Abstract
Overdose of acetaminophen, a widely used analgesic drug, can result in severe hepatotoxicity and is often fatal. This toxic reaction is associated with metabolic activation by the P450 system to form a quinoneimine metabolite, N-acetyl-p-benzoquinoneimine (NAPQI), which covalently binds to proteins and other macromolecules to cause cellular damage. At low doses, NAPQI is efficiently detoxified, principally by conjugation with glutathione, a reaction catalyzed in part by the glutathione S-transferases (GST), such as GST Pi. To assess the role of GST in acetaminophen hepatotoxicity, we examined acetaminophen metabolism and liver damage in mice nulled for GstP (GstP1/P2(−/−)). Contrary to our expectations, instead of being more sensitive, GstP null mice were highly resistant to the hepatotoxic effects of this compound. No significant differences between wild-type (GstP1/P2(+/+)) mice and GstP1/P2(−/−) nulls in either the rate or route of metabolism, particularly to glutathione conjugates, or in the levels of covalent binding of acetaminophen-reactive metabolites to cellular protein were observed. However, although a similar rapid depletion of hepatic reduced glutathione (GSH) was found in both GstP1/P2(+/+) and GstP1/P2(−/−) mice, GSH levels only recovered in the GstP1/P2(−/−) mice. These data demonstrate that GstP does not contribute in vivo to the formation of glutathione conjugates of acetaminophen but plays a novel and unexpected role in the toxicity of this compound. This study identifies new ways in which GST can modulate cellular sensitivity to toxic effects and suggests that the level of GST Pi may be an important and contributing factor in the sensitivity of patients with acetaminophen-induced hepatotoxicity.
Acetaminophen is an extensively used analgesic drug worldwide and, although safe when used at therapeutic doses, is associated with significant morbidity and mortality when taken in overdose, particularly in individuals with preexisting liver disease (1, 2). Despite extensive studies, the precise mechanism of acetaminophen toxicity remains controversial (3). It is now established, however, that acetaminophen is metabolized in the first instance, after normal therapeutic doses, by phase II drug-metabolizing enzymes such as the glucuronyl and sulfotransferases (4, 5). Under these circumstances, only a portion of the acetaminophen dose is available to undergo bioactivation by the cytochrome P450 system (CYP2E1, CYP3A4, CYP1A2; refs. 6 and 7) to create a highly reactive intermediate, N-acetyl-p-benzoquinoneimine (NAPQI; refs. 8 and 9). This intermediate covalently binds to cellular macromolecules, causing damage and cell death (10, 11).
Following therapeutic doses, the low concentrations of NAPQI formed are readily detoxified by reaction with reduced glutathione (GSH), which occurs both nonenzymatically and in a reaction catalyzed by glutathione S-transferases (GST). Among GST, in vitro studies have shown that GST Pi is the most effective catalyst of the conjugation of NAPQI with glutathione in both rats and humans; this enzyme is relatively inefficient at catalyzing the reduction of NAPQI back to the parent compound, i.e., acetaminophen (12). However, under conditions of overdose, rapid GSH depletion and a significant elevation in the levels of NAPQI occur, resulting in oxidative stress, cell damage, and death (13).
In previous studies, we have reported the generation of mice nulled at the Gst Pi gene loci that exhibited increased sensitivity to carcinogen-induced tumorigenesis (14). In the current study, we have exploited this model to establish the role of GST Pi in vivo in acetaminophen toxicity.
Materials and Methods
Reagents.
Acetaminophen, the GP-transaminase kit, 3-(N-morpholino)propanesulfonic acid, and 5,5′-dithio-bis(2-nitrobenzoic acid) were obtained from Sigma (Poole, Dorset). 2-Vinylpyridine was obtained from Aldrich (Gillingham, Dorset). ring-14C-labeled acetaminophen (specific activity 30 mCi/mmol, radiochemical purity 99%) was purchased from Moravek Biochemicals (Brea, CA). 3H(G)-labeled acetaminophen (specific activity 1.9 Ci/mmol, radiochemical purity 99%) was purchased from New England Nuclear. Sodium pentobarbitone (Sagatal) was obtained from Rhone Merieux (Harlow, Middlesex). OptiSolv tissue solubilizer was purchased from Fisons (Loughborough, U.K.). Lumac LSC Aqualuma Plus scintillation mixture was obtained from Packard. The protein assay kit was obtained from Bio-Rad. All other reagents were of analytical grade and were supplied by BDH.
Animals.
All experiments were undertaken in accordance with criteria outlined in a license granted under the Animals (Scientific Procedures) Act 1986 and approved by the Animal Ethics Committees of the University of Liverpool, the University of Dundee, and the Imperial Cancer Research Fund. GstP1/P2 null [GstP1/P2(−/−)] and wild-type [GstP1/P2(+/+)] mouse lines, on a 129xMF1 background, were generated and maintained as previously reported (14).
