Abstract
Aim
To assess recent trends in undertreatment of hypercholesterolaemia (1998–2002).
Methods
Data were obtained from the third cross-sectional examination of the Monitoring Project on Risk Factors for Chronic Diseases (n = 4878; age 31–70 years), conducted in the Netherlands. Treatment eligibility was established according to Dutch guidelines. Data from the second examination (1993–1997) were used to assess time trends. The association between demographic variables, cardiovascular disease risk factors, drug use and lipid-lowering medication was assessed using multivariable logistic regression.
Results
Overall, 45.9%[95% confidence interval (CI) 41.4, 50.4] of respondents eligible for treatment were treated, and 17.4% (95% CI 13.9, 20.9) were both treated and controlled (1998–2002). Treatment increased significantly after 1995, showed a slight decrease in subsequent years until 2000, when treatment increased again. Subgroups less frequently treated for primary prevention included among others males [odds ratio (OR) = 0.08; 95% CI 0.03, 0.21], younger patients (OR = 0.93 per year; 95% CI 0.88, 0.98), diabetics (OR = 0.19; 95% CI 0.07, 0.56), untreated hypertensives (OR = 0.21; 95% CI 0.09, 0.49) and current smokers (OR = 0.09; 95% CI 0.03, 0.25). In secondary prevention, patients with a history of stroke were less likely to receive treatment (OR = 0.41; 95% CI 0.18, 0.94) compared with patients with a history of ischaemic heart disease.
Conclusions
Treatment of hypercholesterolaemia has steadily increased over the past 10 years in the Netherlands. However, at present still less than one out of two eligible for treatment is treated, and only about one out of six is both treated and controlled.
Keywords: antilipaemic agents, cardiovascular diseases, drug therapy, hypercholesterolaemia
Introduction
HMG-CoA reductase inhibitors have proven to be safe and effective in reducing cardiovascular events [1]. Many guidelines on the management of hypercholesterolaemia have been revised over the last 5 years [2–4]. Previously, we reported substantial undertreatment of hypercholesterolaemia in the general Dutch population during the period 1987–1997 [5]. Publications on adherence to guidelines on the management of hypercholesterolaemia are lacking for recent years [6], or focused on patients with ischaemic heart disease (IHD) only [7].
The aim of the present study was to assess undertreatment of hypercholesterolaemia over the period 1998–2002 among subjects living in a single subarea (Doetinchem) of the population-based Monitoring Project on Risk Factors for Chronic Diseases in the Netherlands.
Methods
Data were obtained from the third cross-sectional examination of the population-based Monitoring Project on Risk Factors for Chronic Diseases (MORGEN). This third examination was conducted between 1998 and 2002 among 4920 subjects living in a single subarea (Doetinchem) of the MORGEN project in the Netherlands who also participated in the first (1987–1991) and second (1993–1997) examination [5]. All respondents (now age 31–70 years) completed a questionnaire containing questions on demographic variables, cardiovascular disease (CVD) risk factors and current use of medication.
Additionally, height, weight and blood pressure were measured and blood was drawn (nonfasting) for total cholesterol (TC) and high-density lipoprotein cholesterol (HDLC) determination. Total and HDLC determinations were performed in the Lipid Reference Laboratory (LRL) of the University Hospital Dijkzigt in Rotterdam. A random zero sphygmomanometer was used to measure blood pressure twice by a trained technician (after 5 min) with the subject in an upright position. Information on other cardiovascular risk factors, e.g. smoking status, diabetes and a family history of CVD, were obtained from the questionnaire.
In the screening projects, lipid-lowering drug use was recorded in two ways. First, respondents were asked if they used medication to lower their cholesterol levels, and second, respondents were asked to specify the drug(s) they were using. In the period 1993–1997, lipid-lowering drug use was verified by checking the registered indications of the drug(s) listed by the respondent. Drug use was confirmed in this way in 90.8% of all subjects reporting the use of lipid-lowering treatment [5]. Therefore, all participants reporting the use of lipid-lowering medication were considered pharmacologically treated for hypercholesterolaemia in both our previous and our present study. In the period 1993–1997, approximately 90% of all patients used at least a statin.
