Abstract
Aims
The relationship between β2-adrenoceptor polymorphisms at positions 16 and 27, and the acute systemic β2-adrenoceptor effects of inhaled salbutamol is unclear. We therefore elected to evaluate the influence of common homozygous β2-adrenoceptor haplotypes on the acute systemic β2-adrenoceptor effects following inhaled salbutamol in asthmatic subjects.
Methods
An initial database search of 531 asthmatic subjects identified the two commonest homozygous haplotypes at positions 16 and 27 to be Arg16-Gln27 (12%) and Gly16-Glu27 (19%). After a 1-week washout period where all β2-adrenoceptor agonists were withdrawn, 16 Caucasian subjects (Arg16-Gln27: n = 8 and Gly16-Glu27: n = 8) were given a single dose of inhaled salbutamol (1200 µg), followed by serial blood sampling for serum potassium, along with measurements of diastolic blood pressure and heart rate, at 5-min intervals for 20 min.
Results
The two groups were well matched for age, sex, FEV1, and inhaled corticosteroid dose. Baseline values for serum potassium, diastolic blood pressure and heart rate were not significantly different comparing Arg16-Gln27 vs Gly16-Glu27. The mean ± SEM maximum serum potassium change from baseline over 20 min was significantly greater (P = 0.04) for Arg16-Gln27: −0.37 ± 0.05 mmol l−1 vs Gly16-Glu27: −0.23 ± 0.04 mmol l−1; 95% CI for difference: −0.01 to −0.28 mmol l−1. The maximum diastolic blood pressure change from baseline over 20 min was significantly greater (P = 0.0008) for Arg16-Gln27: −13 ± 1 mmHg vs Gly16-Glu27: −4 ± 2 mmHg; 95% CI for difference: −5, 14 mmHg. There was no significant difference comparing the maximum heart rate change from baseline for Arg16-Gln27: 10 ± 3 beats min−1 vs Gly16-Glu27: 10 ± 3 beats min−1.
Conclusions
Caucasian asthmatic subjects with the Arg16-Gln27 haplotype exhibited a greater systemic response to inhaled salbutamol, compared with those with the Gly16-Glu27 haplotype. The attenuated β2-adrenoceptor response in the Gly16-Glu27 haplotype would be in keeping with increased susceptibility to prior down-regulation by endogenous catecholamines.
Keywords: asthma, β2-adrenoceptor haplotype, β2-adrenoceptor polymorphism, diastolic blood pressure, heart rate, salbutamol
Introduction
In vitro studies in transfected cell lines have shown that β2-adrenoceptor mediated responses are determined by polymorphisms at positions 16 and 27, in terms of the propensity for agonist-induced down-regulation and associated subsensitivity of response [1, 2]. According to Liggett, the dynamic model of receptor kinetics would predict that endogenous catecholamines would promote down-regulation of receptors expressing the homozygous glycine genotype at position 16 (Gly-16), such that the subsequent acute response to an exogenous β2-adrenoceptor agonist would be diminished [3]. Conversely, the homozygous arginine genotype at position 16 (Arg-16) would be relatively resistant to down-regulation by endogenous catecholamines, such that the subsequent response to an exogenous β2-adrenoceptor agonist would be relatively greater, as compared with the homozygous Gly16 genotype. According to the dynamic model, at position 27, the homozygous glutamic acid (Glu-27) genotype confers relative resistance to down-regulation by endogenous catecholamines, with the homozygous glutamine (Gln-27) genotype being relatively sensitive to down-regulation.
However, the response in vivo is determined by the occurrence of complex haplotypes comprising combinations of genotypes at 16, 27 and other positions [4]. In a previous retrospective genotype study in asthmatic subjects [5], we reported on the ex vivo response to acute maximal isoprenaline stimulation on peripheral blood lymphocyte β2-adrenoceptor cyclic adenosine monophosphate response, which showed no difference between homozygous genotypes at positions 16 or 27, although the various haplotype combinations were not evaluated as such. In the same study, we observed no difference in the acute protection afforded by inhaled formoterol against functional antagonism conferred by methacholine bronchial challenge.
