Abstract
Aims
Socioeconomic inequalities in statin use are a public health concern but they may also confound observational studies of statins' effectiveness. We conducted a population-based cross-sectional study in Denmark to examine the association between socioeconomic status (SES) and statin use.
Methods
We obtained data on socioeconomic status of all persons in North Jutland County, Denmark, between 1995 and 1999 from the Prevention Registry at Statistics Denmark. Data on filled statin prescriptions were identified through the County Prescription Database. We compared the 1-year prevalence proportions of statin use for different socioeconomic groups, adjusted for age and urbanization. Separate analyses were done for patients with a history of cardiovascular disease as recorded in the County Hospital Discharge Registry.
Results
Among men with cardiovascular disease, statin use in 1995 was higher in those with the highest socioeconomic status (adjusted relative prevalence proportion (RPP) among top managers 1.86, 95% CI: 1.17–2.96), and lower among retired men (RPP (95% CI) 0.63 [0.43–0.93] in old-age pensioners, and 0.66 [0.45–0.98] in the early retired), when compared with basic-level workers. The socioeconomic differences in statin use among men decreased in magnitude over time but remained throughout the study period. We found no clear social gradient in statin use among women.
Conclusions
Even in a health care system that claims to ensure a high degree of equity in medical care, we found clear indications of a socioeconomic gradient in statin use among men in the years after the launching of these drugs.
Keywords: pharmacoepidemiology, statins, socioeconomic status
Introduction
The development and introduction of the statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors) have marked an important step forwards in the treatment of hyperlipidaemia and in the prevention of atherosclerotic disease, as demonstrated by the consistent results from several large primary and secondary prevention trials [1–4]. The beneficial effects of statins have lead to their widespread use [5]; however, there are large variations in statin use between different populations, e.g. European countries, that are not fully explained by variations in cardiovascular morbidity [6]. Further, within several countries large variations of the statin use in primary care have been observed with respect to age, sex, and physician practice [7]. British and North American studies have suggested that the use of statins reflects social differences [8–11] typically related to income and the extent of self-payment [6, 12]. Most studies, however, have used prescription data and surrogate measures of socioeconomic status (SES) aggregated at a regional or general-practice level [10, 11]. Only a few small cross-sectional studies have examined the association between SES and statin use among individual patients [13, 14]. Thus, the magnitude of this association, in particular in partly tax-financed health care systems, remains unclear.
Besides their obvious public health importance, social inequalities in statin use may also have methodological implications for observational studies of the effectiveness of the drugs. Statins have been associated with so-called pleiotropic effects in observational studies. Suggested beneficial effects include a decreased risk of fractures [15, 16], dementia [17], cancer [18], multiple sclerosis [19], systemic lupus erythematosus [20], deep venous thrombosis [21], glaucoma [22], cardiac transplant rejection [23], and severe infection [24, 25]. These biologically diverse effects of statins have been ascribed to actions beyond the direct lipid-lowering effects, including actions affecting endothelial cells, platelet and macrophage functions, oxidation processes, smooth cell proliferation, and bone metabolism [26, 27]. However, residual or unmeasured confounding by higher SES and better health in patients receiving statins in observational studies may be another explanation for the observed associations. If a social gradient in use is not present in state-sponsored healthcare systems, the nonspecific health effects may be better studied in such populations. We conducted a population-based cross-sectional study in a Danish county to examine the association between SES and the use of statins in a public health care system with presumably equal access to medical care.
Methods
Setting and health care system
This registry-based study was conducted between 1 January 1995 and 31 December 1999 in North Jutland County, Denmark, within a mixed rural and urban population of approximately 500 000 inhabitants, or 9% of the Danish population. The county is served by pharmacies equipped with a computerized accounting system that transmits data to the Danish National Health Service and to the County Prescription Database established in 1991 [28].
The Danish National Health Service provides tax-supported healthcare for all county residents. The National Health Service guarantees free access to hospitals and primary medical care; in North Jutland, the latter is entrusted to 330 general practitioners (GPs). More than 90% of all prescriptions are issued by GPs [29]. The National Health Service partially reimburses the costs of most physician-prescribed drugs. Most drugs are entitled to general reimbursement, which is automatically processed at the pharmacy; for other drugs the physician is required to apply for a ‘single reimbursement’ for the individual patient. For statins, an individual application was required for all patients until December 1998 in order to receive single reimbursement. However from January 1999 and onwards, patients with ischaemic heart disease became eligible for automatic reimbursement. Regardless of the reimbursement mechanism, 75% of the medication costs were refunded to the patient.
Data on SES
Data on SES of all persons aged 18 years or more with a permanent address in North Jutland County between 1995 and 1999 were obtained from the Prevention Registry at Statistics Denmark. Classification of SES was based on the annual central registration of data on income, social benefits, employer, occupation, level of education, and age, collected from tax returns and other public registries.
