Abstract
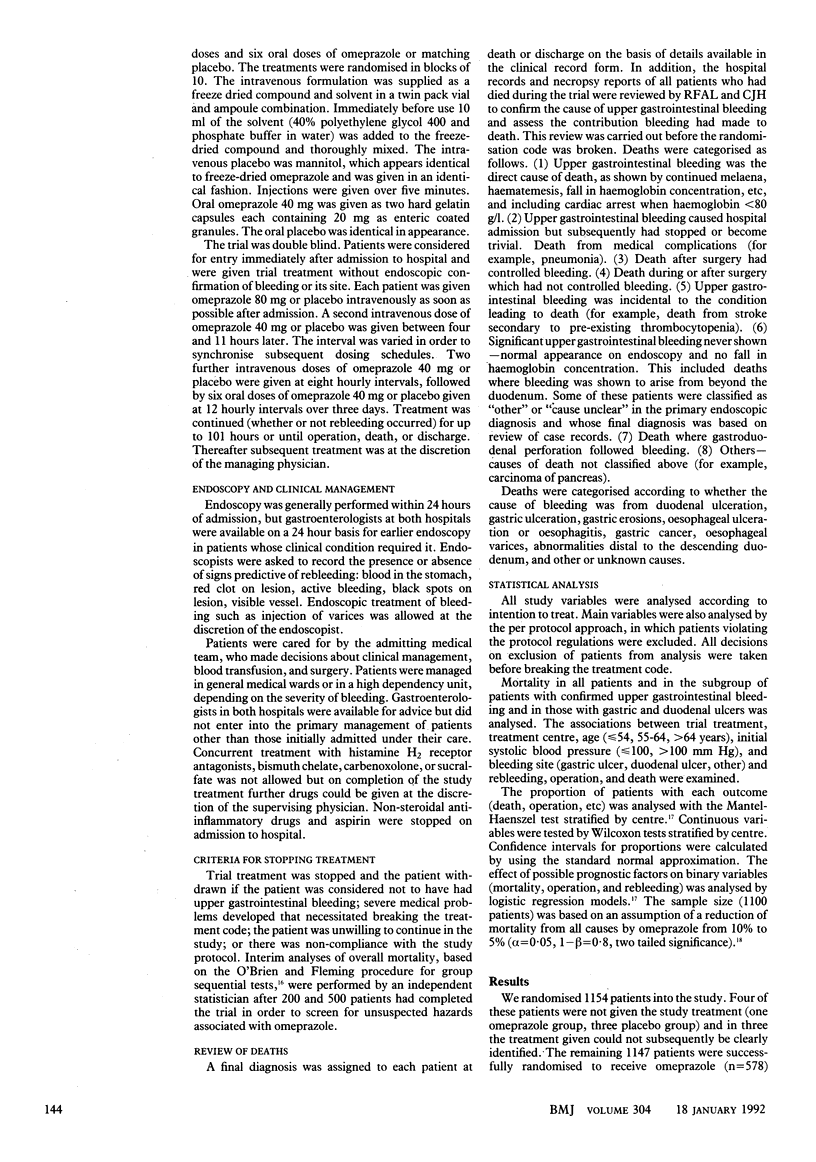
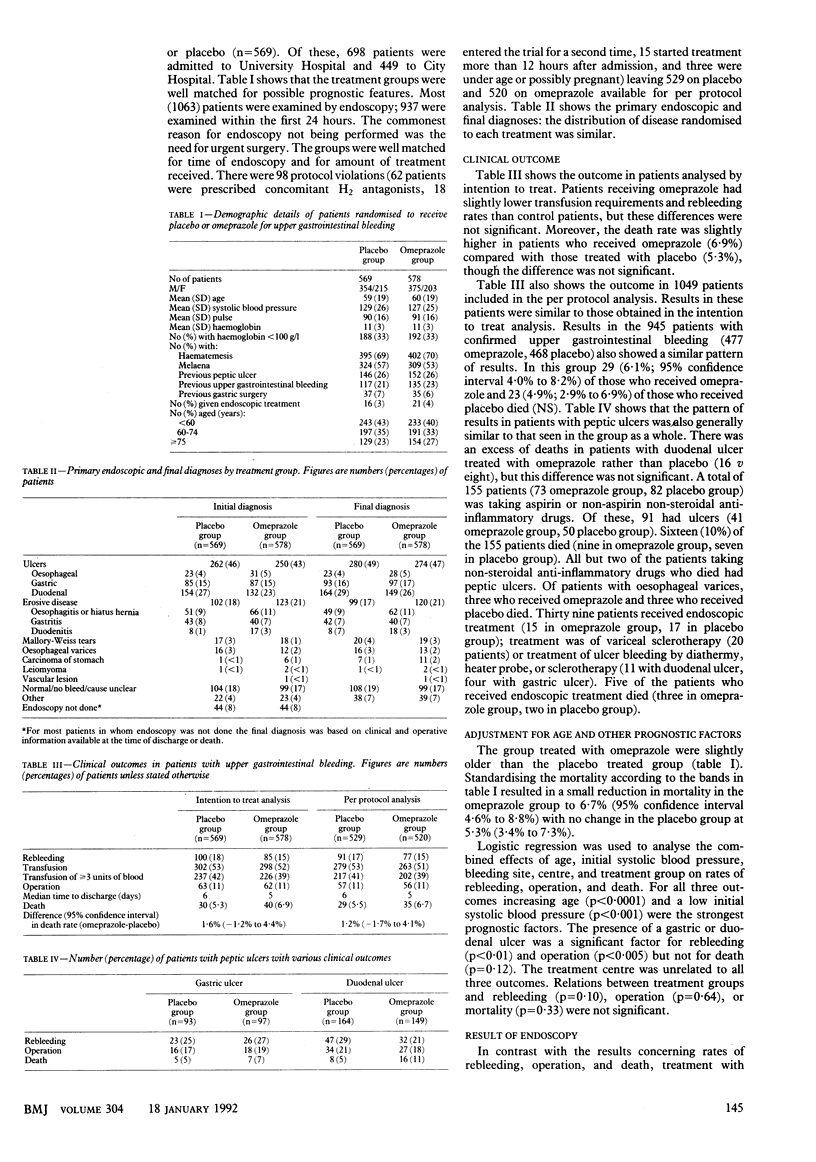
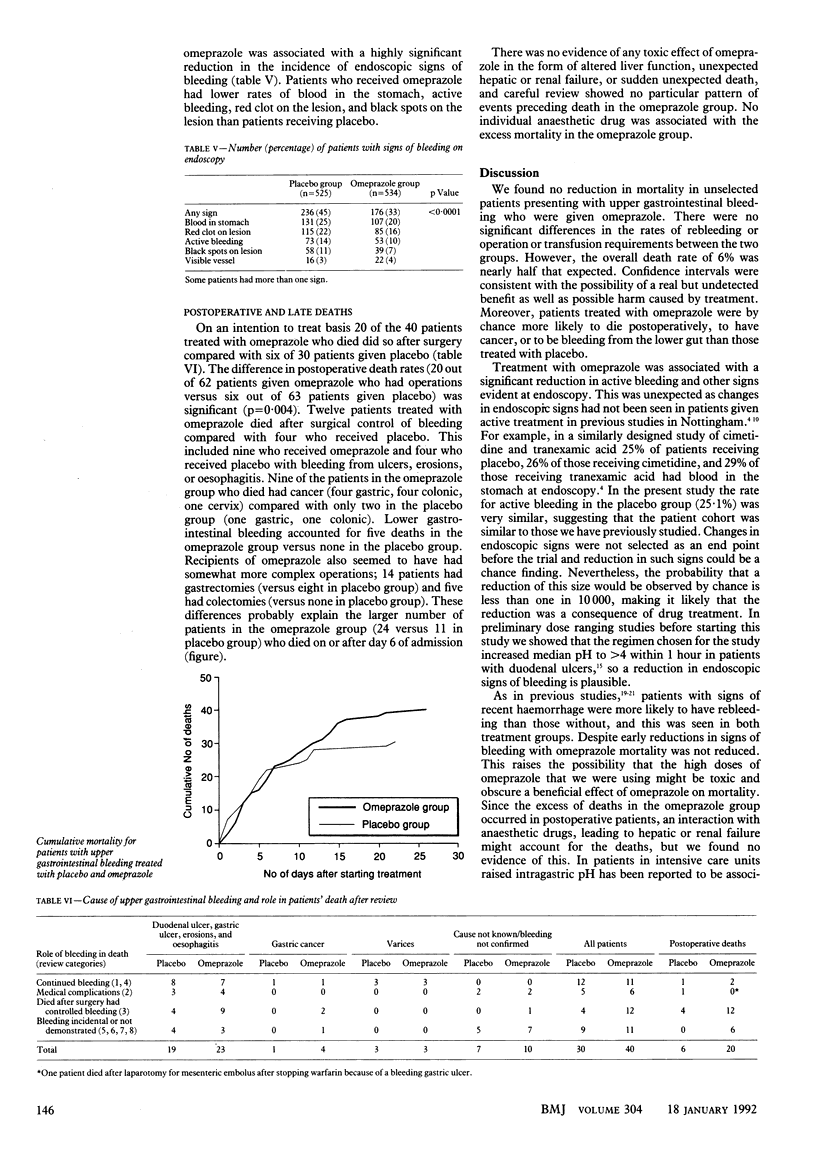
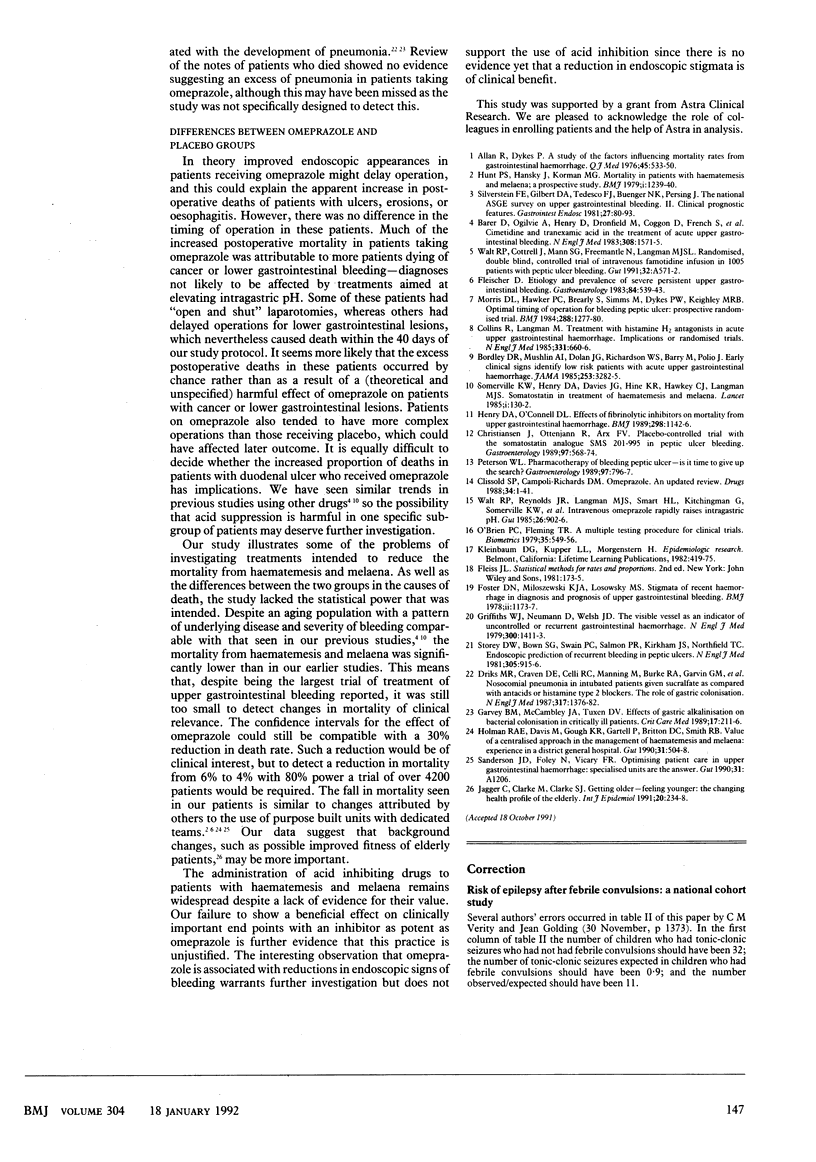
OBJECTIVE--To investigate the possible therapeutic role of omeprazole, a powerful proton pump inhibitor, in unselected patients presenting with upper gastrointestinal bleeding. DESIGN--Double blind placebo controlled parallel group study. Active treatment was omeprazole 80 mg intravenously immediately, then three doses of 40 mg intravenously at eight hourly intervals, then 40 mg orally at 12 hourly intervals. Treatment was started within 12 hours of admission and given for four days or until surgery, discharge, or death. SETTING--The medical wards of University and City Hospitals, Nottingham. SUBJECTS--1147 consecutive patients aged 18 years or more admitted over 40 months with acute upper gastrointestinal bleeding. MAIN OUTCOME MEASURES--Mortality from all causes; rate of rebleeding, transfusion requirements, and operation rate; effect of treatment on endoscopic appearances at initial endoscopy. RESULTS--Of 1147 patients included in the intention to treat analysis, 569 received placebo and 578 omeprazole. No significant differences were found between the placebo and omeprazole groups for