Abstract
There is a pressing need for medical graduates to be fully prepared to take on the responsibilities of prescribing and to be able to respond to continual inevitable rapid changes in therapeutics. The curricula in UK medical schools were greatly influenced by Tomorrow's Doctors, published by the General Medical Council in 1993. This has recently been updated. While it highlights the management of disease and use of drugs as key learning objectives, it offers little specific guidance. In this document we expand on these broad statements, provide a view of how these learning objectives might be achieved, and identify the key elements of a core curriculum in prescribing and therapeutics.
Keywords: clinical pharmacology and therapeutics; curriculum; education; General Medical Council, prescribing; undergraduate
Introduction
Prescribing is a major clinical activity of the National Health Service (NHS). Each member of the population now receives an average of 12 prescriptions per year. The cost of prescribing has grown progressively throughout its existence and now amounts to a total annual expenditure in excess of £7bn, about 13% of the total budget. For most doctors, drug therapy is the main tool that they have for influencing the health of their patients. While drugs can offer great benefits to patients, they can also cause great harm.
There are several important pressures on all NHS prescribers:
New drug developments, extending medicines into new areas.
Increasing complexity of medical care.
Increased specialization.
Increased use of medicines in both primary and secondary care.
More rapid throughput of patients.
Sicker and older patients, more vulnerable to adverse effects.
All of these strengthen the need for newly qualified doctors to have a firm grounding in the principles of safe, effective, and cost-effective prescribing.
Prescribing as a generic skill
Prescribing is the primary intervention that most doctors offer to influence their patients’ health – whatever career medical graduates decide to pursue, most will have to remain ‘specialists’ in drug prescribing. Prescribing is therefore an essential skill for doctors in most medical specialties. Most graduates will require not only a knowledge of today's drugs, but also a firm grounding in the principles of therapeutics, underpinned by a scientific knowledge of drug action, to inform their learning about future developments.
In addition, prescribing rights are now being extended to other health professionals, and doctors will increasingly need to be involved in training and in working collaboratively with these other prescribers.
With the power to bring great benefits comes the risk of causing great harm, as drugs can cause significant morbidity and mortality. Although newly qualified doctors are usually protected from the requirement to undertake high-risk practical procedures, they are often expected to prescribe powerful drugs from their first day of clinical work. This is a high-risk area of practice, and a major clinical governance issue for employers, who look to medical schools to ensure that their graduates have the necessary skills and knowledge for such work.
For all of these reasons, a firm grounding in the principles of prescribing and therapeutics, an understanding of how drugs work, and a basic knowledge about commonly used drugs are essential for all medical graduates. But a concern of a recent Audit Commission report [1] was that current undergraduate medical courses ‘do not provide a thorough knowledge of safe medicines prescribing and administration’ among junior doctors. There is a pressing need to improve the training of prescribers at all levels. Medical education in the UK has undergone significant changes over the last decade, in response to concerns over traditional methods of teaching and driven by recommendations from the General Medical Council (GMC). Now is an appropriate time to consider whether UK graduates are adequately prepared to prescribe.
Medical school curricula
Traditionally, UK medical schools ran a 2- or 3-year preclinical phase of ‘basic sciences’ as a foundation for 3 years of clinical training. In the 1960s, clinical pharmacology and therapeutics (CPT) emerged as a new discipline, and many schools incorporated CPT into curricula as a distinct course. Many medical schools provided courses in both basic pharmacology and CPT. However, there were problems with these general arrangements: an excessively high burden of factual information, an emphasis on basic science, which often excluded time for other patient-centred activities, poor co-ordination across courses, and an artificial divide between preclinical and clinical learning. There were also weaknesses in the learning process, with an excess of didactic lecture-based teaching rather than active problem-based learning.
The GMC document Tomorrow's Doctors in 1993 recommended changes to the structure and content of medical education [2], that the factual burden be reduced, and that integration be improved. The emphasis was on problem-based education and the development of skills for lifelong learning. Learning outcomes in the form of knowledge, skills, and attitudes were to be clarified.
