Abstract
Aims:
To monitor statin prescribing trends over time in order to determine whether prescribers were influenced by study results and/or clinical guidelines in terms of type and dosage of statin prescribed.
Methods
The GMS (General Medical Services) prescription database in Ireland was used to identify a cohort of patients, prescribed statins, in order to investigate prescribing trends from January 1998–December 2002. Statin prescribing rates for patients with ischaemic heart disease and diabetes were compared with rates in the general GMS population. Logistic regression analysis was used in patients with ischaemic heart disease and diabetes and adjusted odds ratios and 95% confidence intervals presented.
Results
Increased statin prescribing over time was noted (test for linear trend P < 0.0001). Pravastatin was the most frequently prescribed, followed by atorvastatin; simvastatin and fluvastatin showed lower rates of prescribing. Atorvastatin showed the greatest increased rate over time. An increase in the overall dose prescribed (test for trend P < 0.01) was chiefly due to increases in pravastatin dose, but doses were still below those recommended from clinical trials. Statins were prescribed more frequently in patients with ischaemic heart disease and diabetes, 44% (95% CI 43–45%) compared with the total GMS population, 7.7% (95% CI 7.6–7.8%), by December 2002. However, statins were only prescribed to 52% (95% CI 51–53%) of ischaemic heart disease patients and 40% (95% CI 39–41%) of patients with diabetes by December 2002. Patients aged 45–64 years were more likely to receive statins, compared with those aged 65 years and older.
Conclusion:
These findings suggest that the beneficial effects of statins shown in clinical studies may not be achieved in practice.
Keywords: Statins, prescribing trends, guidelines, clinical practice
Introduction
Statins (3 - hydroxy -3 - methyl glutaryl coenzyme A reductase inhibitors) have been shown to be effective lipid-lowering agents [1]. Their beneficial effects in the primary and secondary prevention of cardiovascular disease have been well documented in several large randomized controlled studies [2–4]. However, several studies have shown [5, 6] that prescription of statins lags behind the trial results, resulting in inadequate protection for those patients who would benefit from such therapy. A previous study undertaken at primary care level [7] in Ireland examined the prescribing patterns of statins over a 4-year period (1994–8) and noted that, while statin prescribing increased during that period, usage was not directed at the population likely to benefit the most from statin therapy.
Since 1998, several guidelines have been issued at national and international level, recommending the use of statins in patients who have, or who are judged to be at high risk of developing, cardiovascular disease [8–10]. The aims of this study were to monitor the prescribing patterns of statins in Ireland over time to see if prescribers were influenced by study results and/or clinical guidelines in terms of prescribing rates and type of statin prescribed and to determine whether patients were being prescribed adequate dosage of statins.
Methods
The General Medical Services (GMS) prescription database was used to identify the study population. The GMS scheme provides free health services, including provision of medicines without charge to 1.2 million people in Ireland [11]. Eligibility for this service is primarily means-tested, therefore groups such as children, the elderly and the socially disadvantaged are over represented with respect to the general population. In addition, in July 2001 the GMS scheme was expanded to incorporate all people aged 70 years and over, irrespective of their means, which increased the percentage of elderly subjects covered by the GMS scheme to 27% of the total GMS population [11].
Although the GMS covers only approximately 30% of the population, previous reports have estimated that it accounts for up to 70% of all medicines prescribed in primary care in Ireland [12]. In 2002, more than 77% of eligible GMS patients were prescribed for during the year, amounting to a total cost of 550 million [11]. The GMS database records basic demographic information on the patients (such as age and sex) and full details on all items dispensed within the scheme. Medicines are coded using the WHO Anatomical Therapeutic Chemical (ATC) classification system [13]. No data on diagnosis are available on the database.
For the purpose of this study the GMS prescription database from the Eastern Regional Health Authority (the largest health board in the country with approximately 344 000 eligible GMS patients) was used to identify a cohort of patients, aged 16 years of age and older, who had been prescribed statins, in order to investigate prescribing trends. Data were available for review from January 1998–December, 2002.