rates of transfusion (302 (53%) placebo v 298 (52%) omeprazole), rebleeding (100 (18%) v 85 (15%)), operation (63 (11%) v 62 (11%)), and death (30 (5.3%) v 40 (6.9%)). However, there was an unexpected but significant reduction in endoscopic signs of upper gastrointestinal bleeding in patients treated with omeprazole compared with those treated with placebo (236 (45%) placebo v 176 (33%) omeprazole; p less than 0.0001). CONCLUSIONS--Omeprazole failed to reduce mortality, rebleeding, or transfusion requirements, although the reduction in endoscopic signs of bleeding suggests that inhibition of acid may be capable of influencing intragastric bleeding. Our data do not justify the routine use of acid inhibiting drugs in the management of haematemesis and melaena.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allan R., Dykes P. A study of the factors influencing mortality rates from gastrointestinal haemorrhage. Q J Med. 1976 Oct;45(180):533–550. [PubMed] [Google Scholar]
- Barer D., Ogilvie A., Henry D., Dronfield M., Coggon D., French S., Ellis S., Atkinson M., Langman M. Cimetidine and tranexamic acid in the treatment of acute upper-gastrointestinal-tract bleeding. N Engl J Med. 1983 Jun 30;308(26):1571–1575. doi: 10.1056/NEJM198306303082606. [DOI] [PubMed] [Google Scholar]
