Abstract
Self-poisoning by ingestion or inhalation is common, and it is important to study its various epidemiological manifestations with clear definitions. Data on fatal self-poisonings are recorded nationally within the UK and are codified according to the International Classification of Diseases (ICD) revision relevant at the time. Most fatal self-poisonings are codified as suicides, accidental deaths or undetermined deaths (‘open verdicts’). Non-fatal self-poisoning data, whether accidental or as a manifestation of deliberate self-harm, are recorded through hospital discharge information nationally but are not routinely published in the same way as mortality data. The bulk of the UK's published epidemiological information on nonfatal self-poisoning episodes is largely based on individual hospitals' admission or discharge records (‘special studies’). After establishing definitions for different self-poisoning categories we discuss the published data on self-poisoning as they relate to suicide, accidental self-poisoning and deliberate self-harm in the UK.
Keywords: epidemiology, overdose, self-poisoning, suicide, United Kingdom
Introduction
Self-poisoning is one of the commonest acute medical presentations in the UK. It is therefore not only important that clinical pharmacologists be aware of trends in the mortality and morbidity of self-poisoning, but also they be able to recognize the methodological limitations of the epidemiological data underlying them. One such limitation has been confusion over how various types of self-poisoning are described and subsequently registered. Three broad categories of self-poisoning (suicide, accidental self-poisoning and deliberate self-harm) will be defined in this review and the available information on them in the UK examined. Finally, paracetamol will be explored separately as an example bringing together issues from different self-poisoning categories.
Definitions
A self-poisoning episode may be defined as the self-exposure of an individual (by ingestion or inhalation) to an amount of substance associated with the significant potential to cause harm. Self-poisoning episodes may be accidental or deliberate, fatal or nonfatal.
Accidental self-poisoning may occur when an individual unintentionally experiences more of an effect from a substance than planned. This may be through a change in the individual's tolerance for the substance (e.g. a heroin addict going straight back to injecting at their ‘usual’ dose following an enforced ‘drug-free’ period in prison) or through a preparation containing more active substance than expected (e.g. an elderly person getting confused about a change in tablet strength of their regular medication). Alternatively, accidental self-poisonings may occur when an individual has no understanding at all of the significance of what they are exposing themselves to, as in the majority of paediatric self-poisonings.
Deliberate self-poisoning, when it is nonfatal, and particularly when it is grouped together with self-injury, is also called deliberate self-harm (DSH), attempted suicide or parasuicide, and the World Health Organization's definition of parasuicide in a recent international study was: ‘An act with nonfatal outcome, in which an individual deliberately initiates a nonhabitual behaviour that, without intervention from others, will cause self-harm, or deliberately ingests a substance in excess of the prescribed or generally recognized therapeutic dosage and which is aimed at realizing changes which the subject desired via the actual or expected physical consequences’[1].
If death occurs consequent to an episode of deliberate self-poisoning or self-harm then the diagnosis becomes one of suicide.
On the basis of the above definitions, in the absence of clear intent to self-harm, we would consider that overdoses following on from the recreational use of drugs should ideally be classified as accidental rather than deliberate self-poisonings. However, some individual hospital databases do not distinguish between overdoses secondary to recreational drug use and DSH (see below). Although, admittedly, there may be no toxicological difference between an agent taken accidentally or deliberately, we would argue that the different motivations behind the two acts necessitate incorporation into separate categories because of their potential to impact not only on the types, amounts and combinations of agents taken, but also on the risks of concomitant self-injury, self-discharge from hospital and repeat poisoning admissions.
Epidemiological information sources
The main sources of epidemiological data relating to self-poisoning in the UK are NHS hospital discharge records, death certification records (obviously fatal events only), and data from special surveys/studies. Complete hospital discharge and death certification data are available for the whole of the UK. The data are held according to confidentiality guidelines by the Departments of Health of the constituent countries (hospital discharge data), and the Office for National Statistics (England and Wales) and the General Register Offices for Scotland and Nor-thern Ireland (death data). UK mortality data are easily accessible through various government publications or government websites (e.g. http://www.statistics.gov.uk, http://www.show.scot.nhs.uk). Hospital discharge data, however, are not published nationally in the same way and direct contact with the relevant department of health would usually be required to gain access to this information.
