Abstract
Aims
To examine the pattern of adherence to statin therapy and to determine the association of adherence to statin therapy and the control of serum low-density lipoprotein (LDL)-cholesterol in a cohort of Hong Kong Chinese patients at high risk of coronary heart disease (CHD).
Methods
This was a prospective observational cohort study conducted at the outpatient clinics of a public teaching hospital in Hong Kong. Patients at high risk of CHD who had been initiated on statin monotherapy for <12 months were recruited. The statin prescription was dispensed in a bottle with the Medication Event Monitoring System (MEMS). Adherence was assessed in two dimensions: dose-count was defined as the percentage of doses taken, and dose-time was defined as the percentage of doses taken within the suggested time interval. Lipid profiles were obtained at baseline and during two follow-up visits at month 3 and month 6.
Results
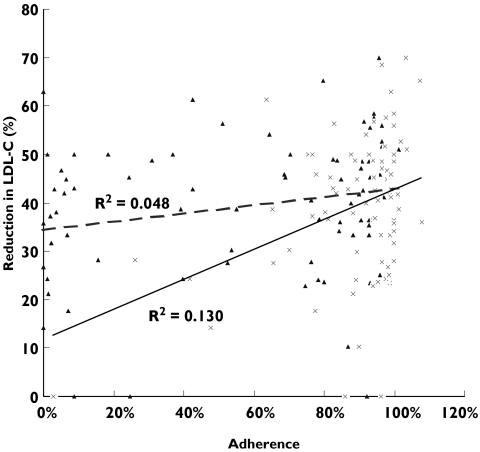
Eighty-three patients completed the study. The median adherence to dose-count and to dose-time were 95% (25-75th percentile = 87–99%) and 78% (25–75th percentile = 17–92%), respectively. Both dose-count and dose-time adherence declined slightly over the first 6 months of therapy. Living with family [relative risk (RR) = 0.79, 95% confidence interval (CI) 0.63, 0.91] and duration of therapy (RR = 0.99, 95% CI 0.98, 1.00) were negative predictors while number of family members (among those living with family) (RR = 1.05, 95% CI 1.00, 1.08) was a positive predictor for adherence to dose-count. Monthly household income (RR = 1.01, 95% CI 1.00, 1.02) and angina (RR = 1.29, 95% CI 1.05, 1.58) were positive predictors while living with family (RR = 0.74, 95% CI 0.55, 0.90) was a negative predictor for dose-time adherence. Percent reduction in serum LDL-cholesterol was correlated to dose-count (P < 0.001) and dose-time (P = 0.047) adherence. Statistically significant correlations were observed between adherence to dose-count and LDL reduction (R2 = 0.130; P = 0.001), and between dose-time adherence and LDL reduction (R2 = 0.048; P = 0.047).
Conclusion
High adherence to statin therapy was found in a cohort of Chinese patients at high risk of CHD and the adherence declined slightly over time. A weak association between adherence to statin dose-count and LDL reduction and a marginal association between dose-time adherence and LDL reduction were observed.
Keywords: Chinese patients, LDL reduction, patient adherence, statin
Background
Cardiovascular disease is the major cause of morbidity and mortality in industrialized countries and coronary heart disease (CHD) accounts for the majority of deaths from heart disease in Hong Kong [1–3]. The dose-related reductions in cholesterol levels paralleled the reductions in the risk of CHD, supporting the conclusion that ‘… a 1% reduction in cholesterol level produces a 2% reduction in the risk of CHD’[4]. Since 1994, the efficacy of HMG Co-A reductase inhibitors (statins) in significant reduction of CHD-related morbidity and mortality has been demonstrated in multiple large randomized clinical trials [5–10]. The Third Report of the National Cholesterol Education Program (NCEP) [Adult Treatment Panel (ATP) III] emphasized that patient adherence to low-density lipoprotein (LDL)-lowering therapy is one of the key elements approximating the magnitude of the benefits demonstrated in clinical trials of cholesterol-lowering [11].
