Abstract
Aims
Previous studies of the prescription patterns of psychotropic medications in patients with schizophrenia have highlighted a high rate of antipsychotic polypharmacy, but data in Asia are sparse. This study seeks to examine the prevalence of antipsychotic polypharmacy in patients with schizophrenia and compare the differences between patients receiving one vs. those receiving more than one antipsychotic.
Methods
Antipsychotic prescription for a sample of 2399 patients with schizophrenia from six countries and territories was evaluated. Daily doses of antipsychotic medications were converted to standard chlorpromazine equivalents (CPZ).
Results
Antipsychotic polypharmacy was found in 45.7% (n = 1097) of the patients with wide intercountry variations. Polypharmacy was associated with male gender [odds ratio (OR) 1.24, 95% confidence interval (CI) 1.06, 1.46, P < 0.01], advanced age (t = −7.81, d.f. = 2396, P < 0.001), psychiatric hospital setting (OR 1.34, 95% CI 1.11, 1.62) as well as higher daily CPZeq doses (411.47 vs. 983.10 CPZeq day−1, z = −25.94, P < 0.001), anticholinergic use (OR 3.17, 95% CI 2.65, 3.79, P < 0.001) and less use of an atypical antipsychotic drug (OR 0.83, 95% CI 0.71, 0.98, P < 0.05). On multivariate analysis, country, age and duration of illness were significantly associated with antipsychotic polypharmacy.
Conclusion
This study highlighted the wide intercountry variations of antipsychotic polypharmacy which are likely to be influenced by a complex combination of clinical, setting, cultural and personal practice factors, requiring more research.
Keywords: antipsychotic, Asia, comparative, polypharmacy, schizophrenia
Introduction
Previous studies of the prescription patterns of antipsychotic drugs in patients with psychotic disorders including schizophrenia have revealed widely variable rates (13–90%) of antipsychotic polypharmacy, defined as the use of more than one antipsychotic [1–5]. The wide variation in the rates of combination antipsychotic therapy between countries has been attributed to differences in healthcare systems affecting availability and economic cost of antipsychotics [6], local prescription traditions and culture as well as personal experience and choice [7]. Antipsychotic polypharmacy is associated with more frequent use of adjunctive medications such as anticholinergic drugs [8], higher daily dosing [9], higher rate of adverse effects and underutilization of atypical antipsychotic medications [3, 4]. There has been a constant call for more rational psychopharmacotherapy [10, 11] in the management of patients with schizophrenia, with the purpose of optimizing the treatment without compromising on the side-effect burden as well as its impact on the patients’ quality of life.
Several multicentre surveys have examined the issue of antipsychotic polypharmacy in Europe and the USA [3, 9, 10, 12]. To the best of our knowledge, there has been no large, systematic study elucidating its comparative prevalence in Asia. Hence the current study aims to evaluate the prevalence of antipsychotic polypharmacy in patients with schizophrenia in East Asia and compare patients given one antipsychotic with those given more than one antipsychotic with respect to a host of sociodemographic and clinical variables.
Methods
Design and participants
A cross-sectional, case record audit study was conducted in July 2001 involving a sample of 2399 inpatients diagnosed with schizophrenia at 32 centres in six East Asian countries and territories (China, Hong Kong, Japan, Korea, Singapore, and Taiwan) using a standardized data collection form. Previous reports had also compared the prescription patterns of inpatients with schizophrenia among psychiatric units in countries with different socio-cultural backgrounds and psychiatric traditions as well as patients of different ethnicities [10, 13]. The rationale for the collection of such international data is supported by the current widespread acceptance of the DSM-IV [14] and ICD-10 [15] which had led to a greater consistency in the diagnosis of schizophrenia. The data were collected from the inpatient psychiatric units serving a defined population within a corresponding catchment area: the Institute of Mental Health, Beijing Medical University (Beijing, China), the Prince of Wales Hospital, Chinese University of Hong Kong (Hong Kong), the Department of Psychiatry, Kobe University School of Medicine (Kobe, Japan), the Seoul National Hospital (Seoul, Korea), the Institute of Mental Health (Singapore) and Department of Psychiatry, Kaohsiung University (Kaohsiung County, Taiwan).
