One in six couples have an unwanted delay in conception. Roughly half of these couples will conceive either spontaneously or with relatively simple advice or treatment. The other half remain subfertile and need more complex treatment, such as in vitro fertilisation and other assisted conception techniques; about half of these will have primary subfertility.
Most couples presenting with a fertility problem do not have absolute infertility (that is, no chance of conception), but rather relative subfertility with a reduced chance of conception because of one or more factors in either or both partners. Most couples with subfertility will conceive spontaneously or will be amenable to treatment, so that only 4% remain involuntarily childless. As each couple has a substantial chance of conceiving without treatment, relating the potential benefit of treatment to their chances of conceiving naturally is important to give a realistic appraisal of the added benefit offered by treatment options.
Chance of spontaneous conception
Conception is most likely to occur in the first month of trying (about a 30% conception rate). The chance then falls steadily to about 5% by the end of the first year. Cumulative conception rates are around 75% after six months, 90% after a year, and 95% at two years. Subfertility is defined as a failure to conceive after one year of unprotected regular sexual intercourse. It is usually investigated after a year, although for some couples it may be appropriate to start investigations sooner. The likelihood of spontaneous conception is affected by age, previous pregnancy, duration of subfertility, timing of intercourse during the natural cycle, extremes of body mass, and pathology present. A reasonably high spontaneous pregnancy rate still occurs even after the first year of trying.
Age
A strong association exists between subfertility and increasing female age. The reduction in fertility is greatest in women in their late 30s and early 40s. For women aged 35-39 years the chance of conceiving spontaneously is about half that of women aged 19-26 years. The natural cumulative conception rate in the 35-39 age group is around 60% at one year and 85% at two years.
Figure 1.
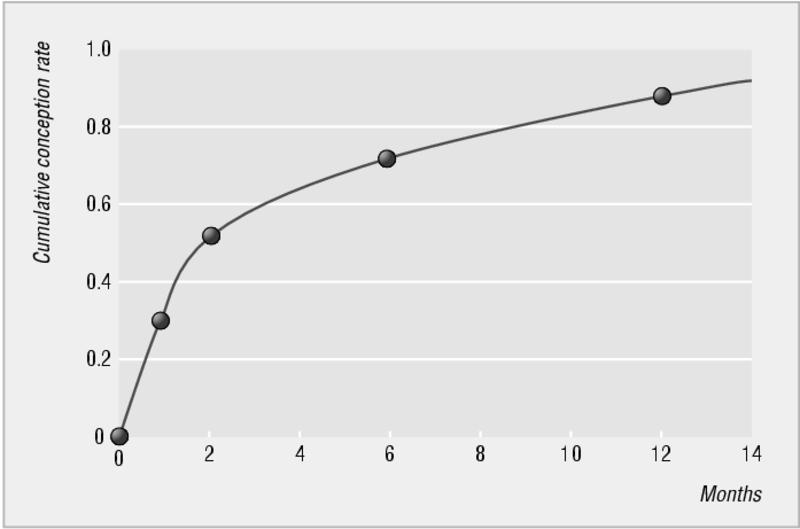
Cumulative conception rate in the first year of trying
This marked, age related decline in spontaneous conception is also mirrored in the outcome of assisted conception treatment. Recent evidence shows that male fertility also declines with age. Genetic defects in sperm and oocytes that are likely to contribute to impaired gamete function and embryonic development increase with age. The age related decline in female fecundity is caused by a steadily reducing pool of competent oocytes in the ovaries.
Figure 2.
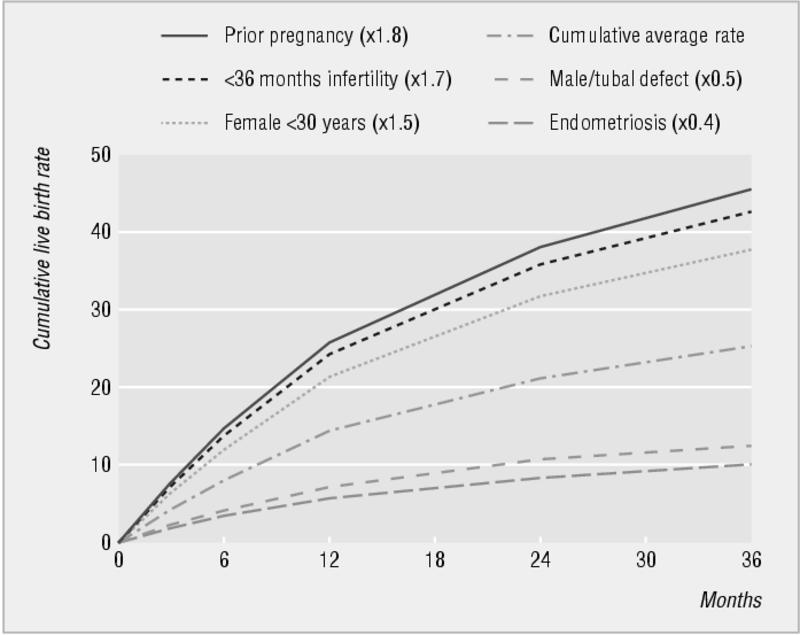
Cumulative live birth rate and prognostic influence of history and findings in couples not conceiving in the first year of trying. The presence of endometriosis, tubal factor, or suboptimal sperm quality may halve the likelihood of spontaneous conception. Data from Collins et al (see Further reading box)
Duration of subfertility
The longer a couple has to try to conceive, the smaller the chance of spontaneous conception. If the duration of subfertility is less than three years, a couple is 1.7 times more likely to conceive than couples who have been trying for longer. With unexplained subfertility of more than three years, the chances of conception occurring are about 1-3% each cycle.