Reasons for concern
For many schools, this prompted a radical redesign of the medical curriculum, one consequence of which was the loss of single-discipline courses, including basic pharmacology and CPT. Indeed, the guidance stated explicitly that it ‘avoided all reference to traditional subjects and disciplines… urging the advantages of interdisciplinarity’ (Para. 42). Although Tomorrow's Doctors did identify ‘the principles of therapy’, including ‘the actions of drugs, their prescription and their administration’ among its knowledge objectives [Para. 40.1(g)(ii)], there was no other mention of drugs or prescribing.
Now learning about CPT has devolved to system- or problem-based components of the curriculum. Although there are no objective data on how this has affected learning outcomes, in practice it is now harder to bring together the core principles of CPT that underpin good prescribing. These concerns have been raised by many, including medical students themselves [3, 4]. The diminished presence of CPT is ironic in that it remains one of the most ‘integrated’ of all clinical disciplines, its core principles applicable to almost all other areas of practice.
The GMC's own recommendations for early postgraduate medical education, The New Doctor[5], clearly identify the need for a sound education in therapeutics: ‘Practical skills frequently required by preregistration house officers … from the first day of the preregistration year … [and that] should not be undertaken without proper training … [include the ability to] calculate a drug dosage’, and ‘write a prescription’.
Tomorrow's Doctors 2002
The GMC has recently revised Tomorrow's Doctors[6], and its implications have been discussed at length elsewhere [7]. The new guidance provides more direction about teaching and assessment of therapeutics than before and specifically refers to effective and safe use of medicines as the basis of prescribing (item 16). The key guidance is that students must be adequately prepared to prescribe drugs when they graduate (item 52). It also addresses evaluation of effectiveness against evidence, the need to take account of patients’ views and beliefs, and the use of complementary and alternative therapies (item 18). Graduates must be able to go beyond a management plan, to work out drug dosages, and write safe prescriptions for different types of drugs (item 19). Importantly, they are expected to know how errors can happen in practice and to apply these principles to risk management (items 4 and 26). The need for a firm grounding in the principles of CPT and knowledge about common drugs is strengthened by the expectation that graduates will be able to provide enough information about conditions and possible treatments to help patients make informed decisions about their care (item 30).
These learning outcomes are now supported by clear recommendations on effective assessment. Medical schools must have valid and reliable schemes of assessment, to ensure that students have achieved the curricular outcomes (items 62–64).
An integrated core curriculum in clinical pharmacology and therapeutics
The 2002 revision of Tomorrow's Doctors does not support the re-emergence of CPT as a specific discipline, but the increasing emphasis on many learning outcomes at the heart of CPT is welcome, as well as the clear principle that all graduates must be demonstrably safe prescribers. While the specific details of this objective are not spelt out, we believe that it must involve most of the generic knowledge, skills, and attitudes suggested later in this paper, as well as specific knowledge about the drugs prescribed. The real challenge now for all medical schools is to deliver and assess these learning objectives within an integrated curriculum.
Previous recommendations about the content of CPT within the curriculum, in both the UK [8] and USA [9], remain valid and should be re-emphasized. There is now a need to re-interpret them in the context of the new curricula and in line with the latest GMC recommendations.
The purpose of the remainder of this document is:
to translate the general objectives related to CPT into more specific learning outcomes;
to prioritize the core learning objectives in CPT;
to identify the minimum knowledge that students should possess to prescribe safely and effectively at the time of graduation;
to indicate how these objectives can be achieved in an integrated medical curriculum;
to provide a template for quality assurance for those who review the undergraduate medical curriculum in UK medical schools;
to support the development of assessments of learning outcomes;
to highlight the importance of strong leadership in therapeutics in all medical schools, as the best way to ensure successful integration of the core content into the curriculum and the development of effective assessments;
to provide direction for curriculum developers, particularly where CPT specialists are absent.
