Abstract
Aims
To describe alprazolam poisoning and the relative toxicity of alprazolam compared with other benzodiazepines.
Methods
A database of consecutive poisoning admissions to a regional toxicology service was searched to identify consecutive benzodiazepine deliberate self poisonings, which were coded as alprazolam, diazepam or other benzodiazepine. Major outcomes used were length of stay (LOS), intensive care (ICU) admission, coma (GCS < 9), flumazenil administration and requirement for mechanical ventilation. Prescription data were obtained for benzodiazepines for the study period.
Results
There were 2063 single benzodiazepine overdose admissions: 131 alprazolam overdoses, 823 diazepam overdoses and 1109 other benzodiazepine overdoses. The median LOS for alprazolam overdoses was 19 h which was 1.27 (95% CI 1.04, 1.54) times longer compared with other benzodiazepines by multiple linear regression. For patients with alprazolam overdoses, 22% were admitted to ICU which was 2.06 (95% CI 1.27, 3.33) times more likely compared with other benzodiazepines after multivariate analysis adjusting for age, dose, gender, time to ingestion and co-ingested drugs. Flumazenil was administered to 14% of alprazolam patients and 16% were ventilated, which was significantly more than for other benzodiazepine overdoses (8% and 11%, respectively). Twelve percent of alprazolam overdoses had a GCS < 9 compared with 10% for other benzodiazepines. From benzodiazepine prescription data, total alprazolam prescriptions in Australia increased from 0.13 million in 1992 to 0.41 million in 2001. Eighty five percent of prescriptions were for panic disorder, anxiety, depression or mixed anxiety/depression.
Conclusions
Alprazolam was significantly more toxic than other benzodiazepines. The increased prescription of alprazolam to groups with an increased risk of deliberate self poisoning is concerning and needs review.
Keywords: alprazolam, benzodiazepines, overdose, toxicity
Introduction
Alprazolam (Xanax®, Kalma®) is a triazolobenzodiazepine used in panic disorder and other anxiety states [1, 2]. Benzodiazepines are commonly used for deliberate self poisoning and are implicated in approximately one third of cases of deliberate self poisoning [3]. Alprazolam is a newer benzodiazepine that is being used more commonly in overdose. MEDLINE was searched from 1966 to 2002 and no previous series of alprazolam poisonings were found. Fourteen case reports have been published including five reported deaths, two in which alprazolam was ingested alone [4–10]. This is potentially significant because benzodiazepine overdose is often thought to be benign.
A review of the Annual Reports of the American Association of Poison Control Centers National Data Collection System showed alprazolam was involved in 34 fatal deliberate self poisonings over 10 years 1992–2001 compared with 30 fatal deliberate self poisonings involving diazepam [11–20]. This suggests significant alprazolam toxicity if prescribing practices in the United States (US) mirror Australian trends where diazepam is prescribed at 5–10 times the rate of alprazolam. In a British study the fatal toxicity index (deaths per million prescriptions) for alprazolam was 5.9 compared with 4.0 for diazepam [21]. More recently a study from New Zealand showed that the rate of deaths per million prescriptions for alprazolam was 38.1 (10.4–97.5) compared with 5.3 (3.9–7.0) for sedatives/anxiolytics as a group [22]. These data suggest that alprazolam is potentially more toxic in overdose than other benzodiazepines.
We hypothesize that alprazolam causes greater toxicity in overdose compared with other benzodiazepines. We therefore report a series of alprazolam poisonings and compare this with other benzodiazepine poisonings to investigate whether alprazolam is more toxic. In addition we report the prescribing patterns of alprazolam and other benzodiazepines in Australia.
Methods
Hunter Area Toxicology Service database
The Hunter Area Toxicology Service is a regional toxicology unit situated at the Newcastle Mater Misericordiae Hospital that services a population of about 350 000 people and is a tertiary referral centre for a further 150 000 [23]. All poisoning presentations to emergency departments in the region are either admitted to the unit or notified to the Hunter Area Toxicology Service and entered prospectively into a clinical database. A validated preformatted admission sheet is used by medical staff to record the history and physical examination at the time of admission [24]. This and additional information from the medical record is entered into the database by two trained personnel, blinded to any study hypotheses, at the time of patient discharge [25]. There was no review or further information retrieved from medical records after formulation of the research question.
