Abstract
Gastrointestinal (GI) toxicity associated with nonsteroidal anti-inflammatory drugs (NSAIDs) is still an important medical and socio-economic problem – despite recent pharmaceutical advances. To prevent NSAID-induced gastropathy, three strategies are followed in clinical routine: (i) coprescription of a gastroprotective drug, (ii) use of selective COX-2 inhibitors, and (iii) eradication of Helicobacter pylori. Proton pump inhibitors are the comedication of choice as they effectively reduce gastrointestinal adverse events of NSAIDs and are safe even in long-term use. Co-medication with vitamin C has only been little studied in the prevention of NSAID-induced gastropathy. Apart from scavenging free radicals it is able to induce haeme-oxgenase 1 in gastric cells, a protective enzyme with antioxidant and vasodilative properties. Final results of the celecoxib outcome study (CLASS study) attenuated the initial enthusiasm about the GI safety of selective COX-2 inhibitors, especially in patients concomitantly taking aspirin for cardiovascular prophylaxis. Helicobacter pylori increases the risk for ulcers particularly in NSAID-naive patients and therefore eradication is recommended prior to long-term NSAID therapy at least in patients at high risk. New classes of COX-inhibitors are currently evaluated in clinical studies with very promising results: NSAIDs combined with a nitric oxide releasing moiety (NO-NSAID) and dual inhibitors of COX and 5-LOX. These drugs offer extended anti-inflammatory potency while sparing gastric mucosa.
Keywords: aspirin, COX/5-LOX, H. pylori, haeme-oxygenase, NO-NSAID, PPI
Introduction
Nonsteroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed drugs worldwide. It is a well-known phenomenon that NSAIDs cause gastric mucosal damage resulting in outcomes ranging from nonspecific dyspepsia to ulceration, upper gastrointestinal (GI) bleeding and death – summarized by the term ‘NSAID gastropathy’. The mechanisms of NSAID-induced GI injury are not fully understood. Topical damage occurs in acidic NSAIDs such as acetylic-salicylic acid (ASA) and includes the accumulation of ionized NSAID in the gastric epithelial cell called ‘ion trapping’ effect [1], the reduction of the hydrophobicity of the gastric mucosal surface [2] and uncoupling of oxidative phosphorylation [3]. Disruption of the epithelial barrier allows back-diffusion of acid into the mucosa.
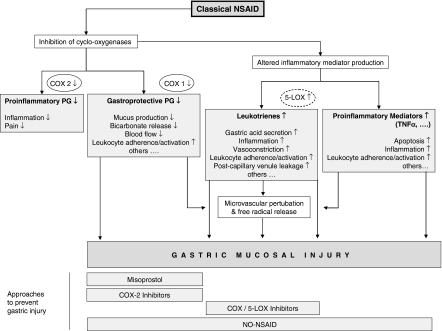
By inhibiting cyclo-oxygenases (COX) NSAIDs block the formation not only of proinflammatory but also of gastroprotective prostaglandins [4]. This is a key element in NSAID gastropathy as prostaglandins maintain gastric mucosal blood flow and increase protective mucus as well as bicarbonate production. The discovery of two different cyclo-oxygenases led to the development of drugs preferentially inhibiting the COX-2 isoform, on the proposition that prostaglandins produced by the constitutively expressed COX-1 protect gastric mucosa, whereas the inducible isoform COX-2 is responsible for inflammation and pain. Inhibition of cyclo-oxygenases by NSAIDs is furthermore associated with an altered inflammatory mediator production. As a consequence of COX-inhibition enhanced synthesis of leukotrienes may occur by shunting the arachidonic acid metabolism towards the 5-lipoxygenase pathway [5–7]. Leukotrienes are supposed to contribute to gastric mucosal injury by promoting tissue ischaemia and inflammation [7, 8]. Increased expression of adhesion molecules such as intercellular adhesion molecule-1 [9, 10] by proinflammatory mediators such as tumour necrosis factor-α[11] leads to an increased neutrophil–endothelial adherence and activation [9]. Wallace [12] postulated that NSAID-induced neutrophil adherence might contribute to the pathogenesis of gastric mucosal damage by two principal mechanisms: (i) occlusion of gastric microvessels by microthrombi leading to reduced gastric blood flow and ischaemic cell damage; (ii) increased liberation of oxygen-derived free radicals (Figure 1). Free oxygen radicals react with poly unsaturated fatty acids of the mucosa leading to lipid peroxidation and tissue damage. NSAIDs not only damage the stomach, but may affect the entire GI tract [13] and may cause a variety of severe extraintestinal complications like renal impairment [14, 15] up to acute renal failure in predisposed patients, sodium and fluid retention [14] and arterial hypertension [16] and, subsequently, heart failure.
Figure 1.
Illustration of NSAID-induced gastric damage: NSAID use alters the production of deleterious as well as gastroprotective prostaglandins, whereas other proinflammatory mediators such as tumour necrosis factor-α and leukotrienes – by a shift towards the 5-LOX pathway – are increased. Damage of gastric mucosa occurs by multiple mechanisms such as microvascular perturbations and neutrophil-mediated free radical release. The lower part of the illustration shows pharmaceutical approaches to prevent gastropathy with specific targets. For mechanisms of action, see Table 3 (modified according to [12])
Clinically and socio-economically, upper GI NSAID-induced injury is predominant: a recent meta-analysis showed that approximately one-third of patients taking NSAIDs long-term had gastric or duodenal ulcers detected by endoscopy [17]. However, the probability of clinically important serious GI complications is much lower (odds ratio between 5.36 in randomized controlled trials and 2.7 in cohort studies according to a meta-analysis by Ofman et al.[18]). Based upon an analysis of patients in the Arthritis, Rheumatism, and Aging Medical Information System (ARAMIS), it is estimated that approximately 107 000 patients are hospitalized per year for NSAID-related GI complications and at least 16 500 NSAID-related deaths occur annually among arthritis patients alone in the USA [19]. The estimated annual costs of direct and indirect NSAID-related adverse effects exceed 7 billion dollars in the USA, which corresponds to $272 per NSAID user [20].
These data emphasize the need to develop strategies to improve gastric tolerability of NSAIDs – especially for patients at high risk for severe GI complications. Principle risk factors for these complications are listed in Table 1 (for review see [21]). In a clinical setting either comedication such as a proton pump inhibitor (PPI) will be prescribed or medication will be switched to a COX-2 preferential drug. This regimen will solve the issue for most patients, but results in higher costs for medication. In this review, currently applied pharmacological strategies to prevent NSAID gastropathy as well as experimental/preclinical approaches will be discussed.
Table 1.
Risk factors for the development of NSAID gastropathy – modified according to [21]
| Older age (over 60–65 years) |
| History of peptic ulcer disease |
| Helicobacter pylori infection prior to NSAID therapy |
| First few months of NSAID use |
| High doses of NSAID |
| Other debilitating disease (especially cardiovascular) |
| Concomitant use of anticoagulants and corticosteroids |
Clinical routine
Three strategies are currently followed in clinical routine to prevent NSAID-induced gastric damage: (i) coprescription of gastroprotective agents, (ii) use of selective COX-2 inhibitors, and (iii) eradication of H. pylori.
Gastroprotective drugs
Misoprostol
Misoprostol is a prostaglandin analogue used to locally replace prostaglandins the formation of which is inhibited by NSAIDs. According to a meta-analysis performed by Koch [22], misoprostol prevents NSAID-induced GI damage: gastric ulceration was found to be significantly reduced in both acute and chronic NSAID treatment, whereas duodenal ulceration was significantly reduced only in chronic treatment. In the MUCOSA study co-application of 200 µg misoprostol four times a day was shown to reduce the overall rate of NSAID-induced complications by about 40%[23]. Unfortunately, its use is limited by a high rate of GI adverse events [23, 24]. Furthermore, misoprostol use was not associated with a reduction of dyspeptic symptoms [25].
Sucralfate/antacids
Apart from diminishing acid exposure to the damaged epithelium by forming a protective gel (sucralfate) or by neutralization of gastric acid (antacids), both regimens have been shown to induce various gastroprotective mechanisms [26–29].
There are only limited data on the use of the aluminium salt of sucrose octasulphate (sucralfate) in the long-term prevention of NSAID-induced gastric damage. Despite promising results with sucralfate in smaller studies [30] or for short-term prophylaxis [26, 31], a randomized, controlled trial conduced by Agrawal and coworkers failed to show a significant benefit of sucralfate in the prevention of gastric ulcers in contrast to misoprostol [32].
Data concerning antacids in the prevention of NSAID-related gastric mucosal injury are scarce, and also disappointing. Especially for long-term prophylaxis no clinical effect was observed with low-dose antacids [26]. In one endoscopic study subjects that were treated with an antacid to prevent naproxen-induced gastric injury developed even greater numbers of gastric erosions compared with placebo [33].
