Abstract
Background
Recent studies have identified the ‘triple whammy’ in which combinations of diuretics, nonsteroidal anti-inflammatory drugs (NSAIDs), ACE inhibitors (ACEI) and/or angiotensin receptor antagonists (ARA) may impair renal function.
Methods
We performed a cross-sectional study of patients admitted to a general medical ward of a teaching hospital. Age, sex, disease status and prior consumption of the ‘target’ drugs, diuretics, NSAIDs (including aspirin), ACEI and ARA were correlated with creatinine and creatinine clearance on admission.
Results
Three hundred and one patients (48% male) were included, 135 were on no prior target drugs, 87 on one, 60 on two and 19 on three such drugs. There was a significant (P < 0.01) correlation between both creatinine and creatinine clearance with male sex, age and number of target drugs. Multivariate analysis confirmed these associations but did not support associations between renal function and heart failure or total number of diagnoses. Increasing doses of diuretics, possibly because in many cases this included two drugs, but not the other drugs, were significantly (P < 0.001) associated with impaired renal function. For the other three drug groups patients on doses of any drug at lower than the defined daily dose (DDD) did not have significantly different creatinine or creatinine clearance from those on doses at or above the DDD.
Conclusion
Taking two or more of the identified drugs was associated with significant renal impairment but did not correlate with heart failure or other diseases for which the drugs might have been prescribed. Care is necessary to balance the demonstrated advantages of these medications against the risk of inducing renal failure.
Keywords: ACE inhibitors, creatinine clearance, diuretics, nonsteroidal anti-inflammatory drugs, renal failure
Introduction
Recent articles have coined the term ‘triple whammy’ for the adverse effect of combinations of angiotensin converting enzyme inhibitors (ACEI)/angiotensin receptor antagonists (ARA), diuretics and nonsteroidal anti-inflammatory drugs (NSAIDs), particularly in the elderly [1, 2]. A number of different mechanisms are probably involved, including inhibition of both prostaglandin-mediated control of glomerular afferent arteriolar tone and angiotensin control of efferent arteriolar tone [3]. Diuretics decrease the plasma volume, thus reducing renal plasma flow.
A recent Australian study found that between 4.7% and 7.9% of patients attending general practices were prescribed combinations of medications that could theoretically precipitate renal failure [4]. There is no information about the frequency with which renal failure occurs in this context or about factors other than age that may contribute to increased risk. In an attempt to clarify some of these issues we conducted a cross-sectional study of patients admitted to a teaching hospital general medical ward. Our hypothesis was that patients taking one or more drugs from ACEI/ARA, diuretics or NSAIDs prior to admission would have reduced creatinine clearance and increased creatinine concentrations on admission compared with patients on no medications from these groups.
Methods
The study was approved by the Northern Sydney Health Human Research Ethics Committee and patients signed a Consent Form. All patients admitted to one medical ward over a 3-month period were considered for the study. We excluded postoperative patients, overdose patients or those previously diagnosed with serious kidney disease, e.g. cancer of the kidney. Patients with known renal failure were not excluded but were subjected to separate subanalysis. Three hundred and one patients were available for analysis.
Data regarding patient demographics, weight, medical diagnoses, drug history prior to admission (ACEI, ARA, diuretics, NSAIDs including aspirin), duration of treatment and dose of each medication [analysed as defined daily dose (DDD) in order to allow dose comparisons between different drugs within a class] were collected [5]. Medications prescribed after admission were not included in the analysis. Where possible creatinine clearance (CrCl) was calculated but in this sick, elderly population accurate weight was only measured in a minority of patients and could only be obtained by asking those patients who were not cognitively impaired. Kidney function was also determined using serum creatinine (Cr) taken on admission (Table 1). Subjects were divided into four groups: none (control), one, two or three of the drugs of interest or ‘target’ drugs (two diuretics were considered as ‘one drug’). Data were analysed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA). Initial analysis for two continuous variables was by bivariate correlation. For one continuous and one categorical variable an unpaired t-test or a one-way anova was used. For two categorical variables χ2 was used. Variables showing significant (P < 0.05) associations with Cr or CrCl were subjected to multivariate analysis.