The current classification of SES was introduced in 1995 and is based on the International Standard Classification of Occupations, ISCO-88 [30]. It is based on both skills and educational level and distinguishes better between persons at work, retired, or on public assistance than a merely income-based classification. Furthermore, the classification appears suitable as the Danish tax system to some extent removes income differences. In the current classification, the population is divided into three main groups: the employed, the unemployed, and persons outside the work force [31]. The group of employed is subdivided into the self-employed with employees; self-employed without employees; assisting spouses; and salaried employees. The group of salaried employees is divided according to the skills required for the job, including not only formal education, but also informal training and experience. Thus, persons in similar positions may fall in the same SES group despite having different educational levels.
The group of salaried employees is classified according to skill level as: (i) top managers in companies, public sector organizations, and legislatures; (ii) upper-level employees (e.g. physicians, nurses, academic workers, schoolteachers); (iii) intermediate-level workers (e.g. social workers, technicians, accountants, secretaries); (iv) basic-level workers (e.g. clerks, sales and service personnel, homecare helpers, craftsmen); and (v) other salaried employees (e.g. cleaners, messengers, labourers).
In 1995–99, the Danish retirement age was 67 years with a frequently used option of early retirement at age 60 for long-term members of an unemployment fund. Persons above the age of 50 receiving transitional allowance or partial retirement benefits were included in the early retirement group for this analysis; persons under the age of 67 with disability-related early retirement were analysed as a separate group. The remaining group of economically inactive persons consisted primarily of social security recipients.
Data on statin prescriptions
In Denmark, statins are available by prescription only. We used the County Prescription Database to identify all prescriptions for statins filled by the study subjects during the study period. The Prescription Database contains data on the type of drug prescribed according to the Anatomic Therapeutic Chemical classification system (ATC), and the date the prescription was filled. We identified all recorded prescriptions for statins (ATC codes: C10AA01-06 and B04AB01).
Data on discharge diagnoses of cardiovascular disease
To examine the association between SES and statin use among patients with a presumed medical indication for statins, we conducted separate analyses for persons with a history of hospitalization with cardiovascular diseases, as recorded in the County Hospital Discharge Registry. This registry stores records of all patient discharges since 1977 from all hospitals in the county, with the exception of psychiatric hospitals [32]. The available data include date of discharge and up to 20 discharge diagnoses, assigned by physicians according to the International Classification of Diseases (8th revision (ICD-8) until the end of 1993; 10th revision (ICD-10) thereafter). We identified all persons with a previous discharge diagnosis of ischaemic heart disease, ischaemic or unspecified stroke, or peripheral atherosclerotic disease (ICD 8 codes 410–414, 433–434, 440; ICD-10 codes I20-I25, I63-I64, I70). Only diagnoses recorded before the date of the first statin prescription in the individual study year were included. Records from the Prevention Registry, the Prescription Database and the Hospital Discharge Registry were linked using the civil registry number. This 10-digit number encoding birth date and gender is assigned to all Danish citizens and is used in most administrative registries to uniquely identify individuals.
Statistical analysis
For each study year, we included all persons with a permanent address in North Jutland County on 1 January. The filling of at least one statin prescription during the calendar year under study was the outcome variable in this study. First, we calculated the annual prevalence proportion of ever-use of statins for each SES group. We defined the annual prevalence proportion as the percentage of persons in the study population with at least one statin prescription during each study year (1995–99). Next, we conducted log-risk analysis, which is similar to logistic regression except that it allows for the estimation of the ratios of prevalence proportions [33]. We estimated the relative prevalence proportions of statin use separately for men and women, using basic-level salaried employees as the reference group. We adjusted for age (in categories 18–39, 40–49, 50–59, 60–66, ≥67 years) and degree of urbanization (residence in a city with >100 000 inhabitants, provincial town with 10 000–40 000 inhabitants, or rural). Basic-level employees formed the largest group and were chosen as the reference group in order to improve the statistical precision of our estimates.
We first performed an analysis of the association between SES group and statin use within the county's entire adult population, irrespective of a history of cardiovascular disease. We then performed the primary analysis of the association between SES group and statin use among persons with a history of cardiovascular disease. A likelihood ratio test for trend was done within the group of salaried employees (other, basic, intermediate and upper level employees, and top managers).
We used SAS software (version 8, SAS Institute Inc., Cary, NC). The study was approved by the Danish Data Protection Agency and by the Aarhus University Hospital Registry Board.
Results
A total of 381 930 persons aged 18 years or more were registered with a permanent address in North Jutland County on 1 January 1995. Sixty-one persons had missing data for socioeconomic status and were excluded, leaving 381 869 persons for analysis. Table 1 shows the SES of the study subjects in 1995. As expected, SES varied according to sex, age, and to a lesser degree, urbanization. A previous discharge diagnosis of cardiovascular disease was recorded in 5–10% of retired persons, and in 0.5–2% of persons within the work force.
Table 1.