- Bordley D. R., Mushlin A. I., Dolan J. G., Richardson W. S., Barry M., Polio J., Griner P. F. Early clinical signs identify low-risk patients with acute upper gastrointestinal hemorrhage. JAMA. 1985 Jun 14;253(22):3282–3285. [PubMed] [Google Scholar]
- Christiansen J., Ottenjann R., Von Arx F. Placebo-controlled trial with the somatostatin analogue SMS 201-995 in peptic ulcer bleeding. Gastroenterology. 1989 Sep;97(3):568–574. doi: 10.1016/0016-5085(89)90626-4. [DOI] [PubMed] [Google Scholar]
- Collins R., Langman M. Treatment with histamine H2 antagonists in acute upper gastrointestinal hemorrhage. Implications of randomized trials. N Engl J Med. 1985 Sep 12;313(11):660–666. doi: 10.1056/NEJM198509123131104. [DOI] [PubMed] [Google Scholar]
- Driks M. R., Craven D. E., Celli B. R., Manning M., Burke R. A., Garvin G. M., Kunches L. M., Farber H. W., Wedel S. A., McCabe W. R. Nosocomial pneumonia in intubated patients given sucralfate as compared with antacids or histamine type 2 blockers. The role of gastric colonization. N Engl J Med. 1987 Nov 26;317(22):1376–1382. doi: 10.1056/NEJM198711263172204. [DOI] [PubMed] [Google Scholar]