Suboptimal lipid control is widely observed in clinical settings, suggesting discrepancy in patient adherence with statin therapy between controlled clinical trials and routine practice [12, 13]. Adherence declines over time especially for treatment of chronic diseases, and often drops to approximately 50%[14]. Persistence on statin therapy at 1 year after initiation varies from 33%[15] to 64.3%[16]. However, nearly 90% continuation of statin treatment was observed in some European countries [17, 18]. Several factors are shown to be predictive of poor patient adherence, such as age, race, education level, household income, family support, cigarette smoking, patients’ beliefs, comorbidities, number of concurrent medications and drug side-effects. Previous studies revealed that patients aged ≥60 years were better adherents, whereas those under 45 or over 75 years old showed significantly lower adherence rates [18–20]. The number of household members was found to modify the way Chinese elderly family member responded to their decline in health [21]. The number of close family members was also significantly associated with the amount of household care received by elderly family members [22]. Higher levels of adherence were reported among Caucasians compared with African-origin groups [19, 23], but few reported the drug-taking behaviour among Asians or Chinese [24–26]. Higher education and household income, cohesive family, positive attitude towards healthy living and patient–healthcare provider relationship may be correlated with increased adherence levels [16, 19, 23, 27–29]. Heavy smoking, complex regimens and the presence of intolerable side-effects may deter patients from adhering to the treatment [20, 27].
Designing adherence-enhancing interventions to achieve the maximum potential benefit requires knowledge of the minimum level of adherence to statin therapy associated with optimal control of serum lipid. The objectives of the present study were to examine the pattern of adherence to statin therapy and to determine the association of adherence to statin therapy and the control of serum LDL-cholesterol in a cohort of Chinese patients at high risk of CHD.
Methods
Setting
This was a prospective, observational cohort study conducted at three outpatient clinics (cardiology, diabetes and lipid) of a 1400-bed public teaching hospital in Hong Kong. The study protocol was approved by the Clinical Research Ethics Committee of The Chinese University of Hong Kong. Chinese patients aged ≥18 years with a history of CHD event or CHD-equivalent risk factors were identified by medical chart review. CHD risk equivalents included diabetes mellitus, a 10-year risk for CHD >20%, or other clinical forms of atherosclerotic disease (peripheral arterial disease, abdominal aortic aneurysm and symptomatic carotid artery disease) [11]. Patients identified with CHD or CHD-equivalent risk factors were recruited during clinic visits, from January to June 2003, to participate in a study to investigate their statin-taking habits and the control of cholesterol. Patients who were receiving statin therapy for less than 12 months, and those who had a baseline lipid profile obtained within 1 month prior to initiation of statin therapy, were included. Atorvastatin (once daily dosing) and simvastatin (once every evening dosing) were the two statin regimens being used interchangeably at the public hospital, and patients were therefore advised to take the drug every evening in order to avoid confusion. Choice of statin and dosage of drug were at the discretion of the primary care physicians. Patients who were receiving nonstatin lipid-lowering drugs, enrolled in other clinical studies, living in a nursing home, or those with psychiatric or neurological disorders were excluded.
Patients’ demographic information and clinical characteristics were collected at entry into the study. Two follow-up visits were scheduled in 3 and 6 months to monitor adherence to statin therapy. Fasting lipid profiles were obtained at study entry and during the follow-up visits.
Adherence assessment
A 3-month supply of the statin prescription was dispensed to the study patients in a bottle with the Medication Event Monitoring System (MEMS 6 Trackcap; AARDEX Ltd, Zug, Switzerland) at study entry and at the first follow-up visit. The lid of the bottle contained a microelectronic circuit that recorded the time when the lid was opened and closed. The patients were instructed to keep the statin prescription in the bottle and open the bottle only for taking the required quantity. They were reminded to bring the bottle back at the next follow-up visit. The mechanism of the electronic monitor device was not disclosed unless the patient asked about the purpose of it.
