Abstract
Background
Utilization of antihypertensive drugs in the hypertension outpatient clinic is surveyed periodically in the Queen Mary Utilization of Antihypertensive Drugs Study (QUADS).
Methods
Two hundred and fifty-one patients (123 men, 128 women) were interviewed in April to December 1996, 439 patients (232 men, 207 women) in January to December 99 and 228 patients (109 men, 119 women) in April to May 2004. Their case notes were reviewed.
Results
The percentages of patients receiving no drug (lifestyle modification), one, two, three and over three drugs were 7%, 48%, 36%, 7%, 3%, respectively, in 1996; 14%, 34%, 36%, 13% and 1%, respectively, in 1999; and 3%, 30%, 40%, 22% and 6%, respectively, in 2004. The number of drugs correlated with age and overweight. In 1996, 51% patients received calcium channel blockers (CCB); 46%β-blockers (BB); 32% angiotensin-converting enzyme inhibitors (ACEI); 15% thiazide diuretics; 5% α-blockers; and 0% angiotensin receptor blockers (ARB). In 1999, the respective figures were 52% CCB, 49% BB, 24% ACEI, 22% thiazide diuretics, 4%α-blockers and 2% ARB. In 2004, the respective figures were 65% CCB, 64% BB, 33% ACEI, 24% thiazide diuretics, 4%α-blockers and 7% ARB. Fewer patients on BBs reported side-effects. Only 11% were on α statin and 9% on aspirin. Blood pressure on treatment was 147 ± 21/84 ± 11 mmHg in 1999 and 144 ± 21/82 ± 11 mmHg in 2004.
Conclusions
Increasingly, multiple drugs were used for blood pressure control. Blood pressure control needs improvement, especially in diabetics. CCBs and BBs were consistently popular. Thiazide diuretics, ARBs, statins and aspirin were underused, despite favourable clinical trial evidence.
Keywords: angiotensin-converting enzyme inhibitor, β-blocker, calcium channel blocker, drug utilization, hypertension, thiazide diuretic
Introduction
About one billion people worldwide suffer from hypertension. There are 50 million people with hypertension in the USA and 130 million in China. Due to the ‘rule of halves’, only a proportion of hypertensives are treated and even fewer have good control of blood pressure [1, 2].
Hypertension is a leading risk factor for coronary heart disease and stroke. There is now strong evidence from large clinical trials that lowering blood pressure effectively prevents these adverse outcomes [3, 4]. It is therefore important that once the diagnosis of hypertension is established, blood pressure should be adequately controlled through regular follow-up and prescription of effective antihypertensive treatment, which often entails using more than one antihypertensive drug. Accordingly, there is a need to survey the pattern of usage of antihypertensive drugs, to see if the current usage is rational, effective and tolerated. In this longitudinal study, we document the utilization of antihypertensive drugs in 1996, 1999 and 2004 as part of the Queen Mary Utilization of Antihypertensive Drugs Study (QUADS) programme [5].
Methods
Altogether, 918 patients attending the Hypertension Clinic of Queen Mary Hospital, Hong Kong, a university teaching hospital, were sampled and studied in three phases. The clinic handles referrals from family physicians, the accident and emergency department and general medical clinics. There were 251 patients interviewed in April to December 1996; 439 patients were interviewed in January to December 99 and 228 patients were interviewed in April to May 2004. In 1996 and 1999, patients were randomly selected from the clinic attendance list for interview. In 2004, every patient attending the clinic was approached. New patients attending the clinic for the first time were excluded because the diagnosis of hypertension might not have been made and any drug they were taking did not reflect the prescription practice of the clinic.
The following information was obtained from the patient through a structured questionnaire: age, duration of hypertension, number of years of treatment, the antihypertensive medications actually taken, other illnesses and medications, history of gestational hypertension, family history and social history. From the medical records, diagnoses of concomitant illnesses, height and weight were obtained. After 1998, use of aspirin, body fat percentage and blood pressure were also documented. In 2004, marital status, body mass index (BMI), waist circumference, hip circumference, heart rate, use of lipid-lowering drugs (statins and fibrates), potassium supplements, oral contraceptive, hormonal replacement therapy, antidiabetic medications, erectile dysfunction, tobacco and alcohol consumption, exercise habit, blood electrolytes and lipid profile were also studied. In 2004, patients were asked directly about adverse drug effects and about compliance.