Treatment eligibility was established for all respondents according to the Dutch Consensus Cholesterol 1998 [2]. This guideline, which is similar to the European guidelines [3], indicates pharmacological treatment for primary prevention when the absolute level of risk exceeds an age- and gender-specific cut-off point (based on the Framingham risk function), and for secondary prevention, unless TC ≤5 mmol l−1. Secondary prevention was defined as a history of myocardial infarction, stroke, coronary artery bypass grafting or percutaneous transluminal coronary angioplasty. Subjects already using lipid-lowering drugs were considered to be eligible for treatment. Undertreatment was defined as inappropriately not receiving lipid-lowering medication, or TC >5 mmol l−1 among treated hypercholesterolaemic patients. These methods have previously been described in detail elsewhere [5].
Prevalence of treatment and control of hypercholesterolaemia (Tc ≤5 mmol l−1) and 95% confidence intervals (CI) were estimated and standardized to the age and gender distribution of the general Dutch population on 1 January 2000. For the present study, we used data from subjects living in Doetinchem and participating in the second cross-sectional examination (1993–1997) of the survey to assess time trends in treatment of hypercholesterolaemia for overlapping age categories (30–59 years). Multivariable logistic regression models were used to assess the association between demographic variables, CVD risk factors, medication use and treatment with lipid-lowering drugs (separate analyses for primary and secondary prevention).
Results
After exclusion of pregnant women (n = 18) and subjects with missing data (n = 24), 4878 subjects remained for the analysis. Overall, almost three out of four respondents had suboptimal cholesterol concentrations (TC >5 mmol l−1). Of the 471 respondents eligible for treatment with lipid-lowering drugs (11% of those with suboptimal cholesterol levels), only 217 (45.9%) were treated and 79 (17.4%) were both treated and controlled (see Table 1). More women (53.6%) than men (42.3%) were treated, but if men were treated, they were better controlled than women. Being treated and controlled among those eligible for treatment was therefore similar for both sexes. Overall, only 37.8% of all respondents treated for hypercholesterolaemia achieved TC ≤5 mmol l−1.
Table 1.
Prevalence and 95% confidence intervals of suboptimal cholesterol concentrations, eligibility for treatment, treated and controlled hypercholesterolaemia in men and women living in a single subarea (Doetinchem) of the MORGEN project in the Netherlands
| Respondents | Suboptimal cholesterol concentrations (TC >5 mmol l–1) | Eligible for treatment* (including those treated) | Treated | Controlled† | |
|---|---|---|---|---|---|
| Overall | 4878 | 3708 (72.8%; 71.5, 74.0) | 471 (11.0%; 10.0, 12.0) | 217 (45.9%; 41.4, 50.4) | 79 (37.8%; 31.4, 44.3/17.4%; 13.9, 20.8) |
| Men | |||||
| 31–70 years | 2338 | 1823 (75.4%; 73.7, 77.2) | 322 (14.4%; 12.8, 16.1) | 137 (42.3%; 37.0, 47.7) | 57 (43.2%; 34.9, 51.5/18.3%; 14.1, 22.5) |
| Women | |||||
| 31–70 years | 2540 | 1885 (70.1%; 68.3, 71.8) | 149 (7.3%; 6.1, 8.4) | 80 (53.6%; 45.5, 61.6) | 22 (28.6%; 18.7, 38.5/15.3%; 9.5, 21.1) |
| Primary prevention‡ | 4599 | 3476 (75.6%; 70.5, 80.6) | 239 (6.9%; 6.0, 7.7) | 114 (47.7%; 41.4, 54.0) | 27 (23.7%; 15.9, 31.5/11.3%; 7.3, 15.3) |
| Secondary prevention‡ | 279 | 232 (83.2%; 78.8, 87.5) | 232 (100%) | 103 (44.4%; 38.0, 50.8) | 52 (50.5%; 40.8, 60.1/22.4%; 17.0, 27.8) |
All estimates are weighted by the age and gender distribution of the general Dutch population on 1 January 2000.
Based on the Dutch Consensus on Cholesterol (1998).
Percentage of those treated and percentage of those eligible for treatment, respectively.
Adjustment for age and gender distribution not possible, because data on the age and gender distribution of the Dutch population among those with or without pre-existing coronary heart disease were not available.
