Abstract
Aims
To assess the level of undertreatment of hypercholesterolaemia in the general population, taking intra-person variability in serum cholesterol concentrations into account, and to identify determinants of undertreatment of hypercholesterolaemia.
Methods
In this cross-sectional study, data from two population-based surveys on cardiovascular disease risk factors conducted between 1987 and 1997 in the Netherlands were used. For all 64 757 respondents aged 20–59 years, treatment eligibility for lipid-lowering drug use was established according to the Dutch Cholesterol Consensus. Multivariate logistic models were used to identify determinants of undertreatment.
Results
During the study period, 56.8% of the study population had undesirable cholesterol concentrations (serum total cholesterol>5 mmol l−1) and 5.5% of those were eligible for pharmacological treatment based on their absolute risk of coronary heart disease. Of those eligible for pharmacological treatment, 16.3% were treated, and 19.6% of those treated had their serum total cholesterol concentration controlled. Only 3.2% of those eligible for pharmacological treatment were both treated and controlled. We identified several determinants for undertreatment, e.g. male gender and younger age for primary prevention and female gender and older age for secondary prevention. Treatment has improved slightly in more recent years.
Conclusions
Over 95% of the population eligible for the pharmacological treatment of hypercholesterolaemia was either untreated or was uncontrolled. To decrease undertreatment, identification of high-risk patients should be increased. Those who are treated with lipid-lowering medication could further benefit from more aggressive treatment, especially with statins.
Keywords: antilipaemic agents, drug therapy, hypercholesterolaemia, risk factors
Introduction
HMG-Co A reductase inhibitors (statins) have proven to be safe and effective in reducing fatal and nonfatal cardiovascular events in both primary [1, 2] and secondary prevention [3–5], and produce a reduction in total mortality of approximately 30%. Hence, new and revised national and international guidelines have been issued to guide their use [6–8].
From a public health perspective as well as for the individual patient, adherence to these guidelines is of great importance. However, undertreatment of hypercholesterolaemia (defined as lack of treatment or inadequate treatment) has frequently been observed [9–31]. Most of these studies have been limited to subjects with established coronary heart disease (CHD) and did not include primary prevention [9, 12, 14, 15, 19–24, 27–31]. In addition, they were either not population-based [17, 18, 25], used old guidelines [13], did not determine treatment eligibility on a patient level [10] or focused exclusively on the elderly [16]. Intra-person variability of serum cholesterol concentrations has not been taken into account in any of these studies. A previous study showed that this may lead to a misclassification rate of National Cholesterol Education Program risk status of at least 7% [32]. This correction requires repeated measurements of serum cholesterol concentrations from a sample of the entire screened population.
The aim of the present study was to assess the level of undertreatment of hypercholesterolaemia in the general population, taking intra-person variability in serum cholesterol concentrations into account, and to identify determinants of undertreatment of hypercholesterolaemia.
Methods
Data
Data were obtained from two population-based surveys on cardiovascular disease risk factors conducted in the Netherlands. The Monitoring Project on Cardiovascular Disease Risk Factors was carried out from 1987 to 1992. Each year a new random sample of men and women aged 20–59 years in Amsterdam, Maastricht and Doetinchem was selected. This project was continued from 1993 to 1997 as the ‘MORGEN’ project (Monitoring Project on Risk Factors for Chronic Diseases). In Amsterdam and Maastricht, new random samples were selected, whereas in Doetinchem the study population consisted of individuals who had participated in the previous study. All respondents completed a questionnaire that contained questions on demographic variables, cardiovascular risk factors and current use of medication. Additionally, height, weight and blood pressure were measured and blood was drawn (nonfasting) for total cholesterol (Tc) and high density lipoprotein (HDL) cholesterol determination. The design of this study has been described in detail elsewhere [33].
Total and HDL cholesterol determinations were performed in the Lipid Reference Laboratory (LRL) of the University Hospital Dijkzigt in Rotterdam. A random zero sphygmomanometer was used to measure blood pressure twice by a trained technician (after 5 min) with the subject in an upright position. Information on other cardiovascular risk factors, e.g. smoking status and diabetes, were obtained from the questionnaire.
In the Monitoring Project on Cardiovascular Disease Risk Factors, the overall response rate was about 50% in men and 57% in women. In the Monitoring Project on Risk Factors for Chronic Diseases, the overall response rate was about 40% in men and 46% in women.
A nonresponse survey was conducted in order to assess possible selection bias. For this survey, all nonrespondents (n = 1620) in the period August–December 1991 were selected [33]. The nonrespondents were approached by telephone (75%) or by mail (25%). The response was 61%; 23% could not be reached and 16% refused to participate. Because information on biological risk factors such as serum cholesterol concentrations and blood pressure could not be obtained from the nonrespondents, educational level was used to evaluate potential selection bias with respect to these risk factors, as educational level is a main determinant of nonresponse and is known to be associated with these risk factors [34, 35]. The results of the nonresponse survey suggested that no substantial selection with respect to educational level had taken place.
