Abstract
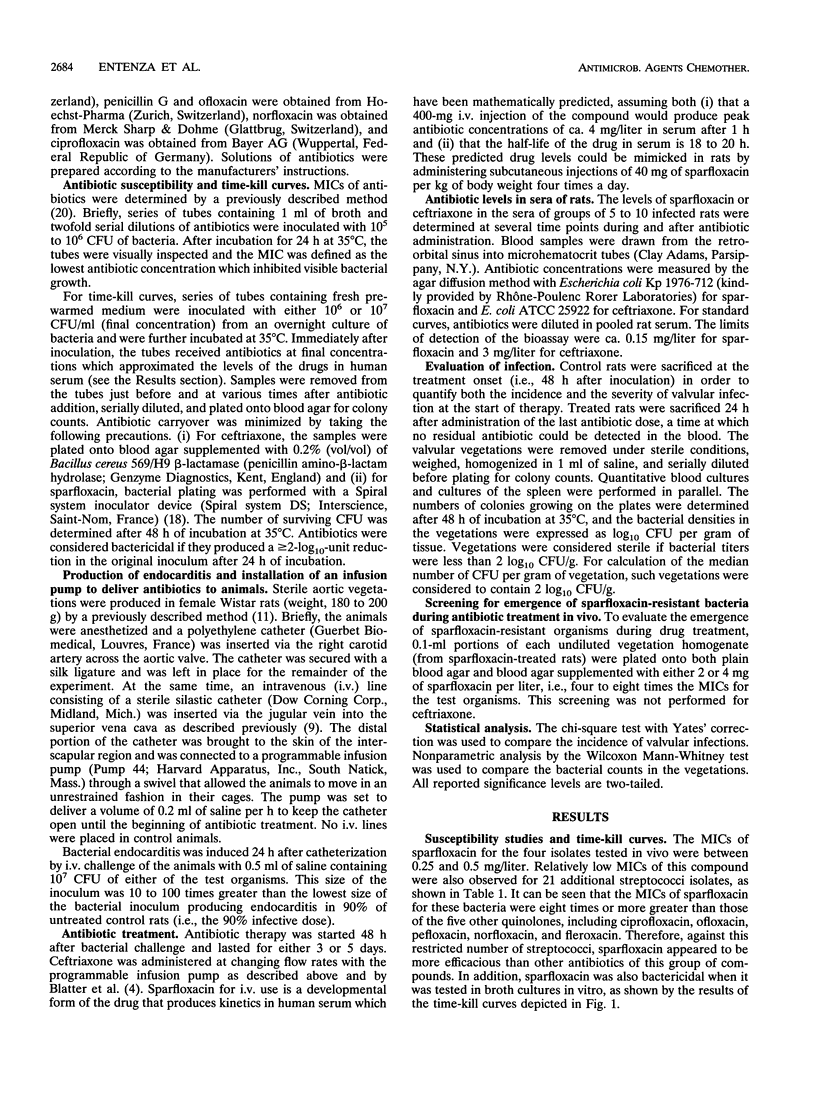
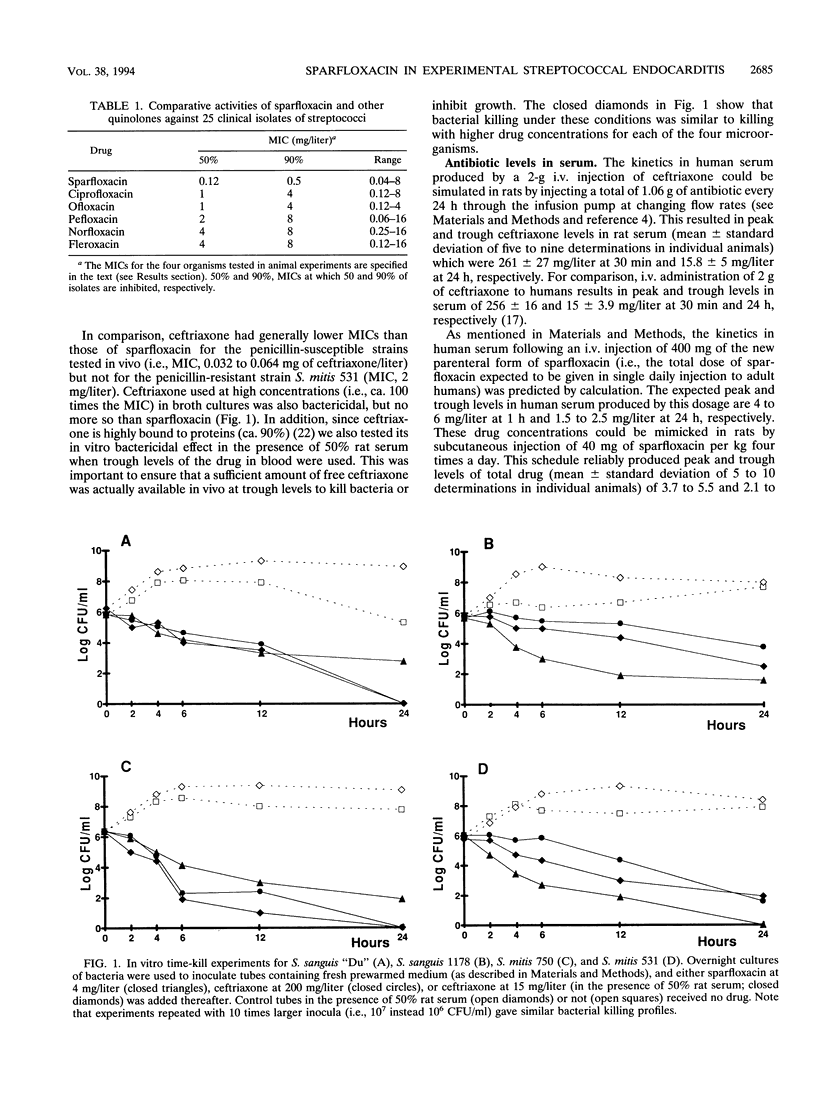
A new, investigational, parenteral form of sparfloxacin was compared with ceftriaxone in the treatment of experimental endocarditis caused by either of three penicillin-susceptible streptococci or one penicillin-resistant streptococcus. Both drugs have prolonged half-lives in serum, allowing single daily administration to humans. Sparfloxacin had relatively low MICs (0.25 to 0.5 mg/liter) for all four organisms and was also greater than or equal to eight times more effective than the other quinolones against 21 additional streptococcal isolates recovered from patients with bacteremia. Ceftriaxone MICs were 0.032 to 0.064 mg/liter for the penicillin-susceptible strains and 2 mg/liter for the resistant isolate. Both antibiotics resulted in moderate bacterial killing in vitro. Rats with catheter-induced aortic vegetations were inoculated with 10(7) CFU of the test organisms. Antibiotic treatment was started 48 h later and lasted either 3 or 5 days. The drugs were injected at doses which mimicked the kinetics in human serum produced by one intravenous injection of 400 mg of sparfloxacin (i.e., the daily dose expected to be given to human adults) and 2 g of ceftriaxone. Both antibiotics significantly decreased the bacterial densities in the vegetations. However, sparfloxacin was slower than ceftriaxone in its ability to eradicate valvular infection caused by penicillin-susceptible bacteria. While this difference was quite marked after 3 days of therapy, it tended to vanish when treatment was prolonged to 5 days. In contrast, sparfloxacin was very effective against the penicillin-resistant isolate, an organism against which ceftriaxone therapy failed in vivo. No sparfloxacin-resistant mutant was selected during therapy. Thus, in the present experimental setting, this new, investigational, parenteral form of sparfloxacin was effective against severe infections caused by both penicillin-susceptible and penicillin-resistant streptococci.
