Abstract
Aim
To investigate the effects of donepezil at steady state on the safety, tolerability and pharmacokinetics of a single dose of thioridazine, in healthy subjects.
Methods
An open, two-way, balanced crossover study, in 12 subjects (six men and six women) aged 19–41 years. During both treatment periods, subjects received a single oral dose of 50 mg thioridazine; in one period the thioridazine was given alone, and in the other period it was given together with the last of 15 daily, oral doses of donepezil 5 mg. The ‘washout’ periods were 1 week when thioridazine was given first, and 2 weeks when thioridazine was given last. Plasma concentrations of thioridazine were measured after each dose, and pharmacokinetic parameters were determined. Interactions were tested by using an equivalence analysis in which thioridazine was the ‘Reference’ and thioridazine + donepezil the ‘Test’ regimen. Safety and tolerability were monitored.
Results
Donepezil had no marked effect on the pharmacokinetics of thioridazine, as judged by the equivalence analysis of AUC0–tn, AUC0–∞, t½ and tmax. Cmax was very similar in the ‘Test’ and ‘Reference’ regimens, but the confidence intervals were too wide to confirm equivalence. Donepezil was well tolerated, whereas thioridazine was associated with light-headedness, tiredness and postural hypotension, irrespective of whether or not donepezil was given concurrently.
Conclusions
Repeated dosing with donepezil, 5 mg daily for 2 weeks, had no significant effect on the safety, tolerability or pharmacokinetics of thioridazine. Thioridazine was poorly tolerated.
Keywords: acetylcholinesterase inhibitor, Alzheimer's disease, donepezil, drug–drug interactions, pharmacokinetics, thioridazine
Introduction
Donepezil is a piperidine-based acetylcholinesterase (AChE) inhibitor for the treatment of Alzheimer's disease (AD), a form of dementia characterized by neuronal cell death and reductions in cortical levels of the neurotransmitter acetylcholine (ACh) [1, 2]. Donepezil increases cortical ACh levels and, by enhancing cholinergic function in the surviving neurones, improves cognition and function in patients with mild to moderate AD [3, 4]. These effects have been demonstrated in double-blind clinical trials lasting up to 1 year [5, 6], and improvements in behavioural symptoms have been shown in patients with moderate to severe AD [7]. Donepezil is well tolerated, with most adverse events (AEs) being transient and gastrointestinal [3–6], consistent with its cholinomimetic mode of action.
After oral administration, donepezil achieves a relative bioavailability of 100% and reaches peak plasma concentrations within 3–4 h of dosing. It has a long plasma elimination half-life, resulting in stable plasma drug concentrations that allow once-daily dosing [8]. The parent compound is metabolized mainly in the liver, by the cytochrome P-450 isoenzyme CYP 3A4 and, to a lesser extent, CYP 2D6 [9]. Donepezil binds to both these enzymes with a low affinity in vitro (mean Ki 50–130 µm), and is therefore unlikely to inhibit the clearance of other drugs metabolized via CYP 3A4 and CYP 2D6 pathways. Nevertheless, it is important to demonstrate that such interactions between drugs that are likely to be administered to patients with AD do not occur in vivo.
Thioridazine, an antipsychotic agent of the phenothiazine group II class, is indicated for the second-line management of acute symptoms of schizophrenia, mania and hypomania. It has also been used as a short-term adjunctive treatment for anxiety and psychomotor agitation, and is the most commonly prescribed phenothiazine in primary care in the UK [10]. Thioridazine used to be frequently prescribed to elderly patients and those with dementia, possibly because of its significant sedative effect and relatively few motor side-effects [11]. However, since the completion of this study, major changes have been made to the labelling of thioridazine in the UK, owing to its potential for causing heart arrhythmias. For safety reasons, the UK Committee on the Safety of Medicines recommends that thioridazine should not be prescribed by primary care physicians, and should only be used to treat schizophrenia patients who have failed to respond to other treatments [12]. However, this view has been challenged by primary care [10] and hospital-based [13] physicians.