Guidelines
Treatment eligibility was established according to the revised Dutch Consensus Cholesterol (DCC), which was released in 1998 [8]. These guidelines on the management of hypercholesterolaemia indicate pharmacological treatment in three situations:
Familial hypercholesterolaemia (FH), which is suspected if Tc concentrations exceed 8 mmol l−1. Patients with Tc > 8 mmol l−1 should be referred to a lipid clinic for further diagnostics and individual treatment strategies.
Secondary prevention, including cerebrovascular accidents (CVA) and peripheral arterial disease (PAD), unless Tc ≤ 5 mmol l−1. In this study secondary prevention was defined as a self-reported history of myocardial infarction (MI), coronary artery bypass graft (CABG), percutaneous transluminal coronary angioplasty (PTCA), heart catheterization or stroke. The questionnaire did not include any specific questions on angina pectoris or PAD.
Primary prevention, when Tc > 5 mmol l−1 and the absolute level of risk of coronary heart disease exceeds an age and gender specific cut-off point. These cut-off points are based on a maximum of approximately ]18 000 per life year saved.
In the DCC, the Framingham risk function is used to estimate the 10-year risk of coronary heart disease (CHD; consisting of myocardial infarction (MI) and CHD death plus angina pectoris and coronary insufficiency) for persons aged 30–74 years. The Framingham risk function includes gender, age (years), SBP (mmHg), the Tc/HDLc ratio, diabetes (yes/no), smoking (yes/no) and ECG-left ventricular hypertrophy (ECG-LVH; yes/no) [36]. As we had no information on ECG-LVH, all patients were considered not to have ECG-LVH. Pharmacological treatment for hypercholesterolaemia is indicated for those aged between 40 and 60 years if the absolute 10-year risk is>25%, for those aged between 60 and 70 years if the 10-year risk is>30% and above age 70 years if the 10-year risk is>40% (men) or > 35% (women). These levels are 5% lower in patients with diabetes mellitus or a family history of CHD (CHD in parents <60 years).
We applied the Framingham risk function to our entire population without established CHD in order to assess treatment eligibility, including respondents with Tc > 8 mmol l−1. As we had no additional information on a patient's genetic profile, we could not distinguish between ‘true’ FH and high Tc concentrations. We chose to apply the Framingham risk function to these respondents as well. Of all the respondents to whom we applied the Framingham risk function, 18.6% (n = 7151) did not meet the criteria for application of this function, mainly because they were younger than 30 years of age (n = 3710) or had serum total cholesterol or HDL-cholesterol concentrations not within the Framingham limits, 3.9–9.4 mmol l−1 and 0.7–2.7 mmol l−1, respectively (n = 2529).
Correction for intra-person variability
Repeated measurements of total cholesterol and HDL cholesterol were available from a sample of 924 subjects examined in 1989 who were re-examined 1 year later. These measurements were used to calculate serum total cholesterol and HDL-cholesterol concentrations corrected for intra-person variability [37].
This correction was performed separately for respondents treated and untreated with lipid-lowering medication and after stratification by sex and 10-year age categories. This correction was performed within these strata because each stratum can be considered as a separate subpopulation with a specific distribution of total cholesterol concentrations. By using this approach, each individual's total cholesterol concentration was corrected by the mean of the stratum to which that individual belonged.
We established treatment eligibility using both crude and corrected serum cholesterol concentrations. As there was only a small difference between both analyses (approximately 5%), we chose to show the results using corrected serum cholesterol concentrations only.
Missing values
Subjects with missing data on gender, serum total cholesterol or HDL-cholesterol concentrations or systolic or diastolic blood pressure were excluded from the analysis (n = 845; 1.3%). For 3176 subjects (4.9%) who accidentally omitted one or more questions on a specific disease in the questionnaire, we assumed that they did not have the disease or condition specified.
Undertreatment
Treatment eligibility was established for all respondents. Use of lipid-lowering medication was assumed to be correctly initiated and therefore all subjects using lipid-lowering drugs were considered eligible for treatment. In the screening projects, lipid-lowering drug use was recorded in two ways. Firstly, respondents were asked if they used medication to lower their cholesterol concentrations and secondly, respondents were asked to specify the drug(s) they were using. In 9.8% of the respondents with a self-reported history of lipid-lowering drug use, the information on the type(s) of drug(s) was missing. In 86.6% of all subjects reporting the use of lipid-lowering treatment, lipid-lowering drug use was confirmed by checking the registered indications of the drug(s) listed by the respondent. Therefore, all participants reporting the use of lipid-lowering medication were considered pharmacologically treated for hypercholesterolaemia.
We distinguished two types of undertreatment. The first type was defined as inappropriately not receiving cholesterol-lowering medication and the second type was defined as receiving pharmacological treatment but having uncontrolled serum total cholesterol concentrations. The treatment target of the DCC is Tc ≤ 5 mmol l−1 for both primary and secondary prevention.
Statistical analysis
Prevalences of the presence, treatment and undertreatment of hypercholesterolaemia and their 95% confidence intervals (CI) were estimated and standardized to the age and gender distribution of the general Dutch population in 1992. Multivariate logistic regression models were used to assess the association between demographic variables, CVD risk factors, medication use and treatment with lipid-lowering drugs (separate analyses for primary and secondary prevention) or reaching the treatment goal.