At the follow-up visit, data recorded by the MEMS were downloaded to a computer, showing the number of times the bottle was opened, and the number of times it was opened within the suggested time interval (18.00 h to 00.00 h). Assuming a dose of statin was administrated for each bottle opening, adherence was assessed in two dimensions: dose-count was defined as the percentage of doses taken, and dose-time was defined as the percentage of doses taken within the suggested time interval. Adherence levels of dose-count and dose-time were categorized into three levels [19, 29, 30]: (i) adherent patients are those with adherence of ≥80%; (ii) partially adherent patients are those with adherence of 20–79%; (iii) non-adherent patients are those with adherence <20%.
Independent predictors of adherence
Potential predictors of adherence assessed in the present study were demographic factors and clinical factors. Demographic factors included age, gender, cigarette smoking and socioeconomic status. Clinical factors were the baseline (within 1 year prior to initiation of statin therapy) comorbidity including CHD events, hypertension, congestive heart failure, stroke, diabetes mellitus, obesity, serum LDL-cholesterol levels prior to statin therapy, the type and tablet size of statin and number of other prescriptions at study entry.
Lipid profile assessment
Serum lipid profile was obtained at entry of study and at each follow-up visit. Percent reduction in serum LDL-cholesterol was calculated from patients’ baseline LDL-cholesterol prior to statin initiation. The NCEP ATP III guideline was adopted to determine the target level of LDL-cholesterol for each patient [11].
Statistical analysis
Descriptive statistics of patient demographics, dose-count and dose-time adherence and changes in serum LDL-cholesterol were reported. Data are presented as mean ± SD or median with the 25–75th percentile, where appropriate. Adherence was used as a continuous variable in the regression analysis. Backward multiple regression analysis was performed using probability of F statistics <0.05 for entry and >0.10 for removal to identify predictors of adherence. Crude relative risks were calculated from the parameter estimates, using RR = eβ. The differences in dosage of statin, baseline LDL-cholesterol, dose-count adherence, and reduction in LDL-cholesterol between simvastatin users and atrovastatin users were tested by Student's t-test or Mann–Whitney test, where appropriate. Linear regression analysis was performed to determine the relationship between statin adherence and serum LDL-cholesterol reduction. A P-value <0.05 was considered to be statistically significant.
Results
One hundred and nineteen patients were invited to participate in the study. Eleven patients refused to participate, five were referred to clinics other than the study clinics, and one insisted on using a pill-box. A total of 102 patients provided written consent and were included in the present study. Of the 102 study patients, one patient lost the bottle 1 month after recruitment, 15 transferred drugs to their pill-boxes and three did not close the bottle cap properly (lids were not completely closed when bottles were returned with dose count of <5% recorded by MEMS). None of the study patients asked about the purpose of using MEMS and no adverse reaction was reported throughout the study.
Eighty-three patients completed the study and their characteristics were listed in Table 1. The mean age of the patients was 60 ± 13 years and 51 (61%) of the patients were male. The average number of concurrent medications was 5 ± 1.6 items. Forty-six (55%) patients received simvastatin and 37 (45%) of them received atorvastatin. The mean simvastatin-equivalent daily dosage (5 mg atorvastatin =10 mg simvastatin) [31] of the 83 patients was 16.5 ± 6.4 mg. Patients on atrovastatin received a significantly (P < 0.001) higher mean simvastatin-equivalent daily dose (19.2 ± 4.9 mg) than those patients on simvastatin (14.3 ± 6.7 mg). The average duration of statin therapy prior to the study was 6.9 ± 3.2 months. The baseline serum LDL-cholesterol before initiation of statin therapy was 3.9 ± 0.7 mmol l−1 (simvastatin users = 3.9 ± 0.8 mmol l−1, atorvastatin users = 3.8 ± 0.7 mmol l−1; P = 0.909). Forty-nine patients (59%) had a diagnosis of diabetes mellitus and it was the most common CHD risk factor in this cohort. Among the patients with diabetes, 34 (70%) did not have other CHD risk factors.
Table 1.