During the period of the study, a total of five statins were available on the market as follows: C10AA01 (simvastatin), C10AA03 (pravastatin), C10AA04 (fluvastatin), C10AA05 (atorvastatin) and C10AA06 (cerivastatin). However cerivastatin, which was placed on the market in 2000 was withdrawn by the company worldwide in 2001; therefore this statin was not included in any analysis.
Patients with presumed ischaemic heart disease (IHD) were identified by prescription of both aspirin and nitrate in any month (using ATC codes C01DA, B01AC06 and N02BA01). Co-prescription of these drugs has been shown to be a valid surrogate marker for identifying IHD patients in previous studies [14, 15]. Patients with diabetes mellitus (DM) were identified by prescription of any of the following: insulin, insulin analogue or oral hypoglycaemic therapy (using ATC codes A10A and A10B)
Statistical analysis
Rates per 1,000 GMS population were computed over time for statins and age-adjusted for gender comparisons. Medians are presented for statins dosing data as these were non-normal; a linear regression was used to test for trend over time, as the data show a monotonically increasing trend for prescribing of statin therapy over time. Differences between slopes were examined and 95% confidence intervals for differences between slopes calculated. Logistic regression analysis was used to predict statin prescribing in subsets of patients with IHD and DM as defined previously. Females, those aged 65 years and over, and the year 1998 were the reference categories. Odds ratios (OR) adjusted for age and gender and 95% confidence intervals are presented. All analyses were performed using SAS version 8.0 (SAS Institute Inc., Cary, NC). Statistical significance at P < 0.05 is assumed throughout.
Results
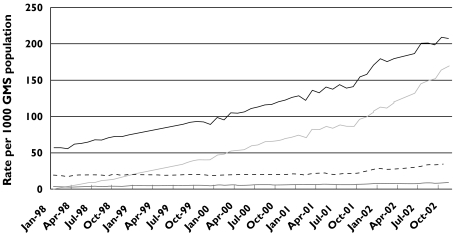
The overall statin prescribing pattern for the period 1998–2002 is shown in Figure 1. Prescribing of each statin increased steadily during this time, the increase showing a significant linear trend from January 1998 up until July 2001 (P < 0.001), at which point all patients over 70 years of age were eligible to join the GMS scheme. After July 2001, a sharper rise in the rate of statin prescription was noted. However, by the end of 2002, statins were prescribed to only 7.7% of the eligible GMS population (n = 20,399/266 626 GMS patients aged ≥16 years). Pravastatin remained the most commonly prescribed statin although the greatest increased rate in prescriptions was noted for atorvastatin. Examining the slopes between the various statins (Figure 1): fluvastatin shows the slowest increase (slope = 0.104, increase per month, P < 0.0001), then simvastatin (slope = 0.255, P < 0.0001), pravastatin (slope = 3.04, P < 0.0001), and atorvastatin (slope = 3.08, P < 0.0001). There was no significant difference between the slopes for atorvastatin and pravastatin (difference in slopes = 0.04, 95% CI −0.16, 0.24). However there was a statistically significant difference between the slopes for simvastatin and pravastatin (difference = −2.79, 95% CI −2.93, −2.64) and between simvastatin and atorvastatin (difference =−2.83, 95% CI −2.98, −2.68).
Figure 1.
Trends in prescribing of statins 1998–2002, by statin type. Simvastatin ( ), fluvastatin (
), fluvastatin ( ), atorvastatin (
), atorvastatin ( ), pravastatin (
), pravastatin ( ). *Test for linear trend P < 0.0001
). *Test for linear trend P < 0.0001
An increase in overall dosage of statins prescribed was noted over time (linear trend P < 0.01), primarily attributable to increased doses of pravastatin. The median dose of pravastatin prescribed rose from 10 mg at the start of the study to 20 mg by December 2002. The median doses for atorvastatin and simvastatin remained constant during the study (10 mg and 20 mg, respectively), with the median dosage of fluvastatin, increasing from 20 mg to 40 mg during the study.