- Garvey B. M., McCambley J. A., Tuxen D. V. Effects of gastric alkalization on bacterial colonization in critically ill patients. Crit Care Med. 1989 Mar;17(3):211–216. doi: 10.1097/00003246-198903000-00002. [DOI] [PubMed] [Google Scholar]
- Griffiths W. J., Neumann D. A., Welsh J. D. The visible vessel as an indicator of uncontrolled or recurrent gastrointestinal hemorrhage. N Engl J Med. 1979 Jun 21;300(25):1411–1413. doi: 10.1056/NEJM197906213002503. [DOI] [PubMed] [Google Scholar]
- Henry D. A., O'Connell D. L. Effects of fibrinolytic inhibitors on mortality from upper gastrointestinal haemorrhage. BMJ. 1989 Apr 29;298(6681):1142–1146. doi: 10.1136/bmj.298.6681.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman R. A., Davis M., Gough K. R., Gartell P., Britton D. C., Smith R. B. Value of a centralised approach in the management of haematemesis and melaena: experience in a district general hospital. Gut. 1990 May;31(5):504–508. doi: 10.1136/gut.31.5.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger C., Clarke M., Clarke S. J. Getting older--feeling younger: the changing health profile of the elderly. Int J Epidemiol. 1991 Mar;20(1):234–238. doi: 10.1093/ije/20.1.234. [DOI] [PubMed] [Google Scholar]
