Abstract
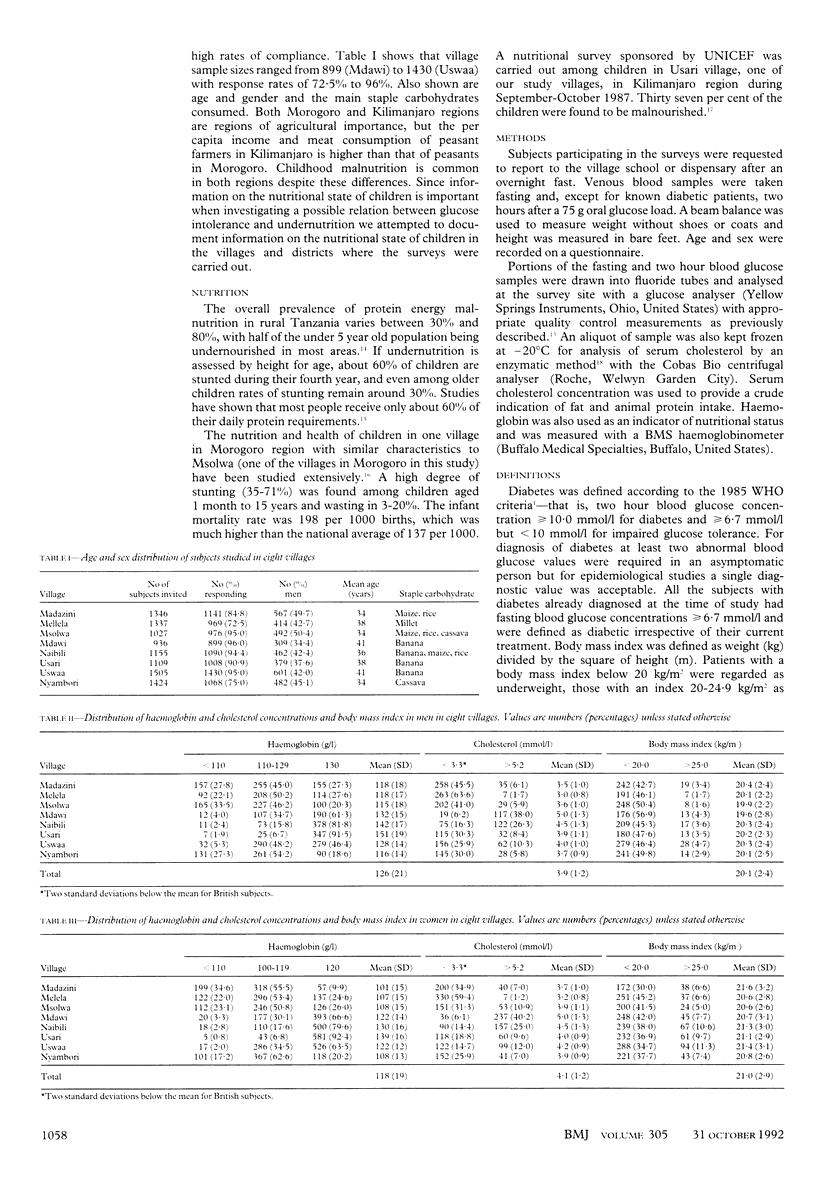
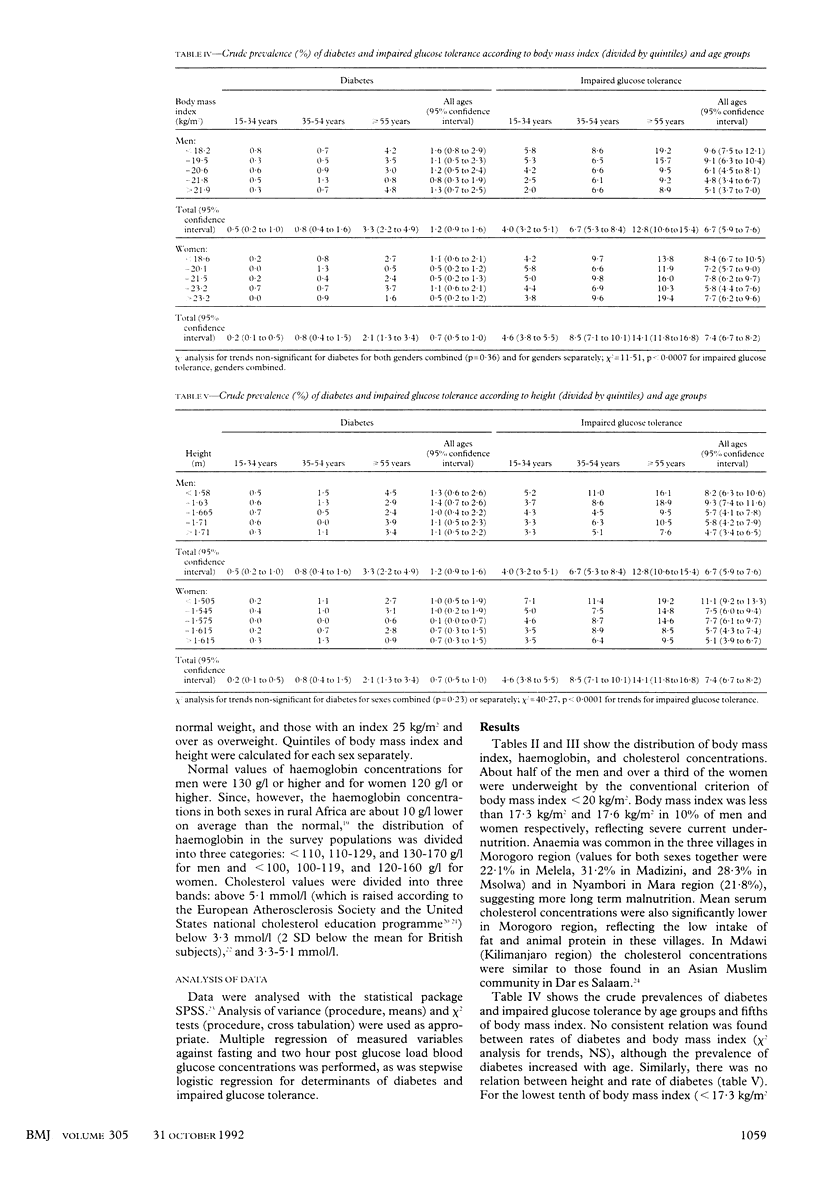
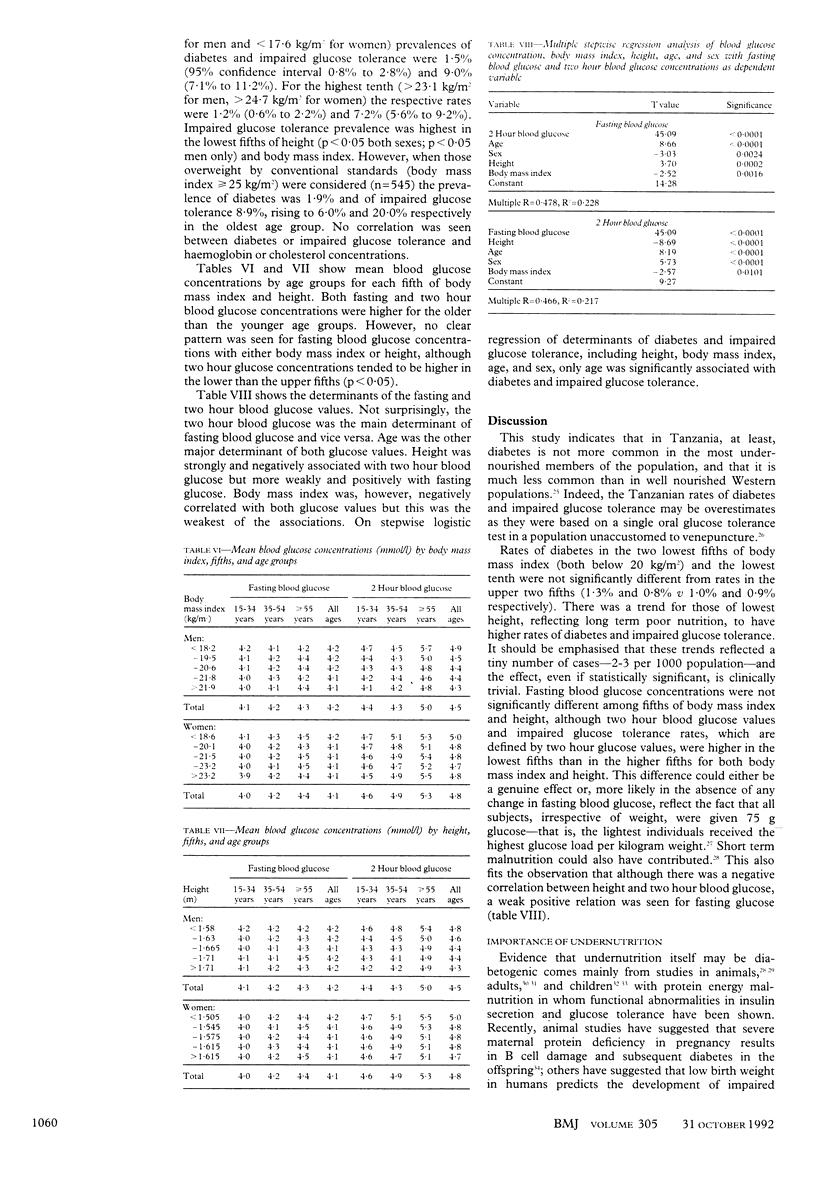
OBJECTIVE--To investigate the relation between undernutrition and diabetes. DESIGN--Survey of glucose tolerance in rural Tanzania. SETTING--Eight villages in three widely separated regions of Tanzania. SUBJECTS--8581 people aged 15 and above: 3705 men and 4876 women. MAIN OUTCOME MEASURES--Oral glucose tolerance, body mass index, height, and low haemoglobin and cholesterol concentrations. RESULTS--In the eight villages 42.7-56.9% of all men and 30.0-45.2% of all women had a body mass index below 20 kg/m2; the lowest quintile was 18.2 kg/m2 in men and 18.6 kg/m2 in women. The prevalence of diabetes did not change significantly from the lowest to the highest fifths of body mass index in men (lowest 1.6% (95% confidence interval 0.8% to 2.9%) v highest 1.3% (0.7% to 2.5%)) or women (1.1% (0.6% to 2.1%) v 0.5% (0.2% to 1.2%)). In men and in women prevalence of impaired glucose tolerance was greater in the lowest fifths of height (8.2% (6.3% to 10.6%), and 11.1% (9.2% to 13.3%)) respectively and body mass index (9.6% (7.5% to 12.1%), and 8.4% (6.7% to 10.5%)) than in the highest fifths (impaired glucose tolerance 4.7% (3.4% to 6.5%); and 5.1% (3.9% to 6.7%); body mass index 5.1% (3.7% to 7.0%), and 7.7% (6.2% to 9.6%). CONCLUSION--Rates of diabetes were not significantly associated with low body mass index or height, but overall rates were much lower than those in well nourished Western populations. Increased impaired glucose tolerance in the most malnourished people may reflect the larger glucose load per kilogram weight. The role of undernutrition in the aetiology of diabetes must be questioned.