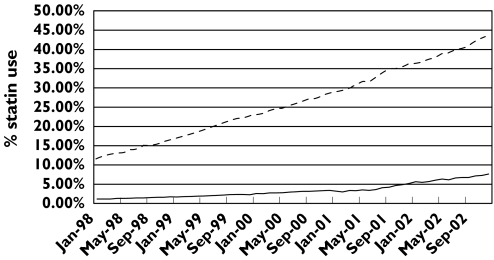
Use of statins was evaluated in patients with IHD and DM. Results showed that statins were prescribed more frequently in these patients compared with the GMS population as a whole (Figure 2). The regression slope for all patients was 0.181 (95% CI 0.17, 0.19) and for the IHD/DM patients 0.53 (95% CI 0.52, 0.54), with a statistically significant difference between slopes (difference in slopes = 0.35, 95% CI 0.33, 0.36, P < 0.01). The annual increase in statin usage was statistically significant for each of these high-risk patient groups throughout the period of review (linear trend P < 0.0001, Table 1). However, statins were still only prescribed to 44% (95% CI 43–45%) of this overall patient population by the end of 2002 – 52% (95% CI 51–53%) of IHD patients and 40% (95% CI 39–41%) of DM patients, respectively. There was no difference in statin prescription rates between males and females in the IHD group (Table 1) although males were slightly less likely than females to be prescribed statins in the diabetes group (OR = 0.86 (0.81, 0.91) Table 1). Patients aged less than 65 years were significantly more likely to receive statins than patients aged 65 years and over in the IHD group (OR = 2.16 (2.07, 2.25) Table 1). In view of the age profile within the DM group, statin prescribing rates in patients aged 65 years and over were compared with those in the following age groups: 45–64 years and 16–44 years. Results showed a significantly increased rate of statin prescribing in the 45–64 years age group compared with those aged 65 years and over (OR = 1.29 (1.21, 1.37) Table 1), but less statin prescribing was noted in the 16–44 years group compared with those 65 years and over (OR = 0.49 (0.44, 0.54)).
Figure 2.
Trends in prescribing of statins 1998–2002, by disease state. All GMS (- - -), IHD/DM only (―)
Table 1.
Adjusted odds ratios (ORs) and 95% confidence intervals (CI) for prescribing of statins in those receiving nitrates and aspirin (IHD) therapies and those receiving therapies for diabetes during the period 1998–2002
| Those receiving therapies for IHD | Those receiving therapies for diabetes | |||
|---|---|---|---|---|
| Factor | OR | 95% CI | OR | 95% CI |
| Male vs. Female | 1.04 | (0.99, 1.08) | 0.86 | (0.81, 0.91) |
| Age <65 vs.≥65 | 2.16 | (2.07, 2.25) | 1.29 | (1.21, 1.37) |
| Age 16–44 vs. ≥65 | 0.49 | (0.44, 0.54) | ||
| Year 1998* | 1.0 | 1.0 | ||
| 1999 | 1.47 | (1.36, 1.58) | 1.42 | (1.26, 1.61) |
| 2000 | 1.95 | (1.82, 2.08) | 2.12 | (1.90, 2.36) |
| 2001 | 2.63 | (2.46, 2.80) | 3.21 | (2.89, 3.57) |
| 2002 | 3.76 | (3.52,4.00) | 4.26 | (3.84,4.72) |
Test for linear trend P < 0.0001.
Discussion
The benefits of statin therapy in the primary and secondary prevention of cardiovascular disease have been shown for a wide range of patients in several large pivotal studies [2] and recommendations for their usage have been incorporated into clinical practice guidelines at national and international level [8–10, 16]. However it has been reported that prescribing frequently lags behind study results in many areas of clinical practice [17–19]. This study has shown that prescription of statins has increased significantly over the years in Ireland, especially in those groups judged to be at particular risk of cardiovascular events (patients with existing IHD and DM), however, the overall prescribing rate in the population did not reach 8% by the end of the study. This is considerably less than published estimates from the UK and Ireland. It has been estimated that 25% of the overall adult population would be potential candidates for statin therapy if the Joint European Guidelines, which have been adopted in Ireland, were implemented [7]; using similar thresholds for intervention, it has been estimated that some 16–25% of the adult UK population would be eligible for statin therapy [20]. Even in the at-risk groups examined in this study, overall usage reached a maximum of just 44% by the end of 2002. Our group has previously estimated that more than 80% of such at-risk populations would be eligible to receive an ‘evidence-based’ statin [21]. Therefore, prescription of statins in our study population was still less than desired. The findings support the lag theory as outlined above. They suggest that the data on optimal use of statins (in terms of target populations), as reported in the pivotal studies, may not have been fully understood by prescribers in primary care, resulting in under-prescribing of statins.