Inhibitors of acid secretion
Acid enhances NSAID-induced mucosal damage, and might activate proteolytic pepsin and increase gastric absorption of acidic NSAID [34]. Interestingly, H2-receptor antagonists and PPIs seem to protect gastric mucosa not only by inhibiting acid secretion and thus elevating gastric pH but also by scavenging free radicals [35, 36]. Biswas et al.[36] recently demonstrated that omeprazole plays an important role in gastroprotection by acting as a potent antioxidant and antiapoptotic molecule – independent of its role in acid secretion.
H2-receptor antagonists
H2-receptor antagonists presented the standard of ulcer treatment up to the development of PPIs. They were the first drugs effectively to heal reflux oesophagitis as well as peptic ulcers. However, in the prevention of NSAID-induced gastric ulceration [37, 38], H2-receptor antagonists at standard doses are not only ineffective but might also increase the risk of ulcer bleeding [39], perhaps because of masking warning symptoms [39, 40]. Doubling the standard dose (famotidine 40 mg twice daily) significantly decreased the 6-month incidence of gastric ulcers [41]. Formation of duodenal ulcers on the other hand can be prevented [37, 38] and upper GI symptoms improved by H2-receptor antagonists [41–43]. Taken together, nowadays H2-receptor antagonists can no longer be recommended to prevent NSAID gastropathy.
Proton-pump inhibitors
Acid suppression by PPI is more effective compared with H2-receptor antagonists and is now standard therapy for the treatment of both peptic ulcers and gastro-oesophageal reflux-disease (GERD). Omeprazole (20 mg once a day) has been demonstrated to be significantly more effective in the prevention of gastroduodenal ulcers than ranitidine (150 mg twice daily) [44] or misoprostol (200 µg bid) [45]. In both studies the PPI provided greater symptomatic relief of dyspepsia associated with NSAID; omeprazole was tolerated better than misoprostol [45]. Graham and coworkers [24] showed in a double-blind, randomized, multicentre study that lansoprazole is superior to placebo in the prevention of NSAID-induced gastric ulcers in H. pylori-negative subjects but not superior to full-dose misoprostol (200 µg four times daily). By week 12 of the study, percentages of ulcer-free patients were: 51% for placebo, 93% for misoprostol and 82% for lansoprazole. Taking into account the poor compliance associated with misoprostol (due to adverse effects and the requirement of four doses), lansoprazole and full-dose misoprostol are clinically equivalent [24]. Esomeprazole, the S-isomer of omeprazole, possesses a higher systemic bioavailability and provides significantly more effective and more sustained gastric acid control compared with other PPIs [46]. Most recently, 20 and 40 mg of esomeprazole have been shown to relieve upper GI symptoms significantly in patients continuing to take NSAID or selective COX-2 inhibitors [47, 48]. Due to the selectivity of their target enzyme the rate of adverse events associated with PPIs is low. Long-term use of PPIs is safe [49, 50]. However, in H. pylori-positive subjects accelerated progression of corpus gastritis may occur [50–52]. Prior to long-term use of PPIs, H. pylori should be eradicated [52]. A disadvantage of PPIs may be that they are unlikely to protect against mucosal injury in more distal parts of the intestine (e.g. in NSAID colonopathy). However, in summary, PPIs present the comedication of choice to prevent NSAID-induced gastropathy.
Selective COX-2 inhibitors/Coxibs
The benefit of selective COX-2 inhibitors for the protection of the GI tract is generally accepted. Overall incidences of GI symptoms are lower in patients on rofecoxib [53] or celecoxib [54] compared with unselective COX-inhibitors. Rates of developing GI ulceration were not significantly different from those of placebo [55, 56] in endoscopic studies. In contrast, large prospective outcome studies were less impressive: the VIGOR study [53] comparing rofecoxib 50 mg with naproxen 1 g daily demonstrated a reduction of all upper GI events in 54%– with similar efficacy against rheumatoid arthritis. Six months’ data of the CLASS study [54] even failed to show significant differences in rates of serious upper GI complications between celecoxib compared with ibuprofen and diclofenac. An important difference between the VIGOR and CLASS studies was that low-dose aspirin was permitted for cardiovascular prophylaxis in the latter. Subgroup analysis showed that GI complications were only reduced in patients not taking aspirin, but the benefit was abolished in this subgroup (21% of the patients) taking aspirin [54]. Much less attention has been paid to the data of the entire CLASS study (12 and 15 months), which questions the benefit of celecoxib: according to a prespecified protocol analysis the rates of serious upper GI complications were similar in the celecoxib group compared with diclofenac or ibuprofen [57–60]; most of the ulcer complications that occurred after 6 months were in users of celecoxib [57–60]. However, bias by confounding factors in the NSAID group can not be completely ruled out [57, 61].
We now know that the differentiation between ‘protective COX-1’ and ‘evil COX-2’ was simplistic and had to be abandoned in favour of a more detailed evaluation of both isoforms [62]: although entitled an inducible isoform, COX-2 is constitutively expressed in several organs maintaining tissue homeostasis [7, 63, 64], e.g. in kidney [65], brain, and reproductive system [7, 64]. COX-2 plays an important role in gastric mucosal defence and ulcer healing [63]. On the other hand, it has been shown that prostaglandins derived from COX-1 significantly contribute to inflammation [66]. The main functions of both isoforms are summarized in Table 2. However, the ‘COX-story’ turns out to be even more complex: in 2002 Chandrasekharan and colleagues [67] identified another cyclo-oxygenase isoform with highest expression in the brain: COX-3. Inhibition of this enzyme by analgesic/antipyretic drugs including acetaminophen and some NSAIDs might be a primary central mechanism by which these drugs decrease pain and possibly fever [68]. As this isoform is a spliced COX-1 variant it is possible that some effects originally attributed to COX 1 were indeed mediated by COX-3 [68]. The discovery that multiple COX isoenzymes can derive from just one gene will provide new insights into the mode of action of the different COX-inhibitors.
Table 2.
Physiological and pathophysiological functions of COX isoforms 1 and 2 – modified according to [7]
| COX-1 | COX-2 | |
|---|---|---|
| Physiological functions | ||
| GI mucosal protection | X | |
| Kidney function | X | X |
| Kidney development | X | |
| Reproduction | X | |
| Regulation of blood flow | X | X |
| CNS function | X | X |
| Bone metabolism | X | X |
| Lung function | X | ? |
| Platelet aggregation | X | |
| Pathophysiological functions | ||
| Inflammatory signs | X | X |
| Inflammation resolution | X | |
| GI mucosal protection under inflammatory conditions | X | X |
| Gastric ulceration | X* | X* |
| Tissue repair/ulcer healing | X | |
| (gastrointestinal) Cancer | X | X |
Inhibition of both isoforms necessary.
Because of the notion that COX-2 is essentially involved in several physiological processes, attention must be drawn to side-effects of coxibs. Ulcer healing has been shown to be impaired by selective COX-2 inhibitors [69, 70], and with regard to renal adverse events, they do not offer an advantage [15] compared with conventional NSAIDs. Results of the VIGOR study made cardiovascular safety a further critical issue: the rate of myocardial infarction was four-fold, the rate of cardiovascular thrombotic events two-fold higher in the rofecoxib group compared with naproxen [53]. On the other hand, the lack of antiplatelet effects might be advantageous in patients with coagulation disorders or patients on anticoagulants. Coxibs of the second generation such as valdecoxib, etoricoxib, lumaricoxib, and the water-soluble parecoxib (given i.v.), possess a several-fold higher selectivity for COX-2. According to the present data these drugs have proven efficacy in the treatment of inflammation and pain, but a further reduction of NSAID-related adverse events is doubtful [71].
Taken together, compared with classical NSAIDs the use of selective COX-2 inhibitors seems to be associated with reduced GI toxicity in patients not taking aspirin concomitantly even in supratherapeutic doses, but further studies have to clarify the risk–benefit profile of these drugs definitively.
Eradication of H. pylori
The interaction between NSAIDs and H. pylori has been a matter of debate, but a recently published meta-analysis showed that both H. pylori and NSAIDs independently increase the risk for – and have synergistic effects in – the development of peptic ulcers as well as ulcer bleeding [17]. Uncomplicated peptic ulcer disease in H. pylori-positive NSAID takers occurred significantly more frequently (41.7%) than in patients not infected with H. pylori (25.9%) [17].
Chan and coworkers [72] studied the effect of H. pylori eradication prior to therapy with diclofenac in infected, NSAID-naive patients with dyspepsia or history of peptic ulcer. Eradication of H. pylori significantly reduced the incidence of ulcers (12.1%vs. 34.4%) and ulcer complications (4.3%vs. 27.1%). Konturek et al. were able to show that H. pylori interferes with the gastric adaptation to ASA [73]. On the other hand, H. pylori eradication alone did not affect the risk for ulcers or dyspepsia in patients on long-term NSAID therapy [74]. Eradication therapy alone has been shown to be less effective in the prevention of recurrent upper GI bleeding (18.8%) in H. pylori-positive patients taking naproxen compared with omeprazole comedication (4%) [75]. Obviously, there seems to be a difference in the role of H. pylori in NSAID-naive patients and long-term NSAID takers [72]. According to the Maastricht 2–2000 consensus report [52], it is advisable to test for and eradicate H. pylori in patients in whom NSAID therapy is planned and who are at increased risk of peptic ulcers [72, 76]. There are no general recommendations if these patients require additional long-term prophylaxis by, for example, PPI. The high incidence of peptic ulcers even after H. pylori eradication (12.1%) in the study performed by Chan [72] pleads for a prophylactic therapy in patients at high risk [76]. According to Hawkey and Langman [77], eradication is also required in appropriate patients using selective COX-2 inhibitors, as H. pylori doubles the risk of ulcers in patients taking rofecoxib. For long-term NSAID takers H. pylori eradication alone is not sufficient to prevent recurrent ulceration/bleeding; in these patients secondary prophylaxis with PPI or switch to selective COX-2 inhibitors is necessary. Which of the two strategies is superior can not be decided from the present data [76]. In a recently published study, celecoxib and diclofenac plus omeprazole were equivalent with regard to the incidence of recurrent ulcer bleeding (4.9%vs. 6.4%), but neither regimen offered complete protection [78].