Table 1.
Creatinine concentrations used to evaluate the level of renal function, creatinine concentrations obtained from Pacific Laboratory Medical Services, creatinine clearance from Nankievell (2001)
| Creatinine (mmol l−1) | Creatinine | ||
|---|---|---|---|
| Kidney function | Females | Males | clearance (ml s−1) |
| Below normal | <0.05 | <0.06 | >2.00 |
| Normal | 0.05–0.09 | 0.06–0.10 | 1.33–2.00 |
| Impaired | 0.10–0.19 | 0.11–0.20 | 0.50–1.32 |
| Renal failure | >0.19 | >0.20 | <0.50 |
Results
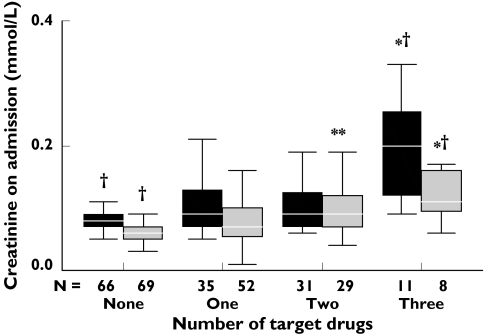
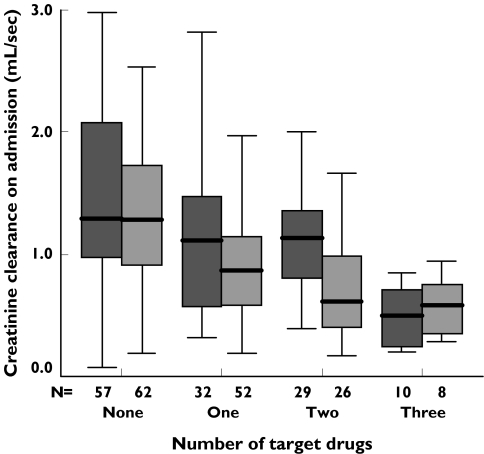
The median age for the total population was 72 years (range 19–100). There was no significant difference in the sex and weight distribution between groups. Weight was either measured or available from the patient in 88–95% of subjects (Table 2). There were 135 control patients on no target drugs, 87 on one, 60 on two and 19 on three with a significant association between both age (P < 0.001) and number of diagnoses (P < 0.01) in subjects of both sexes on one or more target drugs (Table 2). Increasing age was significantly associated with Cr (correlation coefficient R = 0.116, P = 0.04). As expected, median concentrations of serum Cr in males were higher than those observed in females (Figure 1), mean, but not median, Cr concentrations for men in all groups on one or more medications were above the normal male range of the testing laboratory (Table 1 and Fig. 1). This was not associated with type or number of diagnoses. Figure 1 demonstrates significant increases in admission Cr for women on two and three and men on three target drugs compared with those on none, with a significant combined overall trend as number of drugs increased (F = 4.21, P = 0.008). Figure 2 plots CrCl in those patients in whom it could be calculated. For both men and women there was a significant (P < 0.001) deterioration in median CrCl in patients on one or more target drugs compared with those on no target drugs.
Table 2.