Results
From 1987 to 1997, 64 757 men and women between 20 and 59 years of age were examined. After exclusion of pregnant women (n = 489) and subjects with missing data (n = 845), 63 423 subjects remained for the analysis.
Table 1 lists the prevalence of suboptimal cholesterol concentrations (defined as Tc > 5 mmol l−1 or receiving lipid-lowering medication), eligibility for treatment according to the DCC, and treated and controlled hypercholesterolaemia. In the period 1987–97, 56.8% of the population between 20 and 59 years of age had suboptimal cholesterol concentrations, 5.5% of those were eligible for pharmacological treatment based on their total risk profile, 16.3% of those eligible for pharmacological treatment were treated and 19.6% of those treated had their serum total cholesterol concentrations controlled. Only 3.2% of those eligible for pharmacological treatment were both treated and controlled.
Table 1.
Prevalence of suboptimal cholesterol concentrations, eligibility for treatment, treated and controlled hypercholesterolaemia in men and women by 10-year age category, weighted by the age and gender distribution of the general Dutch population in 1992 and corrected for intra-person variability.
| Respondents | Suboptimal cholesterol concentrations (Tc > 5 mmol l−1) | Eligible for treatment (including those treated)* | Treated | Controlled** | |
|---|---|---|---|---|---|
| Overall | 63 423 | 40 064 (56.8%) | 2719 (5.5%) | 430 (16.3%) | 83 (19.6%/3.2%) |
| Men | |||||
| 20–29 years | 5 107 | 1 471 (28.8%) | 6 (0.4%) | 4 (66.7%) | 1 (25.0%/16.7%) |
| 30–39 years | 7 476 | 4 271 (57.1%) | 65 (1.5%) | 16 (24.6%) | 1 (6.2%/1.5%) |
| 40–49 years | 8 693 | 6 705 (77.1%) | 369 (5.5%) | 83 (22.5%) | 15 (18.1%/4.1%) |
| 50–59 years | 8 341 | 7 089 (85.0%) | 1558 (22.0%) | 156 (10.0%) | 39 (25.0%/2.5%) |
| 20–59 years | 29 617 | 19 536 (58.8%) | 1998 (7.9%) | 259 (14.1%) | 56 (20.7%/2.9%) |
| Women | |||||
| 20–29 years | 6 248 | 2 251 (36.0%) | 6 (0.3%) | 1 (16.7%) | 1 (100%/16.7%) |
| 30–39 years | 8 484 | 3 732 (44.0%) | 48 (1.3%) | 7 (14.6%) | 2 (28.6%/4.2%) |
| 40–49 years | 9 734 | 6 328 (65.0%) | 136 (2.1%) | 29 (21.3%) | 8 (27.6%/5.9%) |
| 50–59 years | 9 340 | 8 217 (88.0%) | 531 (6.5%) | 134 (25.2%) | 16 (11.9%/3.0%) |
| 20–59 years | 33 806 | 20 528 (54.8%) | 721 (2.8%) | 171 (23.1%) | 27 (17.4%/4.0%) |
based on the Dutch Consensus Cholesterol
% of those treated and percentage of those eligible for treatment, respectively.
The prevalence of having suboptimal cholesterol concentrations increased with age for both men and women. More men than women were eligible for pharmacological treatment of hypercholesterolaemia. For both genders, eligibility increased with age. The most pronounced differences between men and women were observed in the age category 50–59 years of age. Although eligibility was higher in men than in women, treatment was more prevalent in women. The percentages of those treated and controlled are small for both men and women, not exceeding 6% except in those younger than 30 years of age. Of the 2289 subjects who were eligible for treatment, but not receiving lipid-lowering medication, only 730 (31.9%) were aware of their high cholesterol concentrations.
The prevalence of having suboptimal cholesterol concentrations decreased over time (Table 2), but the prevalence of treatment eligibility increased slightly.
Table 2.
Prevalences of suboptimal cholesterol concentrations, eligibility for treatment, treated and controlled hypercholesterolaemia for different time periods and separately for primary and secondary prevention, weighted by the age and gender distribution of the general Dutch population and corrected for intra-person variability.
| Respondents | Suboptimal cholesterol concentrations | Eligible for treatment | Treated | Controlled* | |
|---|---|---|---|---|---|
| 1987–92 | 41 647 | 27 457 (59.6%) | 1739 (5.1%) | 165 (10.1%) | 12 (7.7%/0.8%) |
| 1993–97 | 21 776 | 12 607 (51.7%) | 980 (6.6%) | 265 (27.0%) | 71 (27.3%/7.4%) |
| Primary prevention** | 61 918 | 38 839 (62.7%) | 1494 (3.8%) | 294 (19.7%) | 36 (12.2%/2.4%) |
| Secondary prevention** | 1 505 | 1 225 (81.4%) | 1225 (100.0%) | 136 (11.1%) | 47 (34.6%/3.8%) |
% of those treated and percentage of those eligible for treatment, respectively
correction for the age and gender distribution not possible, because data on the age and gender distribution of the Dutch population among those with or without pre-existing CHD was not available.