Recommendations differ in H. pylori-positive patients on low-dose aspirin. Screening for H. pylori infection prior to treatment with low-dose aspirin is not generally recommended and would enormously increase costs due to the high number of patients treated with low-dose aspirin for cardiovascular prophylaxis [76], but it is advisable in those patients with a history of peptic ulcer disease [52]. After successful H. pylori eradication, patients on low-dose aspirin do not necessarily need further prophylactic comedication [76].
Agents/regimens commercially available, but not in general use
Besides the above generally accepted approaches to reduce the GI adverse effects of NSAIDs, gastroprotective formulations, especially for aspirin, have been developed: enteric coated/sustained release aspirin and aspirin combined with vitamin C. Although used in clinical routine for decades, the effects of a fixed combination of aspirin and vitamin C have rarely been investigated with regard to its GI side-effects.
Enteric coating
Enteric coating is especially used as a formulation of aspirin. The removal of topically damaging effects associated with NSAIDs due to intestinal release of the drug is the basis of the protection. Because of its use for cardiovascular prophylaxis, a large patient population is exposed to aspirin in daily dosages ranging between 75 and 300 mg. Even low-dose aspirin can be associated with severe GI complications [79–82], although the risk is relatively low. It has recently been demonstrated that the enteric coated formulation does not adversely affect the antithrombotic properties of aspirin [83]. The results of endoscopic studies showed a trend towards a reduction of gastroduodenal lesions of enteric coated compared with plain aspirin both in low and higher dosages [84–87]. Therefore, coating seems to be a promising approach to reduce gastric injury of low-dose aspirin. However, there are conflicting data about the benefit of the enteric coated formulation to prevent ulcer bleeding, in that two studies failed to show a difference compared with plain aspirin [80–82]. Furthermore, care has to be taken concerning mucosal injury in more distal parts of the intestine: sustained release and enteric coating formulations of NSAIDs can be associated with small and large intestinal injury and severe complications [88]. Additionally, when taken together with a PPI, early disruption of enteric coating and intragastric release of the drug might occur due to an increased gastric pH [89]– thus abolishing the desired effect of coating.
Addition of antioxidants/vitamin C
The role of antioxidants, especially vitamins C and E, in the prevention of NSAID-induced gastric injury is relatively little studied, and large outcome studies are missing. We [90] and others [36, 91] demonstrated that ASA generates reactive oxygen metabolites which significantly contribute to gastric mucosal damage in humans – probably by initiating lipid peroxidation. On the other hand, mRNA expression and activity of protective antioxidizing enzymes like superoxide dismutase and glutathione peroxidase in the stomach as well as intragastric vitamin C levels were impaired by ASA. Comedication with vitamin C abolished these effects, was able to scavenge free radicals, and significantly attenuated gastric damage [90]. In animal studies vitamin E protected against ASA-induced gastric injury by inhibition of lipid peroxidation and accumulation of activated neutrophils [92, 93]. Both vitamins C and E seem to play a role in the preservation of gastric mucosal integrity; vitamin C is actively secreted into the gastric lumen of healthy subjects, and its concentrations are decreased in patients with gastroduodenal diseases such as peptic ulcer disease, gastric malignancy [94, 95], or H. pylori-associated gastritis [96]. The underlying molecular mechanisms, however, are not fully understood.
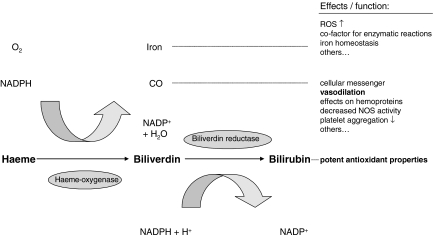
We were recently able to show that the gastroprotective effects of vitamin C as observed in humans might – at least in part – be mediated by haeme-oxygenase-1 (HO-1) [97]. HO-1 is a ubiquitous and crucial tissue-protective enzyme with vasodilative, anti-inflammatory and antioxidant properties. Its pathway and functions are illustrated in Figure 2. In the stomach HO-1 might counteract the two major mechanisms of NSAID-induced gastric injury: disturbance of gastric microcirculation and free radical release (Figure 1). The mechanisms of HO-1 induction seem to be cell-type specific; a nonstressful induction was recently postulated as a therapeutic target [98]. We identified vitamin C as a potential nonstressful inducer of HO-1 in the stomach. However, to date there are only very limited data about this enzyme in the stomach. Guo et al.[99] showed that healing of gastric ulcers in rats is paralleled by an upregulation of HO-1. Further studies are needed to examine the role of HO-1 in the stomach in vivo. Our recent findings, however, are in favour of the supplementation of vitamin C in order to prevent NSAID gastropathy – showing an impact beyond its sole antioxidant properties.
Figure 2.
Pathway of haeme-oxygenase-1 (HO-1) – modified according to [98]. Various stressful and nonstressful stimuli induce HO-1; it catalyses the degradation of haeme into equimolar amounts of carbon monoxide (CO), iron and biliverdin, which is subsequently reduced to bilirubin. These products exert vasodilative, anti-inflammatory and antioxidant effects
Experimental/preclinical approaches
Two very promising alternatives to clinically applied comedication are currently studied in clinical trials: NO-NSAID and dual inhibitors of COX and 5-LOX. Both seem to have extended anti-inflammatory activity while sparing gastric mucosa.
NO-NSAIDs
Under physiological conditions, small amounts of nitric oxide (NO) synthesized by the constitutive isoform enzymes [endothelial (eNOS) and neuronal (bNOS) nitric oxide synthase] contribute to gastric mucosal defence by influencing key elements of gastroprotection. Like prostaglandins, NO increases mucus and bicarbonate secretion as well as microcirculation and decreases neutrophil–endothelial adherence [100]– a key pathogenic element in NSAID gastropathy. We were able to show that in humans the adaptation to chronic aspirin intake is accompanied by an increased expression of mucosal eNOS, which may be responsible for the observed enhancement of mucosal blood flow despite reduced prostaglandin synthesis [101]. The underlying mechanisms involved in the gastroprotection by NO are complex. As the pathways of NO and HO are closely related to each other [102] it seems possible that some of the gastroprotective effects of NO – like those of vitamin C – might be mediated by HO.
The recognition of NO as an important mediator of gastric mucosal defence led to the development of a new class of drugs: nitric oxide releasing NSAIDs (NO-NSAIDs). These drugs consist of a conventional NSAID esterified to a NO-releasing moiety. Multiple studies in animals impressively demonstrated the ability of NO-NSAID to spare GI mucosa in acute [103–105] and chronic administration [106] (for review see [107]). For example, NO-aspirin did not produce detectable mucosal injury, in contrast to aspirin administration, in rats when given in equimolar dosages [103]. Similar results have been obtained with other parent NSAIDs such as NO-naproxen [104] and NO-indomethacin [105]. In experimental models, NO-NSAIDs even protected gastric mucosa against damage induced by other deleterious stimuli and maintained gastric mucosal blood flow [107–109]. Ukawa et al.[110] showed that healing of gastric ulcers was not impaired by NO-aspirin whereas the parent substance as well as a selective COX-2 inhibitor in equimolar dosages delayed the healing process. Apart from diminishing GI toxicity, NO-NSAIDs improve anti-inflammatory and antinociceptive efficacy [111]. Additionally, NO-aspirin has an increased antithrombotic potency compared with conventional aspirin [107, 112]. The broad biological effects of slowly released NO combined with COX inhibition are likely to extend the indication of NO-NSAIDs from the therapy of inflammation and pain to the treatment/prevention of various other diseases such as cancer or cardiovascular disorders as discussed by Keeble and Moore [107]. A recently published study involving a total of 31 volunteers supported the data obtained in animal studies showing significantly reduced but not completely abolished GI toxicity associated with NO-naproxen compared with conventional naproxen in humans [113].
In summary, NO-NSAIDs represent a promising therapeutic alternative to conventional and COX-2 selective NSAIDs with not only reduced profile of GI side-effects but also ameliorated power of desired effects. Large, randomized studies are needed to evaluate definitively the clinical benefit of NO-NSAIDs in humans.