Study population
The study population included all benzodiazepine overdose admissions between January 1987 and October 2002 that were a result of a deliberate self poisoning. Cases where patients had ingested two benzodiazepines were excluded so that only single benzodiazepine overdoses were used in the analysis. If a patient had multiple admissions for a benzodiazepine overdose only the first admission was included. Second and subsequent admissions were excluded to remove the bias of an individual susceptibility to a particular drug. Each benzodiazepine overdose admission was then coded by benzodiazepine type: alprazolam, diazepam or other benzodiazepine (bromazepam, clobazam, flunitrazepam, lorazepam, nitrazepam, oxazepam, temazepam and triazolam).
Data analyzed
From the database, the following information was obtained: patient demography (gender, age), details of alprazolam ingestion (time elapsed from ingestion to admission; estimation of amount ingested in defined daily doses [DDD]; co-ingested drugs); clinical features (including Glasgow coma score [GCS]), outcomes (length of stay [LOS] and intensive care unit [ICU] admission rate) and treatment (mechanical ventilation and flumazenil administration). Coma was defined as a GCS < 9. The DDD of alprazolam is 1 mg and of diazepam is 10 mg. For co-ingestant analysis ‘nontricyclic antidepressants’ included fluoxetine, paroxetine, fluvoxamine, sertraline, citalopram, venlafaxine, moclobemide, mirtazapine and nefazodone.
ICU admission criteria for patients presenting to the Hunter Area Toxicology Service are: mechanically ventilated or intubated patients, patients with a decreased level of consciousness (GCS < 9); patients requiring haemodynamic monitoring or circulatory support or who have other major organ dysfunction requiring dedicated nursing observation. The Hunter Area Toxicology Service has a standardized discharge policy requiring review by both the medical toxicology team and the psychiatry team.
Prescription data
Prescription data for Australia were obtained from the Health Insurance Commission for the years 1992–2002 (data not available prior to 1992). This contains the total number of prescriptions for each drug supplied under the Pharmaceutical Benefits Scheme. The number of prescriptions of all formulations for each benzodiazepine was obtained. The validity of using nationwide statistics for comparisons between drugs taken in the Hunter region has previously been established [26]. Data on the actual indications for the prescription of benzodiazepines was obtained from the Health Communication Network's Copernicus Knowledge System. This represents a cross section of indications provided by Australian general practitioners via an electronic prescribing system for the period July 2002 to September 2002. It reflects the actual indication for the prescription rather those recommended in the product information.
Statistical analysis
Five outcome variables (LOS, ICU admission rate, GCS < 9, flumazenil administration and requirement for mechanical ventilation) were used for comparison of toxicity of alprazolam with other benzodiazepines. The following potential predictor variables were included in univariate and multivariate analysis: benzodiazepine type (alprazolam, diazepam or other benzodiazepine), patient age (years), gender, benzodiazepine dose (converted to DDD), time from ingestion to hospital presentation and binary predictors for co-ingestion of tricyclic antidepressants (TCA), antipsychotics, non-TCA antidepressants, anticonvulsants, opiates, alcohol and paracetamol. To evaluate the relative toxicity of alprazolam the reference was taken as all other benzodiazepines (excluding diazepam). Diazepam was also compared with other benzodiazepines independently because it is the most commonly ingested, creating a categorical variable for benzodiazepine type with three possible values.
Univariate analyses on the binary outcome variables (ICU admission, flumazenil, ventilation, coma) were conducted using simple logistic regression. Multivariate models on these outcome variables were determined using multiple logistic regression, employing both backward and forwards stepwise approaches. The outputs from the final models were reported as odds ratios (OR), with corresponding 95% confidence intervals (CI). Univariate analyses on (the natural log of) LOS was conducted using simple linear regression. Multivariate models of LOS were determined using multiple linear regression, employing both backward and forward stepwise approaches. The output from the final model was reported as coefficients, with corresponding 95% CIs. All statistical analyses were conducted in Stata (version 7, Stata Corporation, Texas USA).
Results
During the study period there were 3081 single benzodiazepine overdose admissions of which 2875 were deliberate self poisonings. Second and subsequent admissions were excluded leaving 2063 single benzodiazepine overdose admissions. There were 131 alprazolam overdoses, 823 diazepam overdoses and 1109 other benzodiazepine overdoses.