Determination of Acetaminophen Hepatotoxicity.
Oral administration.
Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (n = 5) were given a single administration of acetaminophen by gavage as a suspension (15 mg/ml) in PBS at a dose of 250 mg/kg. Animals were killed at 24 or 48 h after dosing, and blood was collected by cardiac puncture into heparinized tubes for measurement of serum transaminase levels. Livers were removed, rinsed in ice-cold PBS, fixed in PBS-formalin, and embedded in paraffin for histological assessment of tissue damage. Samples were subsequently sectioned, stained with hematoxylin and eosin, and examined under a light microscope for cellular damage.
Intraperitoneal administration.
Acetaminophen was administered by a single i.p. injection to both male and female GstP1/P2(−/−) (200–350 mg/kg, n = 5–14 per dose) and GstP1/P2(+/+) (100–250 mg/kg, n = 5–14 per dose) mice in saline (6.7–23.3 ml/kg). After 5 h, animals were anesthetized with pentobarbital (Sagatal; 60 mg/kg, i.p.), and blood was collected via the subclavical artery for determination of serum transaminase levels using the GP-transaminase kit.
Determination of Plasma Acetaminophen Levels.
Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (30–40 g, n = 6) were administered a single i.p. injection of either 150 or 300 mg/kg acetaminophen in saline. Five hours following administration, the animals were anesthetized with pentobarbital (60 mg/kg, i.p.); blood was collected into heparinized tubes and the plasma collected and stored at −20°C until use. Plasma acetaminophen levels were determined by HPLC. The internal control metacetamol (0.5 μg in 200 μl of water) was added to aliquots of plasma (100 μl), and plasma proteins were precipitated with 70 μl each of saturated Ba(OH)2 and 40% ZnSO4. After vortexing (30 s) and centrifugation (10,000 × g, 5 min), 50 μl of the resulting supernatant was injected onto a 250 × 4.6 mm 5 μ Hypersil ODS2 column (Hypersil, Runcorn, Cheshire). Organic compounds were eluted [mobile phase methanol/ethyl acetate/0.05 M sodium acetate buffer, 7.9:0.1:92 (vol/vol)], at a flow rate of 1.5 ml min−1 and were detected by UV absorbance at 254 nm. The retention times of acetaminophen and metacetamol were 6.25 and 10 min, respectively. Peak area measurements were used for quantification and were compared with standard solutions of acetaminophen. Analysis was performed on four separate occasions.
Determination of Biliary and Urinary Metabolism of Acetaminophen.
Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (38–52 g, n = 3) were maintained under anesthesia with pentobarbital (70 mg/kg, i.p. in saline, 2.2 ml/kg). The external jugular veins and common bile ducts were cannulated with polyethylene tubing, and penises were ligated with cotton to prevent loss of urine from the bladder. A sample of pretreatment bile was collected as a control. 3H-Acetaminophen (4–7 μCi, 150 mg/kg in saline, 10 ml/kg) was administered i.v. as a bolus over 2 min. Bile was collected for 3 h postdosing into preweighed Eppendorf tubes. Pentobarbital was administered occasionally as required to maintain adequate anesthesia. After 3 h, the animals were killed by cervical dislocation, and urine was collected from the bladder by aspiration with a syringe. Duplicate 5-μl aliquots of bile and urine were analyzed immediately for radioactivity in 4 ml of Lumac LSC Aqualuma Plus scintillation mixture. Aliquots (20–100 μl) of bile and urine were eluted from an Ultracarb 5-μm C8 column (250 mm × 46 mm i.d.; Phenomenex, Macclesfield, Cheshire) at room temperature with gradients of methanol in aqueous acetic acid (1%, vol/vol) as follows: 5 to 15% over 15 min and 15 to 35% over 10 min. The flow rate was 0.9 ml min−1. The eluate was monitored at 254 nm and split thereafter by a tee-piece; the flow rate to the liquid chromatography–mass spectrometry interface was 40 ml min−1, and the remainder was directed to a Radiomatic Flo-One (model 250) radioactivity detector consuming Ultima Flo AP scintillant at 1.0 ml min−1. Positive-ion electrospray mass spectra were obtained with a Quattro II instrument (Micromass, Manchester, UK) fitted with the standard liquid chromatography–mass spectrometry interface. The major operating conditions were as follows: source temperature, 70°C; capillary voltage, 3.8 × 103 V; lens voltage, 0.35 × 103 V; cone voltage, 30 V. Spectra were acquired between m/z 100–1,050 at one scan per 5 s. Data were processed via MASSLYNX 2.0 software.
Determination of the Covalent Binding of Acetaminophen-Derived Material.