Dual inhibitors of COX and 5-LOX
Beside prostaglandins, leukotrienes are metabolized in the arachidonic acid pathway by the lipoxygenase (5-LOX) enzyme. Leukotrienes are important mediators of inflammation complementary to prostaglandins [7]. Experimental studies demonstrated that particularly cysteinyl leukotrienes contribute to gastric mucosal damage by inducing microvascular injury and promoting a breakdown of the mucosal barrier [7, 8]. Inhibition of COX is often associated with an enhanced synthesis of leukotrienes due to shunting the arachidonic acid metabolism towards the leukotriene pathway [5–7]. Dual inhibitors of COX/5-LOX have been developed in order to achieve enhanced anti-inflammatory activity while sparing gastric mucosa. Licofelone (or ML3000) was demonstrated to exhibit these properties in animal trials [7, 114, 115]. Phase II trials have indicated that this COX/5-LOX inhibitor spares human gastric mucosa. Endoscopically normal findings were reported after 4 weeks of treatment with 200 mg licofelone bid in 93%, with 400 mg licofelone in 89% compared with only 37% in individuals treated with naproxen 500 mg bid [116, 117]. Similar results were obtained in a 12-week, Phase III, randomized, double-blind trial in 148 patients with osteoarthritis. The incidence of gastroduodenal ulcers turned out to be 1.5% with licofelone 200 mg bid compared with 15.3% with naproxen 500 mg bid while analgesic activity was equivalent [118]. In the control of pain licofelone 200 mg bid was as effective as celecoxib 200 mg once daily with identical GI safety in a 12-week randomized trial [119]. In contrast to selective COX-2 inhibitors [54], licofelone has been shown to retain its GI safety profile when taken together with low-dose aspirin in a study involving 75 patients [120]. Fiorucci et al.[121] recently described an underlying mechanism for this difference between selective/nonselective COX inhibitors and licofelone: the balance in the production of the deleterious leukotriene LTB4vs. the protective lipoxin ATL (aspirin triggered lipoxin, generated by acetylated COX-2) is involved in controlling acute and chronic responses to aspirin. While administration of either selective or nonselective COX inhibitors to aspirin-pretreated rats exacerbated gastric injury due to inhibition of ATL and increase in LTB4 formation, licofelone did not – because it additionally inhibited LTB4 generation. Another advantage of licofelone compared with selective COX-2 inhibitors might be its antithrombotic and platelet aggregation inhibiting function [122]. Most data regarding COX/5-LOX inhibitors have been published as an abstract only, and therefore represent only preliminary findings. Previous dual COX/5-LOX inhibitors such as benoxaprofen were withdrawn because of hepatic and other toxicity [123]. This problem may be molecule-specific. Although licofelone has so far not been associated with hepatotoxicity [7], careful monitoring of liver function is advisable during treatment. Again, large outcome studies have to show if these promising findings can be translated into clinical benefit and if the long-term use of this drug is safe.
Conclusions
The best way to prevent NSAID gastropathy is to avoid these drugs. This is, of course, not possible in most cases. When using nonselective NSAIDs, it is important to reduce the doses to a minimum, as most of the adverse events occur dose-dependently. Drugs with a low GI toxicity profile such as ibuprofen [124] should be preferred. It is crucial to identify patients at high risk for NSAID-induced GI complications (Table 1). At least these patients require a gastroprotective comedication or should be switched to a selective COX-2 inhibitor. The different approaches to reduce NSAID gastropathy are listed in Table 3. Comedication with vitamin C in the prevention of NSAID gastropathy has been only little studied, but apart from scavenging free radicals it is able to induce haeme-oxygenase-1 in gastric cells, a protective enzyme with antioxidant and vasodilative properties. PPIs are the comedication of choice, especially because adverse events even in long-term use are minimal. COX-2 inhibitors have been aggressively marketed; although overall GI toxicity seems to be reduced with these coxibs, final data of the CLASS study failed to show an advantage in the reduction of serious upper GI complications compared with unselective NSAIDs.
Table 3.
Advantages and disadvantages of different pharmacological approaches to reduce gastrointestinal toxicity of NSAIDs as well as principal mechanisms of action differentiated in (a) established regimens, (b) less investigated, but clinically used strategies, and (c) experimental/preclinical approaches
| Regimen | Principal mechanism of protective action | Advantages | Disadvantages |
|---|---|---|---|
| A) | |||
| Classical NSAID + misoprostol | Prostaglandin substitution | Effective in reducing occurrence of gastroduodenal ulceration and associated complications* | GI adverse events |
| Ineffective in preventing dyspepsia | |||
| Dosing at least three times daily | |||
| Classical NSAID + PPI | Elevation of intragastric pH (Antioxidant and antiapoptotic properties) | Effective in reducing dyspepsia and occurrence of gastroduodenal ulcers and associated complications* | Possibly acceleration of corpus gastritis in H. pylori-infected patients |
| Minimal adverse events attributable to PPI | |||
| Selective COX-2 inhibitors | Sparing gastroprotective prostaglandins generated by COX-1 isoform | Effective in reducing dyspepsia and occurrence of gastroduodenal ulcers and associated complications* | Lack of gastroprotection with concomitant use of aspirin |
| Lack of antiplatelet effect/possibly prothrombotic effects | |||
| B) | |||
| Enteric coating formulations | Abrogation of topical damaging effects | Cheap | Benefit not proven |
| Possibly shift of mucosal damage to more distal parts of the intestine | |||
| Classical NSAID + vitamin C | Antioxidant properties (Activation of gastric mucosal defence mechanisms Induction of HO-1) | Physiological concept | No data of large outcome studies available |
| No adverse effects attibutable to vitamin C | |||
| Cheap | |||
| C) | |||
| NO-NSAID | Slow release of gastroprotective NO, thereby maintenance of microvascular integrity (Antiapoptotic effects) | Reduction of gastrointestinal toxicity* | Lack of clinical data |
| Increased anti-inflammatory and anti-nociceptive efficacy | |||
| Antithrombotic effects | |||
| Physiological concept | |||
| COX/5-LOX inhibitors | Inhibition of deleterious leukotriene formation | Reduction of gastrointestinal toxicity* | Lack of clinical data |
| Maintenance of gastroprotection despite concomitant use of aspirin | |||
| Antithrombotic effects | |||
Compared with classical NSAID without comedication.
Large outcome studies comparing coxibs with PPI comedication in the prevention of NSAID gastropathy are lacking. According to the present data, in elderly patients without further risk factors both strategies seem to be appropriate. Comedication with PPIs should be preferentially used in patients with cardiovascular disease, patients concomitantly taking low-dose aspirin for cardiovascular prophylaxis and in patients with a history of peptic ulcer disease. Although both regimens have been shown to be equivalent in the prevention of recurrent ulcer bleeding [78], PPIs seems to be more appropriate as, in contrast to coxibs, these drugs promote ulcer healing. A switch to selective COX-2 inhibitors might be advantageous in patients on anticoagulants or with coagulation disorders as well as in patients requiring high doses of NSAIDs [77]. There is no evidence justifying a simultaneous prescription of coxibs together with PPIs in order to reduce GI adverse events further [125] according to National Institute for Clinical Excellence (NICE) guidance on the use of COX-2 selective inhibitors. However, this guidance will be reviewed soon. In case ulcers occur under therapy with coxibs and COX-2 inhibition is still required, the addition of a PPI seems reasonable.
New treatment modalities such as dual COX/5-LOX inhibitors and NO-NSAIDs may be superior to coxibs in many pathophysiological aspects. According to preclinical studies, indications for NO-NSAIDs might extend from simply reducing inflammation and pain to the therapy of various other diseases. However, large outcome studies of both NO-NSAIDs and COX/5-LOX inhibitors are still awaited.