Alprazolam overdose
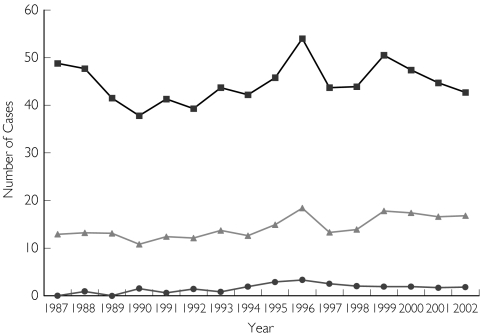
There were 131 cases of alprazolam overdose that presented to the Hunter Area Toxicology Service between January 1987 and October 2002. The incidence of alprazolam deliberate self poisoning for this period is presented in Figure 1. Thirty-eight patients ingested alprazolam alone and 93 took co-ingestants. Of the total 131 cases, patient age ranged from 14 to 73 years with a median age of 36 years (interquartile range [IQR] 30–46) and 42 (32%) were male. The median dose of alprazolam was 23 DDDs (IQR 10–40) and the median LOS was 19 h (IQR 13–39 h). Twenty-nine alprazolam overdoses (22%) were admitted to ICU and 16 (12%) had a GCS <9, 18 (14%) were administered flumazenil and 21(16%) were mechanically ventilated. No patient died. Of the 38 patients ingesting alprazolam alone, two were admitted to ICU, one was ventilated and five were treated with flumazenil.
Figure 1.
Number of benzodiazepine overdoses presenting each year to the Hunter Area Toxicology Service for 1987–2002. All Benzos DSP (▪), Diazepam DSP (▴), Alprazolam DSP (•)
Comparison of alprazolam to other benzodiazepines in overdose
A summary table comparing patients across the three benzodiazepine categories (alprazolam, diazepam, and other benzodiazepine) for each of the outcome variables is shown in Table 1. The multivariate model for the outcomes of ICU admission, mechanical ventilation, coma and flumazenil administration, produced by logistic regression is shown in Table 2. ICU admission, mechanical ventilation and flumazenil administration were significantly more likely for patients who had ingested alprazolam compared with those who had ingested other benzodiazepines after adjusting for other potential predictor variables (Table 2). However, alprazolam ingestion was not associated with an increased risk of coma compared to other benzodiazepines (Table 2).
Table 1. A comparison of patients across the three drug categories (alprazolam, diazepam and other benzodiazepine) and each of the outcome variables.
| Outcome | Alprazolam (n = 131) | Diazepam (n = 823) | Other benzodiazepine (n = 1109) |
|---|---|---|---|
| ICU admission | 22.1% | 11.4% | 14.3% |
| Flumazenil | 13.7% | 4.9% | 7.5% |
| Ventilation | 16.0% | 8.0% | 10.8% |
| Coma | 12.2% | 6.9% | 9.7% |
| LOS (median) | 19.4 h | 15.6 h | 16.3 h |
Table 2. The odds ratios and corresponding 95% confidence intervals obtained from multivariate models for predicting ICU admission, mechanical ventilation, coma and flumazenil administration in benzodiazepine overdose.