Thioridazine, like donepezil, is metabolized in part by the CYP 2D6 system [14], and co-administration of donepezil and thioridazine may therefore reduce the clearance of thioridazine. Reduced clearance of thioridazine could exacerbate its sedative effects, and increase the risk of adverse cardiovascular events, such as arrhythmia [15–17] and postural hypotension [18], associated with its electrocardiographic prolongation of the QTc interval (the QT interval corrected for heart rate) and α-adrenoreceptor antagonistic activity. It is not practical to test for such an interaction in AD patients; therefore this study aimed to investigate whether steady-state dosing with donepezil would alter the safety, tolerability, or pharmacokinetics of a single dose of thioridazine in healthy subjects.
Methods
Subjects
Twelve healthy men and women, aged 19–41 years, with a body mass index in the range 20–25, gave written, informed consent to participate in the study. None had any history or evidence of important illness, and none was taking any other medication. Women of childbearing age had a negative pregnancy test, and were required to use reliable contraception throughout the study period.
The study was conducted in 1998 in accordance with the Declaration of Helsinki and the ICH Guideline for Good Clinical Practice, and was approved by the Brent Medical Ethics Committee.
Study procedures
This was an open-label, two-way, balanced crossover study, randomized with respect to treatment sequence, in which subjects were divided into two groups of six subjects each, with equal numbers of men and women in each group. The study duration was 36 days. All subjects received once-daily oral doses of 5 mg donepezil on the morning of days 8–21 inclusive, and single oral doses of both 5 mg donepezil and 50 mg thioridazine on day 22. Six subjects received a single oral dose of 50 mg thioridazine on day 1, followed by a 1-week washout period (days 2–7), before donepezil treatment. The other six subjects received a single oral dose of 50 mg thioridazine on day 36, after a 2-week washout period (days 23–35).
Subjects came to the unit daily to receive donepezil under supervision, and attended for follow-up 5–10 days after the last dose of study medication. Subjects were admitted on the evening before each dose of thioridazine and fasted overnight until 3 h after drug administration in the morning. Alcohol and caffeine-containing beverages, and smoking, were prohibited for 24 h before each dose of thioridazine until the end of the residential period.
Sample collection and analysis
Venous blood samples (10 ml) for the assay of plasma concentrations of thioridazine were collected at 0.5, 1, 1.5, 2, 2.5, 3, 4, 6, 8, 24, 28, 34 and 48 h after administration of thioridazine. Blood samples for the donepezil assay were taken on days 12, 17 and 22, before dosing with donepezil. All blood samples for the assay of drug concentrations were collected in lithium heparinized tubes, chilled immediately on ice, and then separated by centrifugation at 1000 g for 10 min at 4 °C. Aliquots for subsequent drug assay were stored at −20 °C. Plasma concentrations of thioridazine and donepezil were determined by specific high-performance liquid chromatography (HPLC) [19]. The accuracy of the thioridazine assay was assessed by internal quality control samples: for samples of 15, 30 and 250 µg l−1, the mean measured values were within 5% of expected values, and the coefficients of variation for between-assay precision were 14, 7 and 8%, respectively.
Pharmacokinetic assessments
The pharmacokinetic parameters derived for thioridazine were: the maximum plasma concentration (Cmax), the time at which Cmax was attained (tmax), the elimination half-life (t½), and the area under the concentration–time curve (AUC0–∞). The AUC0–∞ comprised the AUC from zero to time tn (AUC0–tn), where tn was the last time point with concentrations above the lower limit of quantification, which was calculated using the log-linear trapezoidal rule, and AUCtn–∞, derived by extrapolation from time tn to infinity as follows:
where λz is the elimination rate constant calculated from non-linear regression of the terminal portion of the plasma concentration–time curve and Cn the predicted value of the concentration at time tn. The data were iteratively weighted by the reciprocal of the predicted plasma drug concentrations squared.