Socioeconomic status (SES) of 381 869 adults in North Jutland County, Denmark, 1995
| SES | No. | Men (%) | Age (years)* | Urbanization (%)† | Cardiovascular diagnosis (%)‡ |
|---|---|---|---|---|---|
| Self-employed with employees | 5 415 | 85.8 | 46 (19–88) | 22.0 | 2.2 |
| Self-employed without employees | 16 386 | 76.4 | 45 (18–93) | 21.0 | 2.0 |
| Top managers | 4 979 | 85.8 | 47 (18–91) | 31.4 | 1.5 |
| Salaried employees, upper level | 20 887 | 56.9 | 42 (18–82) | 45.4 | 0.9 |
| Salaried employees, intermediate level | 27 973 | 40.3 | 39 (18–87) | 40.5 | 0.9 |
| Salaried employees, basic level | 104 654 | 55.7 | 36 (18–79) | 32.3 | 0.8 |
| Salaried employees, other | 22 381 | 58.9 | 39 (18–78) | 29.1 | 1.1 |
| Employees, not further specified | 10 699 | 44.5 | 27 (18–88) | 31.4 | 0.5 |
| Assisting spouses | 2 826 | 3.5 | 51 (20–81) | 14.7 | 1.1 |
| Unemployed | 24 421 | 42.3 | 40 (18–66) | 32.4 | 1.4 |
| Students | 12 238 | 44.0 | 21 (18–63) | 55.5 | 0.1 |
| Disability supplement | 23 198 | 39.0 | 56 (18–66) | 33.6 | 5.8 |
| Old-age pensioners | 70 439 | 41.7 | 74 (66–105) | 31.2 | 10.1 |
| Early retirement benefit | 15 186 | 50.9 | 62 (19–71) | 31.2 | 5.7 |
| Other economically inactive persons | 20 187 | 30.5 | 35 (18–66) | 40.6 | 1.4 |
| Total | 381 869 | 49.5 | 33.7 | 3.3 |
Median (range);
Proportion living in a city with >100 000 inhabitants;
Previous discharge diagnosis of cardiovascular disease, see text.
We identified 1761 persons who had filled at least one statin prescription in 1995; in 1999, the number rose to 6555 statin users in the county. The prevalence of statin users increased substantially between 1995 and 1999, from 0.5% (95% CI: 0.5–0.6%) to 2.0% (1.9–2.1%) in men, and from 0.4% (0.3–0.4%) to 1.4% (1.4–1.5%) in women.
After adjustment for age and urbanization, we found no substantial socioeconomic gradient in use of statins among men, when comparing upper-level employees, self-employed persons, or unemployed persons with basic-level salaried workers (reference group). However, statin use was higher in top managers throughout the study period with an adjusted relative prevalence proportion (RPP) of 1.33 (95% CI: 0.93–1.90) in 1995, and 1.30 (1.07–1.59) in 1999 compared with basic-level salaried workers. Prevalence of statin use was also higher in old age pensioners: RPP (95% CI) was 1.10 (0.82–1.48) in 1995 and rose to 1.59 (1.36–1.86) in 1999. The largest difference was seen in persons receiving disability supplement: RPP (95% CI) was 2.50 (2.02–3.10) in 1995, and 2.35 (2.08–2.66) in 1999.
In contrast to men, women tended to have a lower prevalence of statin use with increasing socioeconomic status. In 1999, the RPP (95% CI) was 0.52 (0.22–1.26) in self-employed women with employees, 0.52 (0.19–1.38) in top managers, 0.62 (0.44–0.86) in upper-level salaried employees, and 0.82 (0.64–1.06) in intermediate level salaried employees, compared with the basic-level workers. Similarly to men, female old-age retirees and disability supplement recipients were more likely to use statins: RPP (95% CI) in 1999 were, respectively, 2.28 (1.88–2.77) and 2.89 (2.46–3.40).
The use of statins in persons previously hospitalized with cardiovascular disease rose from 7.3% in 1995 to 21.8% in 1999 among men, and from 4.6% in 1995 to 15.9% in 1999 among women. User proportions and adjusted RPPs of statin use according to SES group in 1995 and 1999 are shown in Table 2 (men) and Table 3 (women). In this group of individuals with a medical indication for secondary prevention, among retired men the prevalence of statin use was lower, rather than higher, when compared with that of basic-level workers: in 1995, RPP (95% CI) was 0.63 (0.43–0.93) in old-age retirees and 0.66 (0.45–0.98) in early retirees. For male top managers with cardiovascular disease, the RPP (95% CI) in 1995 was 1.86 (1.17–2.96). The differences in prevalence proportions compared with the reference group diminished during 1995–99, but did not entirely disappear (Figure 1). Thus for men, the adjusted RPPs of statin use in 1999 were lower for the unemployed, the retirees, and the disability supplement recipients, compared with basic-level workers (Table 2). Among male salaried employees, the prevalence proportions of statin use increased with increasing SES group (other, basic, intermediate and upper level employees, and top managers): likelihood ratio test for trend P = 0.03 in 1995 and P = 0.02 in 1999. For women with cardiovascular disease hospitalizations, the RPP estimates were statistically imprecise and no clear pattern was seen (Table 3). Nevertheless, similarly to men, differences in statin use between SES groups in women tended to diminish from 1995 though 1999 (Figure 2).