BMI was calculated as the weight divided by the height squared (kg m−2). Overweight was defined as BMI ≥ 23 kg m−2; the normal range of BMI for the local population is between 18.5 and 22.9 kg m−2. Blood pressure was carefully measured by a trained person in the sitting position after at least 15 min of rest. The target blood pressure was systolic blood pressure (SBP) <140 mmHg and diastolic blood pressure (DBP) <90 mmHg, or SBP <130 mmHg and DBP <80 mmHg for patients with diabetes or renal disease, in whom a lower blood pressure target is beneficial [6, 7].
Antihypertensive drugs were classified into seven groups: thiazide diuretics, β-blockers (BB), calcium channel blockers (CCB), angiotensin-converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB), α-blockers and others. The latter group comprises centrally acting agents (e.g. methyldopa) and vasodilators (e.g. hydralazine).
Statistical analysis
Data were analysed using SPSS for Windows version 11.0 (SPSS Inc., Chicago, IL, USA). Patient characteristics were compared using analysis of variance or χ2 test for continuous and categorical variables, respectively. For bivariate correlations, Spearman's rank correlation coefficients were calculated. Stepwise multiple regression was used to identify independent predictor variables. P < 0.05 was considered statistically significant.
Results
The characteristics of the subjects in the 1996, 1999 and 2004 surveys are shown in Table 1. Age, years since diagnosis, weight and BMI showed an increasing trend across the surveys.
Table 1. Patient characteristics.
| 1996 | 1999 | 2004 | |
|---|---|---|---|
| Total number of patients | 251 | 439 | 228 |
| Men | 123 (49%) | 232 (53%) | 109 (48%) |
| Women | 128 (51%) | 207 (47%) | 119 (52%) |
| Age range (years) | 26–82 | 21–89 | 22–90 |
| Mean age (years) | 49 ± 12 | 56 ± 14 | 53 ± 14* |
| Height (m) | 1.62 ± 0.09 | 1.62 ± 0.09 | 1.60 ± 0.09 |
| Weight (kg) | 66.0 ± 12.0 | 67.2 ± 12.3 | 69.5 ± 14.4* |
| Body mass index (kg m−2) | 25.2 ± 3.9 | 25.7 ± 3.9 | 26.9 ± 4.5* |
| Waist circumference (cm) | – | – | 85.8 ± 10.8 |
| Years since diagnosis | 7.6 ± 7.2 | 9.4 ± 8.4 | 10.1 ± 8.9* |
| Taking antihypertensive drug(s) | 93% | 86% | 97%* |
| Gestational hypertension in female patients | 50/128 (39%) | 71/187 (38%) | 36/119 (30%) |
| Hypertension in parent(s) | 72% | 65% | 68% |
| Hypertension in sibling(s) | 42% | 46% | |
| Systolic blood pressure (mmHg) | – | 147.1 ± 21.3 | 143.9 ± 20.6* |
| Diastolic blood pressure (mmHg) | – | 83.7 ± 11.2 | 81.7 ± 10.8* |
Values are shown as mean ± SD.
P < 0.05, one-way analysis of variance.
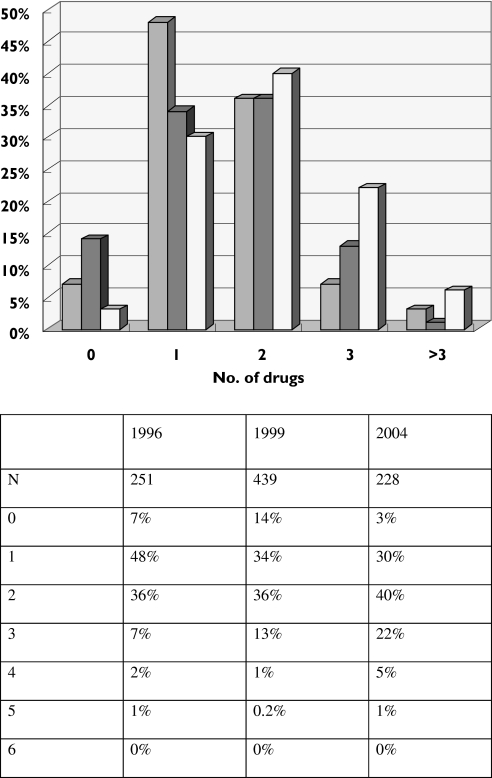
Number of antihypertensive drugs
Figure 1 shows the number of antihypertensive drug classes taken by patients. The number of antihypertensive drugs taken per patient was 1.5 ± 0.06 (mean ± SE) in 1996, 1.5 ± 0.05 in 1999 and 2.0 ± 0.06 in 2004.