Full text
PDF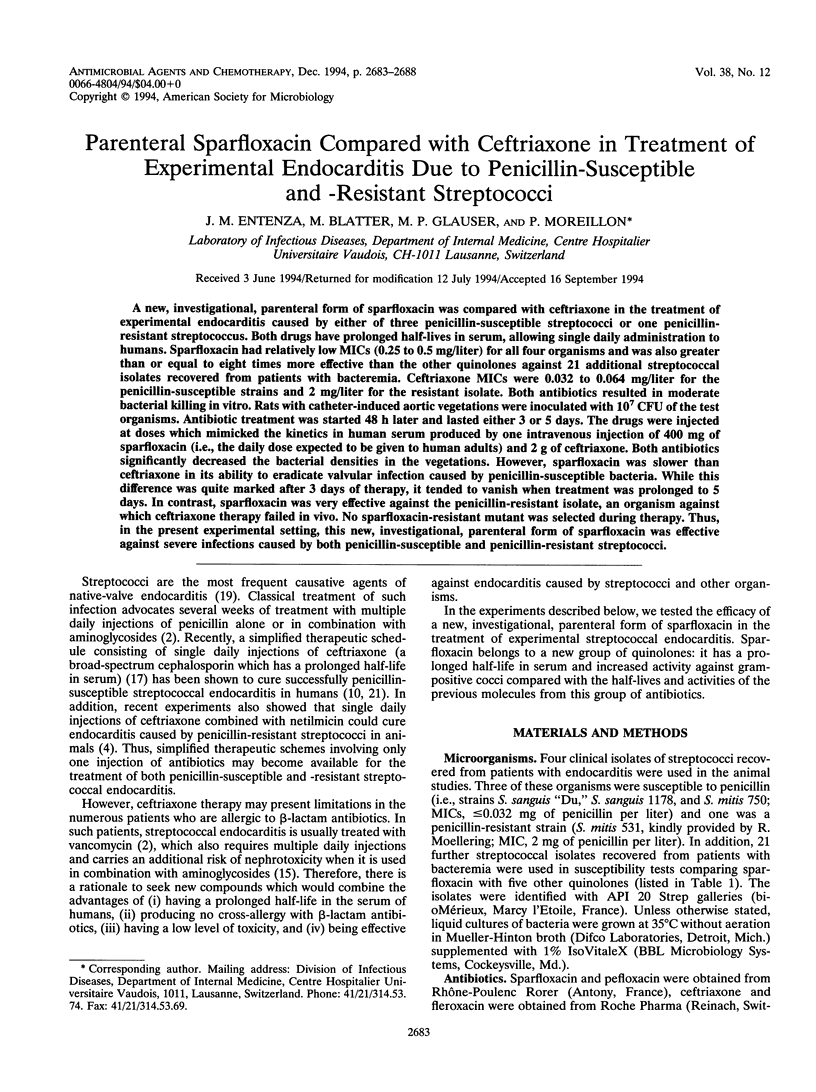


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berney P., Francioli P. Successful prophylaxis of experimental streptococcal endocarditis with single-dose amoxicillin administered after bacterial challenge. J Infect Dis. 1990 Feb;161(2):281–285. doi: 10.1093/infdis/161.2.281. [DOI] [PubMed] [Google Scholar]
- Bisno A. L., Dismukes W. E., Durack D. T., Kaplan E. L., Karchmer A. W., Kaye D., Rahimtoola S. H., Sande M. A., Sanford J. P., Watanakunakorn C. Antimicrobial treatment of infective endocarditis due to viridans streptococci, enterococci, and staphylococci. JAMA. 1989 Mar 10;261(10):1471–1477. [PubMed] [Google Scholar]
- Blatter M., Fluckiger U., Entenza J., Glauser M. P., Francioli P. Simulated human serum profiles of one daily dose of ceftriaxone plus netilmicin in treatment of experimental streptococcal endocarditis. Antimicrob Agents Chemother. 1993 Sep;37(9):1971–1976. doi: 10.1128/aac.37.9.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantón E., Pemán J., Jimenez M. T., Ramón M. S., Gobernado M. In vitro activity of sparfloxacin compared with those of five other quinolones. Antimicrob Agents Chemother. 1992 Mar;36(3):558–565. doi: 10.1128/aac.36.3.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crémieux A. C., Mazière B., Vallois J. M., Ottaviani M., Bouvet A., Pocidalo J. J., Carbon C. Ceftriaxone diffusion into cardiac fibrin vegetation. Qualitative and quantitative evaluation by autoradiography. Fundam Clin Pharmacol. 1991;5(1):53–60. doi: 10.1111/j.1472-8206.1991.tb00701.x. [DOI] [PubMed] [Google Scholar]
- Durack D. T., Beeson P. B. Experimental bacterial endocarditis. I. Colonization of a sterile vegetation. Br J Exp Pathol. 1972 Feb;53(1):44–49. [PMC free article] [PubMed] [Google Scholar]
- Fluckiger U., Francioli P., Blaser J., Glauser M. P., Moreillon P. Role of amoxicillin serum levels for successful prophylaxis of experimental endocarditis due to tolerant streptococci. J Infect Dis. 1994 Jun;169(6):1397–1400. doi: 10.1093/infdis/169.6.1397. [DOI] [PubMed] [Google Scholar]
- Francioli P., Etienne J., Hoigné R., Thys J. P., Gerber A. Treatment of streptococcal endocarditis with a single daily dose of ceftriaxone sodium for 4 weeks. Efficacy and outpatient treatment feasibility. JAMA. 1992 Jan 8;267(2):264–267. [PubMed] [Google Scholar]
- Héraïef E., Glauser M. P., Freedman L. R. Natural history of aortic valve endocarditis in rats. Infect Immun. 1982 Jul;37(1):127–131. doi: 10.1128/iai.37.1.127-131.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joly V., Bergeron Y., Bergeron M. G., Carbon C. Endotoxin-tobramycin additive toxicity on renal proximal tubular cells in culture. Antimicrob Agents Chemother. 1991 Feb;35(2):351–357. doi: 10.1128/aac.35.2.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joly V., Pangon B., Vallois J. M., Abel L., Brion N., Bure A., Chau N. P., Contrepois A., Carbon C. Value of antibiotic levels in serum and cardiac vegetations for predicting antibacterial effect of ceftriaxone in experimental Escherichia coli endocarditis. Antimicrob Agents Chemother. 