In this study, the prescription rates were significantly lower in the 65 years and older age group compared with patients less than 65 years, for both at-risk populations, despite the benefits from statin treatment reported in such older patients [22]. The trend for reduced prescribing in older subjects, shown in this study, has been reported before [23] and suggests a continuing prescribing age bias, reported in previous statin usage studies [5].
Several international studies have reported on the high cost of statin therapy within their health service [20, 24] and therefore the low rate of statin prescription in our study could be due to concerns over cost. Since 2001, special provision has been made for statins in the calculation of indicative drug targets [25] within the GMS drug payment scheme. As a result prescribers are not penalized for higher rates of statin prescribing. Our results showed a steady increase throughout each year of the study, which was not affected by the change in the costing status of statins in 2001. Therefore cost is unlikely to be an inhibitory factor in the prescribing of statins.
Pravastatin was the most frequently prescribed statin throughout the study. This is in keeping with the evidence base from the pivotal trials that used either pravastatin or simvastatin [26]. During the period of review the dosage of pravastatin prescribed doubled from an average of 10 mg day−1 in 1998 to 20 mg day−1 by December 2002. This finding suggests that prescribers were aware of the need to prescribe an adequate dose in order to achieve the desired effect. However, this dosage is still much less than the 40 mg dose used in the pivotal studies [22, 27], a problem that has been shown in other studies [6]. This may reflect physician concern about potential dose-related toxicity with statin use [28, 29]. Therefore, guidance on adequate dosage regimens may be required for primary care physicians in order to ensure that the beneficial clinical trial results are achieved in practice.
The rapid rise in the use of atorvastatin, which is licensed for the management of hyperlipidaemic conditions only [30] suggests that prescribers may perceive the beneficial effects of statins to be due to a class effect. However, it may also be due to the effect of atorvastatin advertising in the marketplace and to the influence of the pharmaceutical company on prescribers. Atorvastatin was introduced into the marketplace around the start of this study [30] and it has been shown previously [31, 32] that primary care physicians rely heavily on information received from pharmaceutical representatives, especially in the prescribing of new drugs. These findings highlight the need to ensure that local and regional guidelines are effectively conveyed to clinicians, in order to provide them with an evidence-based source of information to aid prescribing.
A previous study on the use of statins in this population [7] also showed a rise in statin prescribing during the period of review (1994–8); however, the level was considerably below target in that study. Our study has shown that although statin prescribing has continued to increase significantly in this population on an annual basis, it still remains well short of guideline recommendations. In addition, although the prescribed dosage regimen for pravastatin (approximately 10 mg day−1 in the previous study) has continued to increase, it would appear to be still less than adequate in this current study (at 20 mg day−1) taking into account the evidence from the pivotal studies.
The GMS prescription database relates to prescriptions dispensed and therefore we cannot be sure that the medications were taken as prescribed. Moreover, it does not contain information on patient diagnosis. However, in order to identify patients with IHD we used surrogate markers (coprescription of nitrates and aspirin) that have been judged to be sensitive markers for patients with established IHD [14, 15] with a reported sensitivity >80%. This group therefore could be said to represent a definite ‘at-risk’ population because of the presence of established heart disease, indicating a requirement for statin therapy. Patients with DM were identified by prescription of medicines only used by DM patients, such as insulin, insulin analogues or oral hypoglycaemic agents. Since this does not take into account DM patients managed on diet alone, it is likely that our cohort of DM patients represents a more ‘at-risk’ subgroup, where statin therapy would be definitely indicated.