Table 2.
Prevalence proportions and adjusted relative prevalence proportions (RPPs) of statin use according to socioeconomic status (SES) in 1995 and 1999 among men with a previous discharge diagnosis of cardiovascular disease
| SES | User-proportion in 1995 (%) | User-proportion in 1999 (%) | Adjusted* RPP (95% CI) in 1995 | Adjusted* RPP (95% CI) in 1999 |
|---|---|---|---|---|
| Self-employed with employees | 15.2 | 30.5 | 1.25 (0.77–2.04) | 0.94 (0.75–1.19) |
| Self-employed without employees | 11.6 | 28.7 | 1.04 (0.71–1.52) | 0.94 (0.78–1.15) |
| Top managers | 22.4 | 40.1 | 1.86 (1.17–2.96) | 1.20 (0.97–1.49) |
| Salaried employees, upper level | 15.2 | 39.3 | 1.21 (0.79–1.84) | 1.16 (0.97–1.39) |
| Salaried employees, intermediate level | 19.3 | 33.5 | 1.50 (1.04–2.15) | 0.99 (0.82–1.20) |
| Salaried employees, basic level | 12.9 | 32.8 | 1.00 | 1.00 |
| Salaried employees, other | 13.0 | 31.1 | 1.01 (0.66–1.55) | 0.94 (0.79–1.13) |
| Employees, not further specified | 13.8 | 42.9 | 1.28 (0.51–3.23) | 1.40 (0.98–1.98) |
| Assisting spouses | 16.7 | 33.3 | 1.28 (0.21–7.75) | 0.89 (0.29–2.78) |
| Unemployed | 11.8 | 23.4 | 0.90 (0.60–1.36) | 0.68 (0.50–0.92) |
| Students | 25.0 | 10.0 | 2.01 (0.36–11.13) | 0.33 (0.05–2.08) |
| Disability supplement | 11.6 | 26.4 | 0.93 (0.71–1.23) | 0.79 (0.69–0.89) |
| Old-age pensioners | 2.4 | 13.6 | 0.63 (0.43–0.93) | 0.80 (0.68–0.94) |
| Early retirement benefit | 7.6 | 31.4 | 0.66 (0.45–0.98) | 0.96 (0.83–1.11) |
| Other economically inactive persons | 15.9 | 29.0 | 1.25 (0.83–1.89) | 0.90 (0.72–1.11) |
| Total | 7.3 | 21.8 |
Adjusted for age and degree of urbanization, see text.
Table 3.
Prevalence proportions and adjusted relative prevalence proportions (RPPs) of statin use according to socioeconomic status (SES) in 1995 and 1999 among women with a previous discharge diagnosis of cardiovascular disease
| SES | User-proportion in 1995 (%) | User-proportion in 1999 (%) | Adjusted* RPP (95% CI) in 1995 | Adjusted* RPP (95% CI) in 1999 |
|---|---|---|---|---|
| Self-employed with employees | – | 13.3 | – | 0.56 (0.15–2.05) |
| Self-employed without employees | 4.8 | 25.0 | 0.47 (0.07–3.34) | 1.16 (0.65–2.09) |
| Top managers | – | 16.7 | – | 0.74 (0.12–4.44) |
| Salaried employees, upper level | 6.9 | 21.3 | 0.66 (0.16–2.68) | 0.96 (0.58–1.61) |
| Salaried employees, intermediate level | 7.0 | 17.1 | 0.69 (0.25–1.93) | 0.82 (0.53–1.27) |
| Salaried employees, basic level | 10.4 | 21.8 | 1.00 (ref.) | 1.00 (ref.) |
| Salaried employees, other | 6.5 | 22.1 | 0.64 (0.23–1.79) | 1.06 (0.70–1.62) |
| Employees, not further specified | 3.9 | 26.1 | 0.40 (0.06–2.82) | 1.22 (0.73–2.03) |
| Assisting spouses | 8.0 | 7.4 | 0.73 (0.18–2.95) | 0.29 (0.08–1.12) |
| Unemployed | 12.5 | 21.3 | 1.19 (0.62–2.28) | 0.94 (0.59–1.49) |
| Students | 16.7 | 15.4 | 2.04 (0.32–12.85) | 1.07 (0.30–3.80) |
| Disability supplement | 9.8 | 24.2 | 0.92 (0.57–1.50) | 0.98 (0.78–1.23) |
| Old-age pensioners | 1.9 | 11.1 | 0.66 (0.35–1.21) | 1.05 (0.81–1.37) |
| Early retirement benefit | 8.4 | 33.3 | 0.80 (0.42–1.52) | 1.27 (0.99–1.62) |
| Other economically inactive persons | 14.3 | 25.3 | 1.44 (0.78–2.67) | 1.15 (0.83–1.60) |
| Total | 4.6 | 15.9 |
Adjusted for age and degree of urbanization, see text.