| Predictor variable | ICU admission | Mechanical ventilation | Coma | Flumazenil use |
|---|---|---|---|---|
| Benzodiazepine drug | ||||
| Alprazolam | 2.06 (1.27, 3.33) | 1.89 (1.09, 3.28) | – | 2.22 (1.27, 3.89) |
| Diazepam | 0.78 (0.58, 1.05) | 0.66 (0.47, 0.93) | – | 0.75 (0.50, 1.11) |
| Age (10 year increment) | 1.20 (1.10, 1.31) | – | 1.22 (1.10, 1.35) | 1.44 (1.30, 1.60) |
| Female gender | – | – | – | 0.63 (0.44, 0.89) |
| Alcohol | – | – | 1.90 (1.38, 2.61) | – |
| TCAs | 8.93 (6.51, 12.26) | 12.45 (8.86, 17.47) | 4.53 (3.14, 6.55) | – |
| Opiates | 2.22 (1.26, 3.92) | 2.26 (1.17, 4.35) | 3.57 (2.03, 6.29) | – |
| Anticonvulsants | – | 2.02 (1.04, 3.91) | – | – |
| Antipsychotics | 2.11 (1.34, 3.31) | 1.94 (1.17, 3.23) | – | 0.21 (0.05, 0.86) |
The first column contains all predictor variables that were included in at least one of the multivariate models. The second to fifth columns relate to the model for each outcome variable. Where there are dashes the predictor variable was not included in the model for the outcome variable of that column (not significant). The benzodiazepine drug variable had three categories (other benzodiazepine, alprazolam and diazepam) and other was used as the reference. Age was a continuous variable but the odds ratio applied to 10 year increments (i.e. the odds of the outcome variable with an increase of age by 10 years). All other variables were dichotomous. The reference for gender was male and the reference for co-ingested drugs was the absence of that co-ingested drug (i.e. the odds ratio associated with TCAs is interpreted as the odds ratio of the outcome, such as ICU admission, when TCAs are co-ingested compared with if no TCA is co-ingested).
The distribution of LOS was highly (right) skewed, hence the natural logarithm of LOS was used as the outcome variable [written as ln(LOS)]. The multivariate model for the outcome of LOS, produced by linear regression, is shown in Table 3. The table can be interpreted best by taking the exponential of the coefficients. Hence, LOS is predicted to be 1.27 (95% CI 1.04, 1.54) times longer for patients who ingested alprazolam compared with other benzodiazepines. Patients who co-ingested TCAs had a LOS 1.82 (95% CI 1.58, 2.12) times longer than those who did not. LOS increases by 1.19 (95% CI 1.15, 1.22) times, for every 10 years of age.
Table 3. A multivariate model for predicting the natural logarithm of LOS in benzodiazepine overdose.
| Predictor | Coefficient | 95% CI |
|---|---|---|
| Constant | 1.96 | 1.82, 2.09 |
| Drug | ||
| Alprazolam | 0.24 | 0.04, 0.43 |
| Diazepam | −0.03 | −0.12, 0.06 |
| TCAs | 0.60 | 0.46, 0.75 |
| Anticonvulsants | 0.40 | 0.16, 0.63 |
| Antipsychotics | 0.33 | 0.17, 0.50 |
| Age (10 years increase) | 0.17 | 0.14, 0.20 |
| DDDs Taken (10 unit increase) | 0.03 | 0.01, 0.05 |
The benzodiazepine drug variable had three categories (other benzodiazepine, alprazolam and diazepam) and other was used as the reference. Age was a continuous variable but the coefficient applied to 10 years increments (i.e. the coefficient of the ln[LOS] with an increase of age by 10 years). All other variables were dichotomous. The reference for co-ingested drugs was the absence of that co-ingested drug.
Benzodiazepine prescription data
The number of total benzodiazepine prescriptions has remained constant for the period 1992–2001 at approximately 8.5 million per year for those recorded by the Health Insurance Commission (Australian). However, the numbers of alprazolam prescriptions rose over the same period from 0.13 million in 1992 to 0.41 million in 2001. The indications for which various benzodiazepines were prescribed in general practice are presented in Table 4. Forty-eight percent of alprazolam prescriptions were for panic disorder, but this was the given indication in just 0.7% of prescriptions for all other benzodiazepines. In 85% of prescriptions where an indication was provided, alprazolam was prescribed for panic disorder, anxiety, depression or mixed anxiety and depression. This compares with just 20% for all other benzodiazepines for the same indications.
Table 4. Indications for prescription of alprazolam and other benzodiazepines taken from The Copernicus Knowledge System recorded between 1st July 2002 and 30th September 2002 by general practitioners.