Patient demographic distribution between groups on none, one, two and three target drugs
| Number of target drugs | None | One | Two | Three |
|---|---|---|---|---|
| n (301) | 135 | 87 | 60 | 19 |
| Percent males | 50 | 40 | 52 | 58 |
| Age, mean ± SD | 58 ± 21 | 70 ± 17* | 74 ± 14* | 82 ± 12* |
| Range | 19–100 | 26–96 | 26–96 | 50–95 |
| Number of diagnoses | 2 | 4* | 4* | 5* |
| Previous renal failure diagnosed | 9 | 12 | 6 | 6 |
| Creatinine (mmol l−1), mean ± SD | 0.09 ± 0.11 | 0.10 ± 0.06 | 0.11 ± 0.08 | 0.16 ± 0.08* |
| Median creatinine (mmol l−1) | 0.07 | 0.08 | 0.09 | 0.14 |
| Weight reading available | 119 | 84 | 55 | 18 |
| Mean weight ± SE, kg | 68 ± 14 | 65 ± 13 | 68 ± 15 | 66 ± 8 |
| Range | 40–120 | 42–99 | 40–109 | 50–80 |
| Creatinine clearance (ml s−1) ± SE | 1.39 ± 0.65 | 1.04 ± 0.55** | 0.93 ± 0.46** | 0.53 ± 0.24** |
| Median creatinine clearance (ml s−1) | 1.29 | 0.89 | 0.90 | 0.58 |
Creatinine and creatinine clearance levels:
P < 0.01;
P < 0.001.
Figure 1.
Creatinine levels for males and females vs. number of target drugs. P for trend (for both males and females combined = 0.008). Significant difference from control, *P < 0.05; **P < 0.001. Significant difference between males and females in groups on same number of target drugs, †P < 0.05. The box plot shows median and the quartiles directly above and below the median. The outer bars show the outer two. Male (▪), female ( )
)
Figure 2.
Creatinine clearance for males and females vs. number of target drugs, P for trend (for both males and females combined) <0.001. Decreased creatinine clearance for both sexes on one, two and three target drugs P < 0.001, decreased creatinine clearance for males on two target drugs P < 0.05 and three target drugs P < 0.001, decreased creatinine clearance for females on one, two and three target drugs P < 0.001, significant difference between males and females on the same number of target drugs: one target drug P < 0.05, two target drugs P = 0.001. Male ( ), female (
), female ( )
)
Of the patients on two agents 50% were on an ACEI/diuretic combination. Of those on three drugs all but one were on ACEI/diuretic/NSAID treatment, the other was on ARA/diuretic/NSAID treatment. There was a significant association between increasing dose of individual diuretics and creatinine and creatinine clearance (P < 0.001), but not for any of the other drug groups in whom patients on doses lower than DDD did not have lower mean Cr or higher CrCl than patients on doses at or above the DDD. There were significant positive associations between Cr concentrations, and duration of treatment with diuretics (P < 0.001) and NSAIDs (P < 0.001), but not with ACEI and ARA.
Multivariate analysis
The preliminary data analysis showed that the number of target drugs, heart failure, previously diagnosed renal failure and total number of diagnoses were significantly related to Cr clearance, therefore these variables were used in multivariate analysis. Number of target drugs and previously diagnosed renal failure remained significant (P = 0.036, P = 0.019) but heart failure and total number of diagnoses did not.
The number of target drugs, sex, age, heart failure and previously diagnosed renal failure were significantly related to Cr levels, therefore these variables were used in a multivariate analysis. Number of target drugs (P = 0.002), age (P = 0.025), sex (P = 0.011) and known renal failure (P = 0.001) remained significant. A diagnosis of heart failure did not.
Discussion
In this cross-sectional ‘snapshot’ study 55% of patients admitted to a general medical ward were taking one or more drugs known to be associated with impaired renal function. Over 25% of all patients were on two or three such drugs, which is much higher than in a younger outpatient population [4]. The number of target drugs taken prior to admission showed a very strong association with admission Cr and CrCl, especially in those patients on a combination of three drugs. This was confirmed by multivariate analysis. The median age of the patients on these was 76 years compared with 62 years in the others, suggesting that older patients are at greater risk of experiencing the ‘triple whammy’ effect [1, 2], presumably because of the known reduction in CrCl with increasing age. Simple statistical analysis suggested an association between heart failure with both Cr and CrCl and for number of diagnoses with CrCl. None of these associations was sustained by multivariate analysis. Not surprisingly, the association between previous known renal failure, in 11% of the total population, remained significant. In this subgroup there was no significant association with number of target drugs (Table 2).