Figure 1.
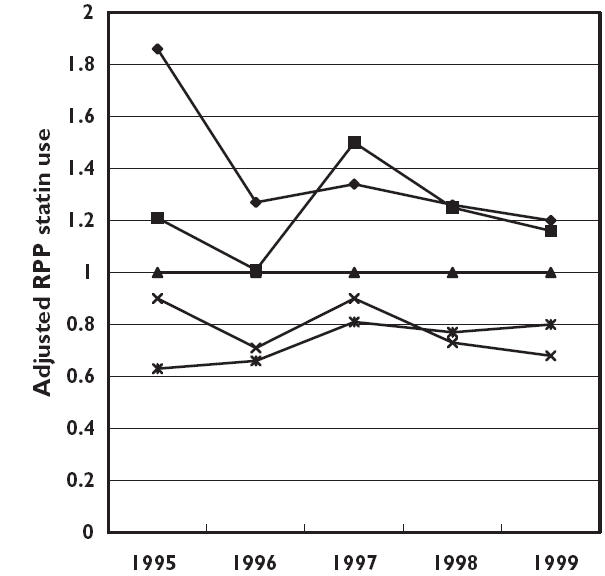
Adjusted relative prevalence proportions (RPP) of statin use in selected socioeconomic groups from 1995 to 1999 among men with a previous discharge diagnosis of cardiovascular disease. Basic level salaried employees served as the reference group in each year. Top managers (♦), upper level employees (▪), basic level employees (▴), unemployed (×), old-age pensioners ( )
)
Figure 2.
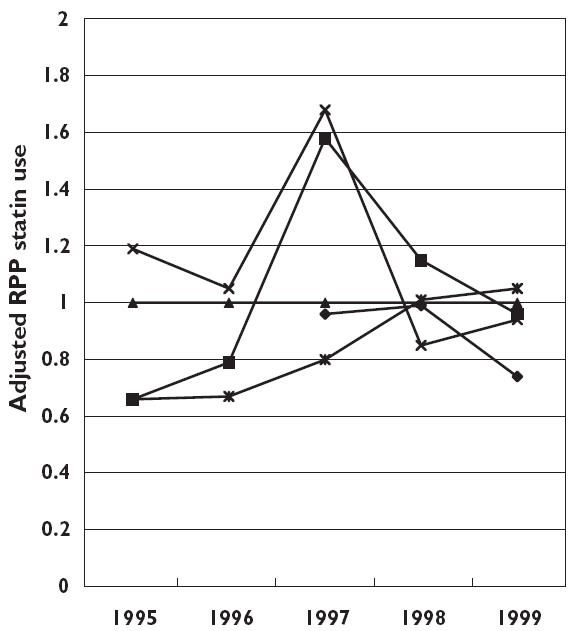
Adjusted relative prevalence proportions (RPP) of statin use in selected socioeconomic groups from 1995 to 1999 among women with a previous discharge diagnosis of cardiovascular disease. Basic-level salaried employees served as the reference group in each year. Top managers (♦), upper level employees (▪), basic level employees (▴), unemployed (×), old-age pensioners ( )
)
Discussion
In this large population-based cross-sectional study, we found substantial social differences in statin use among men with a history of hospital-diagnosed cardiovascular diseases. In this group, statin use was 20–86% higher in those with the highest socioeconomic status and up to 37% lower among retired men, compared with basic-level workers. The socioeconomic differences in statin use among men decreased in magnitude from 1995 through 1999 but did not disappear. We did not observe a clear social gradient among women. Overall in the county's population, the highest statin use was observed among retirees and among other economically inactive persons.
An important limitation of this study is its cross-sectional design, which implies uncertainty regarding whether SES preceded statin use or vice versa. The main strengths of the study are its large size and its population-based design that reduced the risk of selection bias. Approximately 2% of the study population died each year, and we had no information on statin use among persons who emigrated during the study period. However, given the low annual levels of emigration and address changes (2–3%), it is unlikely that relocation would bias our findings substantially.
The prevalence proportion has some drawbacks as a measure of occurrence of statin use, as it does not distinguish new statin users from earlier users, nor does it reflect the duration of use. We therefore cannot exclude the possibility that the results could be different for incident users and for longer-term users. Further, the quantification of statin use based on filled prescriptions is a proxy measure of the actual use. Patient compliance with statin therapy is low in some countries [34], but it is relatively high in Denmark compared, for example, with southern Europe [35]. A low SES is generally associated with decreased compliance with drug therapy [8], and the true socioeconomic differences in statin use may be greater than reported here.
