Abstract
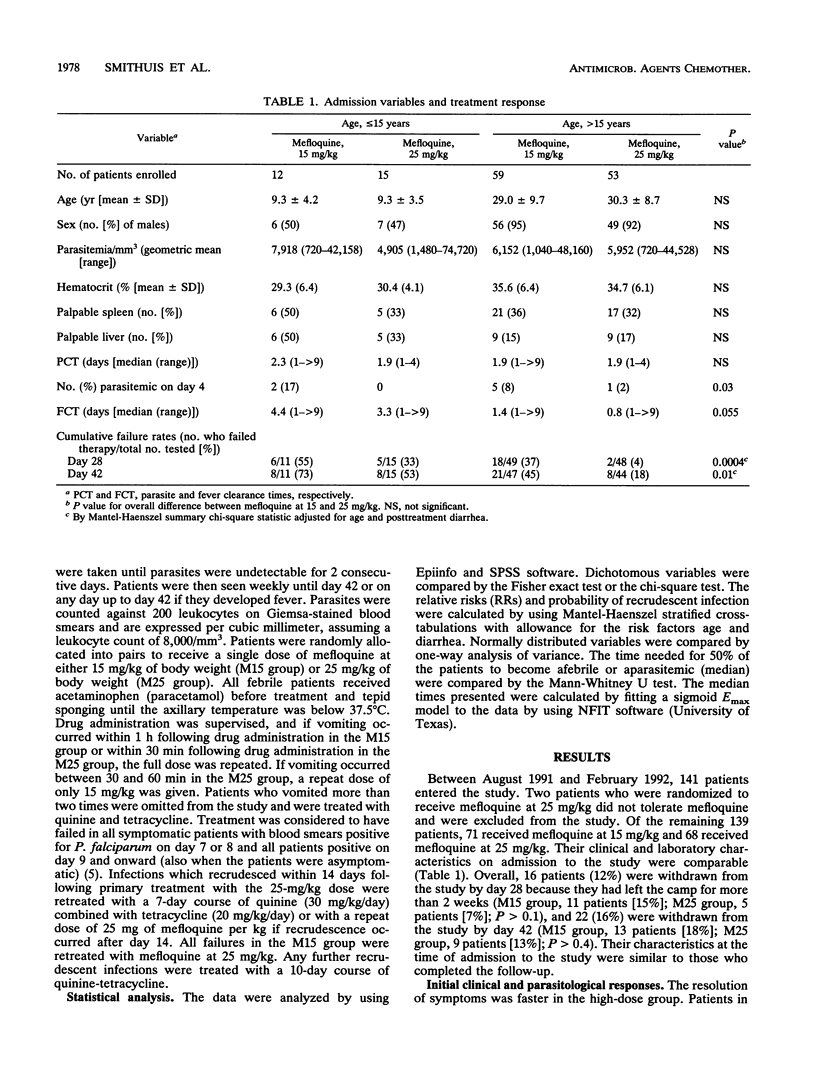
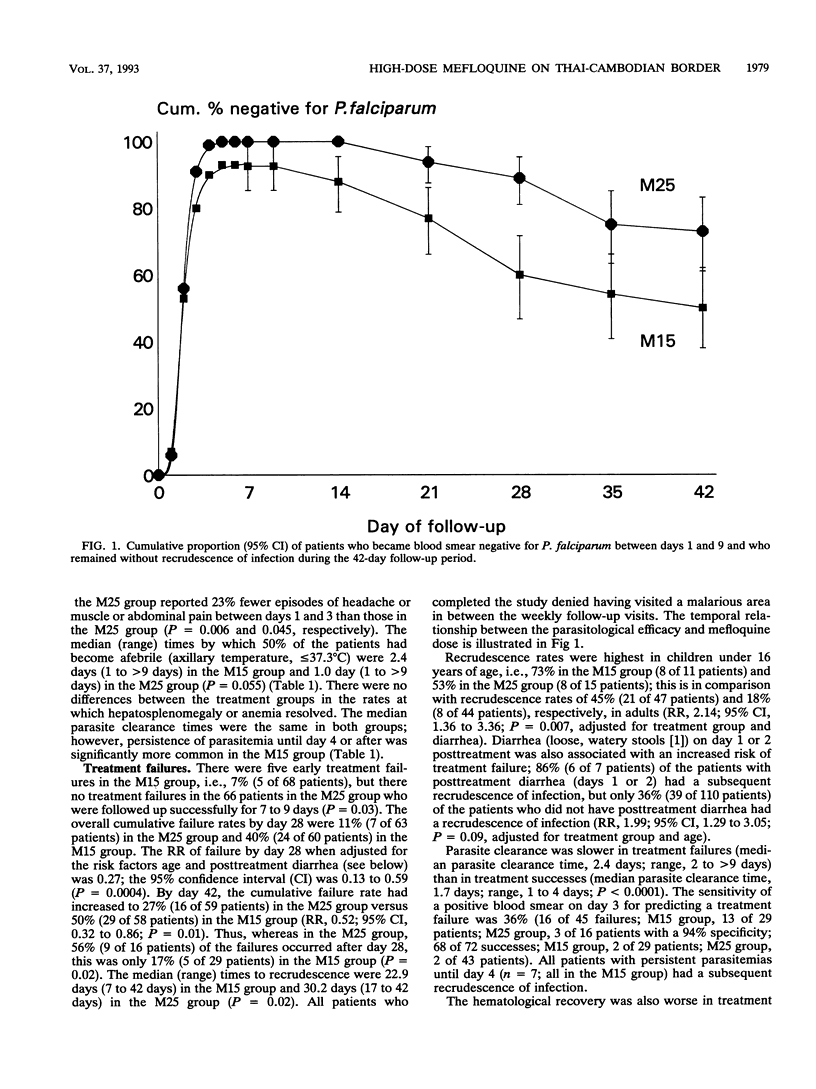
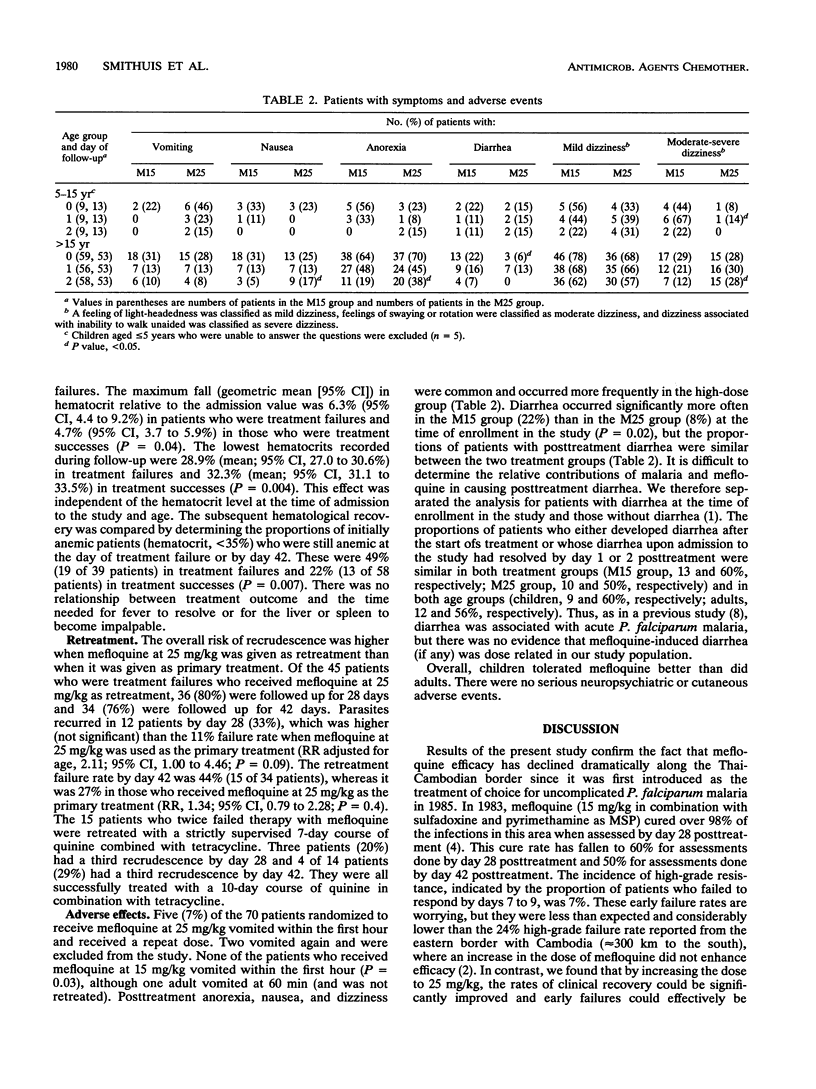
In 1991 and 1992, a prospective randomized trial was conducted on the northern Thai-Cambodian border. That trial compared the efficacy and tolerance of two mefloquine regimens for the treatment of uncomplicated Plasmodium falciparum malaria in an area with multi-drug-resistant P. falciparum. The resolution of fever and other symptoms was faster with high-dose mefloquine (25 mg/kg of body weight [M25 group; n = 68]) than with the conventional 15-mg/kg dose (M15 group; n = 71). There were no early treatment failures (days 7 to 9) in the M25 group, but there were 5 (7%) treatment failures in the M15 group (P = 0.03). The incidences of treatment failures by day 28 were 40% with the M15 group and 11% with the M25 group (P = 0.0004). By day 42, these values had risen to 50 and 27%, respectively (P = 0.01). The risk of treatment failure was highest in children (relative risk, 2.1; 95% confidence interval, 1.3 to 3.4) and patients with posttreatment diarrhea (relative risk, 2.0; 95% confidence interval, 1.3 to 3.1). Over half of the recrudescences in the M25 group occurred between days 28 and 42, whereas 17% of the recrudescences in the M15 group occurred between days 28 and 42 (P = 0.02). Thus, the sensitivity of assessment was significantly increased with longer follow-up. Treatment failure was associated with a delayed parasite clearance and an inadequate hematological recovery. Upper gastrointestinal side effects and dizziness were significantly more common in the M25 group, but overall, the high dose was relatively well tolerated, in particular by children. An increase in the dose to 25 mg/kg can prolong the therapeutic use of mefloquine in areas with multi-drug-resistant P.falciparum malaria where high-grade resistance to mefloquine is still rare.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boudreau E. F., Fleckenstein L., Pang L. W., Childs G. E., Schroeder A. C., Ratnaratorn B., Phintuyothin P. Mefloquine kinetics in cured and recrudescent patients with acute falciparum malaria and in healthy volunteers. Clin Pharmacol Ther. 1990 Oct;48(4):399–409. doi: 10.1038/clpt.1990.168. [DOI] [PubMed] [Google Scholar]
- Looareesuwan S., Harinasuta T., Chongsuphajaisiddhi T. Drug resistant malaria, with special reference to Thailand. Southeast Asian J Trop Med Public Health. 1992 Dec;23(4):621–634. [PubMed] [Google Scholar]
- Meek S. R., Doberstyn E. B., Gaüzère B. A., Thanapanich C., Nordlander E., Phuphaisan S. Treatment of falciparum malaria with quinne and tetracycline or combined mefloquine/sulfadoxine/pyrimethamine on the Thai-Kampuchean border. Am J Trop Med Hyg. 1986 Mar;35(2):246–250. doi: 10.4269/ajtmh.1986.35.246. [DOI] [PubMed] [Google Scholar]
- Nosten F., ter Kuile F., Chongsuphajaisiddhi T., Luxemburger C., Webster H. K., Edstein M., Phaipun L., Thew K. L., White N. J. Mefloquine-resistant falciparum malaria on the Thai-Burmese border. Lancet. 1991 May 11;337(8750):1140–1143. doi: 10.1016/0140-6736(91)92798-7. [DOI] [PubMed] [Google Scholar]
- White N. J. Antimalarial drug resistance: the pace quickens. J Antimicrob Chemother. 1992 Nov;30(5):571–585. doi: 10.1093/jac/30.5.571. [DOI] [PubMed] [Google Scholar]
- ter Kuile F. O., Dolan G., Nosten F., Edstein M. D., Luxemburger C., Phaipun L., Chongsuphajaisiddhi T., Webster H. K., White N. J. Halofantrine versus mefloquine in treatment of multidrug-resistant falciparum malaria. Lancet. 1993 Apr 24;341(8852):1044–1049. doi: 10.1016/0140-6736(93)92409-m. [DOI] [PubMed] [Google Scholar]
- ter Kuile F. O., Nosten F., Thieren M., Luxemburger C., Edstein M. D., Chongsuphajaisiddhi T., Phaipun L., Webster H. K., White N. J. High-dose mefloquine in the treatment of multidrug-resistant falciparum malaria. J Infect Dis. 1992 Dec;166(6):1393–1400. doi: 10.1093/infdis/166.6.1393. [DOI] [PubMed] [Google Scholar]