The donepezil trough plasma concentrations (Cpre) on the mornings of days 12, 17 and 22 were determined directly from the donepezil plasma concentration–time data.
Statistical analysis
Thioridazine pharmacokinetic parameters, Cmax, t½, AUC0–∞ and AUC0–tn were logarithmically transformed and subjected to an analysis of variance (anova). From the anova results, 90% confidence intervals (CI) were calculated for the ratio of geometric means of the parameters of thioridazine alone and in combination with donepezil. Thioridazine alone was defined as the ‘Reference’ and thioridazine with donepezil was defined as the ‘Test’ regimen. If the 90% CI of log ratio of Test : Reference was within the range 80–125%, an absence of interaction between the two drugs was concluded [20]. This procedure is identical to that used conventionally to assess the bioequivalence of two formulations of the same drug, and is equivalent to the two-sided procedure of Schuirmann [21].
The 90% CI of the median of the Test minus Reference difference, calculated from the Wilcoxon signed rank test, was used to compare tmax values.
Safety
Safety was evaluated on the basis of the incidence and severity of all AEs, and changes in vital signs, physical findings, clinical laboratory variables and ECG variables. Standard 12-lead ECGs were recorded using Marquette machines, with automatic QTc printout.
Results
Subjects
Of the 12 subjects who entered the study, 11 completed it. There were no significant differences between the two groups with respect to baseline demographic characteristics. For groups A and B, mean age (s.d.) was 27.8 (8.1) and 24.7 (2.4) years, respectively, and mean weight (s.d.) was 64.1 (8.6) and 65.0 (6.6) kg, respectively.
Pharmacokinetics of thioridazine
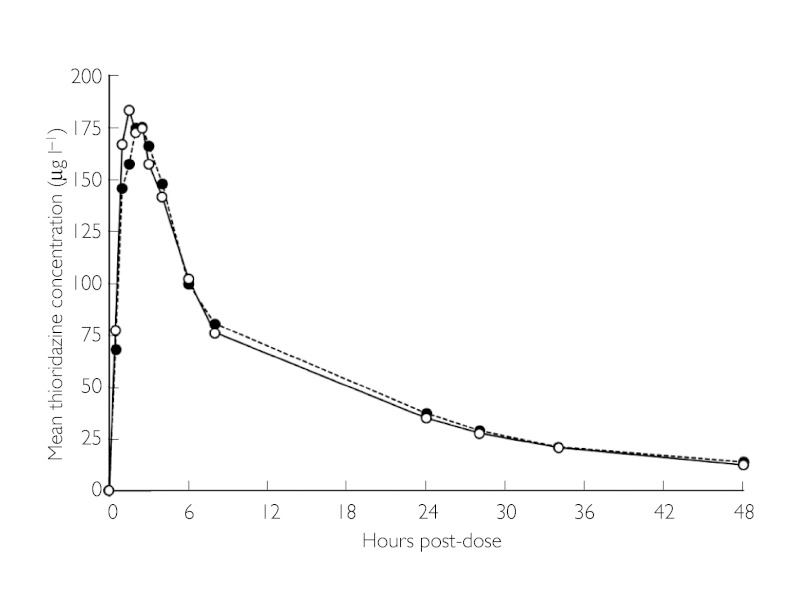
Mean thioridazine concentrations during the 48 h after administration of thioridazine (either alone, or in combination with donepezil on day 22) are shown in Figure 1, and thioridazine pharmacokinetic parameters are summarized in Table 1. Plasma concentrations of thioridazine were similar for the two regimens. The equivalence analysis, in which thioridazine was the Reference and thioridazine + donepezil the Test regimen, also showed that donepezil had no marked effect on the pharmacokinetics of thioridazine as judged by AUC0–tn, AUC0–∞, t½ and tmax (Table 2). Mean and median Cmax values were very similar in the Test and Reference regimens (e.g. median Cmax : thioridazine alone, 180.6; thioridazine + donepezil, 192.2), but the 90% upper CI exceeded 125%, so equivalence was not confirmed.