Frequency of treatment was similar in primary and secondary prevention (47.7 and 44.4%, respectively). However, being treated and controlled was more prevalent among those eligible for secondary prevention (22.4%vs. 11.3% in primary prevention). Stratification by gender yielded remarkable results. In primary prevention, 82.4% of all women eligible for treatment (n = 68) were treated, but only 33.9% of men eligible for treatment (n = 58) received treatment. The opposite result was observed in secondary prevention. Among those eligible for treatment, more men (52.3%) than women (29.6%) were using lipid-lowering medication. In both primary and secondary prevention, serum lipid levels were more frequently controlled in treated men (51.9 and 27.6%, respectively) than in women (45.8 and 19.6%, respectively).
Treatment increased significantly after 1995, and showed a slight decrease in subsequent years until 2000, when treatment increased again (Figure 1). Male patients [odds ratio (OR) =0.08; 95% CI 0.03, 0.21], younger patients (OR = 0.93 per year; 95% CI 0.88, 0.98), patients with diabetes mellitus (OR = 0.19; 95% CI 0.07, 0.56), untreated hypertensives (OR = 0.21; 95% CI 0.09, 0.49), patients with a family history of CVD (OR = 0.35; 95% CI 0.14, 0.91), and current smokers (OR = 0.09; 95% CI 0.03, 0.25) were less frequently treated for primary prevention (see Figure 2A). Antihypertensive drug use was nonsignificantly associated with lipid-lowering treatment (OR = 1.22; 95% CI 0.50, 2.98). In secondary prevention, male gender (OR = 2.81; 95% CI 1.35, 5.82) was strongly associated with lipid-lowering drug use, whereas age was of no influence (Figure 2B). In diabetics eligible for secondary prevention we observed a trend towards more treatment compared with nondiabetics eligible for secondary prevention (OR = 2.23; 95% CI 0.72, 6.95). Compared with patients with IHD only, patients with a stroke were less likely to receive lipid-lowering drugs (OR = 0.41; 95% CI 0.18, 0.94).
Figure 1.
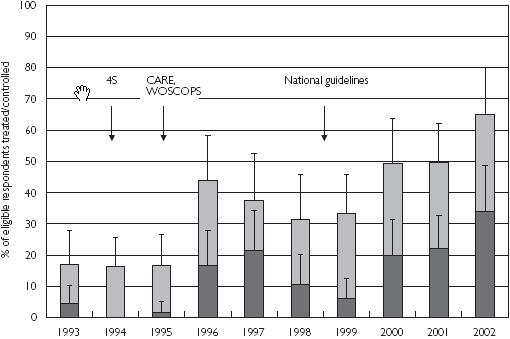
Treatment of hypercholesterolaemia in a single subarea (Doetinchem) of the MORGEN project in the period 1993–2002 among those aged 30–59 years and eligible for pharmacological treatment of hypercholesterolaemia, weighted by the age and gender distribution of the general Dutch population on 1 January 2000. Treated ( ), Treated and controlled (
), Treated and controlled ( )
)
Figure 2.
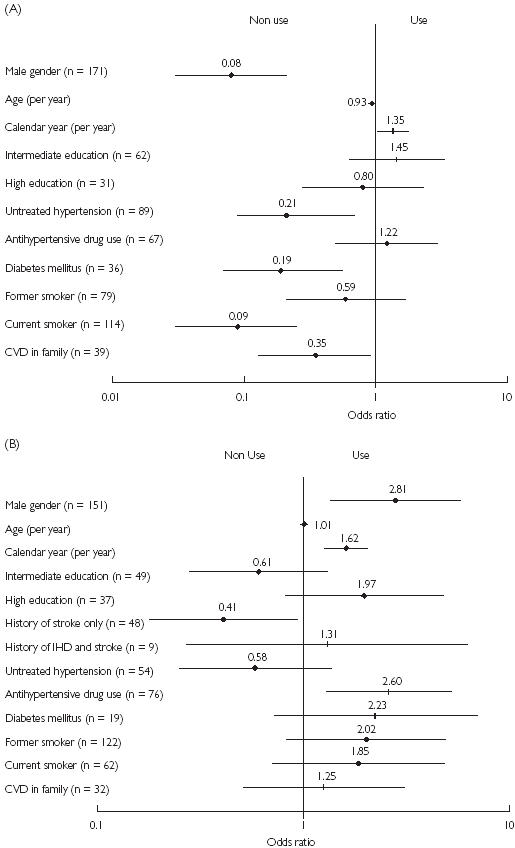
Determinants of use of lipid-lowering drugs among those eligible for primary prevention (A) (n = 239) and secondary prevention (B) (n = 232). All odds ratios are adjusted for demographic variables, cardiovascular risk factors and medication use.
