for low serum cholesterol and suicidal behaviour. Journal of Affective Disorders. 2000;61:69–71. doi: 10.1016/s0165-0327(99)00198-6. [DOI] [PubMed] [Google Scholar]
- Schatzberg AF, Orsulak PJ, Rothschild AJ, Salomon MS, Lerbinger J, Kizuka PP, Cole JO, Schildkraut JJ. Platelet MAO activity and the dexamethasone suppression test in depressed patients. American Journal of Psychiatry. 1983;140:1231–1233. doi: 10.1176/ajp.140.9.1231. [DOI] [PubMed] [Google Scholar]
- Schlesser MA, Winokur G, Sherman BM. Hypothalamic-pituitary-adrenal axis activity in depressive illness. Its relationship to classification. Archives of General Psychiatry. 1980;37:737–743. doi: 10.1001/archpsyc.1980.01780200015001. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Steegmans PH, Fekkes D, Hoes AW, Bak AA, van der Does E, Grobbee DE. Low serum cholesterol concentration and serotonin metabolism in men. British Medical Journal. 1996;312:221. doi: 10.1136/bmj.312.7025.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szigethy E, Conwell Y, Forbes NT, Cox C, Caine ED. Adrenal weight and morphology in victims of completed suicide. Biological Psychiatry. 1994;36:374–380. doi: 10.1016/0006-3223(94)91212-2. [DOI] [PubMed] [Google Scholar]
- Tanskanen A, Vartiainen E, Tuomilehto J, Viinamaki H, Lehtonen J, Puska P. High serum cholesterol and risk of suicide. American Journal of Psychiatry. 2000;157:648–650. doi: 10.1176/appi.ajp.157.4.648. [DOI] [PubMed] [Google Scholar]
- Terao T, Yoshimura R, Ohmori O, Takano T, Takahashi N, Iwata N, Suzuki T, Abe K. Effect of serum cholesterol levels on meta-chlorophenylpiperazine-evoked neuroendocrine responses in healthy subjects. Biological Psychiatry. 1997;41:974–978. doi: 10.1016/S0006-3223(96)00213-2. [DOI] [PubMed] [Google Scholar]
- Tripodianakis J, Markianos M, Sarantidis D, Agouridaki M. Biogenic amine turnover and serum cholesterol in suicide attempt. European Archives of Psychiatry and Clinical Neuroscience. 2002;252:38–43. doi: 10.1007/s004060200007. [DOI] [PubMed] [Google Scholar]
- Zureik M, Courbon D, Ducimetiere P. Serum cholesterol concentration and death from suicide in men: Paris prospective study I. British Medical Journal. 1996;313:649–651. doi: 10.1136/bmj.313.7058.649. [DOI] [PMC free article] [PubMed] [Google Scholar]