Demographic data of study patients
| Characteristics | Number (%)a |
|---|---|
| Number of patients | 83 |
| Age in years (mean ± SD) | 60 ± 13 |
| Male | 51 (61) |
| Statin | |
| Simvastatin | 46 (55) |
| Atorvastatin | 37 (45) |
| Baseline LDL-C in mmol/l (mean ± SD)b | 3.9 ± 0.73 |
| Duration of statin therapy in months (mean ± SD) | 6.9 ± 3.2 |
| Number of concurrent medications (mean ± SD) | 5 ± 1.6 |
| Co-morbidity | |
| Diabetes mellitus | 49 (59) |
| Acute myocardial infarction | 19 (23) |
| Hypertension | 17 (20) |
| Angina | 15 (18) |
| Congestive heart failure | 3 (4) |
| Stroke | 1 (1.2) |
| Education | |
| ≤6 years | 42 (51) |
| 6–12 years | 34 (41) |
| >12 years | 7 (8) |
| Monthly household income (HK$)c | |
| <8000 | 35 (42) |
| 8000 to <15 000 | 16 (19) |
| 15 000 to <20 000 | 9 (11) |
| 20 000 to <25 000 | 10 (12) |
| >25 000 | 13 (16) |
Sum of percentage for underlying risk factors exceeded 100 because some patients had multiple risk factors.
LDL-C, Low-density lipoprotein cholesterol.
1 USD = 7.8 HKD.
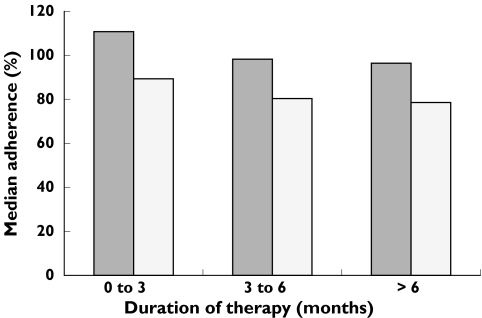
The levels of adherence to dose-count and to dose-time recorded by the electronic device were significantly skewed (P < 0.001); these two variables were therefore presented using median with 25–75th percentile. Table 2 shows the distribution of patients among adherent, partially adherent and non-adherent. The median adherence to dose-count and to dose-time were 95% (25–75th percentile =87–99%) and 78% (25–75th percentile =17–92%), respectively. There was no significant difference in dose-count adherence between simvastatin users (95.3%) and atorvastatin users (96.2%). The pattern of adherence to statin therapy over time is plotted in Figure 1. Both dose-count and dose-time adherence declined slightly over the first 6 months of therapy. The adherence to dose-count normalized from 110% during the first 3 months to 98% during the next 3 months and became stable at 96% after 6 months. Dose-time adherence also showed a similar trend of decline of 89%, 80%, 79% at 3, 6 and >6 months, respectively.
Table 2.
Patient distribution in three levels of adherence
| Number of patients (%) | ||
|---|---|---|
| Adherence level | Dose-count | Dose-time |
| Adherent (≥80%) | 70 (84.3) | 39 (47.0) |
| Partial adherent (20–79%) | 12 (14.5) | 22 (26.5) |
| Non-adherent (<20%) | 1 (1.2) | 22 (26.5) |
Figure 1.
Dose count ( ), dose time (□)
), dose time (□)
Predictors of adherence identified by backward multiple regression analysis are shown in Table 3. Only two patients received regimens with the largest tablet size (atorvastatin 20 mg and simvastatin 40 mg) and their adherence was above the 75th percentile and below the 25th percentile, respectively. The effect of tablet size on adherence therefore cannot be concluded. Twelve factors were associated with dose-count adherence and three of them achieved statistical significance. Living with family and duration of therapy in months were negative predictors, while number of family members among those living with family was a positive predictor of adherence to dose-count. Among the five factors associated with dose-time adherence, monthly household income and angina were positive predictors, while living with family was a negative predictor for dose-time adherence.
Table 3.