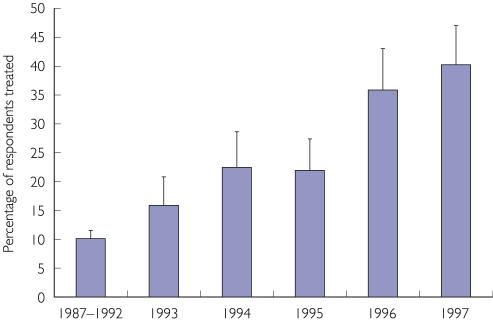
Between 1987 and 1992 10.1% of those eligible for treatment were treated compared with 27.0% in the period 1993–97. In addition, the prevalence of reaching the treatment goal among those treated increased, from 7.7% in the period 1987–92 to 27.3% in the period 1993–97. Figure 1 shows that treatment of hypercholesterolaemia among those eligible for treatment increased slightly over the years 1987–95, but increased sharply between 1995 and 1996.
Figure 1.
Percentage of respondents treated for hypercholesterolaemia among those eligible for pharmacological treatment according to the Dutch Consensus Cholesterol [8]
In secondary prevention all those with suboptimal cholesterol concentrations (81.4% of those with a history of CHD) were eligible for treatment, but only a minority was treated (11.1%) or treated and controlled (3.8%). In primary prevention, the prevalence of treatment eligibility was much lower (3.8%), but the prevalence of being treated and controlled (2.4%) yielded similar results.
Control of serum cholesterol concentrations was better in secondary prevention (34.6%) than in primary prevention (12.2%) (Table 3). Among all pharmacologically treated subjects, 3.5% had a serum total cholesterol concentration exceeding 8 mmol l−1.
Table 3.
Serum total cholesterol concentrations in respondents treated with lipid-lowering drugs, corrected for within-person variability.
| Serum total cholesterol | Primary prevention (n = 294) | Secondary prevention (n = 136) | Total (n = 430) |
|---|---|---|---|
| ≤ 5.00 mmol l−1 | 36 (12.2%) | 47 (34.6%) | 83 (19.3%) |
| 5.01–6.50 mmol l−1 | 164 (55.8%) | 69 (50.7%) | 233 (54.2%) |
| 6.51–8.00 mmol l−1 | 84 (28.6%) | 15 (11.0%) | 99 (23.0%) |
| > 8.00 mmol l−1 | 10 (3.4%) | 5 (3.7%) | 15 (3.5%) |
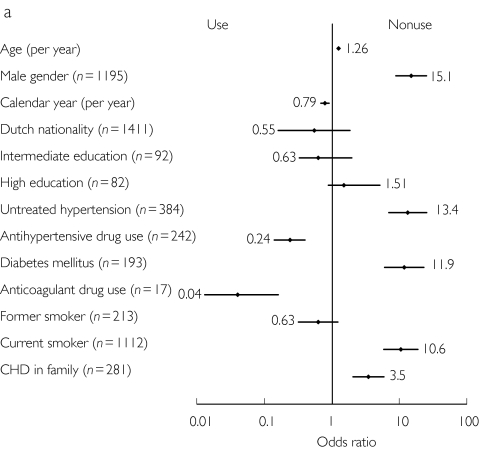
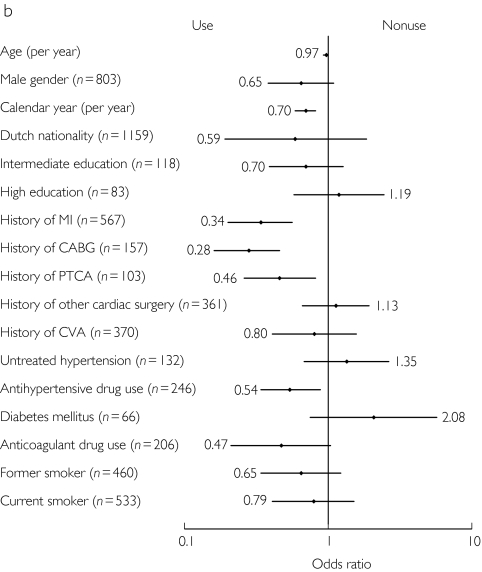
Figure 2 shows the determinants associated with nonuse of lipid-lowering drugs among subjects eligible for treatment of primary prevention (A) and secondary prevention (B). In primary prevention, elderly subjects and men had a higher risk of not receiving lipid-lowering drugs, whereas in secondary prevention women and younger subjects had a higher risk of not receiving lipid-lowering drugs. In more recent years, subjects were more likely to receive lipid-lowering drugs.
Figure 2.
Determinants of nonuse of lipid-lowering drugs among those eligible for primary prevention (A) (n = 1494) and secondary prevention (B) (n = 1225). All odds ratios are adjusted for demographic variables, cardiovascular risk factors and medication use. The odds ratio for anticoagulant drug use is based on data from the Peilstation project only (n = 1048 and n = 687 for primary and secondary prevention, respectively).
Subjects with untreated hypertension, diabetes mellitus and CHD at age < 60 years in first degree family members tended to be less frequently treated, whereas respondents concomitantly treated with either antihypertensive drugs or anticoagulant drugs were more frequently receiving lipid-lowering drugs. Current smoking was associated with nonuse in primary prevention only and former smoking was not significantly associated with lipid-lowering drug use. Although a low educational level was most prevalent in patients eligible for pharmacological treatment (approximately 85%), educational level was not associated with receiving lipid-lowering medication. For further details, see Figure 2.