Hospital discharge records provide information on the personal details of the patient (for example, age, sex, postcode of residence, and date of admission) and on their diagnosis and any procedures/operations carried out whilst they were in hospital. Death certification records provide information on the personal details of the deceased and on their cause of death.
Diagnosis and cause of death are coded according to the International Classification of Diseases (ICD) revision that was relevant at the time. ICD-9 was used in the UK from 1979 to 1999 with, for example, codes E950–E959 being used to divide completed suicide into various categories such as poisoning by solid or liquid substances, gassing or drowning. In addition, subcategories broadly distinguish between the means employed within each category (those relating to suicide by poisoning with solid or liquid substances are detailed in Table 1). With regard to self-poisoning, further information on the agents involved in particular cases, beyond those of such ICD subcategories, may be presented in studies if it has been extracted from death certificates, coroner's or Procurator Fiscal's reports, police reports, doctor's reports or medical notes.
Table 1. The ICD-9 subcategories E950.0–E950.9 for suicide by self-poisoning using solid or liquid substances.
| * | E950.0 Analgesics, antipyretics, and antirheumatics |
| * | E950.1 Barbiturates |
| * | E950.2 Other sedatives and hypnotics |
| * | E950.3 Tranquillizers and other psychotropic agents |
| * | E950.4 Other specified drugs and medicinal substances |
| * | E950.5 Unspecified drug or medicinal substance |
| * | E950.6 Agricultural and horticultural chemical and pharmaceutical preparations other than plant foods and fertilizers |
| * | E950.7 Corrosive and caustic substances |
| * | E950.8 Arsenic and its compounds |
| * | E950.9 Other and unspecified solid and liquid substances |
Since January 2000, ICD-10 has been adopted in the UK for mortality and morbidity recording. When an ICD revision change occurs considerable effort goes into what is called bridge coding, whereby for a few years records are coded in the two revisions concurrently and analysed to check for spurious jumps in incidence. In this way comparability factors may be produced and any potentially confounding effects of the ICD revision change can be estimated.
When looking at event coding it is important to realize that multiple codes can be used for one record, for example, allowing coding of the event as accidental, deliberate, or ‘undetermined’ poisoning (see below for explanation of ‘undetermined’) alongside more detailed coding of the agent used. This is particularly true with regard to the dependent and nondependent abuse of drugs (and is explained further in the section on accidental self-poisonings below).
Since 1968, ‘deaths undetermined whether deliberate or accidental’– also called open or undetermined verdicts – have been included among the ICD codes. Whenever there is insufficient evidence to support a verdict of either homicidal or accidental death by means such as poisoning, UK coroners are advised that to record a verdict of suicide there has to be evidence of suicidal intent ‘beyond reasonable doubt’, and that when this is not the case an open verdict should be returned [2]. Such verdicts are reflected in the national statistics by, for example the ICD-9 codes E980–E980.9 for undetermined deaths involving self-poisoning by solid or liquid substances (covering the same broad categories of drug used in describing suicide mentioned previously). ‘Undetermined’ ICD codes similarly exist for nonfatal events, including self-poisoning, to be used whenever it remains unclear whether an individual's actions were deliberate or not.
Whether such undetermined events should be excluded from epidemiological studies of suicide and deliberate self-poisoning, included en masse, or whether other evidence should be examined to categorize each event as possibly/probably deliberate rather than impossible/unlikely to be deliberate (e.g. an undetermined death in a neonate is unlikely to be suicide) is an area of some debate at present [3]. Care needs to be taken, therefore, when assessing epidemiological information relating to deliberate self-poisoning/suicide to ascertain whether events of undetermined intent have been included or excluded from the dataset.
Repeated hospital admission for deliberate self-harm is one issue that can only properly be studied using routine hospital discharge data in Scotland, and not in the other constituent UK countries. The reason for this is that it is only in Scotland that all hospital discharge records (since 1981) relating to particular individuals are electronically linked together on the national database. This means that in Scotland the chance of re-admission can be quantified, and for any given time period the actual number of different people admitted with deliberate self-harm, in addition to the total number of admission episodes, can be assessed.