Discussion
Treatment of hypercholesterolaemia in those eligible for treatment according to current guidelines has steadily increased over the past 10 years in the Netherlands. However, at present still less than one out of two persons is treated, and only about one out of six is both treated and controlled.
Our results indicate a lag time of about 1–2 years before an increase in treatment of hypercholesterolaemia can be observed after the publication and dissemination of the first landmark trials on the treatment of hypercholesterolaemia (1994/1995), but also after the publication of national guidelines (1998/1999). Another rise in treatment rate occurred after 2001. This increase may reflect an intensified focus on serum cholesterol levels as one of the most important risk factors for CVD by healthcare professionals. A similar time trend has previously been observed in Ireland [8]. In this study, lipid-lowering drug use increased rapidly after the publication of the first pivotal trials, but did not meet the total target population. Additionally, HMG-CoA reductase inhibitors were initially not prescribed to the population most likely to benefit from them.
Substantial undertreatment of hypercholesterolaemia has been observed in both primary and secondary prevention [6, 7, 9–11]. We observed similar rates in secondary prevention compared with an English national survey conducted between 1994 and 2001 [7], but others described higher rates of undertreatment [9, 11]. Ford et al. reported that only 12% of the United States population ≥20 years with elevated total cholesterol levels (TC > 5.2 mmol l−1) were receiving cholesterol-lowering medication [6]. This percentage is far lower than the proportion treated for primary prevention that we present here. One possible explanation is that our data were obtained from the third cross-sectional examination of a single subarea of a national survey. After the first and second round, abnormalities in blood pressure or cholesterol levels have been reported to a subject's general practitioner (GP) if informed consent was obtained. GPs may have responded to these reports by prescribing cholesterol-lowering drugs. In the general Dutch population, treatment rates may therefore be lower than in this survey. Another explanation for the relatively high treatment rates in women compared with men, and in primary prevention compared with secondary prevention, is that overtreatment may have occurred in these subgroups.
In both primary and secondary prevention, men had their serum cholesterol levels more frequently controlled if they were treated, suggesting a more aggressive treatment approach in men. Gender differences in treatment goal attainment have been reported previously. British data from 17 primary care groups showed that 43.2% of women treated with lipid-lowering drugs achieved serum cholesterol concentrations ≤5 mmol l−1, compared with 61.9% of men [12].
In primary prevention, the same subgroups of patients were undertreated for hypercholesterolaemia as in the period 1987–1997 [5]. Although the association was still strong, male gender, diabetes mellitus and untreated hypertension were less strongly associated than in the previous study period, suggesting an increase in treatment rates in these subgroups. Women visit their physicians more frequently [13, 14], and may therefore be more likely to receive lipid-lowering drugs. Whether all women already treated with lipid-lowering drugs were eligible for treatment according to the Dutch guidelines could not be assessed because of the lack of pretreatment cholesterol levels. As many of the women treated for primary prevention had a limited number of other cardiovascular risk factors, overtreatment might have occurred in this subgroup, which would add to the relative undertreatment of men in primary prevention.
Undertreatment of hypercholesterolaemia is especially alarming in patients with Type 2 diabetes mellitus, because they are at considerable risk of CVD [15]. Patients with diabetes mellitus were less frequently undertreated in this study period compared with the previous study period [5]. Several other studies have reported an increase in lipid-lowering drug use among diabetic patients [16, 17]. Although smoking cessation effectively reduces CVD risk [18], smokers are more frequently eligible for lipid-lowering drug use since they have a high absolute risk of CVD. Undertreatment of smokers may indicate that physicians do not seem to focus on this important risk factor or that physicians may be reluctant to initiate lipid-lowering drug use in patients who continue to smoke. The undertreatment of patients with multiple cardiovascular risk factors may indicate that physicians still tend to treat patients with high cholesterol levels as a single risk factor instead of focusing on a multifactorial approach.