Inhaled salbutamol exhibits dose-related systemic adverse effects mediated by extrapulmonary β2-adrenoceptors, including hypokalaemia due to stimulation of skeletal muscle β2-adrenoceptors, and a fall in diastolic blood pressure due to peripheral arteriolar vasodilatation [6, 7]. In addition, chronotropic effects may occur due to direct stimulation of cardiac β1- or β2-adrenoceptors, along with effects due to reflex vagal withdrawal.
The purpose of the present study was to evaluate the influence of the two most common homozygous β2-adrenoceptor haplotypes on the acute systemic β2-adrenoceptor effects following a single dose of inhaled salbutamol in asthmatic subjects, who had been washed out of previous exogenous β2-adrenoceptor agonist exposure.
Methods
An initial exploratory analysis was performed on our asthma database to evaluate the prevalence of homozygous haplotypes within our subject population. We found from a sample of 531 subjects that the homozygous Gly16-Glu27 haplotype was the most prevalent at 19% followed by homozygous Arg16-Gln27 at 12% with the least prevalent homozygous haplotype being Gly16-Gln27 at 5%. There were no subjects with the homozygous Arg16-Glu27 as expected due to linkage disequilibrium between genotypes at positions 16 and 27 [8]. Sixteen subjects were then selected with the two commonest homozygous haplotypes, namely Arg16-Gln27 and Gly16-Glu27. Eligible subjects were required to have a history of persistent asthma [9] receiving inhaled corticosteroid therapy, without recent exacerbation requiring either oral corticosteroids or antibiotics within the past 6 months. All subjects gave informed consent and the study was approved by the Tayside Committee on Medical Research Ethics.
Subjects were required to undergo a 1-week washout period where all short- and long-acting β2-adrenoceptor agonists such as salbutamol (Arg16-Gln27: n = 8, and Gly16-Glu27: n = 8) and salmeterol (Arg16-Gln27: n = 1, and Gly16-Glu27: n = 3) were stopped, while continuing with their usual inhaled corticosteroids. Subjects were given ipratropium bromide 20 µg (Atrovent®, Boehringer Ingelheim Ltd, Bracknell, UK) two puffs as required, for use instead as rescue therapy in order to obviate any exogenous β2-adrenoceptor agonist exposure. After an initial 30 min of supine resting to achieve a stable baseline, subjects were given under supervision, six consecutive puffs of salbutamol 200 µg (Ventolin Accuhaler®, Allen and Hanburys Ltd, Uxbridge, UK), followed by serial blood sampling for serum potassium, along with measurements of supine diastolic blood pressure and heart rate using an automated vital signs monitor (Dynamap®, Critikon Inc, Tampa, USA) with an appropriate sized cuff, at 5-min intervals for 20 min.
Statistical analysis
The maximum change from baseline over 20 min for serum potassium was the primary outcome measure used to power the study at 80%, in order to detect a 50% difference between haplotypes. Secondary outcome measures included the maximum change from baseline for diastolic blood pressure and heart rate. Comparisons were made by two-way analysis of variance with a two-tailed α-error of 0.05 using Statgraphics® statistical software package (STSC Software Publishing Group, Rockville, USA).
Results
Sixteen Caucasian subjects were enrolled and all completed the study per protocol. Eight subjects (three males and five females) with mean ± SEM age of 42 ± 6 years and FEV1 of 85 ± 4% predicted had the Arg16-Gln27 haplotype, and eight subjects (three males and five females) with mean age of 41 ± 4 years and FEV1 of 82 ± 6% predicted had the Gly16-Glu27 haplotype. The mean daily dose of inhaled corticosteroid was 400 ± 80 µg and 444 ± 108 µg for subjects with the Arg16-Gln-27 and Gly-16-Glu27 genotypes, respectively.