Core learning objectives
The key objective is that graduates be competent to prescribe safely and effectively. In addition, they should be able to assimilate information about new drug developments throughout their professional career. These general objectives can be further refined into more specific outcomes, which can be divided into knowledge and understanding, skills, and attitudes, and form the core content of CPT within the curriculum (Appendix). Although this content is identified here as ‘CPT’, that specific label is not a prerequisite for the success of the learning outcomes. To keep these objectives clinically relevant, it is useful to link them to a number of specific drugs (perhaps the basis of a ‘student formulary’, see below) and therapeutic problems that provide relevant clinical examples of the principles of CPT. Each school will wish to develop its own lists and format, but an example of a core drug/therapeutic problem list can be found in a longer version of this paper [10]. Both lists have been set out in relation to the potential clinical modules in which those learning objectives are most likely to be met. This emphasizes the suitability of a problem-based approach to develop learning about CPT, and how CPT can be vertically integrated with most of the curriculum.
A ‘curriculum map’ should be given to the students, who will then be able to identify how the relevant learning objectives can be achieved. A sound knowledge of the basic principles of CPT should allow students to take a logical approach to learning about any of the drugs they encounter during the course, and should therefore be introduced at an early stage of the curriculum.
Core drugs and therapeutic problems: the Student Formulary
Medical students are often overwhelmed by the large number of drugs that they encounter during their clinical attachments. To tackle this, schools should create a list of drugs as the basis for a ‘student formulary’ that helps to prioritize learning. The list should comprise 80–100 commonly used drugs from both primary and secondary care settings, that are used to treat common illnesses and are representative of important drug classes. A newly qualified doctor might be expected to initiate or prescribe these drugs under the direction of a senior doctor. For each of the drugs or its class, students might be expected to:
know its name and class;
understand how it works;
recognize the appropriate indication for its use;
know how to prescribe it – how it is administered, the frequency of administration, the duration of administration;
know its important contraindications, potential drug interactions, and major adverse effects;
be able to name alternatives when available;
know how to monitor the drug's effects;
be able to explain salient features of all of these points to a patient.
Students need not be expected to know exact drug doses, except perhaps for a small number of emergency drugs, but should know where to find the information quickly and easily. The newly qualified prescriber should be expected and encouraged to look up doses before prescribing any drug.
The intention of the student formulary is to provide realistic and attainable learning objectives. A student who achieves these outcomes should be able to cope effectively and safely with most of the prescribing challenges that they are likely to face in their early postgraduate years, as well as establishing the key principles of good prescribing for the rest of their careers.
Delivering the curriculum
The structures of medical courses in the UK differ considerably. While some retain boundaries between preclinical and clinical, others have removed these barriers and have truly integrated curricula, often with an emphasis on problem-based learning. All of the CPT learning objectives can be achieved in either setting. This may be easier in discipline-based courses. In more integrated courses, the absence of protected time to focus on prescribing necessitates the co-ordination of CPT learning opportunities across many different modules and over several years. This task may present practical difficulties.
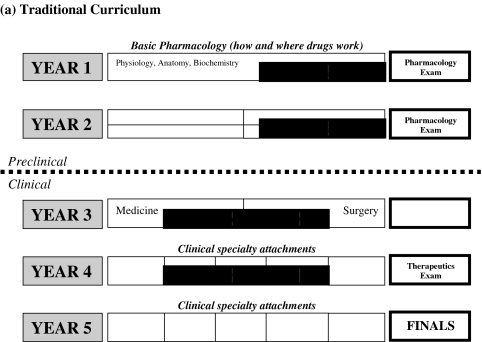
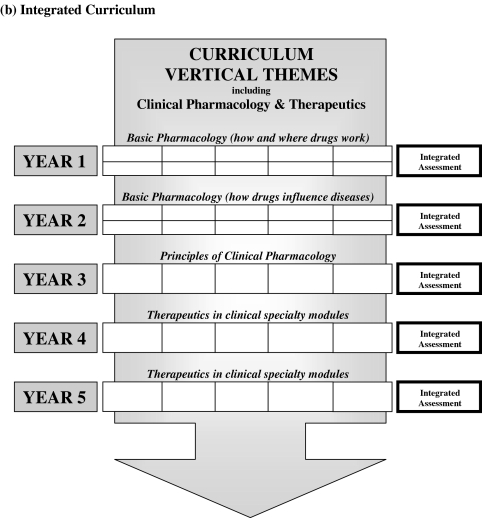
Whether in a traditional or an integrated curriculum (Figure 1), learning about drugs should be built up throughout the course – initially emphasizing understanding where and how drugs act, using core drugs as examples, and later emphasizing clinical aspects, such as when drugs are indicated and how they are prescribed. Curriculum developers might see an advantage in a module in the early years that highlights generic aspects of drug use. With these key principles established, much of the learning about drugs can be undertaken within system-based modules to provide both horizontal and vertical integration.
