Abstract
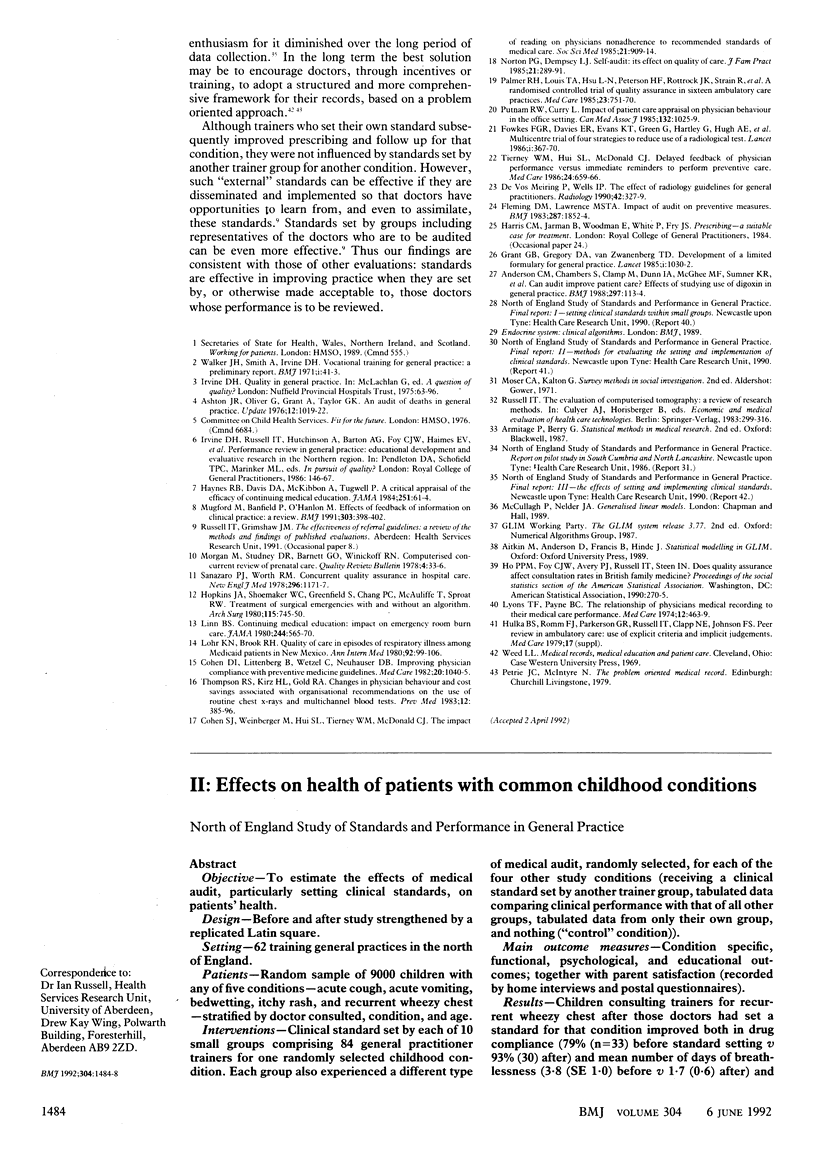
OBJECTIVE--To estimate the effects of medical audit, particularly setting clinical standards, on general practitioners' clinical behaviour. DESIGN--Before and after study strengthened by a replicated Latin square. SETTING--62 training general practices in the north of England. SUBJECTS--92 general practitioner trainers, 84 (91%) of whom completed the study; random sample of 3500 children consulting one of these trainers for any of five conditions--acute cough, acute vomiting, bedwetting, itchy rash, and recurrent wheezy chest--stratified by doctor consulted, condition, and age. INTERVENTIONS--Clinical standard set by each of 10 small groups of general practitioner trainers for one randomly selected childhood condition. Each group also experienced a different type of medical audit, randomly selected, for each of the four other study conditions (receiving a clinical standard set by another trainer group, tabulated data comparing clinical performance with that of all other groups, tabulated data from only their own group, and nothing ("control" condition)). MAIN MEASURES--Content of initial consultation divided into: history, examination, investigation, diagnosis, and management (abstracted from medical records and "enhancement forms" completed by doctors). RESULTS--There was increased prescribing of bronchodilators for acute cough, oral rehydration fluids for acute vomiting, antibiotics for itchy rash, and bronchodilators and oral steroids for recurrent wheezy chest and reduced prescribing of antibiotics for acute cough and recurrent wheezy chest and tricyclic antidepressants for bedwetting. Fewer children were "discharged." Each change was consistent with the standard and either limited to doctors who set a standard for that condition or significantly greater for them than all other doctors. CONCLUSION--Setting clinical standards improved prescribing and follow up.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson C. M., Chambers S., Clamp M., Dunn I. A., McGhee M. F., Sumner K. R., Wood A. M. Can audit improve patient care? Effects of studying use of digoxin in general practice. BMJ. 1988 Jul 9;297(6641):113–114. doi: 10.1136/bmj.297.6641.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D. I., Littenberg B., Wetzel C., Neuhauser D. Improving physician compliance with preventive medicine guidelines. Med Care. 1982 Oct;20(10):1040–1045. doi: 10.1097/00005650-198210000-00006. [DOI] [PubMed] [Google Scholar]
- Cohen S. J., Weinberger M., Hui S. L., Tierney W. M., McDonald C. J. The impact of reading on physicians' nonadherence to recommended standards of medical care. Soc Sci Med. 1985;21(8):909–914. doi: 10.1016/0277-9536(85)90147-9. [DOI] [PubMed] [Google Scholar]
- Fleming D. M., Lawrence M. S. Impact of audit on preventive measures. Br Med J (Clin Res Ed) 1983 Dec 17;287(6408):1852–1854. doi: 10.1136/bmj.287.6408.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowkes F. G., Davies E. R., Evans K. T., Green G., Hartley G., Hugh A. E., Nolan D. J., Power A. L., Roberts C. J., Roylance J. Multicentre trial of four strategies to reduce use of a radiological test. Lancet. 1986 Feb 15;1(8477):367–370. doi: 10.1016/s0140-6736(86)92327-5. [DOI] [PubMed] [Google Scholar]
