Abstract
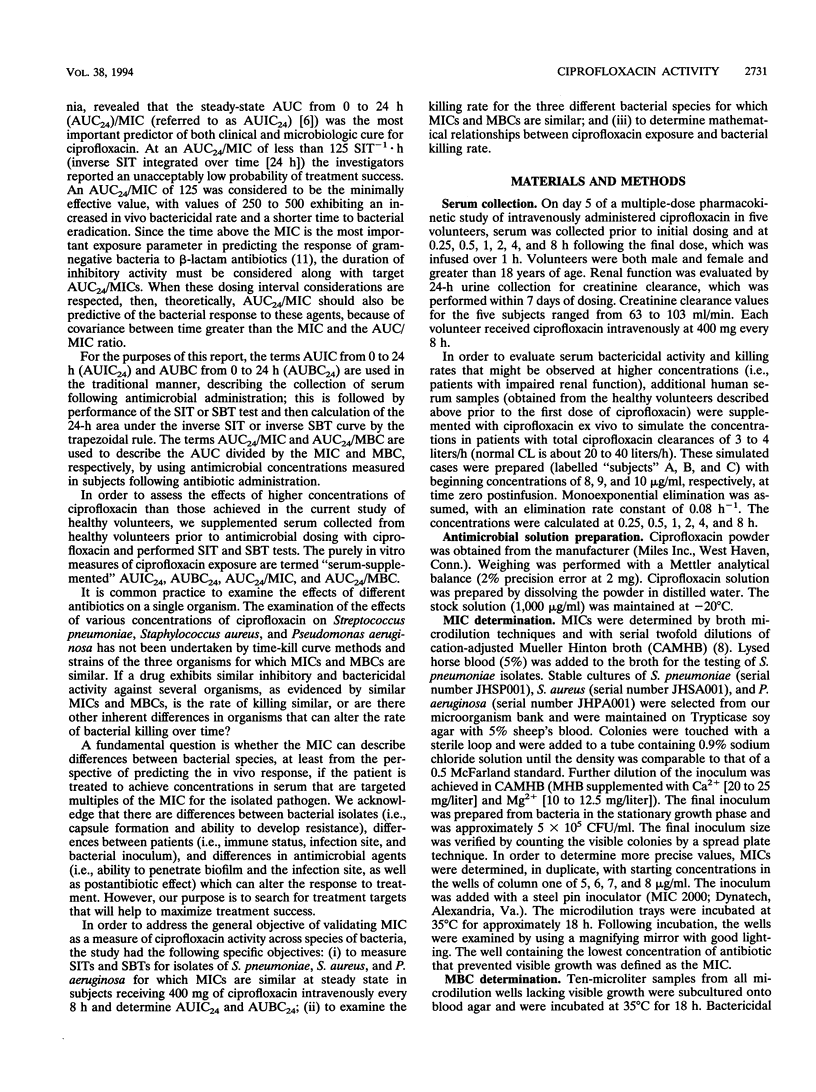
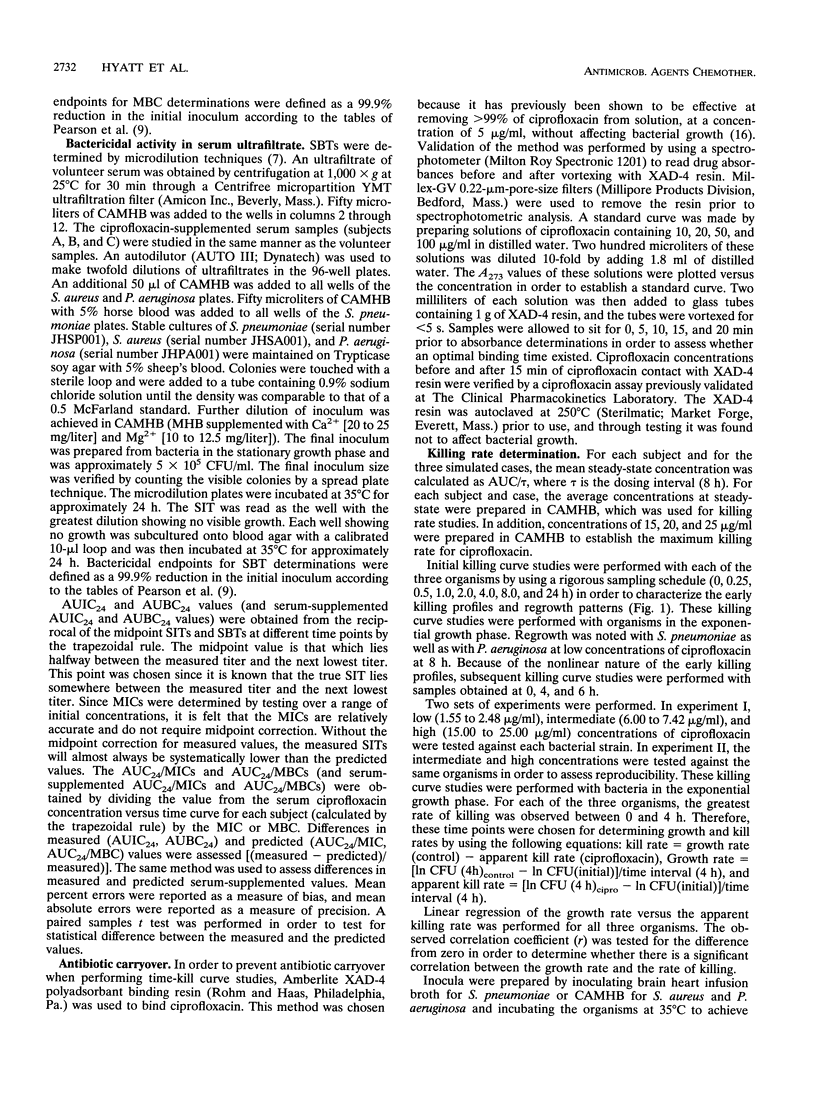
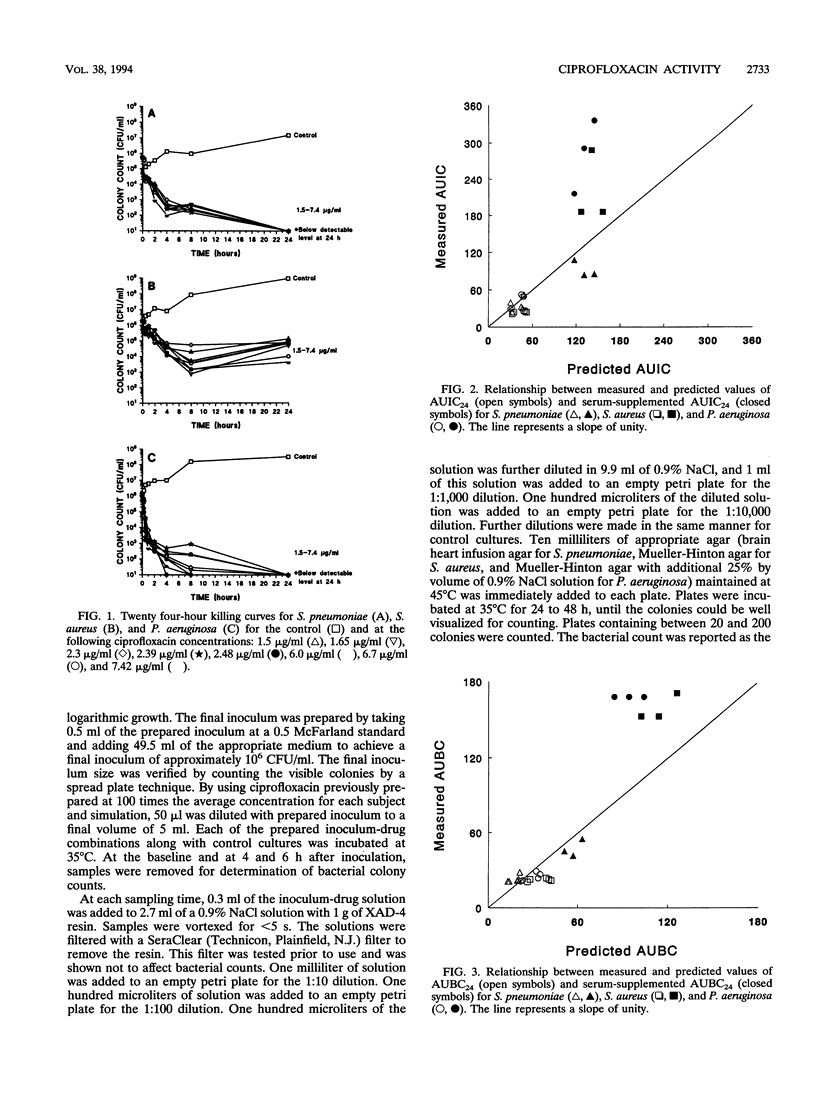
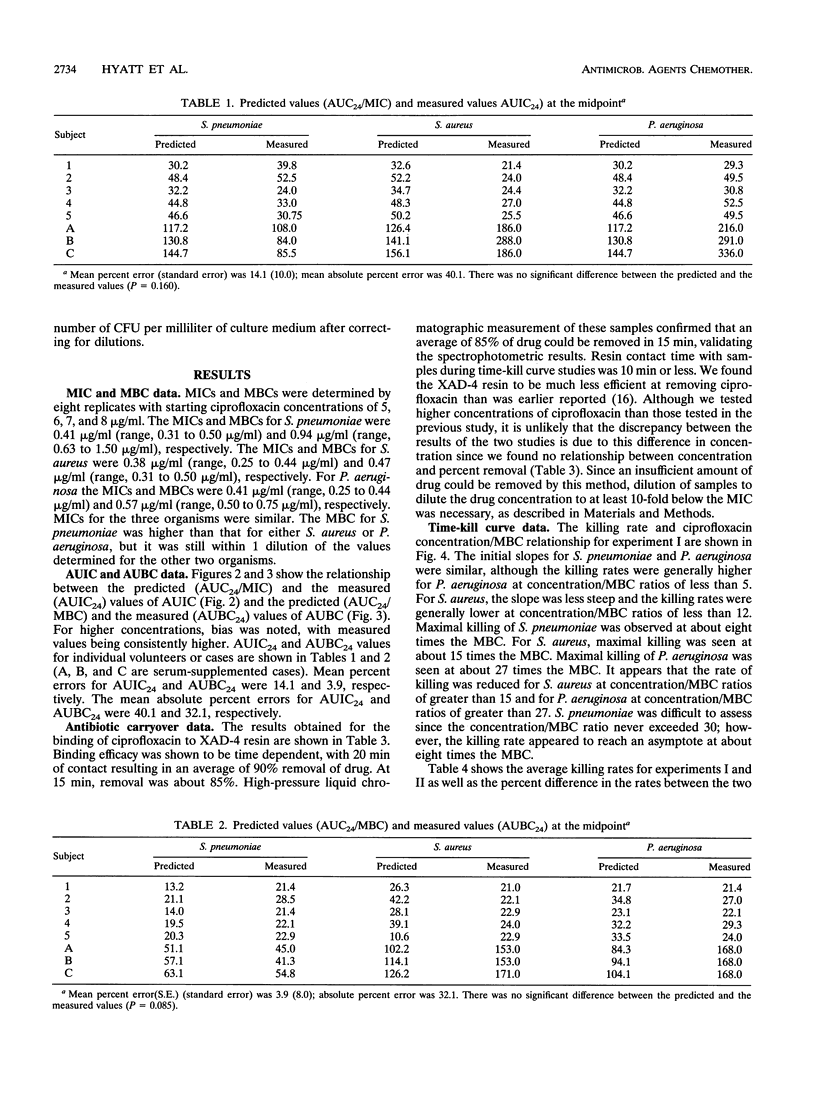
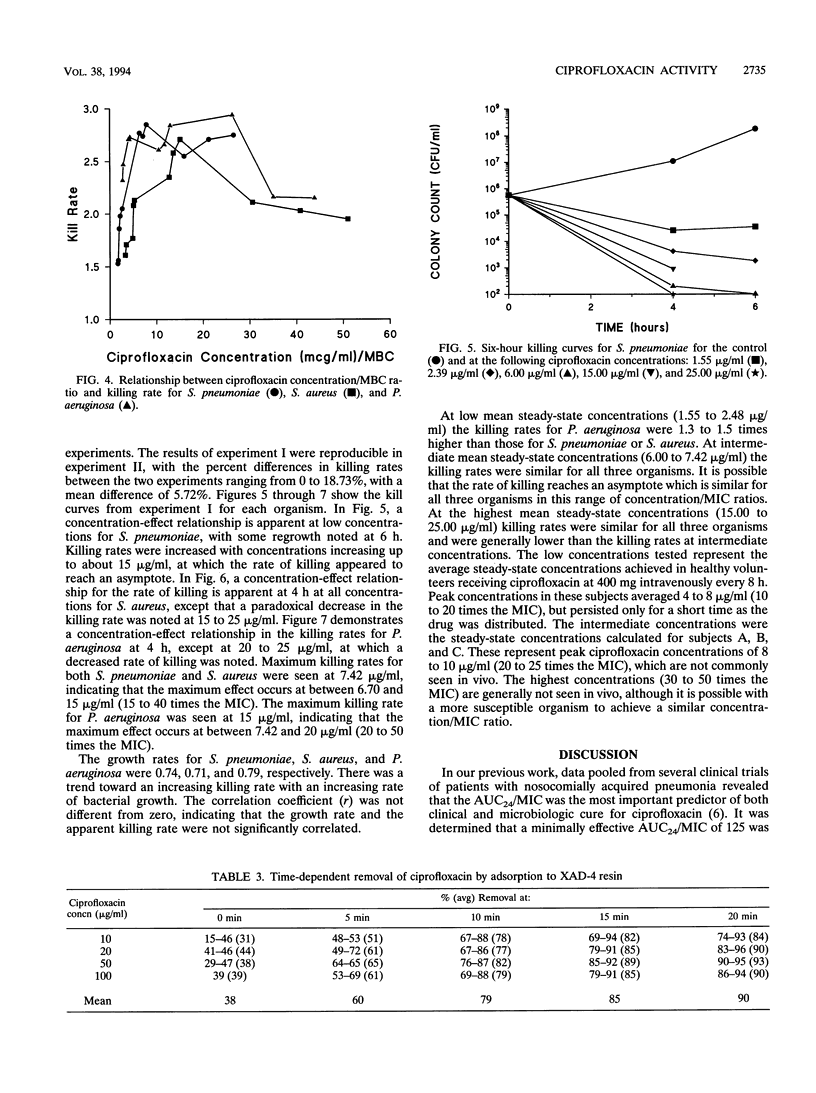
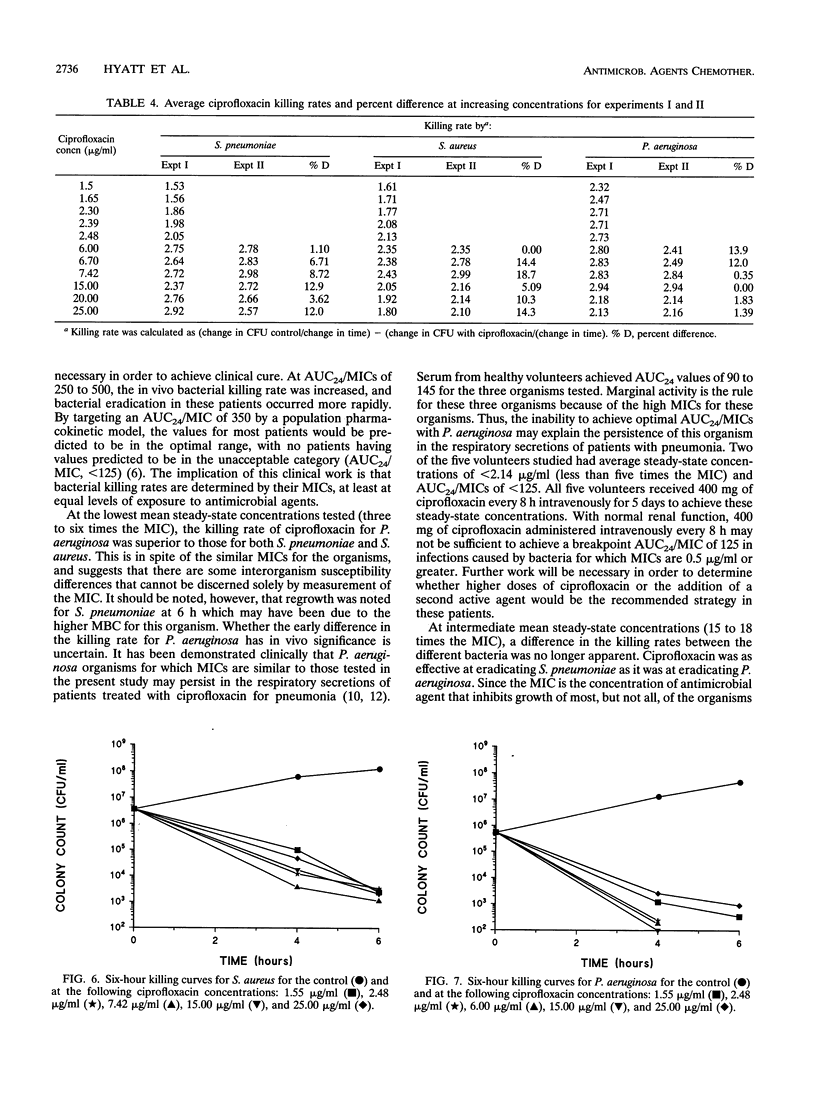
The serum bactericidal activity of ciprofloxacin against strains of Streptococcus pneumoniae, Staphylococcus aureus, and Pseudomonas aeruginosa for which MICs are similar (0.4 microgram/ml) was assessed with serum ultrafiltrates from five healthy volunteers receiving ciprofloxacin at 400 mg intravenously every 8 h. In addition, human serum was supplemented with ciprofloxacin to achieve a mean steady-state concentration (Css) that might be achieved in patients with renal failure, with total clearances of 3 to 4 liters/h (elimination rate constant, 0.08 h-1). The area under the inhibitory titer curve from 0 to 24 h (AUIC24) and the area under the bactericidal titer curve from 0 to 24 h (AUBC24) were both measured and predicted