The completeness and accuracy of ICD coding of hospital discharge and death data in the UK are generally good and certainly of sufficient standard to make the data useful in terms of monitoring trends in the epidemiology of self-poisoning. Mortality data are often analysed in this way but, as has already been stated, as the data on hospital discharges are less freely available than for deaths, the majority of information published on nonfatal self-poisoning episodes in the UK at present tends to arise from individual institutions collating and analysing their own databases. Although data from these special surveys/studies cannot provide the national picture that would be available from using UK-wide hospital discharge and death data, they can sometimes provide a more detailed picture of, for example, the risk factors for, exact nature of, and sequelae of self-poisoning. In addition, they have the potential to provide the only means of examining nonfatal self-poisonings that do not result in hospital admission.
The most significant UK example of a special study on deliberate self harm is the Oxford Monitoring System for Attempted Suicide which has covered DSH referrals to the John Radcliffe Hospital for nearly 30 years [4]. To illustrate the point on the potential vagaries of special studies, however, it is interesting to note that, for example, this prominent database does not routinely collect information on paediatric cases (those < 15 years of age) and that to be included on it no proof of intent to self-harm is required. One consequence of this latter point is that while recreational drug use overdoses would be excluded from the DSH numbers in a special study coming from, for example, King's College Hospital, London [5], they would routinely be included in the numbers coming out of a special study from Oxford.
Self-poisoning in the UK – suicide
In Scotland 200 males and 94 females poisoned themselves to death (predominantly by ingesting drugs or gassing themselves) under both open and suicide verdict categories in the year 2000 (source: http://www.show.scot.nhs.uk). In England and Wales, the numbers were 1271 and 662, respectively, in 1999 (source: http://www.statistics.gov.uk). Given that the ratio of the populations of England and Wales to Scotland is approximately 10 : 1 (source: http://www.statistics.gov.uk), it is important to note that there are clear geographical differences in the self-poisoning suicide rates around the UK.
In the UK the overall suicide rate has been falling since the 1960s [6–8]. This broad picture does not apply to all sections of society however, for in one notable group – young males, aged 15–24 – the rate has been increasing in recent years [7–9].
With regard to self-poisoning, the methods used for suicide have changed considerably over time, largely as a result of their availability. Self-poisoning by gassing with domestic coal gas was the single most popular method employed by both males and females for suicide in the 1950s [10]. Following changes to decrease the carbon monoxide content of coal gas, and eventually its complete abolition, the suicide rate by this popular method fell so dramatically that a significant amount of the overall UK's decline in suicide rates has been attributed to it [6, 10, 11].
Self-poisoning varies as a mode of suicide between the sexes. In a small Newcastle-based study looking at the local coroners’ suicide verdicts the most popular methods of suicide for males of all ages between 1985 and 1994 were hanging> gassing (car exhausts)> self-poisoning with ingestible agents [11]. In females they were self-poisoning with ingestible agents>> jumping from high places> other violent methods, illustrating the consistent gender preferences that exist between males for violent and females for nonviolent methods of suicide.
Temporally, suicide by self-poisoning with drugs in England and Wales increased in the late 1950s/early 1960s in all age groups and for both genders [10]. Although partly attributable to ‘method substitution’ following the detoxification of domestic gas supplies, the increases began before gas supplies changed. The general increase in availability of drugs of all kinds and specifically the increase in potentially lethal drugs, notably barbiturates, are both likely to have contributed to the upturn. Overdoses peaked as the most popular method of suicide for both genders and all age groups in the 1970s, with the exception of men over the age of 55 who marginally preferred hanging [10].
When suicide and open verdicts in England and Wales are considered together, the most recent figures suggest that self-poisoning (including gassing) is used by 26.6% of the population that kill themselves [12]. Interestingly, since self-poisoning as a method of suicide is used more than twice as commonly by women (46.8% of women that commit suicide) than by men (19.5% of men that commit suicide), what the overall UK population figure of 26.6% also shows is just how much the predominance of males among those who commit suicide can bias combined-sex figures.
Suicide by self-poisoning is more common in the young. In the Oxford Regional Health Authority for those committing suicide under the age of 25, the figures for self-poisoning are 41.9% and 65.4% for males and females, respectively [13]. In terms of self-poisoning, approximately twice as many of these males preferred gassing to taking an overdose, whereas five times as many of the females preferred overdosing to gassing [13]. Approximately 45% of all suicides under the age of 25 in this study had a previous history of deliberate self-harm, confirming the impression of a direct link between DSH and suicide later in life [14]. The most popular drug used for suicidal overdoses by both young males and females was coproxamol (37.1%), and notably 37.6% of young suicides had consumed alcohol shortly before their death [13].