Figure 1.
Mean plasma thioridazine concentration vs. time after administration of thioridazine (50 mg) alone, and after co-administration of donepezil (5 mg) to steady state. n = 11 for each treatment. Donepezil HCI + thioridazine HCI (○—○), thioridazine HCI only (•---•), n = 11 for each treatment
Table 1.
Summary of thioridazine pharmacokinetic parameters after administration of thioridazine (50 mg) alone, and after co-administration of donepezil (5 mg) to steady state
| Mean (s.d.) | ||
|---|---|---|
| Parameter | Thioridazinealone(n = 11) | Thioridazine +donepezil(n = 11) |
| Cmax (µg l−1) | 205.5 (106.5) | 214.3 (71.9) |
| tmax (h)* | 1.5 | 1.5 |
| AUC0–tn (µg h−1 l−1) | 2399.0 (1046.3) | 2333.1 (800.3) |
| AUC0–∞ (µg h−1 l−1) | 2689.7 (1214.3) | 2607.1 (941.2) |
| Mean residence time (h) | 19.7 (3.0) | 19.5 (3.5) |
| t½ (h) | 15.3 (2.1) | 15.3 (2.6) |
Median values.
Thioridazine + donepezil was equivalent to thioridazine alone with respect to AUC0–tn, AUC0–∞ and tmax. According to standard criteria, equivalence was not confirmed with respect to Cmax as the upper CI was greater than 125%. There was a high level of confidence that the t1/2 of thioridazine was not influenced by co-administration of donepezil.
Table 2.
Equivalence analysis of thioridazine pharmacokinetic parameters after administration of thioridazine (50 mg) alone (Reference) and after coadministration of donepezil (5 mg) to steady state (Test)
| Parameter | Lower Cl | Upper Cl |
|---|---|---|
| Log AUC0–tn | 87% | 113% |
| Log AUC0–∞ | 86% | 114% |
| Log Cmax | 89% | 134% |
| Log t½ | 93% | 107% |
| tmax difference (h) | −1.00 | 1.00 |
Values are the 90% confidence intervals (CI) of the ratio Test : Reference regimen, expressed as a percentage, except for tmax, where values are the 90% confidence interval of the median of the difference Test – Reference, calculated from the Wilcoxon signed rank test.
n = 11 for each treatment.
Pharmacokinetics of donepezil
Mean plasma concentrations of donepezil on days 12, 17 and 22 are shown in Table 3. Mean plasma concentrations of donepezil were higher on day 17 than on day 12, but changed little from day 17 to day 22, showing that a steady state had been reached by day 17. Intersubject variability in donepezil concentration was small (e.g. plasma donepezil concentration range on day 12: 10.01–15.26 ng ml−1).
Table 3.
Plasma donepezil concentrations (ng ml−1) on days 12, 17 and 22
| Cpre | |||
|---|---|---|---|
| Day 12 | Day 17 | Day 22 | |
| Mean | 12.38 | 18.02 | 18.60 |
| Range | 10.01–15.26 | 11.82–23.64 | 10.61–25.76 |
| Median | 12.33 | 17.40 | 18.64 |
Cpre = trough plasma concentrations; n = 12.
Safety
One woman was withdrawn from the study because she had syncope due to postural hypotension shortly after thioridazine in combination with donepezil on day 22; she did not receive thioridazine without donepezil co-treatment. In most subjects, AEs were mild to moderate in severity, and all resolved spontaneously. After thioridazine alone, 10 of 11 subjects had a total of 32 AEs, of which light-headedness and tiredness were the most common. After thioridazine in combination with donepezil, 11 subjects had 22 AEs; light-headedness and tiredness were again the most common. There were eight AEs reported by five subjects during daily donepezil treatment; tiredness and nausea being the most common (Table 4).
Table 4.