The persons’ SES is recorded annually and need not reflect the lifetime social status. Individuals may have changed social status during the study period, for example, from top manager to old-age retiree. This would probably lead us to underestimate true differences in statin use between SES groups. Other SES classifications are based on income or on the level of organizational seniority and might have lead to different results [36]. It is uncertain if a merely income-based classification would be more or less correlated with differences in statin use in Denmark. The Danish National Health Service covers the majority of prescription costs, and the Danish tax system will level out income differences to a greater extent than in most other countries. Furthermore, persons on public assistance in Denmark will often have all their drug expenses covered by additional allowances from the social security system. Nevertheless, 25% of the cost of statins still represents a substantially greater expenditure for a person on a lower income than on higher income.
We adjusted our analyses for age and urbanization, and performed analyses restricted to individuals with cardiovascular discharge diagnoses only in order to avoid confounding by indication for statin use. There may be unknown or unmeasured confounders, such as comorbidity not included in the study. Finally, although our study population was large, the subdivision of persons into many SES groups resulted in statistical imprecision of the estimates, particularly among women.
Since social determinants of health care vary by time and place, we did not necessarily expect our results to be similar to those of other studies. In fact, our results are in accordance with findings from several other countries. Thus, British cross-sectional studies have suggested modest inequalities of statin use based on surrogate measures of SES such as the area of residence and primary care trusts [10, 11, 37]. In a British cross-sectional study with individual-level data, no clear association of social status with statin use was seen among 760 adults with coronary heart disease. However, nonmanual workers tended to be more likely to have statin treatment compared with manual workers (adjusted odds ratio (95% CI), 1.24 [0.85–1.82]), and statin use was also increased in house owners compared with people living in rented accommodation after adjustment for smoking and severity of coronary heart disease (adjusted odds ratio (95% CI), 1.38 [0.90–2.12]) [13]. In a cross-sectional study from the USA, Brown et al. studied 301 diabetic persons aged 65 and older, with the same pharmacy benefits [14]. Prevalence of statin use was 50% lower in patients with an annual household income under $20,000, than in patients with higher annual income.
A social gradient in statin use may reflect social differences in health, health care use, or health care quality. The information available for this study was not sufficient to distinguish between these different mechanisms. Patients in higher socioeconomic groups may be more aware of prophylactic treatment options and have better communication skills, and be therefore more likely to be prescribed statins in an individual reimbursement system that may be time-consuming for the physician. It is therefore likely that the introduction of an automatic reimbursement policy for statins for patients with ischaemic heart disease in Denmark from January 1999 may have contributed to a decrease in the socioeconomic differences in statin use in this patient group.
The use of statins in Denmark has increased as the scientific evidence for their benefits, including benefits for elderly persons, became available [38]; at the same time, statin use in Denmark has lagged behind that of many other countries, including other Scandinavian countries, probably because of restrictive national guidance and reimbursement policies [6]. The general increase in statin use may have contributed to the reduction in the socioeconomic gradient over time [37], and a recent study showed that statin use among patients with first acute myocardial infarction in Denmark has further increased from 1999 to 2002 [39]. Nevertheless, the possible under-utilization of statins by persons in lower SES groups is a public health concern. Many studies have shown that the mortality after acute myocardial infarction increases with decreasing SES [40–42]. Persons with low SES may have more severe vascular disease and may be hospitalized at a later stage of the disease than persons with high social status, underscoring the necessity of optimal medical prevention among the former.
From a methodological point of view, our results also indicate that SES may have confounded observational studies of the effects of statin use in Denmark, in particular, during the first years after statins’ introduction for secondary prevention. Such confounding could partly explain conflicting results in observational studies and posthoc analyses of randomized trials. For example, an observational study suggested a decreased risk for fractures among older women taking statins [16], while a posthoc analysis of cardiovascular trials did not [15].
In conclusion, this study suggests that even in a health care system aiming at high equity in medical care access, there may be substantial socioeconomic differences in statin use among men who have an indication for their use. Social differences tended to decrease, however, after the first few years after introduction of these drugs and may disappear over time.
Acknowledgments
The study was funded by The Danish Health Insurance Foundation. Vestdansk Forskningsforum (Western Danish Research Forum) supports the Prescription Database and Hospital Discharge Registry. The activities of the Danish Epidemiology Science Centre are partly financed by a grant from The Danish Science Foundation.
Competing interests: None to declare.