Association between potential predictors and percent change of adherence to statin therapy
| Predictorsa | Relative riskb (95% confidence interval) | P-value | |
|---|---|---|---|
| Dose-count | Living with family | 0.79 (0.63, 0.91) | 0.006 |
| Number of family members | 1.05 (1.00, 1.08) | 0.013 | |
| Duration of therapy (months) | 0.99 (0.98, 1.00) | 0.048 | |
| Congestive heart failure | 0.83 (0.67, 1.03) | 0.088 | |
| Retired | 1.05 (0.97, 1.14) | 0.213 | |
| Baseline LDL-C prior to therapyc (mmol/l) | 0.98 (0.93, 1.03) | 0.353 | |
| Number of current medications | 0.99 (0.96, 1.01) | 0.358 | |
| Stroke | 1.16 (0.83, 1.63) | 0.366 | |
| Male | 0.97 (0.95, 1.12) | 0.476 | |
| Smoker | 0.96 (0.85, 1.08) | 0.491 | |
| Hypertension | 0.97 (0.88, 1.07) | 0.535 | |
| Diabetes | 0.98 (0.90, 1.06) | 0.547 | |
| Dose-time | Monthly household income (thousand HKD) | 1.01 (1.00, 1.02) | 0.015 |
| Angina | 1.29 (1.05, 1.58) | 0.016 | |
| Living with family | 0.74 (0.55, 0.90) | 0.043 | |
| Stroke | 1.71 (0.84, 3.48) | 0.137 | |
| PTCAd | 0.89 (0.74, 1.08) | 0.232 |
Number of family members, duration of therapy, baseline LDL-C prior to therapy, number of current medications and monthly household incomes were continuous variables.
Crude relative risk.
LDL-C, Low-density lipoprotein cholesterol.
PTCA, Percutaneous transluminal coronary angioplasty.
The mean level of serum LDL-cholesterol was 2.3 ± 0.6 mmol l−1 and 63 (76%) patients achieved the target LDL-cholesterol of 2.6 mmol l−1 (NCEP ATP III guideline) by the end of the study. The average reduction in serum LDL-cholesterol was 39 ± 14.4%. There were no significant differences between atrovastatin users and simvastatin users in LDL reduction (40.4 ± 16.3% and 38.5 ± 13.1%, respectively). Linear regression analysis showed a more significant correlation of percent reduction in serum LDL-cholesterol to dose-count adherence (P < 0.001) than to dose-time adherence (P = 0.047) (Table 4). About 13% variability in the reduction of serum LDL-cholesterol was attributed to patient dose-count adherence, while dose-time adherence only contributed to 4.8% of the variation (R2 = 0.13 and 0.048, respectively). The changes of percent reduction in serum LDL-cholesterol against adherence of dose-count and dose-time are plotted in Figure 2. It shows a weak correlation of 60% adherence to dose-count to 30% reduction in LDL-cholesterol.
Table 4.
Association between adherence to statin therapy and reduction in LDL-cholesterol
| Y | X | β0 | β1 | R | R2 | P-valueb |
|---|---|---|---|---|---|---|
| % Reduction in LDL-Ca | Dose-count | 0.118 | 0.308 | 0.361 | 0.130 | 0.001 |
| Dose-time | 0.344 | 0.083 | 0.261 | 0.048 | 0.047 |
LDL-C, Low-density lipoprotein cholesterol.
P-value related to β0 and β1 and it indicates whether the regression model achieved statistical significance.
Figure 2.
Dose-time (--×--), dose-count (–▴–)
Discussion
In the present study, high statin adherence was observed in a cohort of Chinese patients at high risk for CHD who were initiated on statin therapy for less than 1 year. Eighty-four percent of patients adhered to taking the amount of prescribed doses (as measured by proportion of pill bottle openings) while 47% of patients took the prescribed dose at the suggested time interval (as recorded by the proportion of pill bottle openings that occurred within the time interval). The median adherence to dose-count (95%) and dose-time (78%) differed by 17%.