In conclusion, this study has shown consistent and significant increases in statin prescribing rates in this patient population over a 4-year period. However, the rate of prescribing is still below that recommended for the population in general and for at-risk groups such as IHD and DM patients in particular. Moreover, the type of drug and dosages prescribed still do not reflect the evidence base available from the pivotal studies. These findings suggest that the beneficial effects of statins shown in clinical studies, especially relating to drug type and appropriate dosage may not have not been adequately conveyed to prescribers and that as a consequence, the results seen in the pivotal studies may not be translated into benefit at primary care level.
Acknowledgments
We would like to thank the Irish GMS (Payments) Board for providing us with the data on which this study is based
Competing interests: None to declare.
References
- 1.Wierzbicki AS, Poston R, Ferro A. The lipid and non-lipid effects of statins. Pharmacol Ther. 2003;99:95–112. doi: 10.1016/s0163-7258(03)00055-x. [DOI] [PubMed] [Google Scholar]
- 2.LaRosa JC, He J, Vupputuri S. Effect of statins on the risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282:2340–6. doi: 10.1001/jama.282.24.2340. [DOI] [PubMed] [Google Scholar]
- 3.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of Cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trial. Lancet. 2002;360:7–22. [Google Scholar]
- 4.Sheperd J, Blauw G, Murphy M, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomized controlled trial. Lancet. 2002;360:1623–30. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 5.DeWilde S, Carey I, Bremner S, Tichards N, Hilton S, Cook D. Evolution of statin prescribing 1994–2001: a case of agism but not of sexism? Heart. 2003;89:417–21. doi: 10.1136/heart.89.4.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krappweis J, Aumann D, Rentsch A, Kirch W. The Prescribing of Lipid Lowering Drugs During a 1-Year Period. Analysis of 7490 Health Insurance Files. Pharmacoepidemiol Drug Saf. 2000;9:119–25. doi: 10.1002/(SICI)1099-1557(200003/04)9:2<119::AID-PDS476>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 7.Feely J, McGettigan P, Kelly A. Growth in use of statins after trials is not targeted to most appropriate patients. Clin Pharmacol Ther. 2000;67:438–41. doi: 10.1067/mcp.2000.105152. [DOI] [PubMed] [Google Scholar]
- 8.Wood D, De Backer G, Faergeman O, Graham I, Mancia G, Pyorala K. Recommendations of the Second Joint Task Force of European and other Societies on Coronary Prevention. Eur Heart J. 1998;19:1434–503. doi: 10.1016/s0021-9150(98)90209-x. [DOI] [PubMed] [Google Scholar]
- 9.National Institute of Clinical Excellence. Prophylaxis for patients who have experienced a myocardial infarction: drug treatment, cardiac rehabilitation and dietary manipulation. 2001 Clinical Guideline A. April, http://www.nice.org.uk.
- 10.The Stationery Office. Building Healthier Hearts. Dublin: The Stationery Office, Government Publications; 1999. The Report of the Cardiovascular Health Strategy Group; p. 74. [Google Scholar]
- 11.General Medical Services (Payments) Board. 2002 Annual Report. Dublin, http://www.gmspb.ie.