References
- 1.Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease. The Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–9. [PubMed] [Google Scholar]
- 2.Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–7. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 3.Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, Langendorfer A, Stein EA, Kruyer W, Gotto AM., Jr Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels. results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–22. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 4.MRC/BHF. Heart Protection Study of cholesterol lowering with simvastatin in 20, 536 high–risk individuals: a randomised placebo–controlled trial. Lancet. 2002. pp. 7–22. [DOI] [PubMed]
- 5.Riahi S, Fonager K, Toft E, Hvilsted-Rasmussen L, Bendsen J, Johnsen SP, Sørensen HT. Use of lipid-Iowering drugs during 1991–98 in Northern Jutland Denmark. Br J Clin Pharmacol. 2001;52:307–11. doi: 10.1046/j.0306-5251.2001.01439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walley T, Folino-Gallo P, Schwabe U, van Ganse E. Variations and increase in use of statins across Europe: data from administrative databases. BMJ. 2004;328:385–6. doi: 10.1136/bmj.328.7436.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Majeed A, Moser K, Maxwell R. Age, sex and practice variations in the use of statins in general practice in England and Wales. J Public Health Med. 2000;22:275–9. doi: 10.1093/pubmed/22.3.275. [DOI] [PubMed] [Google Scholar]
- 8.Avorn J, Monette J, Lacour A, Bohn RL, Monane M, Mogun H, LeLorier J. Persistence of use of lipid-lowering medications: a cross-national study. JAMA. 1998;279:1458–62. doi: 10.1001/jama.279.18.1458. [DOI] [PubMed] [Google Scholar]
- 9.Mamdani MM, Tu K, Austin PC, Alter DA. Influence of socioeconomic status on drug selection for the elderly in Canada. Ann Pharmacother. 2002;36:804–8. doi: 10.1345/aph.1A044. [DOI] [PubMed] [Google Scholar]
- 10.DeWilde S, Carey IM, Bremner SA, Richards N, Hilton SR, Cook DG. Evolution of statin prescribing 1994–2001: a case of agism but not of sexism? Heart. 2003;89:417–21. doi: 10.1136/heart.89.4.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ward PR, Noyce PR, St Leger AS. Are GP practice prescribing rates for coronary heart disease drugs equitable? A cross sectional analysis in four primary care trusts in England. J Epidemiol Community Health. 2004;58:89–96. doi: 10.1136/jech.58.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huskamp HA, Deverka PA, Epstein AM, Epstein RS, McGuigan KA, Frank RG. The effect of incentive-based formularies on prescription-drug utilization and spending. N Engl J Med. 2003;349:2224–32. doi: 10.1056/NEJMsa030954. [DOI] [PubMed] [Google Scholar]
- 13.Reid FD, Cook DG, Whincup PH. Use of statins in the secondary prevention of coronary heart disease: is treatment equitable? Heart. 2002;88:15–9. doi: 10.1136/heart.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown AF, Gross AG, Gutierrez PR, Jiang L, Shapiro MF, Mangione CM. Income-related differences in the use of evidence-based therapies in older persons with diabetes mellitus in for-profit managed care. J Am Geriatr Soc. 2003;51:665–70. doi: 10.1034/j.1600-0579.2003.00211.x. [DOI] [PubMed] [Google Scholar]
- 15.Bauer DC, Mundy GR, Jamal SA, Black DM, Cauley JA, Ensrud KE, van der Klift M, Pols HA. Use of statins and fracture: results of 4 prospective studies and cumulative meta-analysis of observational studies and controlled trials. Arch Intern Med. 2004;164:146–52. doi: 10.1001/archinte.164.2.146. [DOI] [PubMed] [Google Scholar]
- 16.Rejnmark L, Olsen ML, Johnsen SP, Vestergaard P, Sørensen HT, Mosekilde L. Hip fracture risk in statin users – a population-based Danish case-control study. Osteoporos Int. 2004;15:452–8. doi: 10.1007/s00198-003-1568-z. [DOI] [PubMed] [Google Scholar]
- 17.Waldman A, Kritharides L. The pleiotropic effects of HMG-CoA reductase inhibitors: their role in osteoporosis and dementia. Drugs. 2003;63:139–52. doi: 10.2165/00003495-200363020-00002. [DOI] [PubMed] [Google Scholar]
- 18.Friis S, Poulsen AH, Johnsen SP, McLaughlin JK, Fryzek JP, Dalton SO, Sørensen HT, Olsen JH. Cancer risk among statin users: a population-based cohort study. Int J Cancer. 2005;114:643–7. doi: 10.1002/ijc.20758. [DOI] [PubMed] [Google Scholar]
- 19.Zamvil SS, Steinman L. Cholesterol-lowering statins possess anti-inflammatory activity that might be useful for treatment of MS. Neurology. 2002;59:970–1. doi: 10.1212/wnl.59.7.970. [DOI] [PubMed] [Google Scholar]
- 20.Lawman S, Mauri C, Jury EC, Cook HT, Ehrenstein MR. Atorvastatin inhibits autoreactive B cell activation and delays lupus development in New Zealand black/white F1 mice. J Immunol. 2004;173:7641–6. doi: 10.4049/jimmunol.173.12.7641. [DOI] [PubMed] [Google Scholar]