Full text
PDF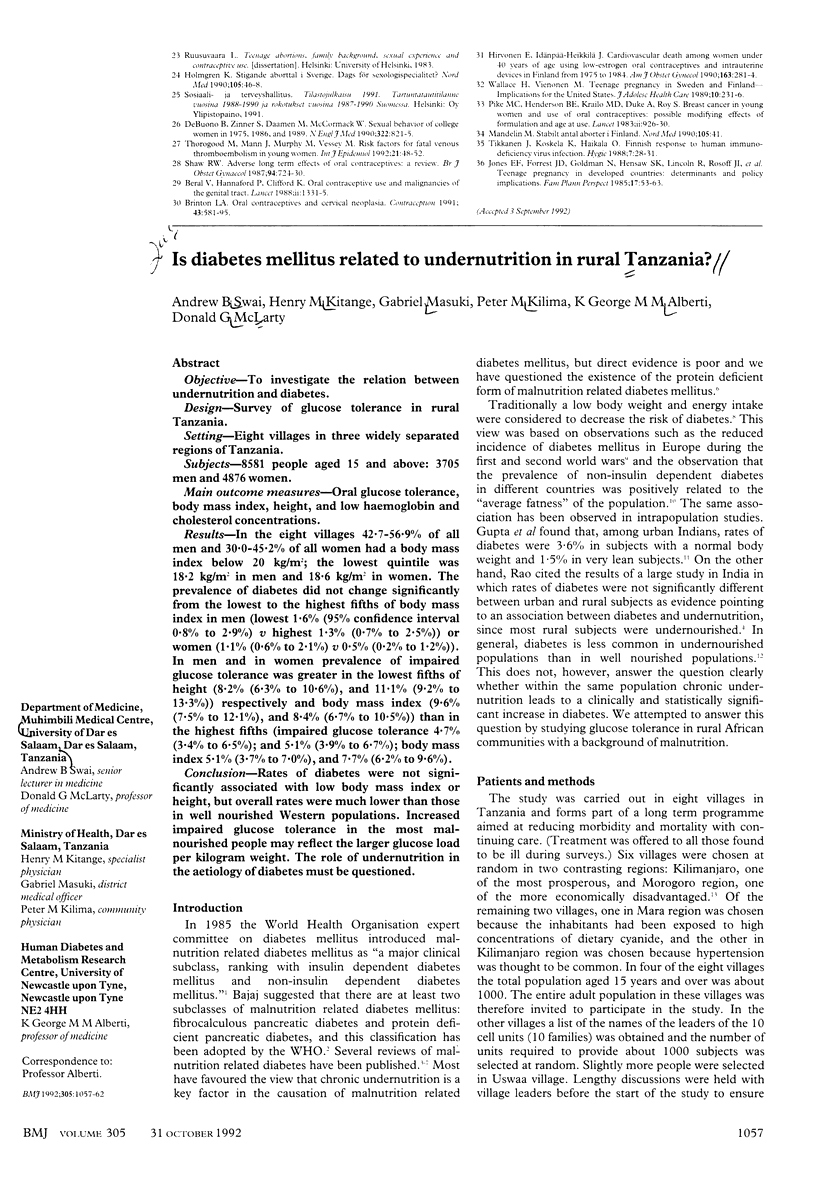


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Abu-Bakare A., Taylor R., Gill G. V., Alberti K. G. Tropical or malnutrition-related diabetes: a real syndrome? Lancet. 1986 May 17;1(8490):1135–1138. doi: 10.1016/s0140-6736(86)91846-5. [DOI] [PubMed] [Google Scholar]
- Allain C. C., Poon L. S., Chan C. S., Richmond W., Fu P. C. Enzymatic determination of total serum cholesterol. Clin Chem. 1974 Apr;20(4):470–475. [PubMed] [Google Scholar]
- Becker D. J., Pimstone B. L., Hansen J. D., Hendricks S. Insulin secretion in protein-calorie malnutrition. I. Quantitative abnormalities and response to treatment. Diabetes. 1971 Aug;20(8):542–551. doi: 10.2337/diab.20.8.542. [DOI] [PubMed] [Google Scholar]
- Cook G. C. Glucose tolerance after kwashiorkor. Nature. 1967 Sep 16;215(5107):1295–1296. doi: 10.1038/2151295a0. [DOI] [PubMed] [Google Scholar]
- DAVIES J. N. P. The essential pathology of kwashiorkor. Lancet. 1948 Feb 28;1(6496):317–320. doi: 10.1016/s0140-6736(48)92087-x. [DOI] [PubMed] [Google Scholar]
- HEALY M. J., LOCKHART R. D., MACKENZIE J. D., TANNER J. M., WHITEHOUSE R. H. Aberdeen growth study. I. The prediction of adult body measurements from measurements taken each year from birth to 5 years. Arch Dis Child. 1956 Oct;31(159):372–381. doi: 10.1136/adc.31.159.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales C. N., Barker D. J., Clark P. M., Cox L. J., Fall C., Osmond C., Winter P. D. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ. 1991 Oct 26;303(6809):1019–1022. doi: 10.1136/bmj.303.6809.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M. I., Hadden W. C., Knowler W. C., Bennett P. H. Prevalence of diabetes and impaired glucose tolerance and plasma glucose levels in U.S. population aged 20-74 yr. Diabetes. 1987 Apr;36(4):523–534. doi: 10.2337/diab.36.4.523. [DOI] [PubMed] [Google Scholar]
- Keen H., Ekoe J. M. The geography of diabetes mellitus. Br Med Bull. 1984 Oct;40(4):359–365. doi: 10.1093/oxfordjournals.bmb.a072005. [DOI] [PubMed] [Google Scholar]
- Khardori R. Undernutrition and diabetes. Diabetes Care. 1985 May-Jun;8(3):302–302. doi: 10.2337/diacare.8.3.302a. [DOI] [PubMed] [Google Scholar]
- Kimati V. P., Scrimshaw N. S. The nutritional status of Tanzanian children: A cross-sectional anthropometric community survey report. East Afr Med J. 1985 Feb;62(2):105–117. [PubMed] [Google Scholar]