Figure 1.
Traditional and integrated patterns of delivery of clinical pharmacology and therapeutics in the undergraduate medical curriculum. (a) Traditional curriculum. (b) Integrated curriculum.
Leadership
A key factor in the successful implementation of the core curriculum will be clear leadership. Tomorrow's Doctors 2002 emphasizes the need to ‘involve individuals with an appropriate range of expertise and knowledge’ to ‘plan curricula and associated assessments, put them into practice and review them’ (item 42 [6]). All medical schools should be able to identify an individual to oversee this area of the curriculum. This role might ideally be undertaken by an individual with training and background in CPT. But the role is not their sole preserve and the key requirements are enthusiasm for ensuring that principles of CPT are prominent throughout the curriculum.
CPT learning opportunities may be devolved to many teachers across the course, often within organ-based specialties. They too should be encouraged to emphasize these principles and remind students about the effects of drugs beyond individual organ systems. Simply providing a link between drugs and clinical conditions is insufficient to develop an appreciation of the complex considerations that surround the decision to prescribe.
Teaching and learning styles
The range of modes of learning will vary in different schools according to local preference, but the key is increasingly inquisitive rather than passive learning. There should be an appropriate balance of teaching in large groups with that in small groups, practical classes and opportunities for self-directed learning. Although the didactic lecture still has a role in delivering a broad overview of individual topics, it is now only one of several approaches.
The core curriculum in CPT is ideally suited to take advantage of problem-based learning. Most prescribing episodes try to solve a clinical problem and require the appropriate knowledge, skills and attitudes outlined in the Appendix. Several schools have developed ‘therapeutic case discussions’ that offer students a case vignette and pose problems relating to prescribing and therapeutics. There are also several initiatives to develop case-based computer-assisted learning packages as aids to CPT learning and self-assessment.
Many opportunities for students to learn about drugs will arise during clinical attachments. Students should observe the process of prescribing from the perspective of other healthcare professionals (e.g. participate in a ward ‘drug round’). They might be asked to review drug sheets, make self-assessments about their knowledge about specific core drugs, look for potential drug interactions, and scrutinize prescriptions. Students should receive instruction in small groups about the practical aspects of writing a legal prescription.
Other styles of learning might involve writing case reports containing discussion about therapeutic aspects (e.g. portfolio cases), discussing prescribing decisions with patients as part of communicating skills, critically analysing clinical trials involving drugs, appraising claims about new drugs, and searching for information about drugs.
Assessment of the core curriculum
Assessment drives learning and consolidates the acquisition of core knowledge and skills. The recent GMC recommendations are clear. Safe and effective use of medicines is also a major factor in clinical governance and risk management within the NHS. For these reasons, a robust assessment of prescribing competence should be mandatory. Its presence should be verified by external examiners and when the GMC visits medical schools.
Students might also be provided with formative assessments and the chance for self-assessment at regular intervals during the medical course. Few schools now have a separate ‘CPT examination’. In an integrated curriculum, the learning process in CPT spans the course and involves the synthesis of numerous learning opportunities. It is therefore logical to reserve important summative assessments for later in the course, preferably the final year, when students can be expected to demonstrate expertise in many different areas of therapeutics (similar to real clinical life). The assessment should identify students who have poor knowledge about drugs and who will be inadequately prepared for the responsibility of prescribing.