References
- 1.Davenport HW. Salicylate damage to the gastric mucosal barrier. N Engl J Med. 1967;276:1307–12. doi: 10.1056/NEJM196706082762308. [DOI] [PubMed] [Google Scholar]
- 2.Lichtenberger LM. The hydrophobic barrier properties of gastrointestinal mucus. Annu Rev Physiol. 1995;57:565–83. doi: 10.1146/annurev.ph.57.030195.003025. [DOI] [PubMed] [Google Scholar]
- 3.Jorgensen TG, Weis-Fogh US, Nielsen HH, Olesen HP. Salicylate- and aspirin-induced uncoupling of oxidative phosphorylation in mitochondria isolated from the mucosal membrane of the stomach. Scand J Clin Lab Invest. 1976;36:649–54. doi: 10.1080/00365517609054490. [DOI] [PubMed] [Google Scholar]
- 4.Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol. 1971;231:232–5. doi: 10.1038/newbio231232a0. [DOI] [PubMed] [Google Scholar]
- 5.Hudson N, Balsitis M, Everitt S, Hawkey CJ. Enhanced gastric mucosal leukotriene B4 synthesis in patients taking non-steroidal anti-inflammatory drugs. Gut. 1993;34:742–7. doi: 10.1136/gut.34.6.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaananen PM, Keenan CM, Grisham MB, Wallace JL. Pharmacological investigation of the role of leukotrienes in the pathogenesis of experimental NSAID gastropathy. Inflammation. 1992;16:227–40. doi: 10.1007/BF00918812. [DOI] [PubMed] [Google Scholar]
- 7.Martel-Pelletier J, Lajeunesse D, Reboul P, Pelletier JP. Therapeutic role of dual inhibitors of 5-LOX and COX, selective and non-selective non-steroidal anti-inflammatory drugs. Ann Rheum Dis. 2003;62:501–9. doi: 10.1136/ard.62.6.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peskar BM. Role of leukotriene C4 in mucosal damage caused by necrotizing agents and indomethacin in the rat stomach. Gastroenterology. 1991;100:619–26. doi: 10.1016/0016-5085(91)80005-t. [DOI] [PubMed] [Google Scholar]
- 9.McCafferty DM, Granger DN, Wallace JL. Indomethacin-induced gastric injury and leukocyte adherence in arthritic versus healthy rats. Gastroenterology. 1995;109:1173–80. doi: 10.1016/0016-5085(95)90576-6. [DOI] [PubMed] [Google Scholar]
- 10.Andrews FJ, Malcontenti-Wilson C, O'Brien PE. Effect of nonsteroidal anti-inflammatory drugs on LFA-1 and ICAM-1 expression in gastric mucosa. Am J Physiol. 1994;266:G657–64. doi: 10.1152/ajpgi.1994.266.4.G657. [DOI] [PubMed] [Google Scholar]
- 11.Santucci L, Fiorucci S, Giansanti M, Brunori PM, Di Matteo FM, Morelli A. Penoxifylline prevents indomethacin induced acute gastric mucosal damage in rats: role of tumor necrosis factor alpha. Gut. 1994;35:909–15. doi: 10.1136/gut.35.7.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallace JL. Nonsteroidal anti-inflammatory drugs and gastroenteropathy: the second hundred years. Gastroenterology. 1997;112:1000–16. doi: 10.1053/gast.1997.v112.pm9041264. [DOI] [PubMed] [Google Scholar]
- 13.Bjorkman D. Nonsteroidal anti-inflammatory drug-associated toxicity of the liver, lower gastrointestinal tract, and esophagus. Am J Med. 1998;105:17S–21S. doi: 10.1016/s0002-9343(98)00276-9. [DOI] [PubMed] [Google Scholar]
- 14.Palmer BF. Renal complications associated with use of nonsteroidal anti-inflammatory agents. J Invest Med. 1995;43:516–33. [PubMed] [Google Scholar]
- 15.Brater DC, Harris C, Redfern JS, Gertz BJ. Renal effects of COX-2-selecitve inhibitors. Am J Nephrol. 2001;21:1–15. doi: 10.1159/000046212. [DOI] [PubMed] [Google Scholar]
- 16.Johnson AG, Nguyen TV, Day RO. Do nonsteroidal anti-inflammatory drugs affect blood pressure ? A meta-analysis. Ann Intern Med. 1994;121:289–300. doi: 10.7326/0003-4819-121-4-199408150-00011. [DOI] [PubMed] [Google Scholar]
- 17.Huang JQ, Sridhar S, Hunt RH. Role of Helicobacter pylori infection and non-steroidal anti-inflammatory drugs in peptic-ulcer disease: a meta-analysis. Lancet. 2002;359:14–22. doi: 10.1016/S0140-6736(02)07273-2. [DOI] [PubMed] [Google Scholar]
- 18.Ofman JJ, MacLean CH, Straus WL, et al. A metaanalysis of severe upper gastrointestinal complications of nonsteroidal antiinflammatory drugs. J Rheumatol. 2002;29:804–12. [PubMed] [Google Scholar]
- 19.Singh G. Recent considerations in nonsteroidal anti-inflammatory drug gastropathy. Am J Med. 1998;105:31S–38S. doi: 10.1016/s0002-9343(98)00072-2. [DOI] [PubMed] [Google Scholar]
- 20.Delco F, Michetti P, Beglinger C, Fried M, Szucs TD. Health care resource utilization and costs of NSAID-induced gastrointestinal toxicity. A population-based study in Switzerland. Digestion. 2004;69:10–19. doi: 10.1159/000076542. [DOI] [PubMed] [Google Scholar]
- 21.Russell RI. Defining patients at risk of non-steroidal anti-inflammatory drug gastropathy. Ital J Gastroenterol Hepatol. 1999;31(Suppl. 1):S14–18. [PubMed] [Google Scholar]
- 22.Koch M. Non-steroidal anti-inflammatory drug gastropathy: clinical results with misoprostol. Ital J Gastroenterol Hepatol. 1999;31(Suppl. 1):S54–62. [PubMed] [Google Scholar]
- 23.Silverstein FE, Graham DY, Senior JR, et al. Misoprostol reduces serious gastrointestinal complications in patients with rheumatoid arthritis receiving nonsteroidal anti-inflammatory drugs. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1995;123:241–9. doi: 10.7326/0003-4819-123-4-199508150-00001. [DOI] [PubMed] [Google Scholar]
- 24.Graham DY, Agrawal NM, Campbell DR, et al. Ulcer prevention in long-term users of nonsteroidal anti-inflammatory drugs: results of a double-blind, randomized, multicenter, active- and placebo-controlled study of misoprostol vs lansoprazole. Arch Intern Med. 2002;162:169–75. doi: 10.1001/archinte.162.2.169. [DOI] [PubMed] [Google Scholar]
- 25.Graham DY, White RH, Moreland LW, et al. Duodenal and gastric ulcer prevention with misoprostol in arthritis patients taking NSAIDs. Misoprostol Study Group. Ann Intern Med. 1993;119:257–62. doi: 10.7326/0003-4819-119-4-199308150-00001. [DOI] [PubMed] [Google Scholar]
- 26.Lazzaroni M, Sainaghi M, Bianchi Porro G. Non-steroidal anti-inflammatory drug gastropathy: clinical results with antacids and sucralfate. Ital J Gastroenterol Hepatol. 1999;31(Suppl. 1):S48–53. [PubMed] [Google Scholar]
- 27.Domschke W, Hagel J, Ruppin H, Kaduk B. Antacids and gastric mucosal protection. Scand J Gastroenterol. 1986;21(Suppl. 125):144–50. doi: 10.3109/00365528609093830. [DOI] [PubMed] [Google Scholar]
- 28.Preclik G, Stange EF, Gerber K, Fetzer G, Horn H, Ditschuneit H. Alimentary tract and pancreas. Stimulation of mucosal prostaglandin synthesis in human stomach and duodenum by antacid treatment. Gut. 1989;30:148–51. doi: 10.1136/gut.30.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Konturek SJ, Brzozowski T, Majka J, Czarnobilski K. Role of nitric oxide and prostaglandins in sucralfate-induced gastroprotection. Eur J Pharmacol. 1992;211:277–9. doi: 10.1016/0014-2999(92)90541-b. [DOI] [PubMed] [Google Scholar]
- 30.Caldwell JR, Roth SH, Wu WC, et al. Sucralfate treatment of nonsteroidal anti-inflammatory drug-induced gastrointestinal symptoms and mucosal damage. Am J Med. 1987;83:74–82. doi: 10.1016/0002-9343(87)90832-1. [DOI] [PubMed] [Google Scholar]
- 31.Lanza FL, Graham DY, Davis RE, Rack MF. Endoscopic comparison of cimetidine and sucralfate for prevention of naproxen-induced acute gastroduodenal injury. Effect of scoring method. Dig Dis Sci. 1990;35:1494–9. doi: 10.1007/BF01540567. [DOI] [PubMed] [Google Scholar]