Patients who were selected fulfilled the diagnostic criteria for schizophrenia according to the ICD-10 or DSM-IV. One hundred and fifty medical records were excluded from analysis as the demographic, medical or drug treatment data were incomplete. Five consensus meetings were held before the study to discuss issues related to methodological issues such as data collection and uniform data entry. Background information collected from the case records included age, gender, duration of illness, treatment setting and type and dose of psychotropic medications prescribed by the psychiatrists.
Daily doses of antipsychotics, including depot antipsychotics, were converted to approximate chlorpromazine equivalents (CPZeq) using published guidelines [16–18]. The study was approved by the Research and Ethics Committees of all the co-ordinating centres.
Statistical analysis
Averages are reported as means ± standard deviation (SD), and relative risks are reported as odds ratios (OR) with their 95% confidence intervals (CIs). Analyses were performed with the Statistical Package for Social Sciences (SPSS) version 11.0 (SPSS Inc., Chicago, IL, USA). The normality of distributions of continuous measures was checked with the Kolmogorov–Smirnov one-sample test. Differences between groups were tested by Student's t-test and one-way anova for normally distributed data, Mann–Whitney U-tests for non-normally distributed continuous data, and by contingency tables (χ2) for categorical variables. Multiple logistic regression was carried out to adjust for relevant covariates and to determine the predictors of antipsychotic polypharmacy. Statistical significance was set at two-tailed P < 0.05.
Results
Demographic and clinical characteristics
The case records of 2399 patients were examined. Table 1 presents the demographic and clinical characteristics of the sample. Overall, antipsychotic polypharmacy was found in the treatment regimens of 45.7% (n = 1097) of the patients, being most common in Japan, followed by Singapore, Korea, China, Taiwan and Hong Kong. Using Hong Kong as a reference, antipsychotic polypharmacy was more likely to occur in Japan (OR 26.89, 95% CI 14.61, 49.49, P < 0.001), Singapore (OR 17.33, 95% CI 9.22, 32.54, P < 0.001), Korea (OR 4.03, 95% CI 2.18, 7.42, P < 0.001) and China (OR 2.46, 95% CI 1.34, 4.52, P < 0.01). The three antipsychotics most commonly prescribed in cases of polypharmacy in the following countries were: Japan (haloperidol, levomepromazine, chlorpromazine), Singapore (chlorpromazine, haloperidol, trifluoperazine), Korea (chlorpromazine, haloperidol, risperidone), China (clozapine, risperidone, chlorpromazine), Taiwan (haloperidol, chlorpromazine, haloperidol decanoate) and Hong Kong (trifluoperazine, sulpiride, chlorpromazine).
Table 1.
Demographic and clinical characteristics (N = 2399)
| N | Japan 627 | Singapore 300 | Korea 442 | China 611 | Taiwan 311 | Hong Kong 108 | P-value |
|---|---|---|---|---|---|---|---|
| Age (years) | |||||||
| Mean | 52.9b,c,d,e,f | 46.2a,c,d,e | 39.1a,b,f | 38.5a,b,f | 38.2a,b,f | 45.4a,c,d,e | <0.001† |
| SD | 13.5 | 10.8 | 9.5 | 12.9 | 10.8 | 13.5 | |
| Gender | |||||||
| Male (%) | 58.4 | 58.7 | 57.0 | 50.9 | 55.6 | 58.3 | NS |
| Female (%) | 41.6 | 41.3 | 43.0 | 49.1 | 44.4 | 41.7 | |
| Duration of illness (%) | |||||||
| <1 year | 2.7 | 1.3 | 3.9 | 11.5 | 1.0 | 0 | <0.001‡ |
| 1–5 years | 6.7 | 7.3 | 12.0 | 20.4 | 12.8 | 7.4 | |
| 6–10 years | 7.9 | 18.3 | 25.8 | 15.1 | 25.7 | 13.9 | |
| 11–20 years | 16.9 | 41.0 | 40.7 | 24.8 | 34.9 | 25.9 | |
| >20 years | 65.8 | 32.0 | 17.7 | 28.1 | 25.7 | 52.8 | |
| Antipsychotic polypharmacy (%) | 78.6b,c,d,e,f | 70.3a,c,d,e,f | 35.5a,b,d,e,f | 25.2a,b,c,f | 22.2a,b,c | 12.0a,b,c,d | <0.001‡ |
| Atypical antipsychotic anticholinergic use (%) | 50.4b,c,d | 6.7a,c,d,e,f | 37.1a,b,d | 64.0a,b,c,e,f | 48.6b,d | 46.3b,d | <0.001‡ |
| Treatment setting | 78.0d | 82.0d,e | 76.0d | 34.7a,b,c,e,f | 61.4b,d | 50.0d | <0.001‡ |
| (Psychiatric hospital, %) | 78.1 | 100.0 | 38.7 | 67.3 | 100.0 | 100.0 | <0.001‡ |
P-values derived from anova test.