Figure 1.
Number of antihypertensive drug classes taken by patients. 1996 ( ), 1999 (
), 1999 ( ), 2004 (
), 2004 ( )
)
In 1996, the number of antihypertensive drug classes taken by a patient correlated with age, sex, weight, BMI and years since diagnosis, but not with history of gestational hypertension or family history of hypertension. It correlated with the use of any of the classes of antihypertensive drugs except methyldopa, indicating that the latter was not used as an add-on medication to control blood pressure. Multiple regression showed that age (β = 0.19, P = 0.009), years since diagnosis (β = 0.19, P = 0.008) and BMI (β = 0.19, P = 0.006) were independent predictors of the number of antihypertensive drug classes (R = 0.34, P < 0.001).
In 1999, the number of antihypertensive drug classes taken by a patient correlated with age, years since diagnosis and DBP, but not with sex, weight, BMI, history of gestational hypertension or family history of hypertension. It correlated with the use of any of the classes of antihypertensive drugs except methyldopa and ARB, indicating that these were not used as add-on medications to control blood pressure. Multiple regression showed that age (β = 0.36, P < 0.001), years since diagnosis (β = 0.20, P < 0.001), BMI (β = 0.10, P = 0.03) and sex (β = 0.09, P = 0.04) were independent predictors of the number of antihypertensive drug classes (R = 0.47, P < 0.001).
In 2004, more variables were studied. The number of antihypertensive drug classes taken by a patient correlated with age, years since diagnosis, SBP, waist circumference, waist–hip ratio, diabetes, blood glucose, smoking and negatively with alcohol and drug compliance, but not with sex, weight, BMI, DBP, history of gestational hypertension or family history of hypertension. It correlated with the use of all classes of antihypertensive drugs including methyldopa and ARB, indicating that these were now used as add-on medications to control blood pressure. Multiple regression showed that age (β = 0.21, P = 0.02), waist circumference (β = 0.23, P = 0.01), SBP (β = 0.27, P = 0.001) and compliance (β = −0.33, P < 0.001) were independent predictors of the number of antihypertensive drug classes (R = 0.58, P < 0.001).
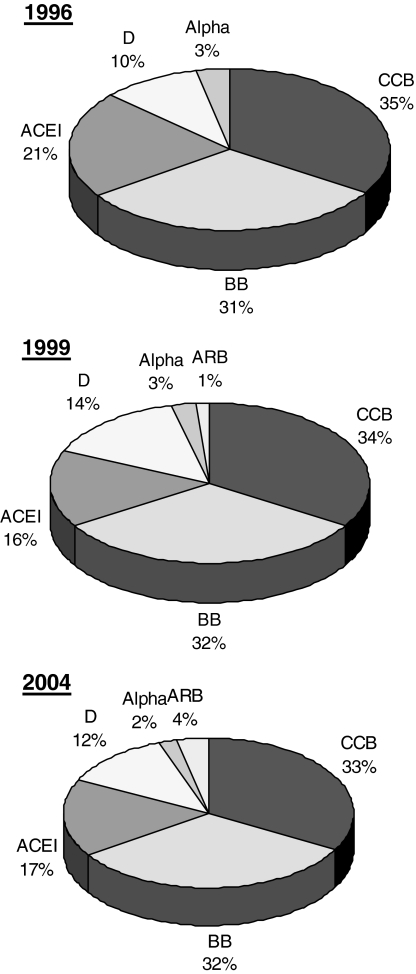
Commonly used antihypertensive drugs
Table 2 shows the percentage of patients surveyed taking a particular class of antihypertensive drug, whereas Figure 2 shows the use of each class as a percentage of all hypertensive drugs taken by patients. Table 2 shows an increase in usage of ARB, BB, CCB and diuretics, but no increase in usage of α-blockers, ACEI, methyldopa or other drug classes. However, Figure 2 shows that the relative popularity of the different classes has remained the same since 1996, with the exception of ARBs, which started to become available in 1996. CCB and BB remained the most popular drugs, as shown in Table 3.