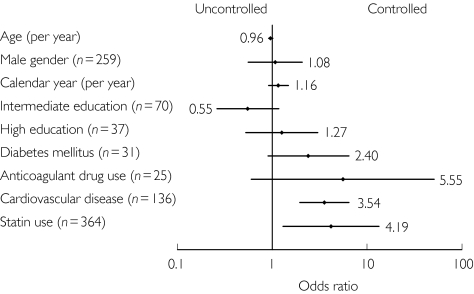
The factors associated with having serum lipids controlled among treated patients are shown in Figure 3. Respondents using statins compared with respondents using nonstatin lipid-lowering drugs and respondents with a history of cardiovascular disease had their cholesterol concentrations more frequently controlled.
Figure 3.
Determinants of having serum total cholesterol controlled among those treated with lipid-lowering drugs (n = 430). All odds ratios are adjusted for demographic variables, cardiovascular risk factors and medication use. The odds ratio for anticoagulant drug use is based on data from the Peilstation project only (n = 165).
Discussion
This study demonstrates that a substantial proportion of the general Dutch population aged 20–59 years who were eligible for lipid-lowering medication were undertreated between 1987 and 1997. Of those eligible for pharmacological treatment of hypercholesterolaemia, only 16.3% were treated, and only 19.6% of these had their serum total cholesterol concentrations controlled. Only 3.2% of those eligible for pharmacological treatment of hypercholesterolaemia were both treated and controlled.
Results were similar for men and women and for primary and secondary prevention, but prevalence of treatment increased over time. The publication and dissemination of landmark trials on the treatment of hypercholesterolaemia (1994/1995) coincided with an increase in treatment of hypercholesterolaemia after a lag time of about 1–2 years. In primary prevention age, male gender, untreated hypertension, diabetes mellitus, current smoking and a family history of CHD increased the chance of not using lipid-lowering drugs when they were indicated, whereas the use of other cardiovascular drugs was associated with greater use of lipid-lowering drugs. In secondary prevention we found that subjects with a history of coronary events and subjects using other cardiovascular drugs were more likely to receive lipid-lowering drugs, while subjects with diabetes mellitus were less likely to receive these drugs (not statistically significant). Respondents with a history of cardiovascular disease and those treated with statins compared with those treated with nonstatin lipid-lowering drugs had their cholesterol concentrations more frequently controlled.
Although this large, population-based study has been carried out in the Netherlands, the results may be applicable to other European and industrialized countries as well. Most of these countries use guidelines based on the joint recommendations of the European Society of Cardiology, the European Atherosclerosis Society and the European Society of Hypertension [6] and treatment eligibility may therefore be comparable. In addition, the use of lipid-lowering drugs in the Netherlands is similar to the use of these drugs in other western countries [38].
Our study may have several limitations affecting the validity of our estimates. We relied on self-reported data on cardiovascular disease risk factors and medication use. Agreement between the questionnaire information and information from general practitioners was variable, but fair to moderate for conditions such as stroke, diabetes mellitus and MI [39]. For antihypertensive drug use, Klungel et al. found that the agreement between self-reporting and pharmacy records was high [40]. Only 86.6% of all subjects reporting lipid-lowering drug use listed a drug that was registered for this indication. Therefore, considering all such respondents as receiving lipid-lowering treatment probably underestimated the actual prevalence of nonuse of lipid-lowering therapy.
We had no valid information on angina pectoris and peripheral artery disease and therefore these diseases could not be included in our definition of secondary prevention. This will have underestimated the prevalence of undertreatment of hypercholesterolaemia in secondary prevention, because respondents suffering from one of these diseases who had a Tc > 5 mmol l−1 would have been eligible for pharmacological treatment. The lack of information on ECG-LHV may also have underestimated prevalence of undertreatment in primary prevention. Subjects with ECG-LVH have a higher 10-year risk of CHD, and more subjects would have been eligible for treatment if we could have taken the presence of ECG-LHV into account.
Also, genetic information on the presence of FH was not available for our analysis. We chose to apply the Framingham risk function to those with higher total cholesterol concentrations to establish treatment eligibility as well. Some of these respondents who are not eligible based on the absolute level of 10-year risk of CHD, may have had familial hypercholesterolaemia and therefore may have been eligible for treatment. This also may have underestimated the prevalence of undertreatment of hypercholesterolaemia in primary prevention.
Besides undertreatment, overtreatment may also occur. In this study, however, we were not able to assess treatment eligibility for those already treated with lipid-lowering drugs. We assumed that the use of lipid-lowering medication was correctly initiated, but the validity of this assumption may be questioned for primary prevention. Many of the respondents treated in primary prevention were women without diabetes mellitus, although the indication for lipid-lowering drug use is rare in this subpopulation [8]. The same was observed for nonsmoking men without diabetes mellitus. Little attention is paid to overtreatment in literature. Abookire et al. observed overuse of statin therapy among 69% of patients receiving lipid-lowering medication for primary prevention and among 47% of patients receiving lipid-lowering medication for secondary prevention [29]. For primary prevention, our observations are probably comparable with the results of the present study.