P-values derived from χ2test.
Significant differences in post hoc analysis when compared with Japan, Singapore, Korea, China, Taiwan and Hong Kong, respectively.
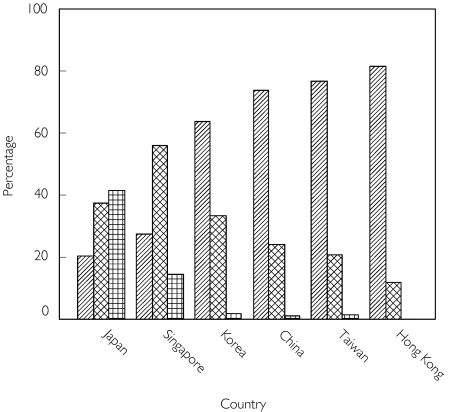
Figure 1 shows the number of antipsychotics prescribed in the participating countries and territories.
Figure 1.
Number of antipsychotics prescribed.  # = 1,
# = 1,  # = 2,
# = 2,  # ≥ 3
# ≥ 3
Correlates of antipsychotic polypharmacy
Table 2 compares the characteristics of patients receiving one antipsychotic with those receiving more than one antipsychotic. Being on a polypharmacy regime was associated with advanced age, male gender, treatment in a psychiatric hospital setting (as opposed to a general hospital psychiatric unit), increased use of anticholinergic as well as decreased use of atypical antipsychotic medications.
Table 2.
Comparison of characteristics between patients on one antipsychotic (NP) and patients on more than one antipsychotic (P)
| NP (n = 1302) | P (n = 1097) | Test statistic | P | |
|---|---|---|---|---|
| Age (years) | t = −7.81,d.f. = 2396 | <0.001 | ||
| Mean | 41.66 | 45.93 | ||
| SD | 13.74 | 12.82 | ||
| Daily CPZeq (mg day−1) | 411.47 | 983.10 | Z = −25.94 | <0.001 |
| Duration of illness* | χ2 = 68.28 | <0.001 | ||
| <1 year | 78 (6.00) | 33 (3.00) | ||
| 1–5 years | 199 (15.30) | 103 (9.40) | ||
| 6–10 years | 251 (19.30) | 152 (13.90) | ||
| 11–20 years | 369 (28.30) | 324 (29.50) | ||
| >20 years | 405 (31.10) | 485 (44.20) |
| OR (95% CI) | P | |||
|---|---|---|---|---|
| Gender* | ||||
| Female | 606 (46.50) | 452 (41.20) | 1.00 | |
| Male | 696 (53.50) | 645 (58.80) | 1.24 (1.06, 1.46) | <0.01 |
| Treatment setting | ||||
| General hospital | 363 (72.10) | 245 (22.30) | 1.00 | |
| Psychiatric hospital | 939 (27.90) | 852 (77.70) | 1.34 (1.11, 1.62) | <0.01 |
| First admission* | ||||
| No | 1058 (81.26) | 898 (81.90) | – | |
| Yes | 244 (18.74) | 199 (18.10) | – | NS |
| Medication use* | ||||
| Atypical antipsychotic | 620 (47.60) | 472 (43.00) | 0.83 (0.71, 0.98) | <0.05 |
| Anticholinergic drugs | 678 (52.10) | 850 (77.50) | 3.17 (2.65, 3.79) | <0.001 |
CPZeq, Chlorpromazine equivalents.
The figures are number of patients with percentage in parentheses.
Using multiple logistic regression analysis and adjusting for covariates (country, age, gender, duration of illness, psychiatric hospital treatment setting and atypical antipsychotic use), factors that were significantly associated with antipsychotic polypharmacy were country, younger age and longer duration of illness.