Table 2. Percentage of patients receiving each class of antihypertensive drug.
| 1996 | 1999 | 2004 | |
|---|---|---|---|
| N | 251 | 439 | 228 |
| Alpha-blockers, % | 5 | 4 | 4 |
| ACEI, % | 32 | 24 | 33 |
| ARB, % | 0 | 2 | 7 |
| BB, % | 46 | 49 | 64 |
| CCB, % | 51 | 52 | 65 |
| Diuretics, % | 15 | 22 | 24 |
| Methyldopa, % | 3 | 1 | 2 |
| Other classes (hydralazine), % | 2 | 0.2 | 1 |
ACEI, Angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, β-blocker; CCB, calcium channel blocker.
Figure 2.
Use of each class of antihypertensive drug as a percentage of all antihypertensive drugs. Alpha, Alpha-blocker; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, β-blocker; CCB, calcium channel blocker; D, diuretic
Table 3. The leading medication regimens.
| 1996 | 1999 | 2004 | |
|---|---|---|---|
| N | 251 | 439 | 228 |
| ACEI, % | 12 | 6 | 1 |
| BB, % | 13 | 10 | 13 |
| CCB, % | 17 | 14 | 11 |
| CCB + BB, % | 16 | 18 | 17 |
| CCB + BB + ACEI,% | 11 | 4 | 10 |
ACEI, Angiotensin-converting enzyme inhibitor; BB, β-blocker; CCB, calcium channel blocker.
Women
In 1996, female hypertensive patients were younger (47.5 ± 10.1 vs. 50.7 ± 13.1, P = 0.04), less likely to be on drug treatment (P = 0.007) and likely to be on fewer drugs (P = 0.003). Calcium channel blockers, but not other drug classes, were less likely to be used in women [odds ratio (OR) 0.39, P < 0.001].
In 1999, female patients were similar to male patients in terms of age, likelihood to be on drug treatment and the number of drugs. In this sample, they were less likely to take an ACEI (OR 0.46, P = 0.001) but not CCB (P = 0.57).
In 2004, male and female patients were similar in age and the number of drugs. However, female patients were less likely to be on a CCB (OR 0.53, P = 0.03). Fewer women were on an ACEI, although this was not statistically significant (OR 0.69, P = 0.18).
The elderly
In 1996, 1999 and 2004, age was associated with drug treatment (respectively, P = 0.004, P < 0.001, P = 0.006), the number of drugs (r = 0.24, P < 0.001; r = 0.39, P < 0.001; r = 0.45, P < 0.001) and the use of a CCB (P = 0.02, P < 0.001, P < 0.001). In the 1999 and 2004 samples, achieved DBP decreased with age (r =−0.32, P < 0.001; r = −0.24, P < 0.001). Surprisingly, age did not predict the occurrence of side-effects (P = 0.25) nor the number of them (P = 0.27).
Achieved blood pressure
In 1999, the blood pressure on treatment was 147.1 ± 21.3/83.7 ± 11.2 mmHg (Table 1).
The DBP on treatment was <90 mmHg in 66% of patients (67% in men and 64% in women), but only 30% of patients (33% in men and 26% in women) had a SBP <140 mmHg as well.