- 32.Agrawal NM, Roth S, Graham DY, et al. Misoprostol compared with sucralfate in the prevention of nonsteroidal anti-inflammatory drug-induced gastric ulcer. A randomized, controlled trial. Ann Intern Med. 1991;115:195–200. doi: 10.7326/0003-4819-115-3-195. [DOI] [PubMed] [Google Scholar]
- 33.Sievert W, Stern AI, Lambert JR, Peacock T. Low-dose antacids and nonsteroidal anti-inflammatory drug-induced gastropathy in humans. J Clin Gastroenterol. 1991;13(Suppl. 1):S145–8. doi: 10.1097/00004836-199112001-00024. [DOI] [PubMed] [Google Scholar]
- 34.Scarpignato C, Pelosini I. Prevention and treatment of non-steroidal anti-inflammatory drug-induced gastro-duodenal damage: rationale for the use of antisecretory compounds. Ital J Gastroenterol Hepatol. 1999;31(Suppl. 1):S63–72. [PubMed] [Google Scholar]
- 35.Lapenna D, De Gioia S, Mezzetti A, et al. H2-receptor antagonists are scavengers of oxygen radicals. Eur J Clin Invest. 1994;24:476–81. doi: 10.1111/j.1365-2362.1994.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 36.Biswas K, Bandyopadhyay U, Chattopadhyay I, Varadaraj A, Ali E, Banerjee RK. A novel antioxidant and antiapoptotic role of omeprazole to block gastric ulcers through scavenging of hydroxyl radical. J Biol Chem. 2003;278:10993–1001. doi: 10.1074/jbc.M210328200. [DOI] [PubMed] [Google Scholar]
- 37.Robinson MG, Griffin JW, Bowers J, et al. Effect of ranitidine on gastroduodenal mucosal damage induced by nonsteroidal antiinflammatory drugs. Dig Dis Sci. 1989;34:424–8. doi: 10.1007/BF01536266. [DOI] [PubMed] [Google Scholar]
- 38.Ehsanullah RS, Page MC, Tildesley G, Wood JR. Prevention of gastroduodenal damage induced by non-steroidal anti-inflammatory drugs: controlled trial of ranitidine. Br Med J. 1988;297:1017–21. doi: 10.1136/bmj.297.6655.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singh G, Ramey DR, Morfeld D, Shi H, Hatoum HT, Fries JF. Gastrointestinal tract complications of nonsteroidal anti-inflammatory drug treatment in rheumatoid arthritis. A prospective observational cohort study. Arch Intern Med. 1996;156:1530–6. [PubMed] [Google Scholar]
- 40.Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med. 1999;340:1888–99. doi: 10.1056/NEJM199906173402407. [DOI] [PubMed] [Google Scholar]
- 41.Taha AS, Hudson N, Hawkey CJ, et al. Famotidine for the prevention of gastric and duodenal ulcers caused by nonsteroidal antiinflammatory drugs. N Engl J Med. 1996;334:1435–9. doi: 10.1056/NEJM199605303342204. [DOI] [PubMed] [Google Scholar]
- 42.Van Groenendael JH, Markusse HM, Dijkmans BA, Breedveld FC. The effect of ranitidine on NSAID related dyspeptic symptoms with and without peptic ulcer disease of patients with rheumatoid arthritis and osteoarthritis. Clin Rheumatol. 1996;15:450–6. doi: 10.1007/BF02229641. [DOI] [PubMed] [Google Scholar]
- 43.Lanza FL, Aspinall RL, Swabb EA, Davis RE, Rack MF, Rubin A. Double-blind, placebo-controlled endoscopic comparison of the mucosal protective effects of misoprostol versus cimetidine on tolmetin-induced mucosal injury to the stomach and duodenum. Gastroenterology. 1988;95:289–94. doi: 10.1016/0016-5085(88)90482-9. [DOI] [PubMed] [Google Scholar]
- 44.Yeomans ND, Tulassay Z, Juhasz L, et al. A comparison of omeprazole with ranitidine for ulcers associated with nonsteroidal antiinflammatory drugs. Acid Suppression Trial: Ranitidine versus Omeprazole for NSAID-associated Ulcer Treatment (ASTRONAUT) Study Group. N Engl J Med. 1998;338:719–26. doi: 10.1056/NEJM199803123381104. [DOI] [PubMed] [Google Scholar]
- 45.Hawkey CJ, Karrasch JA, Szczepanski L, et al. Omeprazole compared with misoprostol for ulcers associated with nonsteroidal antiinflammatory drugs. Omeprozole versus Misoprostol for NSAID-induced Ulcer Management (OMNIUM) Study Group. N Engl J Med. 1998;338:727–34. doi: 10.1056/NEJM199803123381105. [DOI] [PubMed] [Google Scholar]
- 46.Wilder-Smith CH, Rohss K, Nilsson-Pieschl C, Junghard O, Nyman L. Esomeprazole 40 mg provides improved intragastric acid control as compared with lansoparzole 30 mg and rabeprazole 20 mg in healthy volunteers. Digestion. 2003;68:184–8. doi: 10.1159/000075697. [DOI] [PubMed] [Google Scholar]
- 47.Laine L. The role of proton pump inhibitors in NSAID-associated gastropathy and upper gastrointestinal symptoms. Rev Gastroenterol Disord. 2003;3(Suppl. 4):S30–9. [PubMed] [Google Scholar]
- 48.Yeomans ND, Hawkey CJ, Jones R, et al. Esomeprazole provides effective control of NSAID-associated upper GI symptoms in patients continuing to take NSAIDs. Gastroenterology. 2003;124(Suppl. 1):A–107. [Google Scholar]
- 49.Rösch W. Moderne Protonenpumpenhemmer in der Gastroenterologie, 1 Auflage. Bremen: UNI-MED-Verlag; 2000. [German]. [Google Scholar]
- 50.Klinkenberg-Knol EC, Nelis F, Dent J, et al. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety, and influence on gastric mucosa. Gastroenterology. 2000;118:661–9. doi: 10.1016/s0016-5085(00)70135-1. [DOI] [PubMed] [Google Scholar]
- 51.Meining A, Kiel G, Stolte M. Changes in Helicobacter pylori-induced gastritis in the antrum and corpus during and after 12 month of treatment with ranitidine and lansoprazole in patients with duodenal ulcer disease. Aliment Pharmacol Ther. 1998;12:735–40. doi: 10.1046/j.1365-2036.1998.00370.x. [DOI] [PubMed] [Google Scholar]
- 52.Malfertheiner P, Mégraud F, O'Morain C, et al. Current concepts in the management of Helicobacter pylori infection – the Maastricht 2–2000 consensus report. Aliment Pharmacol Ther. 2002;16:167–80. doi: 10.1046/j.1365-2036.2002.01169.x. [DOI] [PubMed] [Google Scholar]
- 53.Bombardier C, Laine L, Reicin A, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med. 2000;343:1520–8. doi: 10.1056/NEJM200011233432103. [DOI] [PubMed] [Google Scholar]
- 54.Silverstein FE, Faich G, Goldstein JL, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long-Term Arthritis Safety Study. JAMA. 2000;284:1247–55. doi: 10.1001/jama.284.10.1247. [DOI] [PubMed] [Google Scholar]
- 55.Laine L, Harper S, Simon T, et al. A randomized trial comparing the effect of rofecoxib, a cyclooxygenase 2-specific inhibitor, with that of ibuprofen on the gastroduodenal mucosa of patients with osteoarthritis. Rofecoxib Osteoarthritis Endoscopy Study Group. Gastroenterolgy. 1999;117:776–83. doi: 10.1016/s0016-5085(99)70334-3. [DOI] [PubMed] [Google Scholar]
- 56.Simon LS, Weaver AL, Graham DY, et al. Anti-inflammatory and upper gastrointestinal effects of celecoxib in rheumatoid arthritis: a randomized controlled trial. JAMA. 1999;282:1921–8. doi: 10.1001/jama.282.20.1921. [DOI] [PubMed] [Google Scholar]
- 57.Micklewright R, Lane S, Linley W, McQuade C, Thomson F, Maskrey N. Review article: NSAIDs, gastroprotection and cyclo-oxygenase-II-selective inhibitors. Aliment Pharmacol Ther. 2003;17:321–32. doi: 10.1046/j.1365-2036.2003.01454.x. [DOI] [PubMed] [Google Scholar]
- 58.Juni P, Rutjes AS, Dieppe PA. Are selective COX 2 inhibitors superior to traditional non steroidal anti-inflammatory drugs? Adequate analysis of the CLASS trial indicates that this may not be the case. Br Med J. 2002;324:1287–8. doi: 10.1136/bmj.324.7349.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Witter J. Medical Officer Review. [Accessibility verified 18 October 2001]; Available at: http://www.fda.gov/ohrms/dockets/ac/01/briefing/3677b1-03_med.pdf.
- 60.Statistical reviewer briefing document for the advisory committee. Lu HL. [10 December 2001]; http://www.fda.gov/ohrms/dockets/ac/01/briefing/3677b1-04_stats.doc.