For the determination of covalent binding, male GstP1/P2(−/−) and GstP1/P2(+/+) mice (30–40 g, n = 4) were administered 14C-acetaminophen (10–15 μCi) by a single i.p. injection at a dose of 300 mg/kg in saline (20 ml/kg). After 1 or 5 h, animals were killed by cervical dislocation. Livers were removed immediately, rinsed in ice-cold saline, frozen in liquid nitrogen, and stored at −80°C until required. Liver (500 mg) was homogenized in 66.7 mM phosphate buffer (1.5 ml) using a glass-Teflon homogenizer, and the protein concentration was determined by the method of Lowry et al. (15). The homogenate was extracted three times with diethyl ether (5 ml) to remove nonconjugated, nonprotein-bound drug. Protein was precipitated from the remaining aqueous phase by acetone (5 ml), and the precipitated residues were washed twice with 100% methanol and twice with 70% (vol/vol) methanol to remove lipid-soluble radiolabeled material. Radioactivity in aliquots of each solvent extract was measured for mass balance analysis of acetaminophen-derived products and also to confirm total removal of unbound radioactivity. The remaining protein pellet was dissolved in sodium hydroxide (1 M, 2 ml) at 60°C for 24 h, and an aliquot was taken for protein determination (15). An aliquot (1 ml) of the remaining protein fraction was decolorized by the addition of hydrogen peroxide (100 μl) and neutralized with glacial acetic acid (25 μl); the samples were then left at 4°C overnight to minimize chemiluminescense. The covalently bound material (nmol/mg of tissue) was quantified by scintillation counting.
Determination of Hepatic Glutathione Levels.
Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (30–40 g, at least n = 4) were administered a single i.p. injection of 300 mg/kg acetaminophen in saline. At 30 min, 1 or 5 h following administration, animals were killed by cervical dislocation, and the livers were removed immediately, rinsed in saline, and frozen in liquid nitrogen. Livers were stored at −80°C until use. Hepatic reduced and oxidized glutathione levels were determined according to the method of Baker et al. (16). Experiments were performed in duplicate on four separate occasions.
Statistical Analysis.
All results are expressed as mean ± standard deviation. All values to be compared were assessed for non-normality using the Shapiro–Wilk test and for equivalence of variance between groups with the F test. Student's unpaired t test and the Mann–Whitney test were used where parametric and nonparametric analyses were indicated, respectively. All calculations were performed using the Arcus Quickstat 1.1 statistical software package (Research Solutions, Cambridge), and results were considered to be significant when P values were less than 0.05.
Results
Hepatotoxicity of Acetaminophen.
Unlike other species, in the mouse there are two GstP genes, GstP1 and GstP2. To study the role of GstP in acetaminophen hepatotoxicity, mice nulled at both gene loci were used (14).
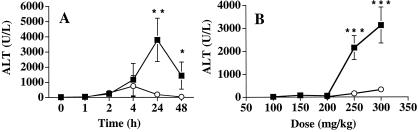
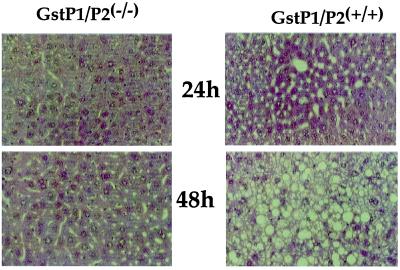
Male GstP1/P2(+/+) and GstP1/P2(−/−) mice treated with acetaminophen by gavage at a single dose of 250 mg/kg had alanine aminotransferase (ALT) levels that were significantly higher in wild-type mice at both 24 and 48 h after dosing (Fig. 1A). The degree of liver damage indicated by the elevated ALT levels was assessed by histochemical examination of liver tissues. Extensive cellular damage was observed in control mouse hepatocytes 24 h after treatment with acetaminophen. In hepatocytes from the null animals, no sign of hepatotoxicity could be seen (Fig. 2). The difference between wild-type and null mice was even more pronounced at 48 h; in control animals there was severe necrosis, with only very minor signs of damage in the GstP null mice.
Figure 1.
Plasma ALT levels in control and GstP null mice after treatment with acetaminophen. (A) Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (n = 5) were treated with a single dose of acetaminophen (250 mg/kg body weight) by gavage, and plasma ALT values were determined as detailed in Materials and Methods. ■, GstP1/P2(+/+); ○, GstP1/P2(−/−). **, P < 0.01; * P < 0.05. (B) Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (n = 5–10) were treated with a single i.p. dose of acetaminophen ranging from 100 to 350 mg/kg body weight, and plasma ALT values were determined as detailed in Materials and Methods. ■, GstP1/P2(+/+); ○, GstP1/P2(−/−). *, statistical difference between controls and nulls (***, P < 0.001).