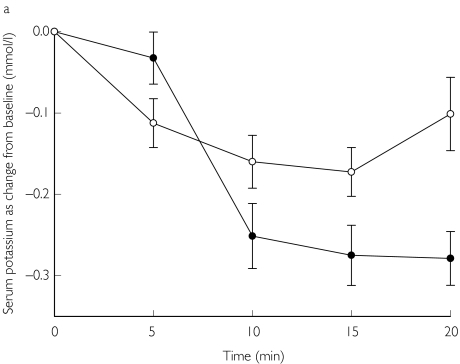
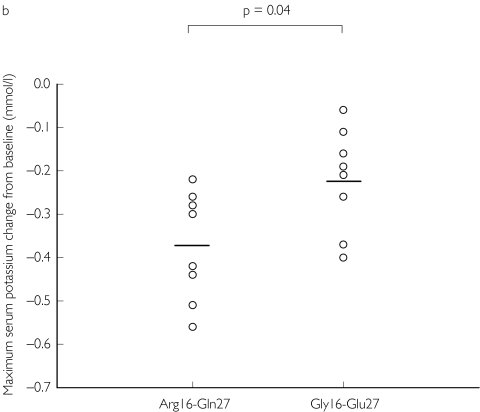
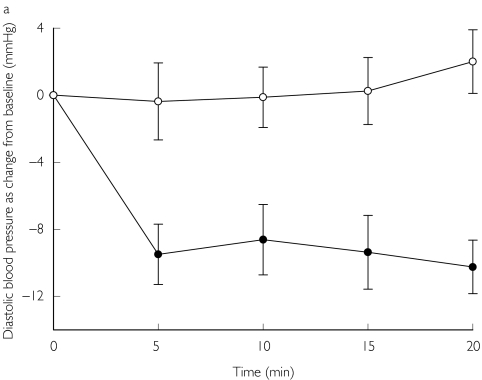
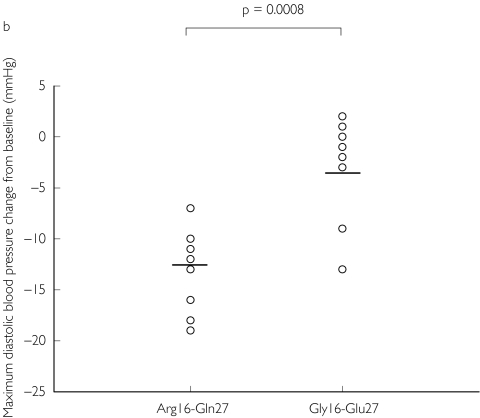
Baseline values for serum potassium were not significantly different comparing Arg16-Gln27 vs Gly16-Glu27: 4.00 ± 0.04 mmol l−1vs 3.90 ± 0.07 mmol l−1. The maximum serum potassium change from baseline over 20 min (Figure 1) was significantly greater (P = 0.04) for Arg16-Gln27: −0.37 ± 0.05 mmol l−1vs Gly16-Glu27: −0.23 ± 0.04 mmol l−1; 95% CI for difference: −0.01, −0.28. Baseline values for diastolic blood pressure and heart rate were not significantly different comparing Arg16-Gln27 vs Gly16-Glu27: 73 ± 6 mmHg vs 72 ± 5 mmHg and 71 ± 4 beats min−1vs 67 ± 5 beats min−1, respectively. The maximum diastolic blood pressure change from baseline over 20 min (Figure 2) was significantly greater (P = 0.0008) for Arg16-Gln-27: −13 ± 1 mmHg vs Gly16-Glu27: −4 ± 2 mmHg; 95% CI for difference: −5, −14. There was no significant difference comparing the maximum heart rate change from baseline for Arg16-Gln27: 10 ± 3 beats min−1vs Gly16-Glu27: 10 ± 3 beats min−1.
Figure 1.
a)Time profile for the serum potassium as change from baseline, with SEM Arg16-Gln27 (•) and Gly16-Glu27 (○). b) individual data for the maximum potassium change from baseline over 20 min, with mean values depicted as horizontal lines.
Figure 2.
a) Time profile for the diastolic blood pressure as change from baseline, with SEM Arg16-Gln27 (•) and Gly16-Glu27 (○). b) individual data for the maximum diastolic blood pressure change from baseline over 20 min, with mean values depicted as horizontal lines.