Discussion
We found that the prevalence of antipsychotic polypharmacy was high in some parts but low in other parts of East Asia, highlighting significant intercountry variations in this prescription practice. Polypharmacy was associated with sociodemographic features (age, being male), clinical features (longer duration of illness, psychiatric hospital setting) and medication use (increased anticholinergic and decreased atypical antipsychotic use).
The wide intercountry rates of antipsychotic polypharmacy are consistent with those reported in the literature [3]. The high rate of antipsychotic polypharmacy in Japan (78.6%) within this study is comparable to the findings of Ito et al.[1], who reported that up to 90% of patients with schizophrenia in several public hospitals were receiving combination antipsychotic therapy. The similar high rate in Singapore (70.3%) was slightly greater than that found in an earlier study (59.0%) [19], suggesting that such a trend persists over time for patients with schizophrenia admitted to a psychiatric hospital.
The higher rates of antipsychotic polypharmacy may be related to the treatment setting, since a psychiatric hospital has a higher likelihood of admitting more seriously ill patients compared with a general hospital psychiatric unit. The combination of more than one antipsychotic may be an attempt at preventing the rapid escalation of the dose of any single medication [20] or as an alternative towards the management of treatment unresponsiveness or partial response [21]. However, in this study the rates of antipsychotic polypharmacy in Taiwan and Hong Kong were considerably lower compared with the other countries despite their patients being recruited from psychiatric hospitals, suggesting that other factors also are likely to be important, including local prescribing traditions and cultural factors.
Polypharmacy may indicate a slow cross-tapering from one antipsychotic to another, or that patients were stuck in the combination during the process of cross titration of polypharmacy [5, 22]. The association of antipsychotic polypharmacy with male gender may also reflect the biases and perception of clinicians in expecting male inpatients to present with a greater severity of illness, agitation, aggression, or that they are physically better able to tolerate combination antipsychotic therapy despite the lack of evidence to support such assumptions [23–25]. The association of polypharmacy with increased age of the patients on univariate analysis, in tandem with a greater length of illness, indicated a longer period of exposure to antipsychotics which could elevate the risk towards the development of adverse effects, especially extrapyramidal side-effects. The increased use of anticholinergic drugs in association with polypharmacy in this study could be for the management and prophylactic treatment of these extrapyramidal effects, although not without its own distressing adverse effects such as urinary retention, constipation and dry mouth. Moreover, the possibility of drug–drug interactions increases with each added drug and can eventually have a negative impact on treatment adherence, potentially leading to more relapses and rehospitalizations [26].
The association of polypharmacy with less use of an atypical antipsychotic further increases and compounds the side-effect burden. To a certain extent, the prescription of these second-generation antipsychotics depends on their availability and affordability in a particular treatment setting which can be related to the nature of the different healthcare delivery systems. For example, at the time of the study, risperidone was a nonsubsidized drug in Singapore and clozapine was not available in Japan but frequently prescribed in China. Similarly, zotepine was only available in Japan, Taiwan and Korea, but not in the other centres. However, when using an atypical antipsychotic, clinicians must also take into account the likely onset of adverse effects such as dyslipidaemias, impaired glucose tolerance, diabetes mellitus and weight gain [27, 28].
Recently, some clinicians have proposed ‘rational’ antipsychotic polypharmacy [20, 29]. Theoretical rationales for the use of combination antipsychotic therapy include boosting the effectiveness of monotherapy [30], optimizing the dopamine-2 receptor occupancy in refractory patients, targeting a diverse range of receptors other than just the dopamine receptors [21] as well as in treatment of patients with partial, inadequate or no response based on pharmacokinetic and pharmacodynamic considerations [29]. Antipsychotic polypharmacy in such instances may lead to better symptom relief and functional outcomes with minimization of side-effects associated with higher doses of any single drug. However, further qualitative and quantitative studies are needed to elucidate the nature of the interactions between the antipsychotics prescribed in combinations.
There were several limitations to this study. First, the formal rating of clinical features such as psychopathology and adverse effects was not performed, as this was a clinical audit study. Second, the cross-sectional nature of the study did not allow drawing any definite conclusions regarding causality between antipsychotic polypharmacy and its correlates. Third, the findings may not be generalizable to patients seen in the community or outpatient treatment settings.