as the area under the concentration-time curve from 0 to 24 h (AUC24)/MIC and AUC24/MBC, respectively. We previously demonstrated that a breakpoint AUC24/MIC of 125 for ciprofloxacin had a significantly higher probability of treatment success than lower values, with 250 to 500 being optimal. Volunteer sera (mean Css, 1.55 to 2.48 micrograms/ml) achieved AUC24/MICs of 90 to 145. Supplemented serum (mean Css, 6.00 to 7.42 micrograms/ml) achieved AUC24/MICs of 350 to 450. Correlation coefficients for measured and predicted values of AUC24/MIC and AUC24/MBC were 0.826 and 0.941, respectively. The mean percent errors were not significantly different from zero for either AUIC24 or AUBC24 values (P > 0.1, P > 0.4). Time-kill curve studies were performed with low (1.55 to 2.48 micrograms/ml), intermediate (6.00 to 7.42 micrograms/ml), and high (15 to 25 micrograms/ml) concentrations of ciprofloxacin for the three organisms. At low concentrations (3 to 6 times the MIC) AUC24/MICs were <125 for two of five volunteers and the killing rates were considerably more rapid for P. aeruginosa than for S. pneumoniae or S.aureus. Intermediate concentrations (15 to 18 times the MIC) achieved optimal AUC24/MICs, and the killing rates were similar for the three organisms. A paradoxical decrease in the killing rate was seen at high concentrations (35 to 60 times the MIC). At clinically achievable concentrations, ciprofloxacin killed P. aeruginosa more rapidly than it did either S. pneumoniae or S. aureus.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barriere S. L., Ely E., Kapusnik J. E., Gambertoglio J. G. Analysis of a new method for assessing activity of combinations of antimicrobials: area under the bactericidal activity curve. J Antimicrob Chemother. 1985 Jul;16(1):49–59. doi: 10.1093/jac/16.1.49. [DOI] [PubMed] [Google Scholar]