In 2004, the achieved blood pressure was 143.9 ± 20.6/81.7 ± 10.8 mmHg. Ten percent of men and 7% of women achieved blood pressure in the normal range (<120/80 mmHg), whereas 36% men and 30% women achieved blood pressure in the prehypertension range (SBP 120–139 mmHg and DBP 80–89 mmHg). Blood pressure control was nonsignificantly better in men than in women (46%vs. 37%, P = 0.22). Overall, 41% had a treated blood pressure better than 140/90 mmHg. There were no significant differences between diabetic and nondiabetic patients in the achieved SBP (143.4 ± 22.8 mmHg vs. 143.9 ± 20.2 mmHg, P = 0.91) and DBP (79.9 ± 9.2 mmHg vs. 82.0 ± 11.1 mmHg, P = 0.29), respectively. Among diabetics, the blood pressure target (<130/80 mmHg) was reached in only 20% of patients. Amongst all patients including diabetics, the proportion reaching the target was only 37%.
Other medications
In 1996, 2% were taking aspirin and 5% were taking a statin. In 1999, 8% were on aspirin and 11% a statin. In 2004, 9% were on aspirin and 11% a statin.
In 1996, 5% of patients attending the hypertension clinic were diabetic and 1% were on diabetic medications. In 1999, 9% of patients attending the hypertension clinic were diabetic and 5% were on diabetic medications. In 2004, 15% were diabetic and 12% were on diabetic medications. The diabetic medications consisted of sulphonylureas and the biguanide, metformin. None of the patients was on insulin.
Adverse effects
In 2004, patients were asked if they experienced drug-related adverse effects. Among patients on antihypertensive drug therapy, 34% reported adverse effects (23% one side-effect, 8% two side-effects, 3% three side-effects). Surprisingly, the likelihood of experiencing adverse effects was unrelated to sex, age, years of treatment, number of drugs used, level of achieved blood pressure, heart rate on treatment or compliance. Fewer patients on a BB reported side-effects (OR 0.46, P = 0.008) and patients on BB reported fewer side-effects (P = 0.004).
Compliance
Compliance was studied in 2004. Of 222 patients on medications for hypertension, 213 (96%) claimed good compliance with no missing medication, whereas nine (4%) reported missing one dose every 1–2 weeks. Among these nine patients, seven were men and two were women (P = 0.19). In this sample of clinic patients of whom relatively few were noncompliant, the only statistically significant difference in patient characteristics between the noncompliant and compliant groups was the overall number of drugs the patients took (P = 0.02), and in particular the number of antihypertensive drugs (P = 0.01). The noncompliant group was not older than the good compliance group (51.4 ± 7.5 years vs. 53.5 ± 13.6 years, P = 0.08), did not report more side-effects (11%vs. 35%, P = 0.14), and also failed to reach blood pressure target (33%%vs. 37%, P = 0.88).
Discussion
It is useful to interpret the results of this study in the context of the large clinical trials and guidelines that were published in the period 1996–2004. Since 1996, many important large clinical trials (Syst-Eur [8], HOT [9], STOP2 [10], INSIGHT [11], HOPE [12], PROGRESS [13], LIFE [14], ALLHAT [15], ANBP2 [16]) have been completed. The first outcome trial using an ARB, albeit in heart failure patients, was published [17]. Major guidelines (JNC [18–20], World Health Organization/International Society of Hypertension [21, 22], European Society of Hypertension/European Society of Cardiology [23]) have been revised.
There are many studies of antihypertensive drug usage, which usually rely on prescription records [24, 25]. However, these computerized records of drug prescription provide mainly descriptive information. We attempted to go beyond a descriptive approach and find out why drugs were being used in a particular way. We interviewed every patient and examined the medical records. In 1996 and 1999, our main objective was to profile the utilization of antihypertensive drugs. In 2004, we examined, in addition, adverse drug effects and compliance, and their relationship with antihypertensive drug usage.
In a longitudinal study, patient characteristics varied over time. In addition to ageing, there is also evidence of increases in body weight and BMI. Thus, hypertension becomes more and more a manifestation of the metabolic syndrome, so that increasingly in the hypertension clinic, patients are being treated with oral medications for Type 2 diabetes and statins for hypercholesterolaemia. This is consistent with our findings of increased prevalence of the components of the metabolic syndrome in a large study of cardiovascular risk factors in the community, the Hong Kong Cardiovascular Risk Factor Prevalence Study-2 [26].