The low rate of lipid-lowering treatment among those eligible for treatment was observed in previous studies as well. The only other large study in a general population was conducted in 1998 in England [26]. This cross-sectional survey showed that only 3% of those eligible for primary prevention used lipid-lowering drugs and only 30% of those eligible for secondary prevention. Other studies on undertreatment in both primary and secondary prevention in the USA yielded estimates of overall treatment prevalence between 14% and 48% [10, 13, 16–18, 25]. The highest prevalences of treatment were observed in high risk patients [13, 17]. Many studies have been conducted in patients with CHD only. The use of lipid-lowering drugs in those studies ranged from 12%-38% [9, 11, 12, 15, 19, 20, 22, 29, 31, 41].
In our study, only 19.6% of those treated with lipid-lowering drugs had their serum total cholesterol concentration controlled (< 5 mmol l−1), ranging from 12.6% in primary prevention to 35.9% in secondary prevention. This pattern was also observed in Norwegian general practices [42]. The overall proportion of patients who achieved the treatment goals was 35.5%, and was higher in secondary prevention (43.9%) than in primary prevention (17.0%). Others found similar overall rates, but observed higher rates in primary prevention (up to 68%) than in secondary prevention (approximately 20%) [43, 44]. The low proportion of patients who reach their treatment goal may at least partially be explained by the fact that they require a larger reduction in serum total cholesterol than can be obtained by many therapies [41]. Over 25% of our population had a serum total cholesterol of>6.5 mmol l−1 despite lipid-lowering treatment. Other explanations include lack of dose adjustment and noncompliance [43].
Adherence to guidelines on the management of hypercholesterolemia might be improved by considering the patient characteristics that are associated with nonuse of lipid-lowering drugs. The use of antihypertensive or anticoagulant drugs was associated with greater likelihood of use of lipid-lowering drugs, whereas untreated hypertension was associated with nonuse. Respondents who visit a physician more frequently might be better treated with lipid-lowering drugs because their lipid profile is determined more frequently or at an earlier stage. Another possible explanation is higher compliance to drug therapy in general by these respondents. A substantial proportion of those who were eligible for treatment but were not treated were unaware of their high serum cholesterol concentrations. This may also explain the high odds ratio we found for the association between male gender and nonuse in primary prevention. Women visit their physician more frequently [45, 46] and may therefore be more likely to receive lipid-lowering drugs. However, diabetes mellitus was strongly associated with nonuse as well, while these patients will receive medical care and diabetes is a well known cause of secondary dyslipidaemia and of cardiovascular diseases. Other determinants associated with nonuse in primary prevention were elderly age and a family history of CHD; physicians should focus on these undertreated subgroups. Furthermore, more attention should be paid to reaching the treatment goal, especially in primary prevention.
In conclusion, a large majority of the population studied were either untreated for hypercholesterolaemia or were uncontrolled. Treatment improved slightly during more recent years, and undertreatment was more prevalent in secondary prevention than in primary prevention. To improve the management of hypercholesterolaemia, the detection of hypercholesterolaemia should be increased, and physicians should focus on patients with diabetes mellitus or a family history of CHD and, in primary prevention, on men. Those who are treated with lipid-lowering medication could further benefit from more aggressive treatment, especially with statins.
References
- 1.Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 2.Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–1622. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 3.Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 4.Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 5.The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 6.Wood D, De Backer G, Faergeman O, Graham I, Mancia G, Pyorala K. Prevention of coronary heart disease in clinical practice. Summary of recommendations of the Second Joint Task Force of European and other Societies on Coronary Prevention. J Hypertens. 1998;16:1407–1414. doi: 10.1097/00004872-199816100-00003. [DOI] [PubMed] [Google Scholar]
- 7.British Cardiac Society, British Hyperlipidaemia Association, British Hypertension Society, endorsed by the British Diabetic Association. Joint British recommendations on prevention of coronary heart disease in clinical practice. Heart. 1998;80(Suppl 2):S1–S29. [PMC free article] [PubMed] [Google Scholar]