Even within an integrated assessment scheme, there should be a clear, identifiable, and robust component devoted to the knowledge and skills that support the prescribing of drugs. Furthermore, it is inappropriate that any student should be able to compensate for a poor performance in prescribing or therapeutics with good performances in other assessments. The GMC guidance is unequivocal on the need for students to be competent prescribers when they graduate (item 52).
The mode of assessments may vary, but they should test the knowledge, skills, and attitudes that are identified in the core curriculum, in a manner that is relevant to early clinical practice. Although knowledge and understanding can be examined by essays and multiple-choice questions, assessments should increasingly focus on testing the acquisition of practical skills. These may be more adequately assessed in the format of an objective structured clinical examination (OSCE) [11].
Conclusion
Although guidance from the GMC has led to substantial improvements in the quality of education, it has posed challenges in ensuring that many learning outcomes, previously the responsibility of individual disciplines, are met within an integrated curriculum. Meeting this challenge in CPT assumes greater importance as the complexities of being a prescriber grow. The medical curriculum should offer all students a firm grounding in core knowledge and understanding about drugs, skills in prescribing, and attitudes towards the use of drugs. These principles should be applied to a limited and identifiable list of common drugs. Although specialists in CPT have an important role to play in leading this area of the curriculum, teachers from other backgrounds can also fulfil this role.
This document is intended as a support to those charged with overseeing the development of this area of the curriculum. The GMC indicates that ‘medical schools have a responsibility to the public, to employers and to the profession to make sure that graduates are fit to practice’ (item 84 [7]). Prescribing drugs is a key component of medical practice. All of tomorrow's doctors must be adequately prepared.
Principal recommendations
Prescribing and therapeutics should be identified as an important theme that runs vertically through the medical curriculum, integrating with and identifiable within relevant horizontal modules.
Core learning objectives should be clearly identified, including knowledge and understanding about drugs, skills related to the prescribing of drugs, and attitudes towards drug therapy.
The factual burden should be eased by prioritizing learning around a core list of commonly used drugs (a student formulary).
There should be identifiable and robust assessment that these learning objectives have been met. This might form part of an integrated assessment, but it should not be possible to compensate for a poor performance in this area by a good performance in other items.
Each medical school should identify an individual teacher to oversee this area of the curriculum and to ensure that the learning objectives set out within the core curriculum are met.
Acknowledgments
The authors would like to acknowledge the contribution of the many individuals who offered constructive comments about earlier versions of this manuscript. A longer version of this article is available on the BPS web site at http://www.bps.ac.uk[10].
Appendix: Core knowledge and understanding, skills and attitudes concerning the use of drugs for the medical curriculum
These should be key learning outcomes of the curriculum and are required by all graduates, to enable them to prescribe safely and effectively at the point of qualification. These core objectives are generic and applicable to most areas of therapeutics. They should be considered in association with a locally identified list of core drugs and therapeutic problems to which they apply. In each case their relevance to clinical practice should be illustrated with appropriate examples.
Core knowledge and understanding
Basic pharmacology
The general mechanisms of action of drugs at molecular, cellular, tissue, and organ level;
the ways in which these actions produce therapeutic and adverse effects;
the receptor as a target of drug action and related concepts such as agonism, antagonism, partial agonism, and selectivity;
the development of tolerance to drugs.
Clinical pharmacokinetics
The mechanisms of drug absorption, distribution, elimination (metabolism and excretion);
the concepts of volume of distribution, clearance, and half-life, and their clinical relevance;
how these factors determine the optimal route, dose, and frequency of drug administration.
Factors that determine interindividual variation in drug response
Pharmaceutical variation;
pharmacokinetic handling of drugs;
pharmacogenetic variation.
Monitoring drug therapy
The importance of monitoring the impact of drug therapy;
the ways in which this can be achieved (measuring clinical outcomes, pharmacodynamic responses, or plasma drug concentrations);
the variable relation between plasma drug concentration and drug effect.
Adverse drug reactions
Types and mechanisms of adverse drug reactions;
the frequency of adverse reactions in primary and secondary care;
recognition of the predisposing factors and how risks can be minimized;
the importance of reporting adverse reactions and the role of the yellow card scheme.