Certain professions seem to avoid suicide by self-poisoning (it is used by only 8% of farmers, for example) [15], while other professions seem to embrace it. Self-poisoning by drugs is used by 57% of doctors who kill themselves, with the preference extending across males and females, those who are working and those who have retired [12]. Specialist medical knowledge appears to be relevant with, for example, 50% of anaesthetists committing suicide by using anaesthetic drugs, and general practitioners using opiates and barbiturates at frequencies far higher than those found in the general suicide population.
The other notable UK group that seem to prefer self-poisoning with drugs as a method of suicide are drug addicts. The Dangerous Drugs Act 1968 established the UK Addicts Index on which all new drug addicts (covering 13 opiates and cocaine) must be registered. This index has been cross-referenced with suicide and open verdicts in the UK for the period between 1968 and 1992 [16]. For clear suicide verdicts 45% of all registered addicts used overdoses of drugs as their preferred method. Between 1968 and 1972 90% of these drug overdose suicides involved barbiturates. Barbiturates became controlled drugs in 1985 and their availability as a method of committing suicide significantly decreased. This appears to be reflected in the data for suicide in addicts between 1988 and 1992 when 23.5% used methadone and 23.5% used antidepressants to end their lives. With regard to open verdicts on addicts, 67% involved drug overdose as the cause of death, with opiates being the commonest drug type throughout the entire time period studied. The differences observed between the drugs used in overdose resulting in suicide vs. open verdicts raise the problem of how difficult it is to ascribe deliberate, accidental or unknown motives to a group of people who habitually run the risk of overdosing on lethal compounds for potentially very different reasons to the general public (see below).
Self-poisoning in the UK – accidental
The number of deaths in England and Wales during 1999 attributable to accidental self-poisoning was 749 males and 280 females (source: http://www.statistics.gov.uk). Approximately 50% of these deaths involved opiates. The majority of published epidemiological information on accidental self-poisoning pertains to drug abusers and drug addicts. Little published information beyond the anecdotal exists with regard to accidental paediatric self-poisoning in the UK.
In Oxford from 1985 to 1997 the percentage of self-poisonings involving opiates and ‘drugs for kicks’ rose from 0.7 to 3.6%, although whether these were accidental or deliberate self-poisonings is unknown [17]. Specific drugs involved in accidental overdoses have shown a less steady rise with time. For example, St George's Hospital in London has recorded data on deaths due to volatile solvent inhalations (‘glue-sniffing’) and shown that these peaked in 1990 and then fell coincident with a public health campaign [18].
In a study of accidental deaths among teenagers in England and Wales between 1985 and 1995, 436 teenagers died from accidental drug overdoses [19]. The male to female ratio was almost 3 : 1 and 21% of the accidental drug deaths were due to opiates. When deaths registered as accidental or undetermined opiate-related deaths and also deaths registered as involving opiate-dependent drug use were analysed for the UK, the death rate as a percentage of all deaths increased from 0.02% in 1985 to 0.12% in 1995 [20]. The average age of these deaths was 28 and 50% of the deaths involved methadone. Deaths ‘registered as involving opiate-dependent drug use’ might include those occurring in association with drug-related criminal or social violence, and this additional way of codifying deaths in national statistics for drug users is another area in which self-poisonings can ‘hide’.
The mortality rate for UK drug abusers on the addicts index is 10 times that of the general population [21], and for teenager drug abusers it is 12 times higher [22]. To give an idea of the scale of the problem of accidental death in drug addicts, in one study of 48 drug-related deaths in 15–19-year-old addicts, 45 of these were considered accidental overdoses and only three were considered suicides [22].
Self-poisoning in the UK – deliberate self-harm
National hospital discharge data for Scotland reveal that the rates of deliberate self-poisoning appear to be among the highest in Europe (379.3/100 000 per year for women and 331.5/100 000 per year for men over 1990–1999) [40]. Over the same 10-year period discharges were most frequent among those aged 15–24 years, with annual average rates rising to 805.5/100 000 per year for young women and 601.8/100 000 per year for young men [40].