- Morris D. L., Hawker P. C., Brearley S., Simms M., Dykes P. W., Keighley M. R. Optimal timing of operation for bleeding peptic ulcer: prospective randomised trial. Br Med J (Clin Res Ed) 1984 Apr 28;288(6426):1277–1280. doi: 10.1136/bmj.288.6426.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien P. C., Fleming T. R. A multiple testing procedure for clinical trials. Biometrics. 1979 Sep;35(3):549–556. [PubMed] [Google Scholar]
- Peterson W. L. Pharmacotherapy of bleeding peptic ulcer--is it time to give up the search? Gastroenterology. 1989 Sep;97(3):796–797. doi: 10.1016/0016-5085(89)90657-4. [DOI] [PubMed] [Google Scholar]
- Silverstein F. E., Gilbert D. A., Tedesco F. J., Buenger N. K., Persing J. The national ASGE survey on upper gastrointestinal bleeding. II. Clinical prognostic factors. Gastrointest Endosc. 1981 May;27(2):80–93. doi: 10.1016/s0016-5107(81)73156-0. [DOI] [PubMed] [Google Scholar]
- Somerville K. W., Henry D. A., Davies J. G., Hine K. R., Hawkey C. J., Langman M. J. Somatostatin in treatment of haematemesis and melaena. Lancet. 1985 Jan 19;1(8421):130–132. doi: 10.1016/s0140-6736(85)91903-8. [DOI] [PubMed] [Google Scholar]
- Walt R. P., Reynolds J. R., Langman M. J., Smart H. L., Kitchingman G., Somerville K. W., Hawkey C. J. Intravenous omeprazole rapidly raises intragastric pH. Gut. 1985 Sep;26(9):902–906. doi: 10.1136/gut.26.9.902. [DOI] [PMC free article] [PubMed] [Google Scholar]