There was a trend towards an increase in the number of antihypertensive drugs taken by patients. This might reflect a worsening of the hypertension or increased intensity of treatment, or both. In 1996, 1999 and 2004, age and indices of obesity were consistent predictors of the number of drugs used, so to an extent, the increase in the number of drugs reflected increased disease severity arising from ageing and obesity. In 2004, the number of drugs was related to SBP, suggesting increasing awareness of the importance of controlling the systolic as much as the diastolic pressure. On the other hand, there was a small but significant fall in both the systolic and diastolic blood pressure on treatment in 2004 compared with 1999, suggesting that clinicians were aiming at better blood pressure control in accordance with management guidelines [20–23], thereby using more classes of drugs to achieve it. The concept of using a combination of more than one class to achieve blood pressure targets was especially promulgated by JNC7 in 2003 and echoed in local publications [20, 27].
Despite the increase in the number of drugs, remarkably, the relative popularity of the different drug classes had not changed markedly since 1996. ARBs were introduced in the clinic in 1996, but due to cost constraints, they were only used in a minority of patients. Evidence of benefit pertained to heart failure initially [17], but later extended to the treatment of hypertension [14]. Thiazides and ACEIs were also underused, perhaps because most clinicians wanted to know the renal function and electrolytes before prescribing these drugs. The prevalence of ACEI-induced cough is high in Hong Kong [28]. As there are many drug classes available for the treatment of hypertension, patients with intolerable cough are likely to stop taking the ACEI. CCBs and BB remained the most popular drugs. The former were particularly likely to be used in men and the elderly. CCBs are popular, despite the fact that there are no guidelines recommending them over and above other drug classes and there had been concerns about their safety [29]. The efficacy of CCBs in lowering blood pressure in the Chinese is excellent [30, 31], and may explain their popularity in Asia [25]. The majority of our hypertensive patients tend to have low rather than high renin [32], so the use of CCBs is appropriate and effective [33, 34]. As renin activity decreases with age [32], CCBs effectively lower blood pressure in the elderly, perhaps explaining our observation that the elderly were more likely to be on a CCB.
We also found that the elderly were likely to take more drugs and consequently have lower diastolic pressures than younger patients. This reflects current concepts of treating hypertension in the elderly, placing the emphasis on controlling systolic and diastolic pressure, using multiple drugs if necessary [20, 27]. Although age was not a predictor of side-effects or compliance in our study, polypharmacy in the elderly can potentially cause adverse effects and noncompliance.
Current guidelines do not have separate treatment algorithms for men and women. Thus, we found very little sex difference in terms of the number of drugs and the classes used, with the exception of CCBs, which appeared to be less popular among women in 1996 and 2004, but not 1999.
In the 2004 sample, we found no relationship between drug class and the likelihood of experiencing side-effects, with the exception of BBs. Patients on BBs reported fewer side-effects, either because BBs were well tolerated or because BB side-effects necessitated withdrawal of treatment. The former is more likely, as BBs are used in nearly two-thirds of our patients.
The compliance reported in this study may be an overestimate because self-assessment of compliance is not completely reliable. Also, patients attending a hypertension clinic in a university hospital may be relatively more compliant than patients in other settings.
The mean diastolic blood pressures achieved were close to the ideal blood pressures proposed in the HOT study [9]. However, SBP needs to be controlled better. Lowering the systolic pressure further necessitates taking more drugs or at higher doses. Therefore, the right balance needs to be struck between controlling the blood pressure and compromising tolerability or compliance. Although the proportion of patients reaching blood pressure target was higher in 2004 compared with 1999, fewer than half of all patients reached blood pressure target, and the proportion was even lower among diabetics. Thus, there is an urgent need to improve blood pressure control, especially among diabetics.
In conclusion, in this study of utlization of antihypertensive drugs, we found a trend towards using multiple drugs to control blood pressure. The relative popularity of different drug classes was consistent, with CCBs and BBs being the most popular, taken by nearly two-thirds of patients. The latter were best tolerated. Diastolic but not systolic pressure was well controlled. Blood pressure control needs to be improved, especially in diabetics. Thiazide diuretics, ACEIs, ARBs, statins and aspirin were underused, despite evidence of benefit in clinical trials.