Figure 2.
Liver histology in control mice compared with GstP null mice treated with a single oral dose of acetaminophen. Male GstP1/P2(−/−) and GstP1/P2(+/+) mice were treated with a single dose of acetaminophen 250 mg/kg body weight by gavage. At 24 and 48 h, the animals were killed and their livers removed, fixed, and sections (10 μm) cut and processed for staining with hematoxylin and eosin as detailed in Materials and Methods.
To establish whether the route of administration affected the differential drug sensitivity, acetaminophen was also administered intraperitoneally. Administration of acetaminophen (100–300 mg/kg) to control, GstP1/P2(+/+), male mice resulted in severe hepatotoxicity reflected in elevated serum ALT values (Fig. 1B). However, in male mice nulled at the GstP locus, ALT levels were virtually unchanged, even at 300 mg/kg. A significant difference in hepatotoxicity was also observed between female null and wild-type mice, with substantially higher doses of acetaminophen required to induce hepatotoxicity in female null mice relative to female wild-type animals (data not shown). These data indicate that the differential toxicity observed after oral administration was not due to differences in absorption across the gastrointestinal tract.
It is feasible that the profound difference in acetaminophen toxicity between GstP1/P2(+/+) and GstP1/P2(−/−) animals is due to a secondary effect on the levels of cytochrome P450s responsible for its activation to NAPQI. However, Western blot analysis using antibodies to P450s involved in acetaminophen activation, i.e., CYP1A2, CYP2E1, and CYP3A4, showed that there were no differences in the hepatic levels of these proteins between mice of either genotype (data not shown).
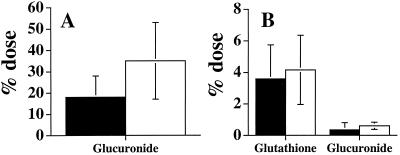
Acetaminophen Disposition.
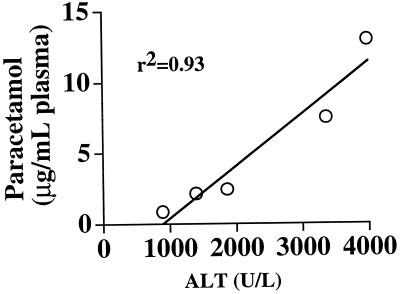
To study possible differences in drug pharmacokinetics, plasma levels of acetaminophen were determined at both a nontoxic (150 mg/kg) and hepatotoxic (300 mg/kg) dose. Five hours after administration of the lower dose, the concentrations of parent drug were identical (1.1 ± 0.5 and 1.1 ± 0.2 μg/ml plasma in wild-type and null mice, respectively). Interestingly, at the higher dose, wild-type mice had on average 5-fold higher levels than the null mice (P < 0.05). At this dose (300 mg/kg), the plasma acetaminophen concentrations in individual animals was directly correlated with the level of hepatotoxicity, i.e., ALT value (r2 = 0.93), indicating that the change in drug disposition of parent drug was a consequence of reduced metabolism due to hepatotoxicity rather than metabolic potential (Fig. 3). This was confirmed by measuring the levels of 3H-acetaminophen metabolites in the bile and urine. In urine, the only acetaminophen metabolite found was the glucuronide conjugate, and although there was some variability in level, no significant difference was evident between null and wild-type mice (Fig. 4A). In bile, both glutathione and glucuronide conjugates were detected, but again no differences were found between GstP1/P2(+/+) and GstP1/P2(−/−) mice (Fig. 4B).
Figure 3.
Correlation of plasma acetaminophen and alanine aminotransferase levels. Male GstP1/P2(+/+) mice (n = 5) were treated with acetaminophen (300 mg/kg, i.p.), and plasma acetaminophen and ALT values were determined 5 h after dosing as detailed in Materials and Methods. Data were subject to a Pearson rank correlation test.
Figure 4.
Metabolism of acetaminophen in control and GstP null mice. Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (n = 3) were treated with 3H-acetaminophen (4–7 μCi; 150 mg/kg in saline, 10 ml/kg), administered i.v. as a bolus over 2 min. Bile and urine were collected from these animals, and the level of acetaminophen metabolites was determined as detailed in Materials and Methods. Data are presented as a percentage of the radioactive dose excreted. (A) Urinary metabolites. (B) Biliary metabolites. Filled columns, GstP1/P2(+/+); open columns, GstP1/P2(−/−).
Covalent Binding of Acetaminophen-Derived Material.