- 61.Silverstein FE, Simon L, Faich G. Reporting of 6-month vs 12-month data in a clinical trial of celecoxib. In reply. JAMA. 2001;286:2399–400. [PubMed] [Google Scholar]
- 62.Stichtenoth DO, Frölich JC. Therapie mit präferentiellen und spezifischen COX-2 Inhibitoren. Internist. 2001;42:421–6. doi: 10.1007/s001080050769. [German]. [DOI] [PubMed] [Google Scholar]
- 63.Peskar BM, Maricic N, Gretzera B, Schuligoi R, Schmassmann A. Role of cyclooxygenase-2 in gastric mucosal defense. Life Sci. 2001;69:2993–3003. doi: 10.1016/s0024-3205(01)01407-2. [DOI] [PubMed] [Google Scholar]
- 64.Katori M, Majima M. Cyclooxygenase-2: its rich diversity of roles and possible application of its selective inhibitors. Inflamm Res. 2000;49:367–92. doi: 10.1007/s000110050605. [DOI] [PubMed] [Google Scholar]
- 65.Harris RC. The macula densa: recent developments. J Hypertens. 1996;14:815–22. doi: 10.1097/00004872-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 66.Wallace JL, Bak A, McKnight W, Asfaha S, Sharkey KA, MacNaughton WK. Cyclooxygenase 1 contributes to inflammatory responses in rats and mice: implications for gastrointestinal toxicity. Gastroenterology. 1998;115:101–9. doi: 10.1016/s0016-5085(98)70370-1. [DOI] [PubMed] [Google Scholar]
- 67.Chandrasekharan NV, Dai H, Roos KL, et al. COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc Natl Acad Sci USA. 2002;99:13926–31. doi: 10.1073/pnas.162468699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schwab JM, Schluesener HJ, Laufer S. COX-3: just another COX or the solitary elusive target of paracetamol? Lancet. 2003;361:981–2. doi: 10.1016/S0140-6736(03)12841-3. [DOI] [PubMed] [Google Scholar]
- 69.Mizuno H, Sakamoto C, Matsuda K, et al. Induction of cyclooxygenase 2 in gastric mucosal lesions and its inhibiton by the specific antagonist delays healing in mice. Gastroenterology. 1997;112:387–97. doi: 10.1053/gast.1997.v112.pm9024292. [DOI] [PubMed] [Google Scholar]
- 70.Schmassmann A, Peskar BM, Stettler C, et al. Effects of inhibition of prostaglandin endoperoxide synthase-2 in chronic gastro-intestinal ulcer models in rats. Br J Pharmacol. 1998;123:795–804. doi: 10.1038/sj.bjp.0701672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stichtenoth DO, Frolich JC. The second generation of COX-2 inhibitors: what advantages do the newest offer? Drugs. 2003;63:33–45. doi: 10.2165/00003495-200363010-00003. [DOI] [PubMed] [Google Scholar]
- 72.Chan FK, To KF, Wu JC, et al. Eradication of Helicobacter pylori and risk of peptic ulcers in patients starting long-term treatment with non-steroidal anti-inflammatory drugs: a randomised trial. Lancet. 2002;359:9–13. doi: 10.1016/s0140-6736(02)07272-0. [DOI] [PubMed] [Google Scholar]
- 73.Konturek JW, Dembinski A, Konturek SJ, Stachura J, Domschke W. Infection of Helicobacter pylori in gastric adaptation to continued administration of aspirin in humans. Gastroenterology. 1998;114:245–55. doi: 10.1016/s0016-5085(98)70474-3. [DOI] [PubMed] [Google Scholar]
- 74.Hawkey CJ, Tulassay Z, Szczepanski L, et al. Randomised controlled trial of Helicobacter pylori eradication in patients on non-steroidal anti-inflammatory drugs: HELP NSAIDs study. Helicobacter Eradication for Lesion Prevention. Lancet. 1998;352:1016–21. doi: 10.1016/s0140-6736(98)04206-8. [DOI] [PubMed] [Google Scholar]
- 75.Chan FK, Chung SC, Suen BY, et al. Preventing recurrent upper gastrointestinal bleeding in patients with Helicobacter pylori infection who are taking low-dose aspirin or naproxen. N Engl J Med. 2001;344:967–73. doi: 10.1056/NEJM200103293441304. [DOI] [PubMed] [Google Scholar]
- 76.Limmer S, Ittel TH, Wietholtz H. [Secondary and primary prophylaxis of gastropathy associated with nonsteroidal antiinflammatory drugs or low-dose-aspirin: a review based on four clinical scenarios] Z Gasteroenterol. 2003;41:719–28. doi: 10.1055/s-2003-41208. [German]. [DOI] [PubMed] [Google Scholar]
- 77.Hawkey CJ, Langman MJ. Non-steroidal anti-inflammatory drugs: overall risks and management. Complementary roles for COX-2 inhibitors and proton pump inhibitors. Gut. 2003;52:600–8. doi: 10.1136/gut.52.4.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chan FK, Hung LC, Suen BY, et al. Celecoxib versus diclofenac and omeprazole in reducing the risk of recurrent ulcer bleeding in patients with arthritis. N Engl J Med. 2002;347:2104–10. doi: 10.1056/NEJMoa021907. [DOI] [PubMed] [Google Scholar]
- 79.Slattery J, Warlow CP, Shorrock CJ, Langman MJ. Risks of gastrointestinal bleeding during secondary prevention of vascular events with aspirin – analysis of gastrointestinal bleeding during the UK-TIA trial. Gut. 1995;37:509–11. doi: 10.1136/gut.37.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Weil J, Colin-Jones D, Langman M, et al. Prophylactic aspirin and risk of peptic ulcer bleeding. Br Med J. 1995;310:827–30. doi: 10.1136/bmj.310.6983.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kelly JP, Kaufman DW, Jurgelon JM, Sheehan J, Koff RS, Shapiro S. Risk of aspirin-associated major upper-gastrointestinal bleeding with enteric-coated or buffered product. Lancet. 1996;348:1413–6. doi: 10.1016/S0140-6736(96)01254-8. [DOI] [PubMed] [Google Scholar]
- 82.Sorensen HT, Mellemkjaer L, Blot WJ, et al. Risk of upper gastrointestinal bleeding associated with use of low-dose aspirin. Am J Gastroenterol. 2000;95:2218–24. doi: 10.1111/j.1572-0241.2000.02248.x. [DOI] [PubMed] [Google Scholar]
- 83.Van Hecken A, Juliano ML, Depre M, et al. Effects of enteric-coated, low-dose aspirin on parameters of platelet function. Aliment Pharmacol Ther. 2002;16:1683–8. doi: 10.1046/j.1365-2036.2002.01332.x. [DOI] [PubMed] [Google Scholar]
- 84.Hoftiezer JW, Silvoso GR, Burks M, Ivey KJ. Comparison of the effect of regular and enteric-coated aspirin on gastroduodenal mucosa of man. Lancet. 1980;2:609–12. doi: 10.1016/s0140-6736(80)90282-2. [DOI] [PubMed] [Google Scholar]
- 85.Jaszewski R. Frequency of gastroduodenal lesions in asymptomatic patients on chronic aspirin or nonsteroidal antiinflammatory drug therapy. J Clin Gastroenterol. 1990;12:10–13. doi: 10.1097/00004836-199002000-00004. [DOI] [PubMed] [Google Scholar]
- 86.Cole AT, Hudson N, Liew LC, Murray FE, Hawkey CJ, Heptinstall S. Protection of human gastric mucosa against aspirin – enteric coating or dose reduction ? Aliment Pharmacol Ther. 1999;13:187–93. doi: 10.1046/j.1365-2036.1999.00470.x. [DOI] [PubMed] [Google Scholar]
- 87.Dammann HG, Burkhardt F, Wolf N. Enteric coating of aspirin significantly decreases gastroduodenal mucosal lesions. Aliment Pharmacol Ther. 1999;13:1109–14. doi: 10.1046/j.1365-2036.1999.00588.x. [DOI] [PubMed] [Google Scholar]
- 88.Davies NM. Sustained release and enteric coated NSAIDs: are they really GI safe ? J Pharm Pharm Sci. 1999;2:5–14. [PubMed] [Google Scholar]
- 89.Nefesoglu FZ, Ayanoglu-Dulger G, Ulusoy NB, Imeryuz N. Interaction of omeprazole with enteric-coated salicylate tablets. Int J Clin Pharmacol Ther. 1998;36:549–53. [PubMed] [Google Scholar]
- 90.Pohle T, Brzozowski T, Becker JC, et al. Role of reactive oxygen metabolites in aspirin-induced gastric damage in humans: gastroprotection by vitamin C. Aliment Pharmacol Ther. 2001;15:677–87. doi: 10.1046/j.1365-2036.2001.00975.x. [DOI] [PubMed] [Google Scholar]
- 91.McAlindon ME, Muller AF, Filipowicz B, Hawkey CJ. Effect of allopurinol, sulphasalazine, and vitamin C on aspirin induced gastroduodenal injury in human volunteers. Gut. 1996;38:518–24. doi: 10.1136/gut.38.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jaarin K, Gapor MT, Nafeeza MI, Fauzee AM. Effect of various doses of palm vitamin E and tocopherol on aspirin-induced gastric lesions in rats. Int J Exp Pathol. 2002;83:295–302. doi: 10.1046/j.1365-2613.2002.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sugimoto N, Yoshida N, Yoshikawa T, et al. Effect of vitamin E on aspirin-induced gastric mucosal injury in rats. Dig Dis Sci. 2000;45:599–605. doi: 10.1023/a:1005417929009. [DOI] [PubMed] [Google Scholar]
- 94.Sobala GM, Pignatelli B, Schorah CJ, et al. Levels of nitrite, nitrate, N-nitroso compounds, ascorbic acid and total bile acids in gastric juice of patients with and without precancerous conditions of the stomach. Carcinogenesis. 1991;12:193–8. doi: 10.1093/carcin/12.2.193. [DOI] [PubMed] [Google Scholar]