- Grant G. B., Gregory D. A., van Zwanenberg T. D. Development of a limited formulary for general practice. Lancet. 1985 May 4;1(8436):1030–1032. doi: 10.1016/s0140-6736(85)91625-3. [DOI] [PubMed] [Google Scholar]
- Haynes R. B., Davis D. A., McKibbon A., Tugwell P. A critical appraisal of the efficacy of continuing medical education. JAMA. 1984 Jan 6;251(1):61–64. [PubMed] [Google Scholar]
- Hopkins J. A., Shoemaker W. C., Greenfield S., Chang P. C., McAuliffe T., Sproat R. W. Treatment of surgical emergencies with and without an algorithm. Arch Surg. 1980 Jun;115(6):745–750. doi: 10.1001/archsurg.1980.01380060043011. [DOI] [PubMed] [Google Scholar]
- Linn B. S. Continuing medical education. Impact on emergency room burn care. JAMA. 1980 Aug 8;244(6):565–570. doi: 10.1001/jama.244.6.565. [DOI] [PubMed] [Google Scholar]
- Lohr K. N., Brook R. H. Quality of care in episodes of respiratory illness among Medicaid patients in New Mexico. Ann Intern Med. 1980 Jan;92(1):99–106. doi: 10.7326/0003-4819-92-1-99. [DOI] [PubMed] [Google Scholar]
- Lyons T. F., Payne B. C. The relationship of physicians' medical recording performance to their medical care performance. Med Care. 1974 May;12(5):463–469. doi: 10.1097/00005650-197405000-00008. [DOI] [PubMed] [Google Scholar]
- Mugford M., Banfield P., O'Hanlon M. Effects of feedback of information on clinical practice: a review. BMJ. 1991 Aug 17;303(6799):398–402. doi: 10.1136/bmj.303.6799.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton P. G., Dempsey L. J. Self-audit: its effect on quality of care. J Fam Pract. 1985 Oct;21(4):289–291. [PubMed] [Google Scholar]
- Palmer R. H., Louis T. A., Hsu L. N., Peterson H. F., Rothrock J. K., Strain R., Thompson M. S., Wright E. A. A randomized controlled trial of quality assurance in sixteen ambulatory care practices. Med Care. 1985 Jun;23(6):751–770. doi: 10.1097/00005650-198506000-00001. [DOI] [PubMed] [Google Scholar]
- Putnam R. W., Curry L. Impact of patient care appraisal on physician behaviour in the office setting. Can Med Assoc J. 1985 May 1;132(9):1025–1029. [PMC free article] [PubMed] [Google Scholar]
- Sanazaro P. J., Worth R. M. Concurrent quality assurance in hospital care. Report of a study by Private Initiative in PSRO. N Engl J Med. 1978 May 25;298(21):1171–1177. doi: 10.1056/NEJM197805252982104. [DOI] [PubMed] [Google Scholar]
- Thompson R. S., Kirz H. L., Gold R. A. Changes in physician behavior and cost savings associated with organizational recommendations on the use of "routine" chest X rays and multichannel blood tests. Prev Med. 1983 May;12(3):385–396. doi: 10.1016/0091-7435(83)90247-5. [DOI] [PubMed] [Google Scholar]
- Tierney W. M., Hui S. L., McDonald C. J. Delayed feedback of physician performance versus immediate reminders to perform preventive care. Effects on physician compliance. Med Care. 1986 Aug;24(8):659–666. doi: 10.1097/00005650-198608000-00001. [DOI] [PubMed] [Google Scholar]
- Walker J. H., Smith A., Irvine D. Vocational training for general practice: a preliminary report. Br Med J. 1971 Jan 2;1(5739):41–43. doi: 10.1136/bmj.1.5739.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de vos Meiring P., Wells I. P. The effect of radiology guidelines for general practitioners in Plymouth. Clin Radiol. 1990 Nov;42(5):327–329. doi: 10.1016/s0009-9260(05)82146-4. [DOI] [PubMed] [Google Scholar]