The Oxford database suggests that 87.9% of DSH cases involve self-poisoning, 8.3% self-injury and 3.8% both self-poisoning and self-injury [23]. Over a 10-year period in Oxford there has been an increase in the rates per 100 000 population of both episodes and persons involved in DSH, particularly among males aged 15–24 [17, 23]. These upward trends have been confirmed elsewhere in the UK [24–26, 40]. The national data for Scotland with regard to paracetamol, antidepressants and opiods is shown in Figure 1[40].
Figure 1.
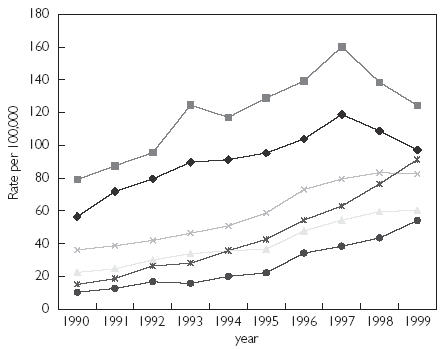
Trends in overdose discharges for paracetamol, antidepressants and opioid overdose and misuse in Scotland by gender (figure reproduced from [40] with permission from the authors and the editorial board of the Quarterly Journal of Medicine). Paracetamol m ( ); paracetamol f (
); paracetamol f ( ); antidepressants m (
); antidepressants m ( ); antipepressants f (
); antipepressants f ( ); opioid misuse and poisoning m (
); opioid misuse and poisoning m ( ); and opioid misuse and poisoning f (•).
); and opioid misuse and poisoning f (•).
To move from observing such trends to ascribing causalities is difficult. For example, although DSH can be correlated with measures of socio-economic deprivation [27], there is no evidence to suggest that socio-economic deprivation has altered over the same time scale to account for the changes. Small ‘blips’ in self-poisoning and in the agents used have been noted following representations of overdoses in the media [28], but no sustained patterns have been observed and the most recent study in question has been heavily criticized for over-interpreting what may have been normal fluctuations in weekly DSH rates [29–31].
How much hospital presentation data (admissions or discharges) represent only the ‘tip of the iceberg’ is unknown, but it is likely that substantial numbers of unrecorded self-poisonings occur in the community [32]. Whether there has been any redistribution of episodes from the community to the hospital to contribute to the apparent rise in DSH rates in the UK is similarly not known.
Self-poisoning episodes presenting to the hospital in Oxford involve a single category of drug on 37.1% of occasions and more than one category of drug on 62.9% of occasions [17]. Similar mean numbers of substances taken by self-poisoners have been noted in South-East London [5]. Women, younger people and persons engaged in their first episode of DSH are more likely to take overdoses involving more than one drug than are men, older people or repeat DSH offenders, respectively [17].
The primary clinical toxicology database for the UK National Poisons Information Service, Toxbase, is accessible to over 3000 UK accident & emergency departments, general practitioners, medicines information/pharmacies and NHS Direct (a government-run telephone advice service for health issues). To give an idea of the agents ingested for self-poisoning in the UK, the 10 most frequently accessed Toxbase products for the year 2000 are shown in Table 2.
Table 2. The 10 most common enquiries to Toxbase during 2000, with frequencies expressed as ratios to that of paracetamol (source: Scottish Poisons Information Bureau).
| 1 | Paracetamol | 1.000 |
| 2 | Diazepam | 0.299 |
| 3 | Aspirin | 0.278 |
| 4 | Ibuprofen | 0.262 |
| 5 | Zopiclone | 0.250 |
| 6 | Ecstasy | 0.232 |
| 7 | Amitriptyline | 0.201 |
| 8 | Dothiepin | 0.199 |
| 9 | Temazepam | 0.176 |
| 10 | Coproxamol | 0.171 |
In Oxford, DSH patients who did not get assessed by the psychiatric services had over twice the risk of re-presenting with an episode of DSH within a year compared with those who were assessed (37.5% vs. 18.2%) [33]. Whether this apparent impact of psychiatric assessment on the rate of re-presentation represents a genuine phenomenon or simply an association between, for example, uncooperative and repeat DSH behaviour at present remains unclear. Certainly antisocial personality disorder is one factor that has been previously associated with an increased risk of repetition of self-harm. Other factors associated with repeated DSH attempts include alcohol or substance dependency, psychiatric history and severe physical illness. A more detailed discussion of the risk factors for self-poisoning and for repeated self-poisoning is beyond the scope of this review, but an excellent educational article on the subject has recently been published for those with an interest in these aspects of the field [41].