- 95.O'Connor HJ, Schorah CJ, Habibzedah N, Axon AT, Cockel R. Vitamin C in the human stomach: relation to gastric pH, gastroduodenal disease, and possible sources. Gut. 1989;30:436–42. doi: 10.1136/gut.30.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sobala GM, Schorah CJ, Shires S, et al. Effect of eradication of Helicobacter pylori on gastric juice ascorbic acid concentrations. Gut. 1993;34:1038–41. doi: 10.1136/gut.34.8.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Becker JC, Grosser N, Boknik P, Schröder H, Domschke W, Pohle T. Gastroprotection by vitamin C – a heme oxygenase-1 dependent mechanism ? Biochem Biophys Res Commun. 2003;312:507–12. doi: 10.1016/j.bbrc.2003.10.146. [DOI] [PubMed] [Google Scholar]
- 98.Immenschuh S, Ramadori G. Gene regulation of heme oxygenase-1 as a therapeutic target. Biochem Pharmacol. 2000;60:1121–8. doi: 10.1016/s0006-2952(00)00443-3. [DOI] [PubMed] [Google Scholar]
- 99.Guo JS, Cho CH, Wang WP, Shen XZ, Cheng CL, Koo MW. Expression and activities of three inducible enzymes in the healing of gastric ulcers in rats. World J Gastroenterol. 2003;9:1767–71. doi: 10.3748/wjg.v9.i8.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wallace JL, Miller MJ. Nitric oxide in mucosal defense: a little goes a long way. Gastroenterology. 2000;119:512–20. doi: 10.1053/gast.2000.9304. [DOI] [PubMed] [Google Scholar]
- 101.Fischer H, Becker JC, Boknik P, et al. Expression of endothelial cell-derived nitric oxide sythase (eNOS) is increased during gastric adaptation to chronic aspirin intake in humans. Aliment Pharmacol Ther. 1999;13:507–14. doi: 10.1046/j.1365-2036.1999.00489.x. [DOI] [PubMed] [Google Scholar]
- 102.Foresti R, Motterlini R. The heme oxygenase pathway and its interaction with nitric oxide in the control of cellular homeostasis. Free Radic Res. 1999;31:459–75. doi: 10.1080/10715769900301031. [DOI] [PubMed] [Google Scholar]
- 103.Fiorucci S, Antonelli E, Santucci L, et al. Gastrointestinal safety of nitric oxide-derived aspirin is related to inhibition of ICE-like cysteine proteases in rats. Gastroenterology. 1999;116:1089–106. doi: 10.1016/s0016-5085(99)70012-0. [DOI] [PubMed] [Google Scholar]
- 104.Davies NM, Roseth AG, Appleyard CB, et al. NO-naproxen vs. naproxen: ulcerogenic, analgesic and anti-inflammatory effects. Aliment Pharmacol Ther. 1997;11:69–79. doi: 10.1046/j.1365-2036.1997.115286000.x. [DOI] [PubMed] [Google Scholar]
- 105.Takeuchi K, Mizoguchi H, Araki H, Komoike Y, Suzuki K. Lack of gastric toxicity of nitric oxide releasing indomethacin, NCX-530, in experimental animals. Dig Dis Sci. 2001;46:1805–18. doi: 10.1023/a:1010638528675. [DOI] [PubMed] [Google Scholar]
- 106.Cuzzolin L, Conforti A, Adami A, et al. Anti-inflammatory potency and gastrointestinal toxicity of a new compound, nitronaproxen. Pharmacol Res. 1995;31:61–5. doi: 10.1016/1043-6618(95)80049-2. [DOI] [PubMed] [Google Scholar]
- 107.Keeble JE, Moore PK. Pharmacology and potential therapeutic applications of nitric oxide-releasing non-steroidal anti-inflammatory and related nitric oxide-donating drugs. Br J Pharmacol. 2002;137:295–310. doi: 10.1038/sj.bjp.0704876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wallace JL, Cirino G, McKnight GW, Elliott SN. Reduction of gastrointestinal injury in acute endotoxic shock by flurbiprofen nitroxybutylester. Eur J Pharmacol. 1995;280:63–8. doi: 10.1016/0014-2999(95)00184-m. [DOI] [PubMed] [Google Scholar]
- 109.Wallace JL, McKnight W, Wilson TL, Del Soldato P, Cirino G. Reduction of shock-induced gastric damage by a nitric-oxide releasing aspirin derivative: role of neutrophils. Am J Physiol. 1997;273:G1246–51. doi: 10.1152/ajpgi.1997.273.6.G1246. [DOI] [PubMed] [Google Scholar]
- 110.Ukawa H, Yamakuni H, Kato S, Takeuchi K. Effects of cyclooxygenase-2 selective and nitric oxide-releasing nonsteroidal antiinflammatory drugs on mucosal ulcerogenic and healing responses of the stomach. Dig Dis Sci. 1998;43:2003–11. doi: 10.1023/a:1018846912032. [DOI] [PubMed] [Google Scholar]
- 111.Cicala C, Ianaro A, Fiorucci S, et al. NO-naproxen modulates inflammation, nociception and downregulates T cell response in rat Freund's adjuvant arthritis. Br J Pharmacol. 2000;130:1399–405. doi: 10.1038/sj.bjp.0703449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wallace JL, McKnight W, Del Soldato P, Baydoun AR, Cirino G. Anti-thrombotic effects of a nitric oxide-releasing, gastric-sparing aspirin derivative. J Clin Invest. 1995;96:2711–8. doi: 10.1172/JCI118338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hawkey CJ, Jones JI, Atherton CT, et al. Gastrointestinal safety of AZD3582, a cyclooxygenase inhibiting nitric oxide donator: proof of concept study in humans. Gut. 2003;52:1537–42. doi: 10.1136/gut.52.11.1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jovanovic DV, Fernandes JC, Martel-Pelletier J, et al. In vivo dual inhibiton of cyclooxgenase and lipooxygenase by ML-3000 reduces the progression of experimental osteoarthritis: suppression of collagenase 1 and interleukin-1beta synthesis. Arthritis Rheum. 2001;44:2320–30. doi: 10.1002/1529-0131(200110)44:10<2320::aid-art394>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 115.Wallace JL, Carter L, McKnight W, Tries S, Laufer S. ML 3000 reduces gastric prostaglandin synthesis without causing mucosal injury. Eur J Pharmacol. 1994;271:525–31. doi: 10.1016/0014-2999(94)90814-1. [DOI] [PubMed] [Google Scholar]
- 116.Palmer R, Bias P, Buchner A, Elsässer R. Licofelone (ML3000), an inhibitor of COX-1, COX-2 and 5-LOX, is associated with less gastric damage than naproxen and is similar to placebo in man. Gastroenterology. 2002;122(Suppl. 1):A54. [Abstract]. [Google Scholar]
- 117.Klesser B, Bias P, Buchner A. Licofelone (ML3000), an inhibitor of COX-1,COX-2 and 5-LOX, has little or no effect on the gastric mucosa after 4 weeks of treatment. Ann Rheum Dis. 2002;61(Suppl.):130S–131S. [Abstract]. [Google Scholar]
- 118.Reginster JY, Bias P, Buchner A. First clinical results of licofelone (ML3000), an inhibitor of COX-1, COX-2 and 5-LOX, for the treatment of osteoarthritis. Ann Rheum Dis. 2002;61(Suppl.):116S. [Abstract]. [Google Scholar]
- 119.Pavelka K, Bias P, Buchner A, Lammerich A, Schulz U. Licofelone, an inhibitor of COX-1, COX-2 and 5-LOX, is as effective as celecoxib and shows improved tolerability during 12 weeks of treatment in patients with osteoarthritis of the knee [EULAR 2003, abstract FRI0215] Ann Rheum Dis. 2003:62. [Google Scholar]
- 120.Buchner A, Bias P, Lammerich A. Twice the therapeutic dose of licofelone – an inhibitor of COX-1, COX-2 and 5-LOX – results in a significantly lower gastrointestinal ulcer incidence than naproxen in osteoarthritis patients, when administered with or without concomitant low-dose aspirin [EULAR 2003; abstract FRI0214] Ann Rheum Dis. 2003:62. [Google Scholar]
- 121.Fiorucci S, Distrutti E, de Lima OM, et al. Relative contribution of acetylated cyclo-oxygenase (COX)-2 and 5-lipoxygenase (LOX) in regulating gastric mucosal integrity and adaptation to aspirin. FASEB J. 2003;17:1171–3. doi: 10.1096/fj.02-0777fje. [DOI] [PubMed] [Google Scholar]
- 122.Tries S, Laufer S, Radziwon P, Breddin HK. Antithrombotic and platelet function inhibiting effects of ML3000, a new antiinflammatory drug with Cox/5-LOX inhibitory activity. Inflamm Res. 2002;51:129–34. doi: 10.1007/pl00000284. [DOI] [PubMed] [Google Scholar]
- 123.Lewis DF, Ioannides C, Parke DV. A retrospective study of the molecular toxicology of benoxaprofen. Toxicology. 1990;65:33–47. doi: 10.1016/0300-483x(90)90077-t. [DOI] [PubMed] [Google Scholar]
- 124.Henry D, Lim LL, Garcia Rodriguez LA, et al. Variability in risk of gastrointestinal complications with individual non-steroidal anti-inflammatory drugs: results of a collaborative meta-analysis. Br Med J. 1996;312:1563–6. doi: 10.1136/bmj.312.7046.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.National Institute for Clinical Excellence. Guidance on the use of cyclo-oxygenase (Cox) II selective inhibitors, celecoxib, rofecoxib, meloxicam and etodolac for osteoarthritis and rheumatoid arthritis. Technol Appraisal Guidance. 2001;27:1–14. Available from: URL: http://www.nice.org.uk.