In conclusion, antipsychotic polypharmacy is a prevalent prescribing practice in the management of patients with schizophrenia in East Asia, showing wide variations across this region. There is probably a complex interplay of factors influencing this prescription trend which include clinical, social and cultural factors. This study will hopefully stimulate further research to examine factors and pathways influencing this prescribing practice with the potential to improve the management of patients.
Acknowledgments
The study was supported by research funds from the Institute of Mental Health, Department of Research, Singapore (Grant 013/2001), Japan Society for Promotion of Science, Japan, and Bureau of National Health Insurance, Taiwan and (D0H90-NH-010).
References
- 1.Ito C, Kubota Y, Sato M. A prospective survey on drug choice for prescriptions for admitted patients with schizophrenia. Psychiatry Clin Neurosci. 1999;53(Suppl 1):S35–40. [PubMed] [Google Scholar]
- 2.Keks NA, Altson K, Hope J, et al. Use of antipsychosis and adjunctive medications by an inner urban community psychiatric service. Aust N Z J Psychiatry. 1999;33:896–901. doi: 10.1046/j.1440-1614.1999.00639.x. [DOI] [PubMed] [Google Scholar]
- 3.Weissman EM. Antipsychotic prescribing practices in the Veterans Healthcare Administration—New York metropolitan region. Schizophr Bull. 2002;28:31–42. doi: 10.1093/oxfordjournals.schbul.a006924. [DOI] [PubMed] [Google Scholar]
- 4.Jaffe AB, Levine J. Antipsychotic medication coprescribing in a large state hospital system. Pharmacoepidemiol Drug Saf. 2003;12:41–8. doi: 10.1002/pds.783. [DOI] [PubMed] [Google Scholar]
- 5.Tapp A, Wood AE, Secrest L, Erdmann J, Cubberley L, Kilzieh N. Combination antipsychotic therapy in clinical practice. Psychiatr Serv. 2003;54:55–9. doi: 10.1176/appi.ps.54.1.55. [DOI] [PubMed] [Google Scholar]
- 6.McCombs JS, Nichol MB, Johnstone BM, Stimmel GL, Shi J, Smith R. Antipsychotic drug use patterns and the cost of treating schizophrenia. Psychiatr Serv. 2000;51:525–7. doi: 10.1176/appi.ps.51.4.525. [DOI] [PubMed] [Google Scholar]
- 7.Fleischhacker WW. New developments in the pharmacotherapy of schizophrenia. J Neural Transm Suppl. 2003;64:105–17. doi: 10.1007/978-3-7091-6020-6_7. [DOI] [PubMed] [Google Scholar]
- 8.Procyshyn RM, Kennedy NB, Tse G, et al. Antipsychotic polypharmacy: a survey of discharge prescriptions from a tertiary care psychiatric institution. Can J Psychiatry. 2001;46:334–9. doi: 10.1177/070674370104600404. [DOI] [PubMed] [Google Scholar]
- 9.Tibaldi G, Munizza C, Bollini P, Pirfo E, Punzo F, Gramaglia F. Utilization of neuroleptic drugs in Italian mental health services: a survey in Piedmont. Psychiatr Serv. 1997;48:213–7. doi: 10.1176/ps.48.2.213. [DOI] [PubMed] [Google Scholar]
- 10.Kiivet RA, Llerena A, Dahl M-L, et al. Patterns of drug treatment of schizophrenic patients in Estonia, Spain and Sweden. Br J Clin Pharmacol. 1995;40:467–76. doi: 10.1111/j.1365-2125.1995.tb05791.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark RE, Bartels SJ, Mellman TA, Peacock WJ. Recent trends in antipsychotic combination therapy of schizophrenia and schizoaffective disorder: implications for state mental health policy. Schizophr Bull. 2002;28:75–84. doi: 10.1093/oxfordjournals.schbul.a006928. [DOI] [PubMed] [Google Scholar]
- 12.Tognoni G. Pharmacoepidemiology of psychotropic drugs in patients with severe mental disorders in Italy. Italian Collaborative Study Group on the Outcome of Severe Mental Disorders. Eur J Clin Pharmacol. 1999;55:685–90. doi: 10.1007/s002280050694. [DOI] [PubMed] [Google Scholar]