- 21.Ray JG, Mamdani M, Tsuyuki RT, Anderson DR, Yeo EL, Laupacis A. Use of statins and the subsequent development of deep vein thrombosis. Arch Intern Med. 2001;161:1405–10. doi: 10.1001/archinte.161.11.1405. [DOI] [PubMed] [Google Scholar]
- 22.McGwin G, Jr, McNeal S, Owsley C, Girkin C, Epstein D, Lee PP. Statins and other cholesterol-lowering medications and the presence of glaucoma. Arch Ophthalmol. 2004;122:822–6. doi: 10.1001/archopht.122.6.822. [DOI] [PubMed] [Google Scholar]
- 23.Mach F. Statins as novel immunomodulators: from cell to potential clinical benefit. Thromb Haemost. 2003;90:607–10. doi: 10.1160/TH03-04-0249. [DOI] [PubMed] [Google Scholar]
- 24.Almog Y, Shefer A, Novack V, Maimon N, Barski L, Eizinger M, Friger M, Zeller L, Danon A. Prior statin therapy is associated with a decreased rate of severe sepsis. Circulation. 2004;110:880–5. doi: 10.1161/01.CIR.0000138932.17956.F1. [DOI] [PubMed] [Google Scholar]
- 25.del Real G, Jimenez-Baranda S, Mira E, Lacalle RA, Lucas P, Gomez-Mouton C, Alegret M, Pena JM, Rodriguez-Zapata M, Alvarez-Mon M, Martinez AC, Manes S. Statins inhibit HIV-1 infection by down-regulating Rho activity. J Exp Med. 2004;200:541–7. doi: 10.1084/jem.20040061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lefer DJ. Statins as potent antiinflammatory drugs. Circulation. 2002;106:2041–2. doi: 10.1161/01.cir.0000033635.42612.88. [DOI] [PubMed] [Google Scholar]
- 27.Almog Y. Statins inflammation, and sepsis: hypothesis. Chest. 2003;124:740–3. doi: 10.1378/chest.124.2.740. [DOI] [PubMed] [Google Scholar]
- 28.Nielsen GL, Sørensen HT, Zhou W, Steffensen FH, Olsen J. The Pharmacoepidemiologic Prescription Database of North Jutland – a valid tool in pharmacoepidemiological research. Int J Risk Safety Medicine. 1997;10:203–5. doi: 10.3233/JRS-1997-10309. [DOI] [PubMed] [Google Scholar]
- 29.Sørensen HT. Regional administrative health registries as a resource in clinical epidemiology. Int J Risk Safety Medicine. 1997;10:1–22. doi: 10.3233/JRS-1997-10101. [DOI] [PubMed] [Google Scholar]
- 30.Statistics Denmark, Statistics Denmark's Socio-economic Classification. 1. Copenhagen: 1997. [Google Scholar]
- 31.Statistics Denmark, Statistics Denmark's Classification of Occupational Skills. 1. Copenhagen: 1996. [Google Scholar]
- 32.Andersen TF, Madsen M, Jørgensen J, Mellemkjær L, Olsen JH. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46:263–8. [PubMed] [Google Scholar]
- 33.McCullagh P, McCullagh P, Nelder JA. Generalized Linear Models. 2. London: Chapman & Hall; 1996. [Google Scholar]
- 34.Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462–7. doi: 10.1001/jama.288.4.462. [DOI] [PubMed] [Google Scholar]
- 35.Larsen J, Andersen M, Kragstrup J, Gram LF. High persistence of statin use in a Danish population: compliance study 1993–98. Br J Clin Pharmacol. 2002;53:375–8. doi: 10.1046/j.1365-2125.2002.01563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lynch J, Kaplan G. Socioeconomic position. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 13–35. [Google Scholar]
- 37.Simpson CR, Hannaford PC, Williams D. Evidence for inequalities in the management of coronary heart disease in Scotland. Heart. 2005;91:630–4. doi: 10.1136/hrt.2004.036723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, MacFarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RG. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–30. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 39.Rasmussen JN, Gislason GH, Abildstrøm SZ, Rasmussen S, Gustafsson I, Buch P, Friberg J, Køber L, Torp-Pedersen C, Madsen M, Stender S. Statin use after acute myocardial infarction: a nationwide study in Denmark. Br J Clin Pharmacol. 2005;60:150–8. doi: 10.1111/j.1365-2125.2005.02408.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morrison C, Woodward M, Leslie W, Tunstall-Pedoe H. Effect of socioeconomic group on incidence of, management of, and survival after myocardial infarction and coronary death: analysis of community coronary event register. BMJ. 1997;314:541–6. doi: 10.1136/bmj.314.7080.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salomaa V, Miettinen H, Niemela M, Ketonen M, Mahonen M, Immonen-Raiha P, Lehto S, Vuorenmaa T, Koskinen S, Palomaki P, Mustaniemi H, Kaarsalo E, Arstila M, Torppa J, Kuulasmaa K, Puska P, Pyorala K, Tuomilehto J. Relation of socioeconomic position to the case fatality, prognosis and treatment of myocardial infarction events; the FINMONICA MI Register Study. J Epidemiol Community Health. 2001;55:475–82. doi: 10.1136/jech.55.7.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rao SV, Schulman KA, Curtis LH, Gersh BJ, Jollis JG. Socioeconomic status and outcome following acute myocardial infarction in elderly patients. Arch Intern Med. 2004;164:1128–33. doi: 10.1001/archinte.164.10.1128. [DOI] [PubMed] [Google Scholar]