- Drusano G. L., Johnson D. E., Rosen M., Standiford H. C. Pharmacodynamics of a fluoroquinolone antimicrobial agent in a neutropenic rat model of Pseudomonas sepsis. Antimicrob Agents Chemother. 1993 Mar;37(3):483–490. doi: 10.1128/aac.37.3.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drusano G., Standiford H., Ryan P., McNamee W., Tatem B., Schimpff S. Correlation of predicted serum bactericidal activities and values measured in volunteers. Eur J Clin Microbiol. 1986 Feb;5(1):88–92. doi: 10.1007/BF02013475. [DOI] [PubMed] [Google Scholar]
- Ellner P. D., Neu H. C. The inhibitory quotient. A method for interpreting minimum inhibitory concentration data. JAMA. 1981 Oct 2;246(14):1575–1578. doi: 10.1001/jama.246.14.1575. [DOI] [PubMed] [Google Scholar]
- Forrest A., Nix D. E., Ballow C. H., Goss T. F., Birmingham M. C., Schentag J. J. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother. 1993 May;37(5):1073–1081. doi: 10.1128/aac.37.5.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leggett J. E., Wolz S. A., Craig W. A. Use of serum ultrafiltrate in the serum dilution test. J Infect Dis. 1989 Oct;160(4):616–623. doi: 10.1093/infdis/160.4.616. [DOI] [PubMed] [Google Scholar]