Male gender is now strongly positively associated with treatment in secondary prevention, whereas age is no longer a determinant. The opposite result was observed in the English survey conducted between 1994 and 2001 [7]. This survey included earlier years than presented in the present study. In our previous study over the period 1987–1997, we also found that the elderly were less likely to receive treatment. Patients with a stroke were even more undertreated for hypercholesterolaemia than patients with coronary events. This is of major concern since patients with stroke and TC > 5 mmol l−1 are all eligible for cholesterol-lowering treatment according to the Dutch guidelines, and treatment with statins can reduce the risk of stroke by approximately 20% according to the results of a recent meta-analysis [19]. The role of cholesterol in stroke, however, has been debated vigorously in literature during the study period [20, 21].
Although results of the MRC/BHF Heart Protection Study (HPS) and the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA) indicate that HMG-CoA reductase inhibitors are also efficacious in subjects with average cholesterol levels [22, 23], our first goal should be to reduce the risk of patients with a high absolute risk. Implementation of guidelines on the management of hypercholesterolaemia should therefore be reinforced. The estimated number of patients eligible for pharmacological treatment of hypercholesterolaemia in the Netherlands is 300 000–530 000 according to the Dutch guidelines. The drug costs involved in the treatment of all these patients based on the current prices of statins would be approximately €200 million per year, which is less than the amount of money spent on statins in 2002 (€286 million) [24].
The focus on the pharmacological treatment of hypercholesterolaemia as in the present study should not hold physicians back from encouraging their patients eligible for lipid-lowering therapy to initiate and adhere to dietary changes, as advocated by all guidelines on the management of hypercholesterolaemia [2–4], and other lifestyle modifications. However, HMG-CoA reductase inhibitors substantially reduce the absolute CVD risk in these high-risk patients and pharmacological treatment of hypercholesterolaemia is therefore warranted. Any possible risks associated with the use of HMG-CoA reductase inhibitors, including myopathy and rhabdomyolysis [25], are by far outweighed by their beneficial effects in patients eligible for lipid-lowering therapy according to current guidelines [1, 22]. Data on long-term use of HMG-CoA reductase inhibitors, e.g. >10–15 years, are necessary to establish long-term safety of these drugs. Until then, there are no reasons to withhold these drugs from patients at high cardiovascular risk.
This study showed that at present still less than one out of two persons eligible for lipid-lowering treatment is treated, and only about one out of six is both treated and controlled. We should focus on patients at high risk for cardiovascular events, e.g. those eligible for secondary prevention and patients with diabetes or similar high risk in primary prevention. Otherwise, the benefits of lipid-lowering drugs will be far less than promised by clinical trials.
References
- 1.LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282:2340–6. doi: 10.1001/jama.282.24.2340. [DOI] [PubMed] [Google Scholar]
- 2.Jukema JW, Simoons ML. Treatment and prevention of coronary heart disease by lowering serum cholesterol levels; from the pioneer work of C.D. de Langen to the third ‘Dutch Consensus on Cholesterol’. Acta Cardiol. 1999;54:163–8. [PubMed] [Google Scholar]
- 3.Second Joint Task Force of European and other Societies. Prevention of coronary heart disease in clinical practice. Recommendations of the Second Joint Task Force of European and other Societies on coronary prevention. Eur Heart J. 1998;19:1434–503. doi: 10.1053/euhj.1998.1243. [DOI] [PubMed] [Google Scholar]