| Panic disorder | Anxiety | Depression | Anxiety/ depression | Total: anxiety/ depression/panic disorder | Insomnia | Other/not specified | Total | No indication provided | |
|---|---|---|---|---|---|---|---|---|---|
| Alprazolam | 310 | 194 | 18 | 26 | 548 | 9 | 80 | 643 | 194 |
| 48% | 30% | 2.6% | 4% | 85% | 1.4% | 12% | |||
| Diazepam | 80 | 1252 | 99 | 242 | 1673 | 414 | 2180 | 4258 | 2304 |
| 1.9% | 29% | 2.3% | 5.7% | 39% | 9.7% | 51% | |||
| Temazepam | 3 | 99 | 164 | 58 | 324 | 5791 | 1427 | 7564 | 3391 |
| 0.03% | 1.3% | 2.2% | 0.8% | 4% | 77% | 19% | |||
| Oxazepam | 27 | 1011 | 49 | 147 | 1234 | 1353 | 741 | 3328 | 2483 |
| 0.75% | 31% | 1.6% | 4.4% | 37% | 41% | 22% | |||
| Nitrazepam | 7 | 26 | 33 | 30 | 96 | 1338 | 404 | 1805 | 873 |
| 0.39% | 1.4% | 1.8% | 1.7% | 5% | 74% | 22% | |||
| Flunitrazepam | 0 | 7 | 4 | 0 | 11 | 167 | 55 | 233 | 59 |
| 3% | 1.7% | 5% | 72% | 27% | |||||
| Benzodiazepine otherthan alprazolam | 117 | 2475 | 349 | 477 | 3418 | 9063 | 4807 | 17188 | 9304 |
| 0.68% | 14% | 2.0% | 2.8% | 20% | 53% | 28% |
Discussion
The incidence of benzodiazepine overdose has mirrored their clinical popularity, increasing from their introduction in the 1960s to peak in the 1990s [27]. In our study the incidence of deliberate self poisoning with alprazolam rose from the late 1980s, peaking in the mid 1990s and then remaining constant (Figure 1). This partially reflects the increasing prescription rate over the decade. The clinical effects of benzodiazepine overdose were minor in the majority of cases, but alprazolam was significantly more toxic that other benzodiazepines, based on a range of outcome measures. Alprazolam had a longer median LOS, greater ICU admission rate, greater requirement for mechanical ventilation and more cases in which flumazenil was administered. The median LOS of 19 h and the ICU admission rate of 22% for alprazolam overdose were slightly greater than for all overdose admissions to the Hunter Area Toxicology Service, 17 h and 16%, respectively [28], and significantly greater than other benzodiazepines and diazepam (Table 1).
Although a number of factors could account for the greater toxicity of alprazolam in overdose, our study provides evidence that alprazolam may be intrinsically more toxic than other benzodiazepines. By using multivariate analysis we adjusted for biologically plausible confounders, including dose, age and co-ingestion of other sedative agents. A previous study suggested that the variable toxicity of benzodiazepines may be related to different rates of absorption [29]. This earlier study did not specifically examine alprazolam focusing on temazepam and oxazepam [29]. In our study alprazolam not only increased LOS and ICU admission rate, but also increased the use of interventions to prevent complications of respiratory depression: mechanical ventilation and flumazenil administration.
The relatively greater toxicity of alprazolam in overdose raises a number of questions about its increasing use (almost trebled in 10 years) and the population in which it is mainly prescribed. Alprazolam was approved for use in panic disorder in 1991 in the United States and made available on the Pharmaceutical Benefits Scheme in Australia for the same condition in 1993 [2, 30]. Concerns regarding the potential over-prescription of alprazolam for panic disorder have been raised [30]. We found that 85% of alprazolam indications were for panic disorder, anxiety, depression or mixed anxiety or depression (Table 4). Because suicidal ideation and suicide attempts are more prevalent in people with panic disorder than in the general population [31], the use of alprazolam in this group needs to be better controlled. It has been argued that while those receiving alprazolam are at increased risk of suicidal behaviour (by virtue of their psychiatric diagnoses), alprazolam actually diminishes suicidal ideation [1].
The presentation of medications in terms of quantity available and packaging is important for the risk and severity of deliberate self poisoning [32]. Quantity per prescription is determined by both the strength and number of tablets/capsules. Initially available in 0.25 mg, 0.5 mg and 1 mg strengths, the 2 mg tablet of alprazolam was introduced for panic disorder in which larger doses are used [2]. In Australia alprazolam (100 DDDs per prescription) is available in quantities four times as large as diazepam (25), twice as large as nitrazepam (50) or oxazepam (50) and more than three times as large as flunitrazepam (30). Thus a person taking alprazolam has access to relatively large quantities of easily ingestible medication. This is of significant concern because this patient group may be at a higher risk of deliberate self poisoning and we have demonstrated that alprazolam is more toxic than other benzodiazepines. The relatively greater toxicity of alprazolam in deliberate self poisoning and its current status as among the two benzodiazepines available in largest quantity per prescription, support restrictions on pack size and limitation of availability in bottles.