The toxicity of acetaminophen has been directly associated with the covalent binding of NAPQI to cellular proteins (10). We therefore compared the level of binding in the livers of GstP1/P2(+/+) and GstP1/P2(−/−) mice after i.p. administration of 300 mg/kg acetaminophen. At 1 h after dosing, the levels of binding were very similar in wild-type and null mice (2.62 ± 0.43 and 2.40 ± 0.45 nmol/mg protein, respectively) and were comparable to those shown in earlier studies in other strains of mice (17). By 5 h, the levels had declined slightly in both mouse lines (1.90 ± 0.57 and 2.07 ± 0.46 nmol/mg protein for wild-type and null mice, respectively) but were still not statistically different.
These data, and those relating to acetaminophen metabolism (above), indicate that despite variability in glucuronide formation between GstP null and control mice, the amount of acetaminophen available for metabolic activation is essentially unchanged between the two lines.
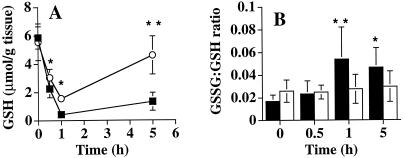
Glutathione Levels Following Acetaminophen Treatment.
A possible alternative mechanism of acetaminophen toxicity is by the induction of oxidative stress, which may occur as a consequence of depletion of reduced glutathione (18, 19). Resting levels of GSH were not significantly different between null and wild-type mice (Fig. 5A) (P = 0.81). Extensive glutathione depletion was observed in both null and wild-type animals following acetaminophen administration; however, GSH levels remained higher at all time points in null animals compared with wild-type mice (Fig. 5A). In the wild-type mice, however, GSH remained depleted throughout the remainder of the experiment, whereas in the GstP null animals it recovered to near pretreatment values by 5 h after injection. Oxidized glutathione, a marker of oxidative stress, accounted for only a small fraction of the total glutathione (5% or less), both before and after acetaminophen administration (Fig. 5B). In null mice, the ratio of oxidized to reduced glutathione remained relatively constant throughout the experiment, whereas in the wild-type animals there was a small but significant increase in the ratio at 1 and 5 h relative to the pretreatment ratio. However, at no time point was there a significant difference in the ratio between wild-type and null animals. These data are in line with previous studies that reported no major increases in biliary GSSG efflux following acetaminophen administration and suggest that oxidative stress, per se, is unlikely to be a significant factor in paracetamol-induced toxicity (20). In additional experiments, treatment with acetaminophen at 250 mg/kg did not change hepatic GSH levels in the GstP1/P2(−/−) mice in the following 24-h period; in contrast, the wild-type mice displayed a depletion similar to that in Fig. 5A (data not shown). The change in the rate of GSH regeneration could not be explained by the protein levels of the GSH biosynthetic enzymes γ-glutamylcysteine synthetase or glutathione synthase, which were essentially unchanged in both mouse lines following acetaminophen treatment, as determined by Western blotting (data not shown).
Figure 5.
Hepatic glutathione levels in control and GstP null mice following treatment with a single dose of acetaminophen. Male GstP1/P2(−/−) and GstP1/P2(+/+) mice (n = 6) were treated with acetaminophen i.p. at a dose of 300 mg/kg, and hepatic reduced and oxidized glutathione content was determined as detailed in Materials and Methods. (A) Reduced glutathione; ■, GstP1/P2(+/+); ○, GstP1/P2(−/−); *, statistical difference between controls and nulls (*, P < 0.05, **, P < 0.005). (B) Oxidized:reduced glutathione ratio (GSSG:GSH). Filled columns, GstP1/P2(+/+); open columns, GstP1/P2(−/−); *, statistical difference between pre- and post-acetaminophen treatment in control animals (*, P < 0.01; **, P < 0.005).
Discussion
Definitive knowledge of the causes of cell damage and death induced by acetaminophen, and how the hepatocyte responds to extreme chemical stress, particularly with respect to the intermediate and late events, could prove invaluable in devising novel strategies for therapeutic intervention under the circumstances of overdose (21). The current antidote of choice in acetaminophen overdose is i.v. N-acetylcysteine; however, the effects of this treatment are extremely limited if it is given more than 16 h after overdose. Furthermore, N-acetylcysteine is associated with a number of adverse reactions (22).
In this study, we have demonstrated that the presence of GstP has a profound effect on the sensitivity of mice to acetaminophen hepatotoxicity, and we have investigated a number of pathways considered important in its etiology. However, of these, no difference in the rate of acetaminophen detoxification, or metabolism to electrophilic products that covalently bind to cellular macromolecules, or in the formation of glutathione conjugates, could be found. This demonstrates conclusively that GstP does not catalyze the formation of acetaminophen–glutathione conjugates leading to detoxification in vivo. An increased level of circulating acetaminophen in control animals was observed at higher doses, but this was directly attributable to the level of hepatotoxicity, which subsequently impairs metabolism. At lower acetaminophen doses, no such difference was observed.