Discussion
The present results showed that Caucasian asthmatic subjects expressing the homozygous Arg16-Gln27 haplotype had a greater acute response to inhaled salbutamol than those with the Gly16-Glu27 haplotype. Our findings lend support to the dynamic model of receptor kinetics proposed by Liggett [3], which postulated that endogenous catecholamines may prior down-regulate β2-adrenoceptors in their basal state to a relatively greater degree in subjects with the Gly-16 genotype compared with the Arg-16 genotype. Thus, the acute response to a subsequent exogenous β2-adrenoceptor agonist such as salbutamol would be more apparent in Arg-16 subjects, as their receptors have not yet been down-regulated to the same degree as subjects with the Gly-16 genotype. Our data are in keeping with previous findings in Caucasian healthy subjects where a systemic infusion of salbutamol produced a greater systemic vasodilator response in the homozygous Arg-16 genotype compared with the homozygous Gly-16 genotype [10]. However, in contrast to our findings, in another study of Caucasian healthy subjects, the forearm blood flow venodilator response to isoprenaline was blunted in the homozygous Arg-16 genotype compared with the homozygous Gly-16 genotype [11]. It was also shown in the same study that there was relative blunting of the isoprenaline vasodilator response in the homozygous Gln-27 genotype compared with the homozygous Glu-27 genotype [11]. However, neither study evaluated haplotype combinations at positions 16 and 27 together.
We were extra vigilant to ensure that our subjects were not exposed to any short- or long-acting β2-adrenoceptor agonists for a 1-week washout period prior to the study day, with ipratropium bromide being used as sole rescue therapy instead throughout that period. The purpose of this washout period was to ensure that any effects on basal β2-adrenoceptor expression were due merely to endogenous catecholamines, prior to administration of the single test dose of salbutamol. Furthermore, we have previously shown that a period of 1 week would have been sufficient to washout the effects of long-acting β2-adrenoceptor agonists [12, 13].
In vitro data would point to the Glu-27 genotype conferring relative resistance from catecholamine-induced down-regulation and the Gln-27 genotype conferring relative susceptibility to down-regulation [1, 2]. However, at the same time, it appears that the susceptibility of the Gly-16 genotype predominates over the resistance due to the Glu-27 genotype, while the Arg-16 genotype predominates over the Gln-27 genotype. In an in vivo study in healthy subjects, homozygous haplotype 16/27 combinations were compared in terms of a dorsal hand vein infusion of isoprenaline, while measuring the acute venodilator response [14]. This showed that it was the presence of the homozygous Arg16-Gln27 haplotype that conferred susceptibility to agonist-induced subsensitivity of response, compared with the homozygous Gly16-Glu27 or Gly16-Gln27 haplotypes, indicating the dominant influence of the Arg-16 genotype over the Gln-27 genotype. We did not evaluate the Gly16-Gln27 haplotype in our study as we only found a prevalence of 5% in our asthma database.
We were interested in pure β2-mediated responses and as such chose not to evaluate effects on the systolic blood pressure which is more mediated by cardiac β1-adrenoceptors, while diastolic blood pressure is mediated only by peripheral arteriolar β2-adrenoceptors [15, 16]. We did not see any difference in chronotropic response between the haplotypes. This may be explained by the relative loss of β2-adrenoceptor selectivity at high doses of salbutamol [17, 18], such that stimulation of cardiac β1-adrenoceptors also occurred. Moreover, as reflex vagal withdrawal may contribute to the chronotropic response, this may have overcome any subtle differences in cardiac β2-adrenoceptor stimulation between the haplotypes. Our subjects were also well matched for age, sex, FEV1 and inhaled corticosteroid dose, especially as the latter may modulate β2-adrenoceptor down-regulation and subsensitivity [19, 20]. Our study did not evaluate subsensitivity during chronic dosing of salbutamol, but only the acute response to a single dose. However, one might predict that the greater response to a single dose of salbutamol in the Arg16-Gln27 haplotype in the present study might also be associated with enhanced subsensitivity during chronic dosing, as shown by Dishy et al. with isoprenaline-induced venodilatation [14]. Further prospective studies with salbutamol are indicated to explore this hypothesis comparing single and chronic dosing responses in these haplotypes in asthmatic subjects. Moreover, with the increasing use of the vasodilator response to salbutamol in assessing vascular endothelial function, our results may have considerable implications for research in this area [21, 22].