In sufficiently large doses benzodiazepines can cause coma, respiratory depression [3] and death [33]. An Australian study of poisoning fatalities during 1997 found benzodiazepines present in toxic concentrations in 9% of cases [34]. Severe toxicity is often related to co-ingestants, especially alcohol and opiates, and advanced age is an additional risk factor for severe toxicity [3, 29, 33, 34]. The increased toxicity of benzodiazepine overdose with co-ingestion of other sedating medications and increasing age was also seen in our study.
An interesting finding in the study was that, of the five outcomes, coma (GCS < 9) was the only one where alprazolam was not significantly different from other benzodiazepines. This suggests that the relative toxicity of alprazolam compared with other benzodiazepines is not related to the level of consciousness that occurs in overdose as measured by the GCS. This may be either due to GCS being a poor measure of coma in overdose patients or that the reason for alprazolam's increased toxicity is more dependent on respiratory depression.
The predictors of flumazenil administration were different to other outcomes reflecting the use and contra-indications of this antidote. It is unclear why female sex was a predictor of its use. That flumazenil was used significantly more often in alprazolam overdose compared with other benzodiazepines is a significant finding because in the Hunter Area Toxicology Service the use of flumazenil is restricted and is generally only given by or at the request of the attending clinical toxicologist. This policy may confound the assessment of risk factors for flumazenil use.
In addition to demonstrating that alprazolam was more toxic than other benzodiazepines, our study showed that co-ingestion of other medications also significantly worsened outcome. TCA co-ingestion was by far the most important and over-shadowed the effect of alprazolam vs other benzodiazepines. This is to be expected based on the known significant toxicity of TCAs. In addition other co-ingestants affected the outcomes, but the effect was of a similar order of magnitude to the difference between alprazolam and other benzodiazepines.
There were a number of limitations of the study. Although a study of pure ingestions provides the best indicator of the intrinsic toxicity of a drug, it is less useful in providing information on the majority of overdoses where more than one drug is ingested. The study included a large number of cases overall and used multivariate analysis to adjust for the effect of major co-ingestant drugs, so still provided a good indication of intrinsic drug toxicity. In addition, observational studies such as this are likely to have good external validity since they are conducted in the clinical context in which care is provided [25]. Although the increase in LOS is unlikely to be clinically significant, the increased ICU admission rate and use of mechanical ventilation is a significant increase in resource use.
Drug concentrations were not available for patients in the study because they are not part of the routine management of patients by the Hunter Area Toxicology Service. However, all poisoned patients admitted to the Hunter Area Toxicology Service have the drug of ingestion confirmed by history taking on at least two occasions, and this is confirmed with history from ambulance officers, family and friends, as well as evidence of empty drug containers. A study of quetiapine overdose in the Hunter Area Toxicology Service has validated this by demonstrating that the peak concentration of quetiapine following overdose highly correlated with reported dose [35].
In conclusion, our study demonstrates that alprazolam is relatively more toxic than other benzodiazepines. Because this effect remains after adjustment for dose, co-ingested medication and age, this greater toxicity appears due to intrinsic toxicity of alprazolam. Alprazolam overdose should be regarded as more significant than other benzodiazepines. In addition, the pack size and packaging of alprazolam should be reviewed to decrease the risk of it being taken for deliberate self poisoning.
Acknowledgments
Geoffrey Isbister designed the study, supervised the data extraction, contributed to data analysis, interpretation and all drafts of the paper. Luke O’Regan did the literature review, collected and contributed to the data analysis and wrote the initial draft. David Sibbritt did all statistical analysis and contributed to all drafts. Ian Whyte designed the database used in the study and contributed to all drafts of the paper. Debbie Whyte and Toni Nash did all data entry. Stuart Allen did all data extraction from the database.
There were no conflicts of interest for any author.
We would like to acknowledge Stuart Allen for extracting the data from the database, and Debbie Whyte and Toni Nash for entering the data into the database. We also thank Jane Robertson and Maxine Robinson for help with prescription data and Geoff Sayer for access to the Copernicus Knowledge System for indications data.