- 8.Dutch Institute for Healthcare Improvement (CBO) Utrecht: CBO; 1998. Treatment and prevention of coronary heart disease by lowering serum cholesterol levels. [In Dutch] [Google Scholar]
- 9.Cohen MV, Byrne MJ, Levine B, Gutowski T, Adelson R. Low rate of treatment of hypercholesterolemia by cardiologists in patients with suspected and proven coronary artery disease. Circulation. 1991;83:1294–1304. doi: 10.1161/01.cir.83.4.1294. [DOI] [PubMed] [Google Scholar]
- 10.Giles WH, Anda RF, Jones DH, Serdula MK, Merritt RK, DeStefano F. Recent trends in the identification and treatment of high blood cholesterol by physicians. Progress and missed opportunities. JAMA. 1993;269:1133–1138. [PubMed] [Google Scholar]
- 11.Sempos CT, Cleeman JI, Carroll MD, et al. Prevalence of high blood cholesterol among US adults. An update based on guidelines from the second report of the National Cholesterol Education Program Adult Treatment Panel. JAMA. 1993;269:3009–3014. doi: 10.1001/jama.269.23.3009. [DOI] [PubMed] [Google Scholar]
- 12.Northridge DB, Shandall A, Rees A, Buchalter MB. Inadequate management of hyperlipidaemia after coronary bypass surgery shown by medical audit. Br Heart J. 1994;72:466–467. doi: 10.1136/hrt.72.5.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nieto FJ, Alonso J, Chambless LE, et al. Population awareness and control of hypertension and hypercholesterolemia. The Atherosclerosis Risk in Communities study. Arch Intern Med. 1995;155:677–684. [PubMed] [Google Scholar]
- 14.Schrott HG, Bittner V, Vittinghoff E, Herrington DM, Hulley S. Adherence to National Cholesterol Education Program Treatment goals in postmenopausal women with heart disease. The Heart and Estrogen/Progestin Replacement Study (HERS) JAMA. 1997;277:1281–1286. [PubMed] [Google Scholar]
- 15.EUROASPIRE Study Group. EUROASPIRE. A European Society of Cardiology survey of secondary prevention of coronary heart disease: principal results. Eur Heart J. 1997;18:1569–1582. doi: 10.1093/oxfordjournals.eurheartj.a015136. [DOI] [PubMed] [Google Scholar]
- 16.Lemaitre RN, Furberg CD, Newman AB, et al. Time trends in the use of cholesterol-lowering agents in older adults: the Cardiovascular Health Study. Arch Intern Med. 1998;158:1761–1768. doi: 10.1001/archinte.158.16.1761. [DOI] [PubMed] [Google Scholar]
- 17.Frolkis JP, Zyzanski SJ, Schwartz JM, Suhan PS. Physician noncompliance with the 1993 National Cholesterol Education Program (NCEP-ATPII) guidelines. Circulation. 1998;98:851–855. doi: 10.1161/01.cir.98.9.851. [DOI] [PubMed] [Google Scholar]
- 18.Danias PG, O'Mahony S, Radford MJ, Korman L, Silverman DI. Serum cholesterol levels are underevaluated and undertreated. Am J Cardiol. 1998;81:1353–1356. doi: 10.1016/s0002-9149(98)00167-2. [DOI] [PubMed] [Google Scholar]
- 19.McBride P, Schrott HG, Plane MB, Underbakke G, Brown RL. Primary care practice adherence to National Cholesterol Education Program guidelines for patients with coronary heart disease. Arch Intern Med. 1998;158:1238–1244. doi: 10.1001/archinte.158.11.1238. [DOI] [PubMed] [Google Scholar]
- 20.Campbell NC, Thain J, Deans HG, Ritchie LD, Rawles JM. Secondary prevention in coronary heart disease: baseline survey of provision in general practice. Br Med J. 1998;316:1430–1434. doi: 10.1136/bmj.316.7142.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCormick D, Gurwitz JH, Lessard D, Yarzebski J, Gore JM, Goldberg RJ. Use of aspirin, beta-blockers, and lipid-lowering medications before recurrent acute myocardial infarction: missed opportunities for prevention? Arch Intern Med. 1999;159:561–567. doi: 10.1001/archinte.159.6.561. [DOI] [PubMed] [Google Scholar]
- 22.Xhignesse M, Laplante P, Grant AM, et al. Antiplatelet and lipid-lowering therapies for the secondary prevention of cardiovascular disease: are we doing enough? Can J Cardiol. 1999;15:185–189. [PubMed] [Google Scholar]
- 23.Sueta CA, Chowdhury M, Boccuzzi SJ, et al. Analysis of the degree of undertreatment of hyperlipidemia and congestive heart failure secondary to coronary artery disease. Am J Cardiol. 1999;83:1303–1307. doi: 10.1016/s0002-9149(99)00117-4. [DOI] [PubMed] [Google Scholar]
- 24.Miller M, Byington R, Hunninghake D, Pitt B, Furberg CD. Sex bias and underutilization of lipid-lowering therapy in patients with coronary artery disease at academic medical centers in the United States and Canada. Prospective Randomized Evaluation of the Vascular Effects of Norvasc Trial (PREVENT) Investigators. Arch Intern Med. 2000;160:343–347. doi: 10.1001/archinte.160.3.343. [DOI] [PubMed] [Google Scholar]
- 25.Lai LL, Poblet M, Bello C. Are patients with hyperlipidemia being treated? Investigation of cholesterol treatment practices in an HMO primary care setting. South Med J. 2000;93:283–286. [PubMed] [Google Scholar]