In conclusion, subjects with the Arg16-Gln27 haplotype exhibited a greater response to the acute systemic β2-adrenoceptor effects of inhaled salbutamol, compared with subjects with the Gly16-Glu27 haplotype, which in turn would suggest a greater susceptibility of the latter haplotype to prior down-regulation by endogenous catecholamines. Individuals with the Arg16-Gln27 haplotype may be at greater risk of developing β2-adrenoceptor mediated systemic adverse effects in response to high dose salbutamol.
References
- 1.Green SA, Cole G, Jacinto M, Innis M, Liggett SB. A polymorphism of the human beta2-adrenergic receptor within the fourth transmembrane domain alters ligand binding and functional properties of the receptor. J Biol Chem. 1993;268:23116–23121. [PubMed] [Google Scholar]
- 2.Green SA, Turki J, Bejarano P, Hall IP, Liggett SB. Influence of beta2-adrenergic receptor genotypes on signal transduction in human airway smooth muscle cells. Am J Respir Cell Mol Biol. 1995;13:25–33. doi: 10.1165/ajrcmb.13.1.7598936. [DOI] [PubMed] [Google Scholar]
- 3.Liggett SB. The pharmacogenetics of beta2-adrenergic receptors: relevance to asthma. J Allergy Clin Immunol. 2000;105:S487–S492. doi: 10.1016/s0091-6749(00)90048-4. [DOI] [PubMed] [Google Scholar]
- 4.Drysdale CM, McGraw DW, Stack CB, Stephens JC, Judson RS, Nandabalan K, et al. Complex promoter and coding region beta2-adrenergic receptor haplotypes alter receptor expression and predict in vivo responsiveness. Proc Natl Acad Sci U S A. 2000;97:10483–10488. doi: 10.1073/pnas.97.19.10483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipworth BJ, Hall IP, Tan S, Aziz I, Coutie W. Effects of genetic polymorphism on ex vivo and in vivo function of beta2-adrenoceptors in asthmatic patients. Chest. 1999;115:324–328. doi: 10.1378/chest.115.2.324. [DOI] [PubMed] [Google Scholar]
- 6.Lipworth BJ, McDevitt DG. Beta-adrenoceptor responses to inhaled salbutamol in normal subjects. Eur J Clin Pharmacol. 1989;36:239–245. doi: 10.1007/BF00558154. [DOI] [PubMed] [Google Scholar]
- 7.Lipworth BJ, Clark RA, Dhillon DP, Brown RA, McDevitt DG. β-adrenoceptor responses to high doses of inhaled salbutamol in patients with bronchial asthma. Br J Clin Pharmacol. 1988;26:527–533. doi: 10.1111/j.1365-2125.1988.tb05292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dewar JC, Wheatley AP, Venn A, Morrison JF, Britton J, Hall IP. Beta2-adrenoceptor polymorphisms are in linkage disequilibrium, but are not associated with asthma in an adult population. Clin Exp Allergy. 1998;28:442–448. doi: 10.1046/j.1365-2222.1998.00245.x. [DOI] [PubMed] [Google Scholar]
- 9.National Asthma Education and Prevention Program. Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma Update on Selected Topics – 2002. J Allergy Clin Immunol. 2002;110:S141–S219. [PubMed] [Google Scholar]
- 10.Gratze G, Fortin J, Labugger R, Binder A, Kotanko P, Timmermann B, et al. Beta2 adrenergic receptor variants affect resting blood pressure and agonist-induced vasodilation in young adult Caucasians. Hypertension. 1999;33:1425–1430. doi: 10.1161/01.hyp.33.6.1425. [DOI] [PubMed] [Google Scholar]