Table 1.
Definitions of subfertility
| Subfertility is a failure to conceive after one year of unprotected regular sexual intercourse. Subfertility can be primary or secondary Primary subfertility—a delay for a couple who have had no previous pregnancies |
| Secondary subfertility—a delay for a couple who have conceived previously, although the pregancy may not have been successful (for example, miscarriage, ectopic pregnancy) |
Social changes mean that more couples are delaying the start of their family until women are in their late 30s and this brings a substantial reduction in their likelihood of conception
Previous pregnancy
When a delay in conception has no obvious cause the likelihood of conception is increased 1.8-fold if the couple has secondary rather than primary subfertility.
Timing of intercourse during ovulatory cycle
The chance of conception in an ovulatory cycle is related to the day in the cycle on which intercourse takes place. The window of opportunity lasts six days, ending on the day of ovulation. A study by Dunson et al (2002) showed that the probability of conception rose from six days before ovulation, peaked two days before ovulation, then fell markedly by the day of ovulation. This shows that sperm need to be deposited in the female genital tract before ovulation to maximise chances of conception. This is consistent with the progesterone induced changes in cervical mucus that occur immediately after ovulation and impede the penetration of sperm.
Weight
Pregnancy is less likely if the woman's body mass index (BMI) (weight (kg)/(height (m)2)) is > 30 or < 20. Women with a BMI > 30 need advice about modifying their diet and doing more exercise to lose weight and they should aim for a BMI < 30.
Women with a BMI < 20 should be advised to gain weight and reduce exercise if they are exercising excessively. Being considerably underweight is associated with an increased risk of miscarriage and intrauterine growth retardation.
Figure 3.

Being underweight and exercising excessively can increase the risk of anovulation, subfertility, and intrauterine growth retardation in pregnancy
Other factors affecting fertility
The chance of conception may be reduced by smoking, caffeine, and use of recreational drugs. The effect of some of these factors may be attributed in part to an association with other factors that affect fertility, such as an increased risk of sexually transmitted infection.
The effect of alcohol on fertility is not clear as the results of studies are conflicting. Some studies have found impaired fertility in women drinking more than five units of alcohol a week, whereas others have found that low to moderate alcohol consumption may be associated with a higher conception rate than in non-drinkers. Excess alcohol consumption in men can contribute to impotence and difficulties with ejaculation and may impair spermatogenesis.
Is subfertility getting more common?
Fecundity rates may be declining. However, it is difficult to separate changes in social behaviour and trends in delaying starting a family from other factors that might reduce the chance of conception, such as environmental factors. Several studies have reported a steady decline in mean sperm counts over the past few decades in Europe and the United States. They also reported that the incidence of testicular tumours, cryptorchidism, and hypospadias is increasing. Skakkebaek et al (1994) have suggested that a rise in environmental oestrogenic pollutants may be causing these changes.
Table 2.
Factors affecting fertility
| Increased chance of conception |
| • Woman aged under 30 years |
| • Previous pregnancy |
| • Less than three years trying to conceive |
| • Intercourse occurring during six days before ovulation, particularly two days before ovulation |
| • Woman's body mass index (BMI) 20-30 |
| • Both partners non-smokers |
| • Caffeine intake less than two cups of coffee daily |
| • No use of recreational drugs |
| Reduced chance of conception |
| • Women aged over 35 years |
| • No previous pregnancy |
| • More than three years trying to conceive |
| • Intercourse incorrectly timed, not occurring within six days before ovulation |
| • Woman's BMI < 20 or > 30 |
| • One or both partners smoke |
| • Caffeine intake more than two cups of coffee daily |
| • Regular use of recreational drugs |
Major causes of subfertility
The major causes of subfertility can be grouped broadly as ovulation disorders, male factors (which include disorders of spermatogenesis or obstruction), tubal damage, unexplained, and other causes, such as endometriosis and fibroids. The proportion of each type of subfertility varies in different studies and in different populations. Tubal infertility is more common in those with secondary subfertility and in populations with a higher prevalence of sexually acquired infections.