Summary of frequency of treatment-emergent adverse events after administration of thioridazine (50 mg) alone, and after co-administration of donepezil (5 mg) to steady state
| Adverse event | Donepezil alone | Thioridazine alone | Thioridazine + donepezil |
|---|---|---|---|
| Light-headedness/dizziness/fainting | 0 | 14 | 9 |
| Drowsiness/tiredness/fatigue | 3 | 6 | 6 |
| Nausea | 2 | 2 | 1 |
| Other | 3 | 10 | 6 |
| Total | 8 | 32 | 22 |
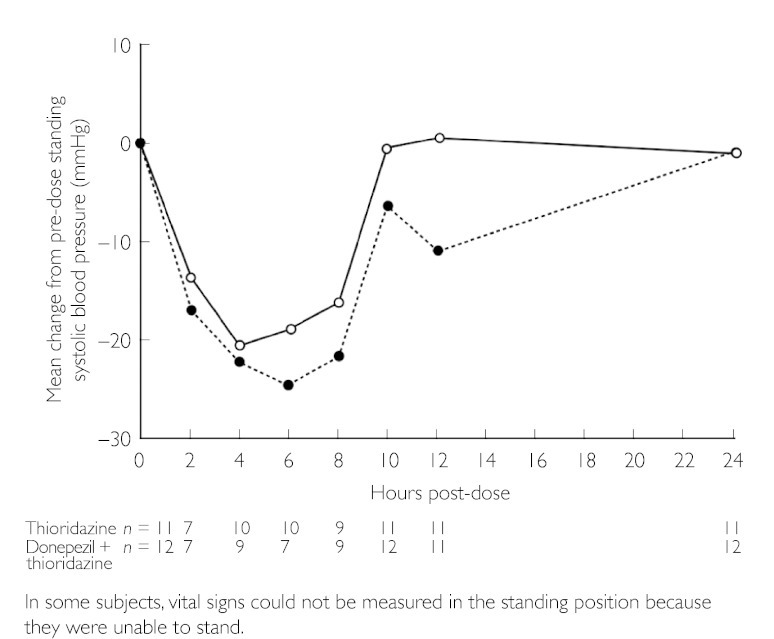
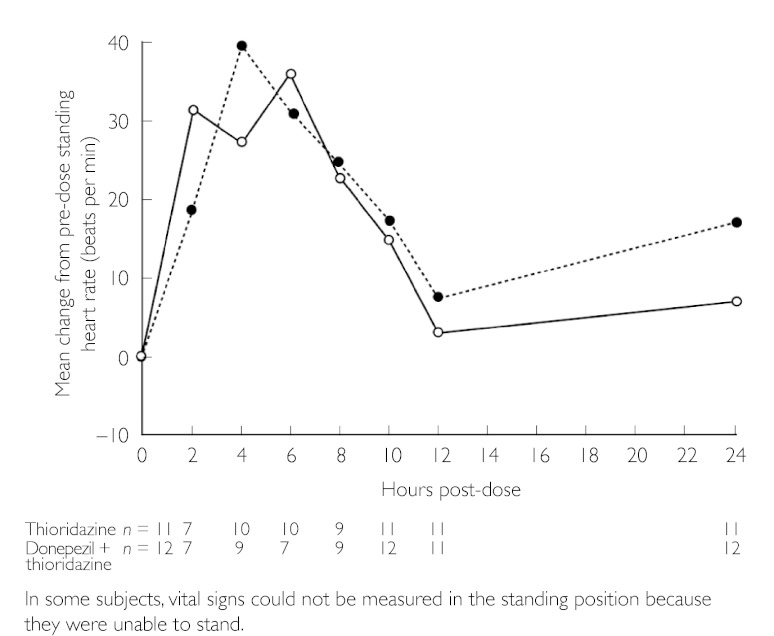
Up to about 12 h after thioridazine, many subjects had reductions in supine and standing systolic (Figure 2) and diastolic blood pressures, and increases in heart rate (Figure 3). The results of ECG and physical examination were generally normal, and there were no clinically significant changes in laboratory variables. There was a slight increase in QTc interval after thioridazine administration, which was not affected by donepezil treatment (Table 5).