Drug interactions
The potential for drugs to interact to cause beneficial and harmful effects;
the mechanisms by which drugs interact (pharmacokinetic, pharmacodynamic);
the ways in which interactions can be predicted and avoided.
Medication errors
The common reasons medication errors occur in practice;
the ways in which individual prescribers can reduce the risks of medication errors.
Poisoned patients
Principles of treating the poisoned patient;
the assessment of poisoned patients;
the recognition and treatment of common presentations (e.g. paracetamol);
the principles of removing or counteracting the effects of toxic substances after ingestion.
Prescribing for patients with special requirements because of their altered physiology, pharmacokinetic handling, or pharmacodynamic responses, including
Elderly patients;
children;
women of child-bearing potential;
pregnant and breast-feeding women;
patients with renal disease;
patients with liver disease.
Legal aspects of prescribing drugs
Categorization of drugs as over-the-counter formulations (General Sales List and Pharmacy medicines), prescription-only medicines, and controlled drugs;
the prescribing of ‘unlicensed’ medicines or medicines ‘off label’;
the responsibilities associated with prescribing controlled drugs.
Developing new drugs
Drug development, including clinical trials (Phase I to Phase IV);
the approval process and major regulatory authorities in UK and Europe;
the requirements of good clinical trial design;
consent, ethics, bias, statistics, dissemination of information.
Medicines management
The role of local formularies;
the roles of drug and therapeutics committees;
the influences that affect individual prescribing choices;
the rational assessment of new drugs, based on safety, efficacy and cost-effectiveness.
Ethics of prescribing
Informed patient consent and concordance.
Commonly used drugs
The mechanism of action, the indications for use, the appropriate route of administration, and the important contraindications and adverse effects of a locally identified list of commonly used drugs (see for an example http://www.bps.ac.uk[10]).
Common therapeutic problems
The management of common acute and chronic therapeutic problems (see for an example http://www.bps.ac.uk[10]).
Complementary and alternative medicine
The motivations that lead patients to seek complementary and alternative therapies;
some common methods and appraisal of the evidence for their efficacy;
how such therapies can interact with prescription drugs that patients are receiving.
Core skills
Taking a drug history
Obtaining accurate information about current prescription and non-prescription drugs;
making an assessment of adherence to a medication regimen;
recording current and past adverse drug reactions, including allergies.
Prescription writing
Choosing a safe and effective drug and an appropriate dosage regimen;
writing accurate, legible, and legal prescriptions, including controlled drugs;
keeping accurate records of prescriptions and responses;
calculating drug doses;
calculating the strength of an infusion based on the required rate of drug administration;
prescribing oxygen (flow rate, delivery);
prescribing intravenous fluids.
Drug administration
Selecting the appropriate route of administration;
giving subcutaneous, intramuscular, and intravenous injections;
preparing drugs for parenteral administration, including mixing and dissolving drugs;
preparing and giving drugs by an infusion pump;
preparing and giving nebulized drugs;
advising patients about special modes of drug delivery, e.g. topical, inhaled, insulin.
Prescribing drugs in special groups
Elderly, children, pregnancy, breast-feeding, renal and hepatic failure.
Prescribing drugs to relieve pain and distress
Palliation of pain and other distressing symptoms.
Adverse drug reactions and interactions
Assessing drugs as possible causes of symptoms and signs;
recognizing the potential for adverse drug interactions;
reporting adverse drug reactions and interactions.
Drug allergy
Recognizing allergic drug reactions and taking a history of an allergic reaction;
treating allergic reactions, the emergency treatment of acute anaphylaxis.
Clinical pharmacokinetics
Using core knowledge of pharmacokinetics to inform safe prescribing.
Monitoring drug therapy
Identifying which therapeutic effect to observe;
using measurements of plasma drug concentrations appropriately (which and when);
acting appropriately on the results.
Analysing new evidence
Practising evidence-based prescribing;
assessing the validity of evidence about new drugs or therapies;
reading, assessing, and critically analysing clinical studies;
spotting methodological flaws, including sources of bias;
recognizing the difference between true and surrogate end-points.