It is therefore necessary to rationalize mechanistically the finding that Gst Pi potentiates rather than protects against acetaminophen toxicity. The almost identical levels of protein arylation in the wild-type and null mice indicate that Gst Pi must exert its effect subsequent to the bioactivation and direct protein-damaging events that occur within the first hour following acetaminophen administration. As an alternative to inducing cellular damage by covalent binding, there is evidence that acetaminophen causes cellular damage through the induction of oxidative stress, a consequence of depletion of reduced glutathione (18, 19). The rapid regeneration of GSH in the nulls vs. control animals following acetaminophen treatment suggests either that there is a higher level of oxidative stress in the liver of wild-type mice or that the wild-type mice have a lower capacity to defend against such oxidative stress. The role of oxidative stress in the mechanism of acetaminophen toxicity has been intimated by the studies of Mirochnitchenko et al. (23). These authors showed that transgenic mice overexpressing either Cu-Zn-superoxide dismutase or the extracellular form of glutathione peroxidase exhibited an increased resistance to acetaminophen hepatotoxicity, whereas transgenic mice overexpressing the intracellular form of glutathione peroxidase were significantly more sensitive, a finding that was explained by delayed hepatic GSH regeneration. It is interesting to note, however, that while the Mirochnitchenko study reported liver GSH levels in both transgenic and nontransgenic mice were approximately 30% of pretreatment values 5 h after acetaminophen treatment, in the current study at the corresponding time-point hepatic GSH levels in the Gst Pi null mice had already returned to pretreatment levels, whereas in wild-type mice liver GSH levels were only 25% of control values. It would therefore appear that the absence of Gst Pi in the null mice significantly enhances the ability of the liver to maintain GSH homeostasis in the face of oxidative stress. Because Cu-Zn-superoxide dismutase and extracellular glutathione peroxidase are enzymes involved in combating oxidative stress, the implication from these findings of Mirochnitchenko et al. (23) is that the superoxide anion may be involved in mediating acetaminophen toxicity, and another study (19) has reported elevated (>2-fold) levels of superoxide anion in mice after treatment with a high dose of acetaminophen. GstP could therefore either cause a higher level of oxidative stress in the hepatocytes by redox cycling or protect against cellular damage resulting from such oxidative stress.
The possibility that redox cycling can occur after paracetamol overdose has recently been strengthened by the demonstration that labile ipso adducts can be formed between NAPQI and protein or non-protein thiols (24). Such adducts with reduced glutathione are readily reversible, yielding parent compound and glutathione disulfide. It is not known whether glutathione transferases can mediate ipso addition; however, the finding raises the possibility that glutathione conjugation of acetaminophen may result in high levels of GSSG and that the Gst Pi null mice are protected because they form less ipso product. The precise role of oxidative stress in the etiology of paracetamol hepatotoxicity remains controversial. Smith and Jaeschke (20) observed small increases in intracellular glutathione disulfide after acetaminophen administration in mice but no increase in the biliary excretion of this oxidative product. In the current study, the ratio of oxidized to reduced glutathione was 5% or less at all time points, although there was a small but significant increase in the ratio at the later time points in the wild-type animals. GST Pi null mice showed no variation in the oxidized:reduced glutathione ratio throughout the course of the experiment; however, no significant difference between the two mouse lines was observed, suggesting that differences in oxidative stress, particularly at the early time points, are unlikely to account for the altered acetaminophen sensitivity. It thus seems more likely that the difference lies in a protective mechanism.
Several years ago we suggested that GST formed part of a general adaptive response against cellular stress (25, 26); Adler et al. have recently demonstrated a novel function for GST Pi as an inhibitor of the stress-inducible Jun N-terminal kinase (27). In the absence of GST Pi, the constitutive activation of Jun N-terminal kinase results in activation of the transcription factor c-Jun, which is known to be involved in the regulation of many genes concerned with both cytoprotection (i.e., cell survival) and apoptosis (28–30), and which contain AP-1 sites in their promoters. We and others have shown that acetaminophen induces AP-1 DNA binding activity, suggesting the pathway is important in protecting against cytotoxicity of this compound (31, 32). It is therefore conceivable that GST P potentiates acetaminophen toxicity through its inhibition of Jun N-terminal kinase.