Figure 2.
Mean change from pre-dose standing systolic blood pressure over time after administration of thioridazine (50 mg) alone, and after co-administration of donepezil (5 mg) to steady state. Donepezil HCl + thioridazine HCl (○—○), thioridazine HCl only (•---•)
Figure 3.
Mean change from pre-dose standing heart rate over time after administration of thioridazine (50 mg) alone, and after co-administration of donepezil (5 mg) to steady state. Donepezil HCl + thioridazine HCl (○—○), thioridazine HCl only (•---•)
Table 5.
Mean (s.d.) QTc intervals (ms) at screening (prior to drug dosing), after dosing with thioridazine (50 mg) alone and after coadministration of donepezil (5 mg). The QTc interval is the electrocardiographic QT interval corrected for heart rate
| Mean (s.d.) | |||
|---|---|---|---|
| Pre-drug(n = 12) | Thioridazine alone (n = 11) | Thioridazine + donepezil(n = 12) | |
| Screening | 388.2 (14.82) | – | – |
| Pre-dose | – | 394.5 (19.95) | 389.4 (24.96) |
| 3 h post-dose | – | 410.3 (23.93) | 410.8 (24.61) |
Discussion
This study showed that donepezil had no significant effect on the pharmacokinetics of thioridazine: equivalence was confirmed for AUC, t½ and tmax. Equivalence for Cmax was not confirmed according to standard criteria, but the mean and median values were very similar between the two regimens, and it was clear that donepezil did not alter the pharmacokinetics of thioridazine to any clinically significant extent. These findings are consistent with other studies, which have shown that donepezil has a low propensity for interaction with drugs metabolized by the P450 isoenzyme CYP 2D6 [22–26].
Donepezil alone was well tolerated: the nature and frequency of AEs were consistent with those reported in other multiple-dosing studies [22–26]. Co-administration of donepezil in our study did not worsen the tolerability of thioridazine. AEs were mainly postural hypotension, lightheadedness and tiredness, consistent with other studies of thioridazine [27].
However, thioridazine was poorly tolerated: either alone or in combination with donepezil, it was followed by reductions in supine and standing systolic and diastolic blood pressure, and increases in heart rate. The mean QTc interval was slightly increased 3 h after the administration of a single dose of thioridazine, compared to the value at screening. Thioridazine not only has an anti-dopaminergic effect, but is also an α-adrenoreceptor antagonist. The resulting arterial and venous vasodilation probably accounted for the reductions in blood pressure. The anti-cholinergic activity of thioridazine may also have contributed to the increase in heart rate.
The effects of thioridazine alone on blood pressure, heart rate and QTc interval in our study are similar to those observed following single doses of thioridazine (50 mg) in a pharmacodynamic study in healthy subjects [18]. The results of that study suggested that thioridazine impairs cardiac repolarization in a dose-dependent manner. Several studies have shown that thioridazine increases the risk of sudden cardiac death in psychiatric patients [16, 17]. This increased risk is attributed to drug-induced arrhythmias, such as torsade de pointes, which is associated with a prolongation of the QTc interval [15].
The potential of thioridazine for causing life-threatening adverse effects means that chronic dosing might expose volunteers to health risks. Therefore, in this study, the effects of donepezil were examined on single doses of thioridazine. None of the effects of thioridazine on heart rate and blood pressure were influenced by the co-administration of donepezil.
The results of our study show that repeated dosing with donepezil has no clinically important effect on the safety, tolerability or pharmacokinetics of thioridazine in healthy subjects. However, co-administration of donepezil and thioridazine in patients with AD is probably best avoided, since the marked anti-cholinergic activity of thioridazine could further impair cognition in these patients and diminish or prevent the beneficial effects of co-administered donepezil. Indeed, single doses of thioridazine have been shown to impair cognition in healthy subjects [18], and very limited data are available to support the use of thioridazine in the treatment of dementia [11]. Furthermore, the poor tolerability of thioridazine confirms that the drug should be given most cautiously to patients with AD, whether alone or in combination with donepezil.