- 4.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 5.Mantel-Teeuwisse AK, Verschuren WMM, Klungel OH, et al. Undertreatment of hypercholesterolaemia: a population-based study. Br J Clin Pharmacol. 2003;55:389–97. doi: 10.1046/j.1365-2125.2003.01769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999–2000. Circulation. 2003;107:2185–9. doi: 10.1161/01.CIR.0000066320.27195.B4. [DOI] [PubMed] [Google Scholar]
- 7.DeWilde S, Carey IM, Bremner SA, Richards N, Hilton SR, Cook DG. Evolution of statin prescribing 1994–2001: a case of agism but not of sexism? Heart. 2003;89:417–21. doi: 10.1136/heart.89.4.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feely J, McGettigan P, Kelly A. Growth in use of statins after trials is not targeted to most appropriate patients. Clin Pharmacol Ther. 2000;67:438–41. doi: 10.1067/mcp.2000.105152. [DOI] [PubMed] [Google Scholar]
- 9.Primatesta P, Poulter NR. Lipid concentrations and the use of lipid lowering drugs: evidence from a national cross sectional survey. Br Med J. 2000;321:1322–5. doi: 10.1136/bmj.321.7272.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.EUROASPIRE I and II Group. Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries. EUROASPIRE I and II Group. European Action on Secondary Prevention by Intervention to Reduce Events. Lancet. 2001;357:995–1001. doi: 10.1016/s0140-6736(00)04235-5. [DOI] [PubMed] [Google Scholar]
- 11.Ruof J, Klein G, Marz W, Wollschlager H, Neiss A, Wehling M. Lipid-lowering medication for secondary prevention of coronary heart disease in a German outpatient population: the gap between treatment guidelines and real life treatment patterns. Prev Med. 2002;35:48–53. doi: 10.1006/pmed.2002.1050. [DOI] [PubMed] [Google Scholar]
- 12.Hippisley-Cox J, Cater R, Pringle M, Coupland C. Cross sectional survey of effectiveness of lipid lowering drugs in reducing serum cholesterol concentration in patients in 17 general practices. Br Med J. 2003;326:689–93. doi: 10.1136/bmj.326.7391.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stoverinck MJ, Lagro-Janssen AL, Weel CV. Sex differences in health problems, diagnostic testing, and referral in primary care. J Fam Pract. 1996;43:567–76. [PubMed] [Google Scholar]
- 14.Nathanson CA. Sex, illness, and medical care. A review of data, theory, and method. Soc Sci Med. 1977;11:13–25. doi: 10.1016/0037-7856(77)90141-x. [DOI] [PubMed] [Google Scholar]
- 15.Saydah SH, Eberhardt MS, Loria CM, Brancati FL. Age and the burden of death attributable to diabetes in the United States. Am J Epidemiol. 2002;156:714–9. doi: 10.1093/aje/kwf111. [DOI] [PubMed] [Google Scholar]
- 16.Safford M, Eaton L, Hawley G, et al. Disparities in use of lipid-lowering medications among people with type 2 diabetes mellitus. Arch Intern Med. 2003;163:922–8. doi: 10.1001/archinte.163.8.922. [DOI] [PubMed] [Google Scholar]
- 17.Wandell PE, Gafvels C. Drug prescription in men and women with type-2 diabetes in Stockholm in 1995 and 2001: change over time. Eur J Clin Pharmacol. 2002;58:547–53. doi: 10.1007/s00228-002-0510-1. [DOI] [PubMed] [Google Scholar]
- 18.Critchley JA, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA. 2003;290:86–97. doi: 10.1001/jama.290.1.86. [DOI] [PubMed] [Google Scholar]
- 19.Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. Br Med J. 2003;326:1423–9. doi: 10.1136/bmj.326.7404.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Demchuk AM, Hess DC, Brass LM, Yatsu FM. Is cholesterol a risk factor for stroke?: Yes. Arch Neurol. 1999;56:1518–20. doi: 10.1001/archneur.56.12.1518. [DOI] [PubMed] [Google Scholar]
- 21.Landau WM. Is cholesterol a risk factor for stroke? Arch Neurol. 1999;56:1521–4. doi: 10.1001/archneur.56.12.1521. [DOI] [PubMed] [Google Scholar]
- 22.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 23.Sever PS, Dahlof B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–58. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- 24.Stichting Farmaceutische Kengetallen. Data en feiten 2003. Den Haag: SFK; 2003. [Google Scholar]
- 25.Gaist D, Garcia Rodriguez LA, Huerta C, Hallas J, Sindrup SH. Lipid-lowering drugs and risk of myopathy: a population-based follow-up study. Epidemiology. 2001;12:565–9. doi: 10.1097/00001648-200109000-00017. [DOI] [PubMed] [Google Scholar]