Since the observed dose-count in the present cohort was over 100% during the first few months of treatment, adherence tended to normalize from the third month onwards. From the first 3 months of therapy to the next quarter, the adherence to both dose-count and dose-time decreased by 10%, and by 2% from the second quarter to 6 months after. The rate of decline of adherence to statin therapy reported in a Danish study was similar to that of the present study [18]. Larsen et al. reviewed the statin prescription filling records of 3623 patients in Denmark from 1993 to 1998. The proportion of statin users remaining in treatment declined from 100% to 75% after 10 months of treatment. In a US study, however, Benner et al. reported that adherence to statin prescription filling, in a cohort of 34 501 patients who were ≥65 years of age, declined substantially over time, especially in the first 6 months. The proportion of patients who were adherent to statin therapy was 79%, 56%, and 50% after 3, 6, and 12 months, respectively [19]. The persistently high adherence rate observed in the present study could be explained by the fact that the study cohort who provided written consent might be more adherent than those who refused to participate in the study. Also, all the study patients had CHD-equivalent risk or a history of CHD events, and, CHD and diabetes were identified as negative predictors of suboptimal persistence [19]. In the present study, no patient asked about the purpose of using the bottle with the MEMS lid and the measurement of adherence was therefore unlikely to be affected by the electronic monitoring device.
Opposite effects of living with family and number of family members on adherence to dose-count were observed in the present cohort. Living with family was found as a negative predictor for dose-count adherence. Adherence among patients living with their families was around 0.8 times that of those who were living alone. Apparently, study patients who were not living in nursing home, old age home or with their families showed better adherence to statin therapy than those who were living with their families. It was suggested that patients living alone are more adherent to treatment because they may realize that their health is their own responsibility [32]. Nevertheless, adherence to dose-count increased with the number of family members among those patients who were living with family (RR = 1.05 for each additional family member). This is consistent with previous reports that the number of close family members was significantly associated with the amount of household care elderly patients received, and elderly patients responded positively to their own decline in health in a family with more adult members [21, 22]. Monthly household income was a statistically significant positive predictor of statin adherence. However, its effect was negligible. An increase in HKD 1000 corresponded to approximately 1% increase in adherence (RR = 1.01). Angina was the only CHD risk factor found to be significantly associated with high adherence in the present cohort. Patients with a history of angina were 1.29 times more adherent to the prescription than those without angina. Since only one patient had a history of stroke, no conclusions regarding association between stroke and adherence can be drawn.
In the present study, more patients (76%) achieved the target LDL-cholesterol and a lower level of adherence (≥60%) was weakly correlated to target LDL-cholesterol reduction compared with the findings of overseas clinical trials. An analysis of the effect of pravastatin reported that high level of adherence (≥75%) was required to demonstrate substantial CHD risk reductions in comparison with that achieved in the intention-to-treat analysis in the West of Scotland Coronary Prevention Study (WOSCOPS) [33]. Despite the level of adherence to pravastatin observed in Sweden being well above 90%, less than 20% of patients achieved the target total cholesterol of 5.2 mmol l−1[17]. Compared with Western populations, the lower level of adherence correlated to target cholesterol reduction may be explained by the lower baseline LDL-cholesterol level in the Chinese population [34]. The baseline LDL-cholesterol (3.9 mmol l−1) prior to statin therapy in the present Chinese cohort was significantly lower than the baseline LDL-cholesterol (4.9 mmol l−1) in 4S (P < 0.001) [9]. Although Asians share similar CHD risk factors with Caucasians, lower doses of lipid-lowering drugs were reported to achieve the same target lipid level [35]. Our study also found a lower mean statin dosage (equivalent to simvastatin 16.5 mg) being used in the present Chinese cohort compared with the usual starting dose of simvastatin (20–40 mg) as used in 4S [9, 36], yet a comparable LDL-cholesterol reduction was achieved (39% in the present study and 35% in 4S). Our findings suggested that the Chinese elderly patients may be more sensitive to statin therapy, and this hypothesis needs to be confirmed prospectively. The Chinese diet is lower in total fat, saturated and trans fatty acid than the Western diet, and such diversity in dietary habits may also contribute to the better clinical response to statin therapy among Chinese [37, 38].
The present study was limited by a small sample size of 102 patients and only 83 of them (81%) completed the study. The high adherence rate observed might be biased by the fact that patients who gave consent to participate in the study might be more motivated to adhere to statin therapy than those patients who refused to participate, resulting in a skewed distribution. A larger study is required to confirm these findings and whether they also apply to populations with low adherence and those patients at lower CHD risk.