References
- 1.Katzman R, Saitoh T. Advances in Alzheimer's disease. FASEB J. 1991;5:278–86. [PubMed] [Google Scholar]
- 2.Becker RE. Therapy of the cognitive deficit in Alzheimer's disease: the cholinergic system. In: Becker R, Giacobini E, editors. In Cholinergic Basis for Alzheimer Therapy. Boston: Birkhäuser; 1991. pp. 1–30. [Google Scholar]
- 3.Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT. A 24-week, double-blind, placebo-controlled trial of donepezil in patients with Alzheimer's disease. Neurology. 1998;50:136–45. doi: 10.1212/wnl.50.1.136. [DOI] [PubMed] [Google Scholar]
- 4.Burns A, Rossor M, Hecker J, Gauthier S, Petit H, Moller HJ, Rogers SL, Friedhoff LT. The effects of donepezil in Alzheimer's disease – results from a multinational trial. Dement Geriatr Cogn Disord. 1999;10:237–44. doi: 10.1159/000017126. [DOI] [PubMed] [Google Scholar]
- 5.Winblad B, Engedal K, Soininen H, Verhey F, Waldemar G, Wimo A, Wetterholm AL, Zhang R, Haglund A, Subbiah P Donepezil Nordic Study Group. A 1-year, randomized, placebo-controlled study of donepezil in patients with mild to moderate AD. Neurology. 2001;57:489–95. doi: 10.1212/wnl.57.3.489. [DOI] [PubMed] [Google Scholar]
- 6.Mohs RC, Doody RS, Morris JC, Ieni JR, Rogers SL, Perdomo CA, Pratt RD. A 1-year placebo-controlled preservation of function survival study of donepezil in AD patients. Neurology. 2001;57:481–8. doi: 10.1212/wnl.57.3.481. “312” Study Group. [DOI] [PubMed] [Google Scholar]
- 7.Feldman H, Gauthier S, Hecker J, Vellas B, Subbiah P, Whalen E Donepezil MSAD Study Investigators Group. A 24-week, randomized, double-blind study of donepezil in moderate to severe Alzheimer's disease. Neurology. 2001;57:613–20. doi: 10.1212/wnl.57.4.613. [DOI] [PubMed] [Google Scholar]
- 8.Rogers SL, Friedhoff LT. Pharmacokinetic and pharmacodynamic profile of donepezil following single oral doses. Br J Clin Pharmacol. 1998;46(Suppl. 1):1–6. doi: 10.1046/j.1365-2125.1998.0460s1001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tiseo PJ, Perdomo CA, Friedhoff LT. Metabolism and elimination of 14C-donepezil in healthy volunteers: a single-dose study. Br J Clin Pharmacol. 1998;46(Suppl. 1):19–24. doi: 10.1046/j.1365-2125.1998.0460s1019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright N. Removal of thioridazine from primary care formulary will result in prescribing vacuum. BMJ. 2001;323:695. doi: 10.1136/bmj.323.7314.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirchner V, Kelly CA, Harvey RJ. Thioridazine for dementia. Cochrane Database Syst Rev. 2001 doi: 10.1002/14651858.CD000464. CD000464. [DOI] [PubMed] [Google Scholar]
- 12.Committee on Safety of Medicines. Thioridazine: Restricted Indications and New Warning on Cardiotoxicity. London: CSM; 2000. [Google Scholar]
- 13.Davies SJ, Cooke LB, Moore AG, Potokar J. Discontinuation of thioridazine in patients with learning disabilities: balancing cardiovascular toxicity with adverse consequences of changing drugs. BMJ. 2002;324:1519–21. doi: 10.1136/bmj.324.7352.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Otani K, Aoshima T. Pharmacogenetics of classical and new antipsychotic drugs. Ther Drug Monit. 2000;22:118–21. doi: 10.1097/00007691-200002000-00025. [DOI] [PubMed] [Google Scholar]