1987 Oct;31(10):1632–1639. doi: 10.1128/aac.31.10.1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura S., Kurobe N., Ohue T., Hashimoto M., Shimizu M. Pharmacokinetics of a novel quinolone, AT-4140, in animals. Antimicrob Agents Chemother. 1990 Jan;34(1):89–93. doi: 10.1128/aac.34.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura S., Minami A., Nakata K., Kurobe N., Kouno K., Sakaguchi Y., Kashimoto S., Yoshida H., Kojima T., Ohue T. In vitro and in vivo antibacterial activities of AT-4140, a new broad-spectrum quinolone. Antimicrob Agents Chemother. 1989 Aug;33(8):1167–1173. doi: 10.1128/aac.33.8.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odio C., McCracken G. H., Jr, Nelson J. D. Nephrotoxicity associated with vancomycin-aminoglycoside therapy in four children. J Pediatr. 1984 Sep;105(3):491–493. doi: 10.1016/s0022-3476(84)80036-0. [DOI] [PubMed] [Google Scholar]
- Pangon B., Joly V., Vallois J. M., Abel L., Buré A., Brion N., Contrepois A., Carbon C. Comparative efficacy of cefotiam, cefmenoxime, and ceftriaxone in experimental endocarditis and correlation with pharmacokinetics and in vitro efficacy. Antimicrob Agents Chemother. 1987 Apr;31(4):518–522. doi: 10.1128/aac.31.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel I. H., Chen S., Parsonnet M., Hackman M. R., Brooks M. A., Konikoff J., Kaplan S. A. Pharmacokinetics of ceftriaxone in humans. Antimicrob Agents Chemother. 1981 Nov;20(5):634–641. doi: 10.1128/aac.20.5.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perronne C. M., Malinverni R., Glauser M. P. Treatment of Staphylococcus aureus endocarditis in rats with coumermycin A1 and ciprofloxacin, alone or in combination. Antimicrob Agents Chemother. 1987 Apr;31(4):539–543. doi: 10.1128/aac.31.4.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamboulian D., Bonvehi P., Arevalo C., Bologna R., Cassetti I., Scilingo V., Efron E. Antibiotic management of outpatients with endocarditis due to penicillin-susceptible streptococci. Rev Infect Dis. 1991 Jan-Feb;13 (Suppl 2):S160–S163. doi: 10.1093/clinids/13.supplement_2.s160. [DOI] [PubMed] [Google Scholar]
- Stoeckel K., McNamara P. J., Brandt R., Plozza-Nottebrock H., Ziegler W. H. Effects of concentration-dependent plasma protein binding on ceftriaxone kinetics. Clin Pharmacol Ther. 1981 May;29(5):650–657. doi: 10.1038/clpt.1981.90. [DOI] [PubMed] [Google Scholar]
- Vazquez J., Perri M. B., Thal L. A., Donabedian S. A., Zervos M. J. Sparfloxacin and clinafloxacin alone or in combination with gentamicin for therapy of experimental ampicillin-resistant enterococcal endocarditis in rabbits. J Antimicrob Chemother. 1993 Nov;32(5):715–721. doi: 10.1093/jac/32.5.715. [DOI] [PubMed] [Google Scholar]
- Visser M. R., Rozenberg-Arska M., Beumer H., Hoepelman I. M., Verhoef J. Comparative in vitro antibacterial activity of sparfloxacin (AT-4140; RP 64206), a new quinolone. Antimicrob Agents Chemother. 1991 May;35(5):858–868. doi: 10.1128/aac.35.5.858. [DOI] [PMC free article] [PubMed] [Google Scholar]