Approximately 1% of people successfully commit suicide within one year of an episode of DSH [41].
Self-poisoning in the UK – the case of paracetamol
Using the Oxford data as a basis from which to extrapolate, a crude estimate of the annual number of paracetamol overdoses in England and Wales has been made at 41 200 [34]. For the UK as a whole this figure may be closer to 70 000 [35].
On 16 September 1998 the UK introduced legislation limiting the amount of paracetamol, salicylates and their compounds that could be bought in a single purchase. For paracetamol the limit was 16 g in pharmacies (except under special circumstances) and 8 g in nonpharmacies. In addition, blister-packs rather than bottles for containing the tablets became mandatory in almost all situations. Since existing domestic supplies would take some time to be used up, it was expected that there would be a delay in any impact of the legislation.
The first reports of a potentially beneficial effect were published in 2000. Median monthly referral rates to the Freeman Liver Unit in Newcastle and to the UK Transplant Special Support Authority for liver transplantation following paracetamol-induced hepatotoxicity fell from 2.5 to 1 and 3.5 to 2, respectively, after September 1998 compared with the 3 years beforehand [36]. In addition, at the Royal Free Hospital in London 12 monthly paracetamol-related overdose figures fell by 21% (and by 64% for ‘severe’ overdoses) after September 1998 compared with the preceding 3 years [37].
On a national scale, Scotland has reported that hospital discharges for paracetamol self-poisoning fell for both men and women from a peak in 1997, but this fall predated the changes [40]. Figures published in 2001 do confirm that the number of ‘UK’ deaths attributable to paracetamol overdose have recently decreased by 21% [38], but Scotland and Ireland were not included in the dataset on which these national mortality figures were presented (even though it was labelled as a ‘UK’ study). Intriguingly, the Scottish Liver Transplantation Unit have so far published the only study showing no change in paracetamol-induced liver failure referrals after the introduction of restrictive legislation [39].
Summary
Self-poisoning may be analysed by regarding data collected nationally on deaths or hospital discharges or through published special studies based largely on individual hospitals’ databases. It is important to note, particularly with special studies, that different studies may include or exclude different categories within their definitions of ‘DSH’ and ‘suicide’. Accidental overdoses are presumed to be behind the majority of paediatric overdoses and overdoses in drug addicts. Both deliberate self-harm and suicides are increasing in the youngest age groups (over the age of 15) in the UK and particularly in males. Psychiatric assessment of DSH patients may reduce the rate of subsequent representation. Gassing has fluctuated over time as a method of suicidal self-poisoning but drug overdose remains the preferred choice in most females, in the young, in drug addicts and in the medical profession. Paracetamol is the most commonly taken drug by young people committing DSH, whereas coproxamol appears to be more commonly taken by the same age group successfully completing suicide. Legislation restricting the availability of paracetamol may have influenced both the number and severity of paracetamol overdoses in the UK, but certain inconsistencies in changes in outcomes across the UK mean that it is probably still too early to judge fully the long-term effects of this intervention.
References
- 1.Kerkhof AJFM, Schmidtke A, Bille-Brahe U, et al., editors. Attempted suicide in Europe: findings from the Multicentre Study on Parasuicide by the WHO Regional Office for Europe. Leiden: DSWO Press; 1994. [Google Scholar]
- 2.Mathews P, Foreman J. Jervis on Coroners. 11. London: Sweet and Maxwell; 1993. [Google Scholar]