In conclusion, a cohort of Chinese patients at high risk of CHD showed high adherence to statin therapy and the adherence normalized over time. A weak association between adherence to statin dose-count and LDL reduction and a marginal association between adherence to dose-time and LDL reduction were observed.
Acknowledgments
This study was supported by the School of Pharmacy, The Chinese University of Hong Kong.
References
- 1.Chan WK, Chui A, Ko GTC, et al. Ten-year cardiovascular risk in a Hong Kong population. J Cardiovasc Risk. 1999;6:163–9. doi: 10.1177/204748739900600307. [DOI] [PubMed] [Google Scholar]
- 2. [3 November 2003]; Website: Government of Hong Kong, SAR, China. http://www.info.gov.hk/dh/diseases/index.htm.
- 3.Fu FH. The prevalence of cardiovascular disease risk factors of Hong Kong Chinese. J Sports Med Phys Fitness. 2001;41:491–9. [PubMed] [Google Scholar]
- 4.Lipid Research Clinic Program. The Lipid Research Clinics Coronary Primary Prevention Trial Results. (I) Reduction in Incidence of Coronary Heart Disease; (II) the relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984;251:351–74. [Google Scholar]
- 5.Downs JR, Clearfield M, Weis S, et al. for the AFCAPS/TexCAPS Research Group. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. JAMA. 1998;279:1615–22. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 6.The Long-term intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–57. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 7.Sacks FM, Pfeffer MA, Moye LA for the Cholesterol and Recurrent Events Trial Investigators. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–9. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 8.Shepherd J, Cobbe SM, Ford I for the West of Scotland Coronary Prevention Study Group. Prevention of coronary heart disease in men with hypercholesterolemia. N Engl J Med. 1995;333:1301–7. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 9.Scandinavian Simvastatin Survival Study Group. Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–9. [PubMed] [Google Scholar]
- 10.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 11.Anonymous. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 12.Majumdar SR, Gurwitz JH, Soumerai SB. Undertreatment of hyperlipidemia in the secondary prevention of coronary artery disease. J General Intern Med. 1999;14:711–7. doi: 10.1046/j.1525-1497.1999.02229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LaRose JH, LaRose JC. Enhancing drug compliance in lipid-lowering treatment. Arch Fam Med. 2000;9:1169–75. doi: 10.1001/archfami.9.10.1169. [DOI] [PubMed] [Google Scholar]
- 14.Cramer JA, Mattson RH, Prevey ML, et al. How often is medication taken as prescribed% A novel assessment technique. JAMA. 1989;261:3273–7. [PubMed] [Google Scholar]
- 15.Catalan VS, LeLorier J. Predictors of long-term persistence on statins in a subsidized clinical population. Value Health. 2000;3:417–26. doi: 10.1046/j.1524-4733.2000.36006.x. [DOI] [PubMed] [Google Scholar]
- 16.Avorn J, Monette J, Lacour A, et al. Persistence of use of lipid-lowering medications. JAMA. 1998;279:1458–62. doi: 10.1001/jama.279.18.1458. [DOI] [PubMed] [Google Scholar]
- 17.Eriksson MHA, Dell K, Holme I, et al. Compliance with and efficacy of treatment with pravastatin and cholestyramine: a randomized study on lipid-lowering in primary care. J Intern Med. 1998;243:373–80. doi: 10.1046/j.1365-2796.1998.00294.x. [DOI] [PubMed] [Google Scholar]
- 18.Larsen J, Andersen M, Kragstrup J, Lars F. High persistence of statin use in a Danish population: compliance study 1993–1998. Br J Clin Pharm. 2002;53:375–8. doi: 10.1046/j.1365-2125.2002.01563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benner JS, Glynn RJ, Mogun H, et al. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288:455–61. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- 20.Kiortsis DN, Giral P, Bruckert E, Turpin G. Factors associated with low compliance with lipid-lowering drugs in hyperlipidemic patients. J Clin Pharm Ther. 2000;25:445–51. doi: 10.1046/j.1365-2710.2000.00315.x. [DOI] [PubMed] [Google Scholar]