- 11.Cockcroft JR, Gazis AG, Cross DJ, Wheatley A, Dewar J, Hall IP, et al. Beta2-adrenoceptor polymorphism determines vascular reactivity in humans. Hypertension. 2000;36:371–375. doi: 10.1161/01.hyp.36.3.371. [DOI] [PubMed] [Google Scholar]
- 12.Aziz I, Hall IP, McFarlane LC, Lipworth BJ. Beta2-adrenoceptor regulation and bronchodilator sensitivity after regular treatment with formoterol in subjects with stable asthma. J Allergy Clin Immunol. 1998;101:337–341. doi: 10.1016/S0091-6749(98)70245-3. [DOI] [PubMed] [Google Scholar]
- 13.Aziz I, McFarlane LC, Lipworth BJ. Comparative trough effects of formoterol and salmeterol on lymphocyte beta2-adrenoceptor – regulation and bronchodilatation. Eur J Clin Pharmacol. 1999;55:431–436. doi: 10.1007/s002280050652. [DOI] [PubMed] [Google Scholar]
- 14.Dishy V, Sofowora GG, Xie HG, Kim RB, Byrne DW, Stein CM, et al. The effect of common polymorphisms of the beta2-adrenergic receptor on agonist-mediated vascular desensitization. N Engl J Med. 2001;345:1030–1035. doi: 10.1056/NEJMoa010819. [DOI] [PubMed] [Google Scholar]
- 15.Lipworth BJ, Irvine NA, McDevitt DG. A dose-ranging study to evaluate the beta1-adrenoceptor selectivity of bisoprolol. Eur J Clin Pharmacol. 1991;40:135–139. doi: 10.1007/BF00280067. [DOI] [PubMed] [Google Scholar]
- 16.Lipworth BJ, Tregaskis BF, McDevitt DG. Comparison of hypokalaemic, electrocardiographic and haemodynamic responses to inhaled isoprenaline and salbutamol in young and elderly subjects. Eur J Clin Pharmacol. 1991;40:255–260. doi: 10.1007/BF00315205. [DOI] [PubMed] [Google Scholar]
- 17.Lipworth BJ, Brown RA, McDevitt DG. Assessment of airways, tremor and chronotropic responses to inhaled salbutamol in the quantification of β2-adrenoceptor blockade. Br J Clin Pharmacol. 1989;28:95–102. doi: 10.1111/j.1365-2125.1989.tb03510.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newnham DM, Wheeldon NM, Lipworth BJ, McDevitt DG. Single dosing comparison of the relative cardiac beta1/beta2 activity of inhaled fenoterol and salbutamol in normal subjects. Thorax. 1993;48:656–658. doi: 10.1136/thx.48.6.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aziz I, McFarlane LC, Lipworth BJ. Concomitant inhaled corticosteroid resensitises cardiac beta2-adrenoceptors in the presence of long-acting beta2-agonist therapy. Eur J Clin Pharmacol. 1998;54:377–381. doi: 10.1007/s002280050478. [DOI] [PubMed] [Google Scholar]
- 20.Aziz I, Lipworth BJ. A bolus of inhaled budesonide rapidly reverses airway subsensitivity and beta2-adrenoceptor down-regulation after regular inhaled formoterol. Chest. 1999;115:623–628. doi: 10.1378/chest.115.3.623. [DOI] [PubMed] [Google Scholar]
- 21.Chowienczyk PJ, Kelly RP, MacCallum H, Millasseau SC, Andersson TL, Gosling RG, et al. Photoplethysmographic assessment of pulse wave reflection: blunted response to endothelium-dependent beta2-adrenergic vasodilation in type II diabetes mellitus. J Am Coll Cardiol. 1999;34:2007–2014. doi: 10.1016/s0735-1097(99)00441-6. [DOI] [PubMed] [Google Scholar]
- 22.Wilkinson IB, Hall IR, MacCallum H, Mackenzie IS, McEniery CM, van der Arend BJ, et al. Pulse-wave analysis: clinical evaluation of a noninvasive, widely applicable method for assessing endothelial function. Arterioscler Thromb Vasc Biol. 2002;22:147–152. doi: 10.1161/hq0102.101770. [DOI] [PubMed] [Google Scholar]