- 12.Feely J, Chan R, McManus J, O'Shea B. The influence of hospital-based prescribers on prescribing in General Practice. Pharmacoeconomics. 1999;16:175–81. doi: 10.2165/00019053-199916020-00006. [DOI] [PubMed] [Google Scholar]
- 13.WHO Collaborating Centre for Drug Statistics Methodology. Oslo, Norway: WHO; 2003. ATC Index with DDDs. [Google Scholar]
- 14.Gray J, Majeed A, Kerry S, Rowlands G. Identifying patients with ischaemic heart disease in general practice: cross sectional study of paper and computerised medical records. BMJ. 2000;321:548–50. doi: 10.1136/bmj.321.7260.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cannon PJ, Connell PA, Stockley IH, Garner SJ, Hampton JR. Prevalence of angina as assessed by a survey of prescriptions for nitrates. Lancet. 1988:979–81. doi: 10.1016/s0140-6736(88)91790-4. [DOI] [PubMed] [Google Scholar]
- 16.Anonymous. Natl Med Information Centre Bulletin. Dublin: St James's Hospital; 1999. The role of statins in prevention of coronary heart disease. 5. [Google Scholar]
- 17.Baker R, Fraser R, Stone M, Lambert P, Stevenson K, Shiels C. Randomized controlled trial of the impact of guidelines, prioritised review criteria and feedback on implementation of recommendations for angina and asthma. Br J General Pract. 2003;53:284–91. [PMC free article] [PubMed] [Google Scholar]
- 18.McKee S, Leslie S, LeMaitre J, Webb D, Denvir M. Management of chronic heart failure due to systolic left ventricular dysfunction by cardiologist and non-cardiologist physicians. Eur J Heart Fail. 2003;5:549–55. doi: 10.1016/s1388-9842(03)00003-5. [DOI] [PubMed] [Google Scholar]
- 19.Vikman S, Airaksinen KE, Peuhkurinen K, Tierala I, Majamaa-Voltti K, Niemela M, Niemela K. Gap between guidelines and management of patients with acute coronary syndrome without persistent ST elevation. Finnish prospective follow-up survey. Scand Cardiovasc J. 2003;37:187–92. doi: 10.1080/14017430310014919. [DOI] [PubMed] [Google Scholar]
- 20.Pickin D, McCabe C, Ramsay L, Payne N, Haq I, Yeo Q, Jackson P. Cost effectiveness of HMG-CoA reductase inhibitor (statin) treatment related to the risk of coronary heart disease and cost of drug treatment. Heart. 1998;82:325–32. doi: 10.1136/hrt.82.3.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feely J. The therapeutic gap – compliance with medication and guidelines. Atherosclerosis. 1999;147(Suppl 1):31–7. doi: 10.1016/s0021-9150(99)00253-1. [DOI] [PubMed] [Google Scholar]
- 22.The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–57. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 23.Williams D, Bennett K, Feely J. Evidence for an age and gender bias in the secondary prevention of ischaemic heart disease in primary care. Br J Clin Pharmacol. 2003;55:604–8. doi: 10.1046/j.1365-2125.2003.01795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ballesteros L, Fernandez San Martin M, Cuesta T, Mayor E, Lopez Bilbao C and the VICAF group. The cost of inadequate prescriptions for hypolipidaemic drugs. Pharmacoeconomics. 2001;19:513–22. doi: 10.2165/00019053-200119050-00006. 5 Part 1. [DOI] [PubMed] [Google Scholar]
- 25.Personal communication from GMS. Methodology for calculation of indicative drug targets 2001. 2001.
- 26.Anonymous. Statins: new data in secondary prevention and diabetes. Pravastatin and simvastatin are the best assessed statins. Prescrire Int. 2003;12:143–8. [PubMed] [Google Scholar]
- 27.Sacks F, Pfeffer M, Moye L, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–9. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 28.Moghadasian MH. A safety look at currently available statins. Expert Opin Drug Saf. 2002;1:269–74. doi: 10.1517/14740338.1.3.269. [DOI] [PubMed] [Google Scholar]
- 29.Ballantyne C, Corsini A, Davidson M, et al. Risk for myopathy with statin therapy in high-risk patients. Arch Intern Med. 2003;163:553–64. doi: 10.1001/archinte.163.5.553. [DOI] [PubMed] [Google Scholar]
- 30.2000 Summary of Product Characteristics for Lipitor. Pfizer October http://www.medicines.ie.
- 31.Prosser H, Almond S, Walley T. Influences on GPs’ decision to prescribe new drugs – the importance of who says what. Fam Pract. 2003;20:61–8. doi: 10.1093/fampra/20.1.61. [DOI] [PubMed] [Google Scholar]
- 32.Peay M, Peay E. The role of commercial sources in the adoption of a new drug. Soc Sci Med. 1988;26:1183–9. doi: 10.1016/0277-9536(88)90149-9. [DOI] [PubMed] [Google Scholar]