Sensitivity to acetaminophen toxicity is subject to very marked variability, and it has been reported that relatively low doses can induce fatal hepatitis (5, 33–35). Although it is usually considered that GST Pi levels in human hepatocytes are low, we have little knowledge about the regulation of this gene in such cells, and it remains to be established whether those individuals who are sensitive to acetaminophen are so because they express GST Pi. We have previously shown that the promoter of the GST Pi gene contains an AP-1 site, which will result in regulation by a wide range of factors including growth factors and cellular stress (36). In this regard, it is interesting to note that individuals with liver disease such as cirrhosis, hepatitis, or hepatocellular carcinoma where GST Pi is expressed are highly sensitive to acetaminophen toxicity (1, 37, 38), which could be explained by the expression of GST Pi. Furthermore, the kidney contains significant levels of GST Pi, and it could play an important role in the pathway of renal damage, a secondary toxicity associated with acetaminophen (5). Initial studies indicate that GstP1/P2 null mice are also protected against the nephrotoxic effects of this compound (data not shown). Taken together, these data suggest that GstP inhibitors may protect against liver and renal damage induced by acetaminophen, an intriguing possibility that is currently under investigation.
The data presented in this study demonstrate an unexpected and novel role for GstP in chemical toxicity downstream of the initial cytotoxic event. The widespread expression of this protein in almost all normal and tumor cells indicates that it will be an important factor in cell sensitivity to many other chemicals whose toxicity impinges on these pathways, and we have preliminary evidence indicating that this is indeed the case.
Acknowledgments
We thank Dr. Dennis Koop for his generous gift of antiserum to CYP2E1. We also thank Dr. Lesley McLellan for advice on glutathione biosynthesis and antibodies to γ-glutamylcysteine synthetase and glutathione synthase. This work was funded by the Imperial Cancer Research Fund and the Wellcome Trust; B.K.P. is a Wellcome Principal Research Fellow.
Abbreviations
- ALT
alanine aminotransferase
- GST
glutathione S-transferase
- NAPQI
N-acetyl-p-benzoquinoneimine
- GSH
hepatic reduced glutathione
Footnotes
This paper was submitted directly (Track II) to the PNAS office.
Article published online before print: Proc. Natl. Acad. Sci. USA, 10.1073/pnas.220176997.
Article and publication date are at www.pnas.org/cgi/doi/10.1073/pnas.220176997
References
- 1.Villeneuve J P, Raymond G, Bruneau J, Colpron L, Pomier-Layrargues G. Gastroenterol Clin Biol. 1983;7:898–902. [PubMed] [Google Scholar]
- 2.Thomson J S, Prescott L F. Br Med J. 1966;5512:506–507. doi: 10.1136/bmj.2.5512.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vermeulen N P, Bessems J G, Van de Straat R. Drug Metab Rev. 1992;24:367–407. doi: 10.3109/03602539208996298. [DOI] [PubMed] [Google Scholar]
- 4.Anker A L, Smilkstein M J. Conc Controversies Toxicol. 1994;12:335–349. [PubMed] [Google Scholar]
- 5.Prescott L F. Paracetamol (Acetaminophen): A Critical Bibliographic Review. London: Taylor & Francis; 1996. [Google Scholar]
- 6.Patten C J, Thomas P E, Guy R L, Lee M, Gonzalez F J, Guengerich F P, Yang C S. Chem Res Toxicol. 1993;6:511–518. doi: 10.1021/tx00034a019. [DOI] [PubMed] [Google Scholar]
- 7.Raucy J L, Lasker J M, Lieber C S, Black M. Arch Biochem Biophys. 1989;271:270–283. doi: 10.1016/0003-9861(89)90278-6. [DOI] [PubMed] [Google Scholar]
- 8.Bergman K, Muller L, Teigen S W. Mutat Res. 1996;349:263–288. doi: 10.1016/0027-5107(95)00185-9. [DOI] [PubMed] [Google Scholar]
- 9.Dahlin D C, Miwa G T, Lu A Y, Nelson S D. Proc Natl Acad Sci USA. 1984;81:1327–1331. doi: 10.1073/pnas.81.5.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nelson S D. Drug Metab Rev. 1995;27:147–177. doi: 10.3109/03602539509029821. [DOI] [PubMed] [Google Scholar]