- 3.Linsley KR, Schapira K, Kelly TP. Open verdict v. suicide – importance to research. Br J Psychiatry. 2001;178:465–468. doi: 10.1192/bjp.178.5.465. [DOI] [PubMed] [Google Scholar]
- 4.Hawton K, Fagg J. Trends in deliberate self-poisoning and self-injury in Oxford, 1976–1990. BMJ. 1992;304:1409–1411. doi: 10.1136/bmj.304.6839.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neeleman J, Wessely S. Drugs taken in fatal and non-fatal self-poisoning: a study in South London. Acta Pysychiatr Scand. 1997;95:283–287. doi: 10.1111/j.1600-0447.1997.tb09633.x. [DOI] [PubMed] [Google Scholar]
- 6.Kreitman N. The coal gas story. United Kingdom suicide rates 1960–71. Br J Preventative Social Medicine. 1976;30:86–93. doi: 10.1136/jech.30.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charlton J, Kelly S, Dunnell K, et al. Trends in suicide deaths in England and Wales. Population Trends. 1992;69:10–16. [PubMed] [Google Scholar]
- 8.McClure GM. Changes in suicide in England & Wales 1960–97. Br J Psychiatry. 2000;176:64–67. doi: 10.1192/bjp.176.1.64. [DOI] [PubMed] [Google Scholar]
- 9.McClure GM. Suicide in children and adolescents in England and Wales, 1970–1998. Br J Psychiatry. 2001;178:469–474. doi: 10.1192/bjp.178.5.469. [DOI] [PubMed] [Google Scholar]
- 10.Gunnell D, Middleton N, Frankel S. Method availability and the prevention of suicide – a re-analysis of secular trends in England and Wales 1950–75. Soc Psychiatry Psychiatr Epidemiol. 2000;35:437–443. doi: 10.1007/s001270050261. [DOI] [PubMed] [Google Scholar]
- 11.Schapira K, Linsley KR, Linsley JA, et al. Relationship of suicide rates to social factors and availability of lethal methods. Br J Psychiatry. 2001;178:458–464. doi: 10.1192/bjp.178.5.458. [DOI] [PubMed] [Google Scholar]
- 12.Hawton K, Clements A, Simkins S, et al. Doctors who kill themselves: a study of the methods used for suicide. Q J Med. 2000;93:351–357. doi: 10.1093/qjmed/93.6.351. [DOI] [PubMed] [Google Scholar]
- 13.Hawton K, Houston K, Shepperd R. Suicide in young people. Br J Psychiatry. 1999;175:271–276. doi: 10.1192/bjp.175.3.271. [DOI] [PubMed] [Google Scholar]
- 14.Kreitman N. Can suicide and parasuicide be prevented? J R Soc Med. 1989;82:648–652. doi: 10.1177/014107688908201106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hawton K, Fagg J, Simkin S, et al. Methods used for suicide by farmers in England and Wales. Br J Psychiatry. 1998;173:320–324. doi: 10.1192/bjp.173.4.320. [DOI] [PubMed] [Google Scholar]
- 16.Oyefesu A, Ghodse H, Clancy C, et al. Suicide among drug addicts in the UK. Br J Psychiatry. 1999;175:277–282. doi: 10.1192/bjp.175.3.277. [DOI] [PubMed] [Google Scholar]
- 17.Townsend E, Hawton K, Harriss L, et al. Substances used in deliberate self-poisoning: trends and associations with age, gender, repetition and suicide intent, 1985–1997. Soc Psychiatry Psychiatr Epidemiol. 2001;36:228–234. doi: 10.1007/s001270170053. [DOI] [PubMed] [Google Scholar]
- 18.Bland JM, Taylor J. Deaths from accidental drug poisoning in teenagers. BMJ. 1998;316:146. (letter) [PMC free article] [PubMed] [Google Scholar]
- 19.Roberts I, Barker M, Li L. Analysis of trends in deaths from accidental drug poisoning in teenagers, 1985–1995. BMJ. 1997;315:289. doi: 10.1136/bmj.315.7103.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall W, Lynskey M, Degenhardt L. Trends in opiate-related deaths in the United Kingdom and Australia, 1985–1995. Drug Alcohol Dependence. 2000;57:247–254. doi: 10.1016/s0376-8716(99)00057-5. [DOI] [PubMed] [Google Scholar]
- 21.Ghodse AH, Sheehan M, Taylor C, et al. Deaths of drug addicts in the United Kingdom, 1967–1981. BMJ. 1985;290:425–428. doi: 10.1136/bmj.290.6466.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oyefesu A, Ghodse H, Clancy C, et al. Drug abuse-related mortality: a study of teenage addicts over a 20-year period. Soc Psychiatry Psychiatr Epidemiol. 1999;34:437–441. doi: 10.1007/s001270050166. [DOI] [PubMed] [Google Scholar]