References
- 1.Jonas JM, Cohon MS. A comparison of the safety and efficacy of alprazolam versus other agents in the treatment of anxiety, panic, and depression: a review of the literature. J Clin Psychiatry. 1993;54(Suppl):25–45. [PubMed] [Google Scholar]
- 2.Abramowicz M. Alprazolam for panic disorder. Med Lett Drugs Ther. 1991;33:30–1. [PubMed] [Google Scholar]
- 3.Henderson A, Wright M, Pond SM. Experience with 732 acute overdose patients admitted to an intensive care unit over six years. Med J Aust. 1993;158:28–30. doi: 10.5694/j.1326-5377.1993.tb121644.x. [DOI] [PubMed] [Google Scholar]
- 4.Augenstein WL, Kulig KW, Rumack BH. Captopril overdose resulting in hypotension. JAMA. 1988;259:3302–5. [PubMed] [Google Scholar]
- 5.Michaud K, Augsburger M, Romain N, Giroud C, Mangin P. Fatal overdose of tramadol and alprazolam. Forensic Sci Int. 1999;105:185–9. doi: 10.1016/s0379-0738(99)00118-8. [DOI] [PubMed] [Google Scholar]
- 6.Jenkins AJ, Levine B, Locke JL, Smialek JE. A fatality due to alprazolam intoxication. J Anal Toxicol. 1997;21:218–20. doi: 10.1093/jat/21.3.218. [DOI] [PubMed] [Google Scholar]
- 7.Rathod NR. Alprozolam poisoning. Indian J Med Sci. 2001;55:218–21. [PubMed] [Google Scholar]
- 8.Mur P, Rodriguez M, Martinez-Cano H, et al. Allergic and toxic reaction to alprazolam. Postgrad Med. 1995;71:444. doi: 10.1136/pgmj.71.837.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fraser AD, Isner AF, Moss MA. A fatality involving clomipramine. J Forensic Sci. 1986;31:762–7. [PubMed] [Google Scholar]
- 10.Mullins ME. First-degree atrioventricular block in alprazolam overdose reversed by flumazenil. J Pharm Pharmacol. 1999;51:367–70. doi: 10.1211/0022357991772385. [DOI] [PubMed] [Google Scholar]
- 11.Litovitz TL, Holm KC, Clancy C, Schmitz BF, Clark LR, Oderda GM. 1992 annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 1993;11:494–555. doi: 10.1016/0735-6757(93)90093-q. [DOI] [PubMed] [Google Scholar]
- 12.Litovitz TL, Clark LR, Soloway RA. 1993 annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 1994;12:546–84. doi: 10.1016/0735-6757(94)90276-3. [DOI] [PubMed] [Google Scholar]
- 13.Litovitz TL, Felberg L, Soloway RA, Ford M, Geller R. 1994 annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 1995;13:551–97. doi: 10.1016/0735-6757(95)90171-X. [DOI] [PubMed] [Google Scholar]
- 14.Litovitz TL, Felberg L, White S, Klein-Schwartz W. 1995 annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 1996;14:487–537. doi: 10.1016/S0735-6757(96)90160-6. [DOI] [PubMed] [Google Scholar]
- 15.Litovitz TL, Smilkstein MJ, Felberg L, Klein-Schwartz W, Berlin R, Morgan JL. 1996 annual report of the American Association of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med. 1997;15:447–500. doi: 10.1016/s0735-6757(97)90193-5. [DOI] [PubMed] [Google Scholar]
- 16.Litovitz TL, Klein-Schwartz W, Dyer KS, Shannon M, Lee S, Powers M. 1997 annual report of the American Association of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med. 1998;16:443–97. doi: 10.1016/s0735-6757(98)90000-6. [DOI] [PubMed] [Google Scholar]
- 17.Litovitz TL, Klein-Schwartz W, Caravati EM, Youniss J, Crouch B, Lee S. 1998 annual report of the American Association of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med. 1999;17:435–87. doi: 10.1016/s0735-6757(99)90254-1. [DOI] [PubMed] [Google Scholar]