- Mann J. I., Lewis B., Shepherd J., Winder A. F., Fenster S., Rose L., Morgan B. Blood lipid concentrations and other cardiovascular risk factors: distribution, prevalence, and detection in Britain. Br Med J (Clin Res Ed) 1988 Jun 18;296(6638):1702–1706. doi: 10.1136/bmj.296.6638.1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao R. H. The role of undernutrition in the pathogenesis of diabetes mellitus. Diabetes Care. 1984 Nov-Dec;7(6):595–601. doi: 10.2337/diacare.7.6.595. [DOI] [PubMed] [Google Scholar]
- SHAPER A. G. Chronic pancreatic disease and protein malnutrition. Lancet. 1960 Jun 4;1(7136):1223–1224. doi: 10.1016/s0140-6736(60)91103-x. [DOI] [PubMed] [Google Scholar]
- Smith S. R., Edgar P. J., Pozefsky T., Chhetri M. K., Prout T. E. Insulin secretion and glucose tolerance in adults with protein-calorie malnutrition. Metabolism. 1975 Sep;24(9):1073–1084. doi: 10.1016/0026-0495(75)90101-8. [DOI] [PubMed] [Google Scholar]
- Snoeck A., Remacle C., Reusens B., Hoet J. J. Effect of a low protein diet during pregnancy on the fetal rat endocrine pancreas. Biol Neonate. 1990;57(2):107–118. doi: 10.1159/000243170. [DOI] [PubMed] [Google Scholar]
- Swai A. B., McLarty D. G., Kitange H. M., Kilima P. M., Masuki G., Mtinangi B. I., Chuwa L., Alberti G. M. Study in Tanzania of impaired glucose tolerance. Methodological myth? Diabetes. 1991 Apr;40(4):516–520. doi: 10.2337/diab.40.4.516. [DOI] [PubMed] [Google Scholar]
- Swenne I., Crace C. J., Milner R. D. Persistent impairment of insulin secretory response to glucose in adult rats after limited period of protein-calorie malnutrition early in life. Diabetes. 1987 Apr;36(4):454–458. doi: 10.2337/diab.36.4.454. [DOI] [PubMed] [Google Scholar]
- Tanner M., Burnier E., Mayombana C., Betschart B., de Savigny D., Marti H. P., Suter R., Aellen M., Lüdin E., Degrémont A. A. Longitudinal study on the health status of children in a rural Tanzanian community: parasitoses and nutrition following control measures against intestinal parasites. Acta Trop. 1987 Jun;44(2):137–174. [PubMed] [Google Scholar]
- Walker M., Shaper A. G., Wannamethee G. Height and social class in middle-aged British men. J Epidemiol Community Health. 1988 Sep;42(3):299–303. doi: 10.1136/jech.42.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West K. M., Kalbfleisch J. M. Influence of nutritional factors on prevalence of diabetes. Diabetes. 1971 Feb;20(2):99–108. doi: 10.2337/diab.20.2.99. [DOI] [PubMed] [Google Scholar]
- Whincup P. H., Cook D. G., Shaper A. G. Social class and height. BMJ. 1988 Oct 15;297(6654):980–981. doi: 10.1136/bmj.297.6654.980-c. [DOI] [PMC free article] [PubMed] [Google Scholar]