- 23.Hawton K, Fagg J, Simkin S, et al. Trends in deliberate self-harm in Oxford, 1985–1995. Br J Psychiatry. 1997;171:556–560. doi: 10.1192/bjp.171.6.556. [DOI] [PubMed] [Google Scholar]
- 24.McEvedy CJB. Trends in self-poisoning: admissions to a central London teaching hospital, 1991–1994. J R Soc Med. 1997;90:496–498. doi: 10.1177/014107689709000908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLoonie P, Crombie IK. Hospitalisation for deliberate self-poisoning in Scotland from 1981 to 1993: trends in rates and types of drugs used. Br J Psychiatry. 1996;169:81–86. doi: 10.1192/bjp.169.1.81. [DOI] [PubMed] [Google Scholar]
- 26.Bialas M, Reid PG, Beck JH, et al. Changing patterns in self-poisoning in a UK health district. Q J Med. 1996;89:893–901. doi: 10.1093/qjmed/89.12.893. [DOI] [PubMed] [Google Scholar]
- 27.Hawton K, Harriss L, Hodder K, et al. The influence of the economic and social environment on deliberate self-harm and suicide: an ecological and person-based study. Psychol Med. 2001;31:827–836. doi: 10.1017/s0033291701003993. [DOI] [PubMed] [Google Scholar]
- 28.Hawton K, Simkin S, Deeks JJ, et al. Effects of a drug overdose in a television drama on presentations to hospital for self-poisoning: time series and questionnaire study. BMJ. 1999;318:972–977. doi: 10.1136/bmj.318.7189.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Veysey MJ, Kamanyire R, Volans GN. Antifreeze poisonings give more insight into copycat behaviour. BMJ. 1999;319:1131. (letter) [PMC free article] [PubMed] [Google Scholar]
- 30.Pell J, Murdoch R. A causal association cannot yet be inferred. BMJ. 1999;319:1131. (letter) [PubMed] [Google Scholar]
- 31.Davies SJC, Atherton M, Williams T, et al. Study is impressive but raises methodological concerns. BMJ. 1999;319:1131–1132. (letter) [PubMed] [Google Scholar]
- 32.Kennedy PF, Kreitman N. An epidemiological survey of parasuicide (‘attempted suicide’) in general practice. Br J Psychiatry. 1973;123:43–44. doi: 10.1192/bjp.123.1.23. [DOI] [PubMed] [Google Scholar]
- 33.Hickey L, Hawton K, Fagg J, et al. Deliberate self-harm patients who leave the accident and emergency department without a psychiatric assessment – a neglected population at risk of suicide. J Psychosomatic Res. 2001;50:87–93. doi: 10.1016/s0022-3999(00)00225-7. [DOI] [PubMed] [Google Scholar]
- 34.Gunnell D, Hawton K, Murray V, et al. Use of paracetamol for suicide and non-fatal poisoning in the UK and France: are restrictions on availability justified? J Epidemiol Community Health. 1997;51:175–179. doi: 10.1136/jech.51.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fagan E, Wannan G. Reducing paracetamol overdoses. BMJ. 1996;313:1417–1418. doi: 10.1136/bmj.313.7070.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prince MI, Thomas SHL, James OFW, et al. Reduction in the incidence of severe paracetamol poisoning. Lancet. 2000;355:2047–2048. doi: 10.1016/S0140-6736(00)02354-0. [DOI] [PubMed] [Google Scholar]
- 37.Turvill JL, Burroughs AK, Moore KP. Change in occurrence of paracetamol overdose in UK after introduction of blister packs. Lancet. 2000;355:2048–2049. [PubMed] [Google Scholar]
- 38.Hawton K, Townsend E, Deeks J, et al. Effects of legislation restricting pack sizes of paracetamol and salicylate on self poisoning in the United Kingdom: before and after study. BMJ. 2001;322:1203–1207. doi: 10.1136/bmj.322.7296.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Newsome PN, Bathgate AJ, Henderson NC, et al. Referral patterns and social deprivation in paracetamol-induced liver injury in Scotland. Lancet. 2001;358:1612–1613. doi: 10.1016/S0140-6736(01)06663-6. [DOI] [PubMed] [Google Scholar]
- 40.Bateman DN, Bain M, Gorman D, et al. Changes in paracetamol, antidepressants and opioid poisoning in Scotland during the 1990s. QJM. 2003;96:1–8. doi: 10.1093/qjmed/hcg015. [DOI] [PubMed] [Google Scholar]
- 41.Horrocks J, House A. Self-poisoning and self-injury in adults. Clin Med. 2002;2:509–512. doi: 10.7861/clinmedicine.2-6-509. [DOI] [PMC free article] [PubMed] [Google Scholar]