Obtaining accurate objective information to support safe and effective prescribing
Using the British National Formulary;
accessing reliable drug information from medical journals and medical databases;
accessing Poisons Information Services;
discriminating between the reliability of varying sources of evidence and opinion.
Obtaining informed consent to treatment
Providing patients with enough information about drugs to allow them to make informed decisions about their treatment;
discussing benefits and risks of drug therapy with patients;
exploring patients’ own views and wishes in relation to drug treatment.
Core attitudes
A rational approach to prescribing and therapeutics
Identifying the correct diagnosis;
understanding the pathophysiological processes involved;
knowing the drugs that might beneficially influence these processes;
establishing the end-points with which to monitor the therapeutic response;
assessing the potential risks and benefits of treatment;
communicating with the patient in making the decision to treat.
Risk–benefit analysis
Recognizing that there are risks and benefits associated with all drug treatments;
recognizing that these may differ between patients, depending on a variety of factors;
recognizing that doctors should monitor the impact of the drugs they prescribe.
Recognizing the responsibilities of a doctor as part of the prescribing community
Avoidance of wasteful prescribing and consumption of limited resources;
recognizing the need to report adverse drug reactions for the common good;
controlling the availability of restricted drugs;
adhering to therapeutic guidelines and drug formularies, as appropriate;
avoiding indiscriminate antibiotic prescribing.
Recognizing personal limitations in knowledge
Recognizing the need to seek further information about drugs when faced with unfamiliar prescribing problems.
Responding to the future
Recognizing the need to update prescribing practices;
ensuring that patients benefit, when possible, from advances in medical knowledge;
recognizing the need to assess the benefits and hazards of new therapies;
knowing the limitations of applying clinical trial data to individual patients.
References
- 1.Audit Commission. A spoonful of sugar – improving medicines management in hospitals. Audit Commission; 2001. ( http://www.audit-commission.gov.uk/publications/spoonfulsugar.shtml) [Google Scholar]
- 2.General Medical Council. Tomorrow's doctors. London: General Medical Council; 1993. [Google Scholar]
- 3.Maxwell S, Walley T, Ferner RE. Using drugs safely: undergraduates must be proficient in basic prescribing. Br Med J. 2002;324:930–931. doi: 10.1136/bmj.324.7343.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ellis A. Prescribing rights: are medical students properly prepared for them? Br Med J. 2002;324:1591. [Google Scholar]
- 5.General Medical Council. The new doctor. London: General Medical Council; 1997. [Google Scholar]
- 6.General Medical Council. Tomorrow's doctors. London: General Medical Council; 2002. ( http://www.gmc-uk.org/med_ed/tomdoc.htm) [Google Scholar]
- 7.Webb DJ, Maxwell SRJ. A spoonful of sugar? Tomorrow's doctors 2002. Br J Clin Pharmacol. 2002;54:341–343. doi: 10.1046/j.1365-2125.2002.t01-1-01715.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walley T, Webb DJ. Core content for a course in clinical pharmacology. Br J Clin Pharmacol. 1997;44:171–174. doi: 10.1046/j.1365-2125.1997.00668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nierenberg DW and the Council for Medical Student Education In Clinical Pharmacology and Therapeutics. A core curriculum for medical students in clinical pharmacology and therapeutics. Clin Pharmacol Ther. 1990;48:606–610. doi: 10.1038/clpt.1990.201. [DOI] [PubMed] [Google Scholar]
- 10.Maxwell S, Walley T. doi: 10.1046/j.1365-2125.2003.01878.x. Teaching safe and effective prescribing in uk medical schools: a core curriculum for tomorrow's doctors (long version). http://www.bps.ac.uk/ [DOI] [PMC free article] [PubMed]
- 11.Langford NJ, Martin U, Kendall MJ, Ferner RE. Medical errors. Medical schools can teach safe drug prescribing and administration. Br Med J. 2001;322:1424. [PubMed] [Google Scholar]