- 18.Litovitz TL, Klein-Schwartz W, White S, et al. 1999 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance system. Am J Emerg Med. 2000;18:517–74. doi: 10.1053/ajem.2000.9261. [DOI] [PubMed] [Google Scholar]
- 19.Litovitz TL, Klein-Schwartz W, White S, et al. 2000 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 2001;19:337–95. doi: 10.1053/ajem.2001.25272. [DOI] [PubMed] [Google Scholar]
- 20.Litovitz TL, Klein-Schwartz W, Rodgers GC, Jr, et al. 2001 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 2002;20:391–452. doi: 10.1053/ajem.2002.34955. [DOI] [PubMed] [Google Scholar]
- 21.Serfaty M, Masterton G. Fatal poisonings attributed to benzodiazepines in Britain during the 1980s. Br J Psychiatry. 1993;163:386–93. doi: 10.1192/bjp.163.3.386. [DOI] [PubMed] [Google Scholar]
- 22.Reith DM, Fountain J, McDowell R, Tilyard M. Comparison of the fatal toxicity index of zopiclone with benzodiazepines. J Toxicol Clin Toxicol. 2003;41(7):975–80. doi: 10.1081/clt-120026520. [DOI] [PubMed] [Google Scholar]
- 23.Buckley NA, Whyte IM, Dawson AH, McManus PR, Ferguson NW. Self-poisoning in Newcastle, 1987–92. Med J Aust. 1995;162:190–3. doi: 10.5694/j.1326-5377.1995.tb126020.x. [DOI] [PubMed] [Google Scholar]
- 24.Buckley NA, Whyte IM, Dawson AH, Reith DA. Preformatted admission charts for poisoning admissions facilitate clinical assessment and research. Ann Emerg Med. 1999;34:476–82. [PubMed] [Google Scholar]
- 25.Whyte IM, Buckley NA, Dawson AH. Data collection in clinical toxicology: are there too many variables? J Toxicol Clin Toxicol. 2002;40:223–30. doi: 10.1081/clt-120005492. [DOI] [PubMed] [Google Scholar]
- 26.Buckley N, McManus P. Fatal toxicity of drugs used in the treatment of psychotic illnesses. Br J Psychiatry. 1998;172:461–4. doi: 10.1192/bjp.172.6.461. [DOI] [PubMed] [Google Scholar]
- 27.Greenblatt DJ, Allen MD, Noel BJ, Shader RI. Acute overdosage with benzodiazepine derivatives. Clin Pharmacol Ther. 1977;21:497–514. doi: 10.1002/cpt1977214497. [DOI] [PubMed] [Google Scholar]
- 28.Isbister GK, Balit CR, Dawson AH, Whyte IM. Valproate overdose: a comparative cohort study of self poisonings. Br J Clin Pharmacol. 2003;55:398–404. doi: 10.1046/j.1365-2125.2003.01772.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buckley NA, Dawson AH, Whyte IM, O'Connell DL. Relative toxicity of benzodiazepines in overdose. Br Med J. 1995;310:219–21. doi: 10.1136/bmj.310.6974.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mant A. Panic disorders and the listing of alprazolam on authority on the PBS. Beware of overdiagnosis. Aust Fam Physician. 1994;23:658–60. [PubMed] [Google Scholar]
- 31.Lepine JP, Chignon JM, Teherani M. Suicide attempts in patients with panic disorder. Arch Gen Psychiatry. 1993;50:144–9. doi: 10.1001/archpsyc.1993.01820140070008. [DOI] [PubMed] [Google Scholar]
- 32.Chan TYK. Packaging of drugs and the risk of severe toxicity in adult self- poisonings. J Clin Pharm Ther. 1997;22:157–8. doi: 10.1046/j.1365-2710.1997.8675086.x. [DOI] [PubMed] [Google Scholar]
- 33.Drummer OH, Ranson DL. Sudden death and benzodiazepines. Am J Forensic Med. 1996;17:336–42. doi: 10.1097/00000433-199612000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Bystrzycki A, Coleridge J. Drug – and poison-related deaths in Victoria during 1997. Emerg Med. 2000;12:303–9. [Google Scholar]
- 35.Balit CR, Isbister GK, Whyte IM. Quetiapine poisoning: a case series. Ann Emerg Med. 2003;42(6):751–8. doi: 10.1016/s0196-0644(03)00600-0. [DOI] [PubMed] [Google Scholar]