Competing interests
B.M.Y.C. and C.P.L. have, at various times in the past 5 years, been reimbursed by Astra-Zenica, Boehringer, MSD, Novartis, Pfizer, Sanofi, Schwarz and Servier for organizing, attending or speaking in scientific meetings.
Acknowledgments
B.M.Y.C. is a member of the Institute of Cardiovascular Science and Medicine, University of Hong Kong, and an investigator of the Heart, Brain, Hormone and Healthy Ageing Research Centre of the Faculty of Medicine, University of Hong Kong. Amy Cheung and Fefe Law were research nurses who performed much of the data collection and documentation. Some of the results have been presented in abstract form at the First Global Conference on Cardiovascular Clinical Trials and Pharmacotherapy, Hong Kong, 2004: Wong YL, Cheung BMY. Utilization of antihypertensive drugs in a hypertension outpatient clinic in 1998 & 2004. Cardiovasc Drugs Ther 2004; 18 (Suppl. 1): 23. Financial support: none.
References
- 1.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 2.Cheung BMY, Law FCY, Lau CP. The rule of halves applies in Chinese hypertensive patients. Am J Hypertens. 2002;15:209A. [Google Scholar]
- 3.Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomized trials. Lancet. 2000;355:1955–64. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 4.Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358:1305–15. doi: 10.1016/S0140-6736(01)06411-X. [DOI] [PubMed] [Google Scholar]
- 5.Cheung BMY, Cheung AHK, Ho SPC, Lau CP, Kumana CR. Utilisation of antihypertensive drugs in a hypertension clinic in 1996 and 1998. J Clin Pharmacol. 1999;39:969. [Google Scholar]
- 6.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes. UKPDS 38. BMJ. 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 7.Lazarus JM, Bourgoignie JJ, Buckalew VM, Greene T, Levey AS, Milas NC, Paranandi L, Peterson JC, Porush JG, Rauch S, Soucie JM, Stollar C. Achievement and safety of a low blood pressure goal in chronic renal disease: the Modification of Diet in Renal Disease Study Group. Hypertension. 1997;29:641–50. doi: 10.1161/01.hyp.29.2.641. [DOI] [PubMed] [Google Scholar]
- 8.Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, Bulpitt CJ, de Leeuw PW, Dollery CT, Fletcher AE, Forette F, Leonetti G, Nachev C, O'Brien ET, Rosenfeld J, Rodicio JL, Tuomilehto J, Zanchetti A. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350(9080):757–64. doi: 10.1016/s0140-6736(97)05381-6. [DOI] [PubMed] [Google Scholar]
- 9.Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, Menard J, Rahn KH, Wedel H, Westerling S. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;51:1755–62. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 10.Hansson L, Lindholm LH, Ekbom T, Dahlöf B, Lanke J, Scherstén B, Wester P-O, Hedner T, de Faire U STOP-Hypertension-Study Group. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity in the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354:1751–6. doi: 10.1016/s0140-6736(99)10327-1. for the. [DOI] [PubMed] [Google Scholar]
- 11.Brown MJ, Palmer CR, Castaigne A, de Leeuw PW, Mancia G, Rosenthal T, Ruilope LM. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT) Lancet. 2000;356:366–72. doi: 10.1016/S0140-6736(00)02527-7. [DOI] [PubMed] [Google Scholar]
- 12.The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342:145–53. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]
- 13.PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41. doi: 10.1016/S0140-6736(01)06178-5. [DOI] [PubMed] [Google Scholar]
- 14.Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, Fyhrquist F, Ibsen H, Kristiansson K, Lederballe-Pedersen O, Lindholm LH, Nieminen MS, Omvik P, Oparil S, Wedel H LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995–1003. doi: 10.1016/S0140-6736(02)08089-3. [DOI] [PubMed] [Google Scholar]