- Pearson R. D., Steigbigel R. T., Davis H. T., Chapman S. W. Method of reliable determination of minimal lethal antibiotic concentrations. Antimicrob Agents Chemother. 1980 Nov;18(5):699–708. doi: 10.1128/aac.18.5.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peloquin C. A., Cumbo T. J., Nix D. E., Sands M. F., Schentag J. J. Evaluation of intravenous ciprofloxacin in patients with nosocomial lower respiratory tract infections. Impact of plasma concentrations, organism, minimum inhibitory concentration, and clinical condition on bacterial eradication. Arch Intern Med. 1989 Oct;149(10):2269–2273. [PubMed] [Google Scholar]
- Schentag J. J., Smith I. L., Swanson D. J., DeAngelis C., Fracasso J. E., Vari A., Vance J. W. Role for dual individualization with cefmenoxime. Am J Med. 1984 Dec 21;77(6A):43–50. doi: 10.1016/s0002-9343(84)80074-1. [DOI] [PubMed] [Google Scholar]
- Scully B. E., Neu H. C., Parry M. F., Mandell W. Oral ciprofloxacin therapy of infections due to Pseudomonas aeruginosa. Lancet. 1986 Apr 12;1(8485):819–822. doi: 10.1016/s0140-6736(86)90937-2. [DOI] [PubMed] [Google Scholar]
- Smith J. T. The mode of action of 4-quinolones and possible mechanisms of resistance. J Antimicrob Chemother. 1986 Nov;18 (Suppl 500):21–29. doi: 10.1093/jac/18.supplement_d.21. [DOI] [PubMed] [Google Scholar]
- Stratton C. W., Weinstein M. P., Reller L. B. Correlation of serum bactericidal activity with antimicrobial agent level and minimal bactericidal concentration. J Infect Dis. 1982 Feb;145(2):160–168. doi: 10.1093/infdis/145.2.160. [DOI] [PubMed] [Google Scholar]
- Zabinski R. A., Larsson A. J., Walker K. J., Gilliland S. S., Rotschafer J. C. Elimination of quinolone antibiotic carryover through use of antibiotic-removal beads. Antimicrob Agents Chemother. 1993 Jun;37(6):1377–1379. doi: 10.1128/aac.37.6.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]