- 21.Kaneda T. Health, work, and family support in China. Dissertations Abstracts Int, A Humanities Social Sci. 2003;63:4107–A. [Google Scholar]
- 22.Chou KL, Chi I. Social support exchange among elderly Chinese people and their family members in Hong Kong: a longitudinal study. Int J Aging Hum Dev. 2001;53:329–46. doi: 10.2190/QPUD-4FVJ-8KB2-CU4D. [DOI] [PubMed] [Google Scholar]
- 23.Golin CE, Liu HH, Hays RD, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J General Intern Med. 2002;17:756–65. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leung TN, Haines CJ, Chung TKH. Five-year compliance with hormone replacement therapy in postmenopausal Chinese women in Hong Kong. Maturitas. 2001;39:195–201. doi: 10.1016/s0378-5122(01)00210-9. [DOI] [PubMed] [Google Scholar]
- 25.Molassiotis A, Nahas-Lopez V, Chung WYR, Lam SWC, Li CKP, Lau TFJ. Factors associated with adherence to antiretroviral medication in HIV infected patients. Int J STD AIDS. 2002;13:301–10. doi: 10.1258/0956462021925117. [DOI] [PubMed] [Google Scholar]
- 26.Fong OW, Ho CF, Fung LY, et al. Determinants of adherence to highly active antiretroviral therapy (HAART) in Chinese HIV/AIDS patients. HIV Med. 2003;4:133–8. doi: 10.1046/j.1468-1293.2003.00147.x. [DOI] [PubMed] [Google Scholar]
- 27.Ammassari A, Trotta MP, Murri R, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J Acquir Immune Defic Syndr. 2002;31(Suppl. 3):123–7. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- 28.Brown J, Fitzpatrick R. Factors influencing compliance with dietary restrictions in dialysis patients. J Psychosom Res. 1998;32:191–6. doi: 10.1016/0022-3999(88)90054-2. [DOI] [PubMed] [Google Scholar]
- 29.Insull W. The problem of compliance to cholesterol altering therapy. J Intern Med. 1997;24:317–35. doi: 10.1046/j.1365-2796.1997.112133000.x. [DOI] [PubMed] [Google Scholar]
- 30.Rudd P. Compliance with antihypertensive therapy: a shifting paradigm. Cardiol Rev. 1994;2:230–40. [Google Scholar]
- 31.Jones P, Kafonek S, Laurora I, Hunninghake D. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study) Am J Cardiol. 1998;81:582–7. doi: 10.1016/s0002-9149(97)00965-x. [DOI] [PubMed] [Google Scholar]
- 32.McLane CG, Zyzanski SJ, Flocke SA. Factors associated with medication noncompliance in rural elderly hypertensive patients. Am J Hypertens. 1995;8:206–9. doi: 10.1016/0895-7061(94)00194-G. [DOI] [PubMed] [Google Scholar]
- 33.Anonymous. Compliance and adverse event withdrawal. Their impact on the West of Scotland Coronary Prevention Study. Eur Heart J. 1997;18:1718–24. doi: 10.1093/oxfordjournals.eurheartj.a015165. [DOI] [PubMed] [Google Scholar]
- 34.Tomlinson B, Lan W. Hypothyroidism and simvastatin. HKMJ. 2001;7:219–20. [PubMed] [Google Scholar]
- 35.Itoh T, Matsumoto M, Hougaku H, et al. Effects of low-dose simvastatin therapy on serum lipid levels in patients with moderate hypercholesterolemia: a 12-month study. Clin Ther. 1997;19:487–97. doi: 10.1016/s0149-2918(97)80133-6. [DOI] [PubMed] [Google Scholar]
- 36.Merck & Co., Inc. Zocor (Simvastatin) Prescribing Information. Whitehouse Station, NJ: Merck, Inc; 2004. [Google Scholar]
- 37.Zhou BF, Stamler J, Dennis B, et al. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003;17:623–30. doi: 10.1038/sj.jhh.1001605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Woo J, Leung SS, Ho SC, et al. Dietary intake and practice in the Hong Kong Chinese population. J Epidemiol Community Health. 1998;52:631–7. doi: 10.1136/jech.52.10.631. [DOI] [PMC free article] [PubMed] [Google Scholar]