- 15.Reilly JG, Ayis SA, Ferrier IN, Jones SJ, Thomas SH. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet. 2000;355:1048–52. doi: 10.1016/s0140-6736(00)02035-3. [DOI] [PubMed] [Google Scholar]
- 16.Ray WA, Meredith S, Thapa PB, Meador KG, Hall K, Murray KT. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiatry. 2001;58:1161–7. doi: 10.1001/archpsyc.58.12.1161. [DOI] [PubMed] [Google Scholar]
- 17.Glassman AH, Bigger JT., Jr Antipsychotic drugs: prolonged QTc interval, torsade de pointes, and sudden death. Am J Psychiatry. 2001;158:1774–82. doi: 10.1176/appi.ajp.158.11.1774. [DOI] [PubMed] [Google Scholar]
- 18.Hartigan-Go K, Bateman DN, Nyberg G, Martensson E, Thomas SH. Concentration-related pharmacodynamic effects of thioridazine and its metabolites in humans. Clin Pharmacol Ther. 1996;60:543–53. doi: 10.1016/S0009-9236(96)90150-2. [DOI] [PubMed] [Google Scholar]
- 19.Lee JW, Rogers SL, Freidhoff LT, Stiles MR, Cooper NM. Validation and application of an HPLC method for the determination of 1-benzyl-4-[(5,6-dimethoxy-1-indanon)-2-yl] methyl piperidine (E2020) in human plasma. Pharm Res. 1992;9:S350. [Google Scholar]
- 20.Committee for Proprietary Medicinal Products (CPMP) Note for Guidance Investigation of bioavailability and bioequivalence. European Union; 1991. III/54/89. [Google Scholar]
- 21.Schuirmann DJ. A comparison of the two one-sided tests procedure and power approach for assessing equivalence of average bioavailability. J Pharmacokin Biopharmacol. 1987;15:657–80. doi: 10.1007/BF01068419. [DOI] [PubMed] [Google Scholar]
- 22.Tiseo PJ, Perdomo CA, Freidhoff LT. Concurrent administration of donepezil and cimetidine: assessment of pharmacokinetic changes following single and multiple doses. Br J Clin Pharmacol. 1998;46(Suppl. 1):25–9. doi: 10.1046/j.1365-2125.1998.0460s1025.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tiseo PJ, Perdomo CA, Freidhoff LT. Concurrent administration of donepezil and ketoconazole: assessment of pharmacokinetic changes following single and multiple doses. Br J Clin Pharmacol. 1998;46(Suppl. 1):30–4. doi: 10.1046/j.1365-2125.1998.0460s1030.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tiseo PJ, Foley K, Freidhoff LT. Concurrent administration of donepezil and theophylline: assessment of pharmacokinetic changes following multiple-dose administration in healthy volunteers. Br J Clin Pharmacol. 1998;46(Suppl. 1):35–9. doi: 10.1046/j.1365-2125.1998.0460s1035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tiseo PJ, Perdomo CA, Freidhoff LT. Concurrent administration of donepezil and digoxin: assessment of pharmacokinetic changes. Br J Clin Pharmacol. 1998;46(Suppl. 1):40–4. doi: 10.1046/j.1365-2125.1998.0460s1040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tiseo PJ, Foley K, Freidhoff LT. The effect of multiple doses of donepezil on the pharmacokinetic and pharmacodynamic profile of warfarin. Br J Clin Pharmacol. 1998;46(Suppl. 1):45–50. doi: 10.1046/j.1365-2125.1998.0460s1045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.BMA. British National Formulary. Royal Pharmaceutical Society of Great Britain:; Number 34, September 1997. [Google Scholar]