- 11.Rogers L K, Moorthy B, Smith C V. Chem Res Toxicol. 1997;10:470–476. doi: 10.1021/tx960159i. [DOI] [PubMed] [Google Scholar]
- 12.Coles B, Wilson I, Wardman P, Hinson J A, Nelson S D, Ketterer B. Arch Biochem Biophys. 1988;264:253–260. doi: 10.1016/0003-9861(88)90592-9. [DOI] [PubMed] [Google Scholar]
- 13.Miner D J, Kissinger P T. Biochem Pharmacol. 1979;28:3285–3290. doi: 10.1016/0006-2952(79)90123-0. [DOI] [PubMed] [Google Scholar]
- 14.Henderson C J, Smith A G, Ure J, Brown K, Bacon E J, Wolf C R. Proc Natl Acad Sci USA. 1998;95:5275–5280. doi: 10.1073/pnas.95.9.5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lowry O H, Rosebrough N J, Farr A L, Randall R J. J Biol Chem. 1951;193:265–275. [PubMed] [Google Scholar]
- 16.Baker M A, Cerniglia G J, Zaman A. Anal Biochem. 1990;190:360–365. doi: 10.1016/0003-2697(90)90208-q. [DOI] [PubMed] [Google Scholar]
- 17.Jollow D J, Mitchell J R, Potter W Z, Davis D C, Gillette J R, Brodie B B. J Pharmacol Exp Ther. 1973;187:195–202. [PubMed] [Google Scholar]
- 18.Adamson G M, Harman A W. Biochem Pharmacol. 1993;45:2289–2294. doi: 10.1016/0006-2952(93)90201-7. [DOI] [PubMed] [Google Scholar]
- 19.Lores Arnaiz S, Llesuy S, Cutrin J C, Boveris A. Free Radical Biol Med. 1995;19:303–310. doi: 10.1016/0891-5849(95)00023-q. [DOI] [PubMed] [Google Scholar]
- 20.Smith C V, Jaeschke H. Chem Biol Interact. 1989;70:241–248. doi: 10.1016/0009-2797(89)90047-1. [DOI] [PubMed] [Google Scholar]
- 21.Routledge P, Vale J A, Bateman D N, Johnston G D, Jones A, Judd A, Thomas S, Volans G, Prescott L F, Proudfoot A. Br Med J. 1998;317:1609–1610. doi: 10.1136/bmj.317.7173.1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dawson A H, Henry D A, McEwen J. Med J Aust. 1989;150:329–331. doi: 10.5694/j.1326-5377.1989.tb136496.x. [DOI] [PubMed] [Google Scholar]
- 23.Mirochnitchenko O, Weisbrot-Lefkowitz M, Reuhl K, Chen L, Yang C, Inouye M. J Biol Chem. 1999;274:10349–10355. doi: 10.1074/jbc.274.15.10349. [DOI] [PubMed] [Google Scholar]
- 24.Chen W, Shockcor J P, Tonge R, Hunter A, Gartner C, Nelson S D. Biochemistry. 1999;38:8159–8166. doi: 10.1021/bi990125k. [DOI] [PubMed] [Google Scholar]
- 25.Adams K J, Carmichael J, Wolf C R. Cancer Res. 1985;45:1669–1673. [PubMed] [Google Scholar]
- 26.Black S M, Wolf C R. Pharmacol Ther. 1991;51:139–154. doi: 10.1016/0163-7258(91)90044-m. [DOI] [PubMed] [Google Scholar]
- 27.Adler V, Zhimin Y, Fuchs S Y, Benezra M, Freer S, Tew K D, Pincus M R, Hsiang-Fu K, Henderson C J, Wolf C R, et al. EMBO J. 1999;18:1321–1334. doi: 10.1093/emboj/18.5.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Herdegen T, Skene P, Bahr M. Trends Neurosci. 1997;20:227–231. doi: 10.1016/s0166-2236(96)01000-4. [DOI] [PubMed] [Google Scholar]
- 29.Herdegen T, Mielke K, Kallunki T. Neuroscientist. 1999;5:147–154. [Google Scholar]
- 30.Wisdom R, Johnson R S, Moore C. EMBO J. 1999;18:188–197. doi: 10.1093/emboj/18.1.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blazka M E, Bruccoleri A, Simeonova P P, Germolec D R, Pennypacker K R, Luster M I. Res Commun Mol Pathol Pharmacol. 1996;92:259–273. [PubMed] [Google Scholar]
- 32.Kitteringham N R, Powell H, Clement Y N, Dodd C C, Tettey J N, Pirmohamed M, Smith D A, McLellan L I, Kevin Park B. Hepatology. 2000;32:321–333. doi: 10.1053/jhep.2000.9602. [DOI] [PubMed] [Google Scholar]
- 33.Floren C H, Thesleff P, Nilsson A. Acta Med Scand. 1987;222:285–288. doi: 10.1111/j.0954-6820.1987.tb10672.x. [DOI] [PubMed] [Google Scholar]
- 34.Hartleb M. Am J Gastroenterol. 1994;89:1269–1270. [PubMed] [Google Scholar]
- 35.Luquel L, Azzi R, Desaint B, Massart J D, Offenstadt G. Presse Med. 1988;17:1318. [PubMed] [Google Scholar]
- 36.Moffat G J, McLaren A W, Wolf C R. J Biol Chem. 1994;269:16397–16402. [PubMed] [Google Scholar]
- 37.Hayes P C, May L, Hayes J D, Harrison D J. Gut. 1991;32:1546–1549. doi: 10.1136/gut.32.12.1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leung N W, Critchley J A. Cancer Lett. 1991;57:45–48. doi: 10.1016/0304-3835(91)90061-l. [DOI] [PubMed] [Google Scholar]