That there was a significant positive association between number of drugs, Cr and CrCl, even in subjects on lower than DDD, suggests that low doses of several drugs in combination will not necessarily reduce adverse reactions. Particular care will be necessary with regard to the recent availability of fixed combinations of ACEI or ARA with diuretics.
We included aspirin in the NSAID group as many older patients take daily, small, prophylactic doses of this drug and almost three-quarters of those on three drugs were taking aspirin. A recent study has suggested that both paracetamol and aspirin might contribute to chronic renal failure [6]. In older patients it is therefore of especial importance to limit the number of drugs taken at any one time and to include low-dose aspirin in medication reviews. It is difficult to interpret the significance of our finding that increased duration of treatment with diuretics and/or anti-inflammatory agents (but not ACEI/ARA) correlated with renal impairment. In the case of diuretics it might relate to duration of hypertension or of heart failure. The lack a similar correlation with ACEI/ARA may be due to our relatively small sample.
Our study has a number of limitations. We assessed creatinine and creatinine clearance only on admission and without consideration of other possible reasons for elevated Cr such as increasing heart failure or dehydration prior to admission, but an association with heart failure or any diagnosis other than renal failure was not sustained on multivariate analysis. We consider that the strength of association we found between renal function and number of target drugs suggests a true relationship, particularly in the context where known associations such as age and sex were identified as statistically significant. A much larger prospective study would be required to identify the complex relationships between disease, age, medications, duration of therapy and renal function.
In performing this study we were disturbed to find that only about one-third of patients had their weight measured on admission to hospital. In some cases this related to their degree of sickness or frailty, but in many instances it appeared due to lack of appropriate equipment or procedures in the wards. Since the calculation of CrCl is critical for appropriate prescribing of many drugs, e.g. aminoglycosides and low-molecular-weight heparin, we are currently addressing this problem in our hospital.
Our results reinforce previously reported observations of the ‘triple whammy’ effect and we share concerns about the widespread use of two or more of these drugs. Medications for hypertension and heart failure have the important potential to reduce the likelihood of stroke and myocardial infarction, but care must be taken to ensure that this is not achieved at the price of inducing renal failure, especially in the elderly. Consideration should also be given by regulatory authorities to including appropriate Precautionary statements in the Product Information of all relevant medications.
References
- 1.Thomas MC. Diuretics, ACE inhibitors and NSAIDs – the triple whammy. Med J Aust. 2000;172:184–5. doi: 10.5694/j.1326-5377.2000.tb125548.x. [DOI] [PubMed] [Google Scholar]
- 2.Mathew T. Drug-induced renal disease. Med J Aust. 1992;156:724–8. doi: 10.5694/j.1326-5377.1992.tb121517.x. [DOI] [PubMed] [Google Scholar]
- 3.Greger R. Physiology of renal sodium transport. Am J Med Sci. 2000;319:51–62. doi: 10.1097/00000441-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Kerr SJ, Mant A, Horn F, et al. Lessons from early large-scale adoption of celecoxib and rofecoxib by Australian general practitioners. Med J Aust. 2003;179:403–7. doi: 10.5694/j.1326-5377.2004.tb05939.x. [DOI] [PubMed] [Google Scholar]
- 5.Walley T, Roberts D. Average daily quantities: a tool for measuring prescribing volume in England. Pharmacoepidemiol Drug Saf. 2000;9:55–8. doi: 10.1002/(SICI)1099-1557(200001/02)9:1<55::AID-PDS467>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 6.Fored CM, Ejerblad E, Lindblad P, et al. Aceaminophen, aspirin, and chronic renal failure. N Engl J Med. 2001;345:1801–8. doi: 10.1056/NEJMoa010323. [DOI] [PubMed] [Google Scholar]