- 13.Dollfus S, van Os J, Petit M. Do we need a European consensus on the use of antipsychotic medication. Eur Psychiatry. 1996;11:400–2. doi: 10.1016/S0924-9338(97)82577-1. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington DC: American Psychiatric Press; 1994. [Google Scholar]
- 15.World Health Organisation. International Statistical Classification of Diseases and Related Health Problems. Geneva: World Health Organisation; 1992. 10th revision. [Google Scholar]
- 16.American Psychiatric Association. Practice Guidelines for the Treatment of Patients with Schizophrenia. Washington DC: American Psychiatric Press; 1997. [Google Scholar]
- 17.Inagaki A, Inada T, Fujii Y, Yagi G. Equivalent Doses of Psychotropics. Tokyo: Seiwa Shoten; 1999. [Google Scholar]
- 18.Kane JM, Aguglia E, Altamura AC, et al. Guidelines for depot antipsychotic treatment in schizophrenia. European Neuropsychopharmacology Consensus Conference in Siena, Italy. Eur Neuropsychopharmacol. 1998;8:55–66. doi: 10.1016/s0924-977x(97)00045-x. [DOI] [PubMed] [Google Scholar]
- 19.Chong SA, Sachdev P, Mahendran R, et al. Neuroleptic and anticholinergic drug use in Chinese patients with schizophrenia resident in a state psychiatric hospital in Singapore. Aust NZ J Psychiatry. 2000;34:988–91. doi: 10.1080/000486700274. [DOI] [PubMed] [Google Scholar]
- 20.Freudenreich O, Goff DC. Antipsychotic combination therapy in schizophrenia. A review of efficacy and risks of current combinations. Acta Psychiatr Scand. 2002;106:323–30. doi: 10.1034/j.1600-0447.2002.01331.x. [DOI] [PubMed] [Google Scholar]
- 21.Stahl SM. Antipsychotic polypharmacy: squandering precious resources? J Clin Psychiatry. 2002;63:93–4. doi: 10.4088/jcp.v63n0201. [DOI] [PubMed] [Google Scholar]
- 22.Tempier RP, Pawliuk NH. Conventional, atypical, and combination antipsychotic prescriptions: a 2-year comparison. J Clin Psychiatry. 2003;64:673–9. doi: 10.4088/jcp.v64n0609. [DOI] [PubMed] [Google Scholar]
- 23.Andia AM, Zisook S, Heaton RK, et al. Gender differences in schizophrenia. J Nerv Ment Dis. 1995;183:522–8. doi: 10.1097/00005053-199508000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Pinals DA, Malhotra AK, Missar CD, Pickar D, Breier A. Lack of gender differences in neuroleptic response in patients with schizophrenia. Schizophr Res. 1996;22:215–22. doi: 10.1016/s0920-9964(96)00067-9. [DOI] [PubMed] [Google Scholar]
- 25.Cernovsky ZZ, Landmark JA, O'Reilly RL. Symptom patterns in schizophrenia for men and women. Psychol Rep. 1997;80:1267–71. doi: 10.2466/pr0.1997.80.3c.1267. [DOI] [PubMed] [Google Scholar]
- 26.Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull. 1997;23:637–51. doi: 10.1093/schbul/23.4.637. [DOI] [PubMed] [Google Scholar]
- 27.McIntyre RS, McCann SM, Kennedy SH. Antipsychotic metabolic effects: weight gain, diabetes mellitus, and lipid abnormalities. Can J Psychiatry. 2001;46:273–81. doi: 10.1177/070674370104600308. [DOI] [PubMed] [Google Scholar]
- 28.Wirshing DA, Boyd JA, Meng LR, Ballon JS, Marder SR, Wirshing WC. The effects of novel antipsychotics on glucose and lipid levels. J Clin Psychiatry. 2002;63:856–65. doi: 10.4088/jcp.v63n1002. [DOI] [PubMed] [Google Scholar]
- 29.Kennedy NB, Procyshyn RM. Rational antipsychotic polypharmacy. Can J Clin Pharmacol. 2000;7:155–9. [PubMed] [Google Scholar]
- 30.Stahl SM. Antipsychotic polypharmacy, Part 1: Therapeutic option or dirty little secret? J Clin Psychiatry. 1999;60:425–6. doi: 10.4088/jcp.v60n0701. [DOI] [PubMed] [Google Scholar]