- 26.Primatesta P, Poulter NR. Lipid concentrations and the use of lipid lowering drugs: evidence from a national cross sectional survey. Br Med J. 2000;321:1322–1325. doi: 10.1136/bmj.321.7272.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Irving RJ, Oram SH, Boyd J, Rutledge P, McRae F, Bloomfield P. Ten year audit of secondary prevention in coronary bypass patients. Br Med J. 2000;321:22–23. doi: 10.1136/bmj.321.7252.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bittner V, Olson M, Kelsey SF, et al. Effect of coronary angiography on use of lipid-lowering agents in women: a report from the Women's Ischemia Syndrome Evaluation (WISE) study. Am J Cardiol. 2000;85:1083–1088. doi: 10.1016/s0002-9149(00)00700-1. [DOI] [PubMed] [Google Scholar]
- 29.Abookire SA, Karson AS, Fiskio J, Bates DW. Use and monitoring of ‘Statin’ lipid-lowering drugs compared with guidelines. Arch Intern Med. 2001;161:53–58. doi: 10.1001/archinte.161.1.53. [DOI] [PubMed] [Google Scholar]
- 30.EUROASPIRE I and II Group. Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries. Lancet. 2001;357:995–1001. doi: 10.1016/s0140-6736(00)04235-5. [DOI] [PubMed] [Google Scholar]
- 31.Yarzebski J, Spencer F, Goldberg RJ, Lessard D, Gore JM. Temporal trends (1986–97) in cholesterol level assessment and management practices in patients with acute myocardial infarction: a population-based perspective. Arch Intern Med. 2001;161:1521–1528. doi: 10.1001/archinte.161.12.1521. [DOI] [PubMed] [Google Scholar]
- 32.Roeback JR, Cook JR, Guess HA, Heyse JF. Time-dependent variability in repeated measurements of cholesterol levels: clinical implications for risk misclassification and intervention monitoring. J Clin Epidemiol. 1993;46:1159–1171. doi: 10.1016/0895-4356(93)90115-h. [DOI] [PubMed] [Google Scholar]
- 33.Verschuren WMM, van Leer EM, Blokstra A, et al. Cardiovascular disease risk factors in The Netherlands. Neth J Cardiol. 1993;6:205–210. [Google Scholar]
- 34.Jacobsen BK, Thelle DS. Risk factors for coronary heart disease and level of education. The Tromso Heart Study. Am J Epidemiol. 1988;127:923–932. doi: 10.1093/oxfordjournals.aje.a114895. [DOI] [PubMed] [Google Scholar]
- 35.Kraus JF, Borhani NO, Franti CE. Socioeconomic status, ethnicity, and risk of coronary heart disease. Am J Epidemiol. 1980;111:407–414. doi: 10.1093/oxfordjournals.aje.a112915. [DOI] [PubMed] [Google Scholar]
- 36.Anderson KM, Odell PM, Wilson PWF, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1990;121:293–298. doi: 10.1016/0002-8703(91)90861-b. [DOI] [PubMed] [Google Scholar]
- 37.Klungel OH, de Boer A, Paes AH, Nagelkerke NJ, Seidell JC, Bakker A. Estimating the prevalence of hypertension corrected for the effect of within-person variability in blood pressure. J Clin Epidemiol. 2000;53:1158–1163. doi: 10.1016/s0895-4356(00)00228-6. [DOI] [PubMed] [Google Scholar]
- 38.Mantel-Teeuwisse AK, Klungel OH, Verschuren WMM, Porsius AJ, de Boer A. Time trends in lipid lowering drug use in The Netherlands. Has the backlog of candidates for treatment been eliminated? Br J Clin Pharmacol. 2002;53:379–385. doi: 10.1046/j.1365-2125.2002.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klungel OH, de Boer A, Paes AH, Seidell JC, Bakker A. Cardiovascular diseases and risk factors in a population-based study in The Netherlands: agreement between questionnaire information and medical records. Neth J Med. 1999;55:177–183. doi: 10.1016/s0300-2977(99)00045-5. [DOI] [PubMed] [Google Scholar]
- 40.Klungel OH, de Boer A, Paes AH, Herings RM, Seidell JC, Bakker A. Agreement between self-reported antihypertensive drug use and pharmacy records in a population-based study in The Netherlands. Pharm World Sci. 1999;21:217–220. doi: 10.1023/a:1008741321384. [DOI] [PubMed] [Google Scholar]
- 41.Hoerger TJ, Bala MV, Bray JW, Wilcosky TC, LaRosa J. Treatment patterns and distribution of low-density lipoprotein cholesterol levels in treatment-eligible United States adults. Am J Cardiol. 1998;82:61–65. doi: 10.1016/s0002-9149(98)00227-6. [DOI] [PubMed] [Google Scholar]
- 42.Svilaas A, Risberg K, Thoresen M, Ose L. Lipid treatment goals achieved in patients treated with statin drugs in Norwegian general practice. Am J Cardiol. 2000;86:1250–1253. doi: 10.1016/s0002-9149(00)01212-1. [DOI] [PubMed] [Google Scholar]
- 43.Marcelino JJ, Feingold KR. Inadequate treatment with HMG-CoA reductase inhibitors by health care providers. Am J Med. 1996;100:605–610. doi: 10.1016/s0002-9343(96)00011-3. [DOI] [PubMed] [Google Scholar]
- 44.Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid- lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000;160:459–467. doi: 10.1001/archinte.160.4.459. [DOI] [PubMed] [Google Scholar]
- 45.Stoverinck MJ, Lagro-Janssen AL, Weel CV. Sex differences in health problems, diagnostic testing, and referral in primary care. J Fam Pract. 1996;43:567–576. [PubMed] [Google Scholar]
- 46.Nathanson CA. Sex, illness, and medical care. A review of data, theory, and method. Soc Sci Med. 1977;11:13–25. doi: 10.1016/0037-7856(77)90141-x. [DOI] [PubMed] [Google Scholar]