- 15.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288:2981–97. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- 16.Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL, Johnston CI, McNeil JJ, Macdonald GJ, Marley JE, Morgan TO, West MJ Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med. 2003;348:583–92. doi: 10.1056/NEJMoa021716. [DOI] [PubMed] [Google Scholar]
- 17.Pitt B, Segal R, Martinez FA, Meurers G, Cowley AJ, Thomas I, Deedwania PC, Ney DE, Snavely DB, Chang PI. Randomised trial of losartan versus captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE) Lancet. 1997;349(9054):747–52. doi: 10.1016/s0140-6736(97)01187-2. [DOI] [PubMed] [Google Scholar]
- 18.Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V) Arch Intern Med. 1993;153:154–83. [PubMed] [Google Scholar]
- 19.Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–46. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 20.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 21.Guidelines Subcommittee. 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. J Hypertens. 1999;17:151–83. [PubMed] [Google Scholar]
- 22.Whitworth JA World Health Organization International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–92. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 23.European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension–European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–53. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Stafford RS, Furberg CD, Finkelstein SN, Cockburn IM, Alehegn T, Ma J. Impact of clinical trial results on national trends in alpha-blocker prescribing, 1996–2002. JAMA. 2004;291:54–62. doi: 10.1001/jama.291.1.54. [DOI] [PubMed] [Google Scholar]
- 25.Chou CC, Lee MS, Ke CH, Chung MH. Prescription patterns of hypertension—National Health Insurance in Taiwan. J Chin Med Assoc. 2004;67:123–30. [PubMed] [Google Scholar]
- 26.Cheung BMY, Lam TH, Lam KSL, Tam SCF, Wat NMS, Man YB, Cheng CH, Kumana CR, Lau CP. The Hong Kong Cardiovascular Risk Factor Prevalence Survey cohort—results at 7 years. J Hypertens. 2004;22(Suppl. 2):S268–9. [Google Scholar]
- 27.Cheung BMY, Lau CP, Kumana CR. Combination therapy for hypertension. Hong Kong Med J. 2003;9:224–6. [PubMed] [Google Scholar]
- 28.Woo KS, Norris RM, Nicholls G. Racial difference in incidence of cough with angiotensin-converting enzyme inhibitors (a tale of two cities) Am J Cardiol. 1995;75:967–8. doi: 10.1016/s0002-9149(99)80703-6. [DOI] [PubMed] [Google Scholar]
- 29.Pahor M, Psaty BM, Alderman MH, Applegate WB, Williamson JD, Cavazzini C, Furberg CD. Health outcomes associated with calcium antagonists compared with other first-line antihypertensive therapies: a meta-analysis of randomised controlled trials. Lancet. 2000;356(9246):1949–54. doi: 10.1016/S0140-6736(00)03306-7. [DOI] [PubMed] [Google Scholar]
- 30.Lau CP, Cheung BMY. Relative efficacy and tolerability of lacidipine and amlodipine in patients with mild-to-moderate hypertension: a randomised double-blind study. J Cardiovasc Pharmacol. 1996;28:328–31. doi: 10.1097/00005344-199608000-00021. [DOI] [PubMed] [Google Scholar]
- 31.Cheung BMY, Lau CP, Wu BZ. Efficacy and tolerability of three new dihydropyridine calcium channel blockers: amlodipine, felodipine and isradipine. Clin Ther. 1998;20:1159–69. doi: 10.1016/s0149-2918(98)80111-2. [DOI] [PubMed] [Google Scholar]
- 32.Cheung BMY, Law FCY, Tam SCF, Kumana CR, Lau CP. Plasma renin activity and aldosterone level in patients with essential hypertension. Am J Hypertens. 2002;15:210A. [Google Scholar]
- 33.Dickerson JE, Hingorani AD, Ashby MJ, Palmer CR, Brown MJ. Optimisation of antihypertensive treatment by crossover rotation of four major classes. Lancet. 1999;353:2008–13. doi: 10.1016/s0140-6736(98)07614-4. [DOI] [PubMed] [Google Scholar]
- 34.Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, Sever PS, Thom SMcG British Hypertension Society. Guidelines for management of hypertension: Report of the fourth Working Party of the British Hypertension Society, 2004—BHS IV. J Hum Hypertens. 2004;18:139–85. doi: 10.1038/sj.jhh.1001683. [DOI] [PubMed] [Google Scholar]