Obesity is also associated with an increased risk of miscarriage and obstetric complications such as hypertension, gestational diabetes, thromboembolism, and complicated delivery
It has been estimated that smokers are 3.4 times more likely to take more than a year to conceive than non-smokers, and in each cycle smokers have two thirds the chance of conceiving compared with non-smokers
The impact of subfertility
The impact of experiencing difficulty conceiving should not be underestimated for couples presenting with the problem. Many find it stressful to seek professional help for such an intimate problem and feel a sense of failure at having to do so. It is not uncommon for the problem to put a strain on the relationship and many couples experience a deterioration in their sexual relationship which exacerbates the problem. General practitioners can provide invaluable support to couples undergoing investigation and treatment and for those faced with intractable infertility.
Preconception advice
If a couple are considering starting a family they may approach their general practitioner for advice on conceiving. Areas for discussion should include things that may improve the chances of conception or increase the chance of a successful outcome to the pregnancy (by minimising the risk of abnormality or of pregnancy related complications for baby and mother).
Table 3.
Preconception advice
| Pre-existing medical problems* |
| • Stabilise medical conditions and ensure that medical control is optimal |
| • Check that drugs needed are safe for use in pregnancy and do not affect sperm function |
| • Where appropriate, refer woman to an obstetric physician for advice on implications of the condition in pregnancy |
| Weight |
| • Check BMI |
| • Advise on weight gain or loss where BMI is < 20 or > 30 |
| Smoking |
| • Advise both partners to stop smoking |
| Recreational drugs |
| • Advise both partners to stop using recreational drugs |
| Folic acid |
| • Women who are trying to conceive should take folic acid supplements (0.4 mg) daily to reduce the risk of neural tube defects. Women with a history of neural tube defect or epilepsy should take 5 mg daily |
| Virology screening |
| • Screen for rubella immunity and offer immunisation to those not immune |
| • Consider screening for HIV and hepatitis B and C in groups at risk |
| Prenatal diagnosis |
| • Tell older women about options for prenatal diagnosis |
| Timing of intercourse |
| • Check couple's understanding of ovulatory cycle and relate most fertile days to the length of woman's cycle |
| • Advise that intercourse occurs regularly. Two to three times a week should cover the most fertile time |
| Factors affecting fertility |
| • Discuss any factors in either partner's history that might warrant early referral for specialist infertility advice |
For example, hypertension, diabetes, epilepsy, thyroid disorder, cardiac problems, and drug history
Managing subfertility
A couple presenting with a delay in conception should be dealt with sympathetically and systematically according to a locally agreed protocol of investigations. Many of these investigations can be started by the couple's general practitioner and completed in secondary care. A cooperative approach allows prompt diagnosis of the problem, after which a realistic discussion can take place about the prognosis—the couple's chance of conceiving spontaneously and of conceiving with different treatment options. Formulating a plan of action with the couple can help ease some of the distress associated with the problem.
The role of general practitioners
General practitioners are often the first contact for couples concerned about their fertility. They can offer advice and support that can alleviate anxiety. Their role includes giving general preconception advice, taking a history, and starting appropriate tests. They should try to see both partners together, although this may be difficult if they are registered with different practices. However, the couple should be encouraged to approach the problem together and must understand that they will both need investigation. General practitioners can also ensure prompt and appropriate referral, and advise on local services available in secondary and tertiary care and local funding policies for investigation and treatment.
The ABC of subfertility is edited by Peter Braude, professor and head of department of women's health, Guy's, King's, and St Thomas's School of Medicine, London, and Alison Taylor, consultant in reproductive medicine and director of the Guy's and St Thomas's assisted conception unit. The series will be published as a book in the winter.
Competing interests: None declared.
Further reading and resources
- • Management of infertility in primary care: The initial investigation and management of the infertile couple. Evidence based clinical guidelines, 1998 www.rcog.org.uk/guidelines.asp?pageID = 108&GuidelineID = 25
- • Balen AH, Jacobs HS Infertility in practice. Churchill Livingstone:London, 1997
- • Bolumar F, Olsen J, Boldsen J. Smoking reduces fecundity: a European multicenter study on infertility and subfecundity. The European Study Group on Infertility and Subfecundity. Am J Epidemiol 1996;143: 578-7 [DOI] [PubMed] [Google Scholar]
- • Bolumar F, Olsen J, Rebagliato M, Saez-Lloret I, Bisanti L. Body mass index and delayed conception: a European multicenter study on infertility and subfecundity. Am J Epidemiol 2000;151: 1072-9 [DOI] [PubMed] [Google Scholar]
- • Collins JA, Burrows EA, Willan AR. The prognosis for live birth among untreated infertile couples. Fertil Steril 1995;64: 22-8 [PubMed] [Google Scholar]
- • Forman R, Gilmour-White S, Forman N. Drug-induced infertility and sexual dysfunction. Cambridge: Cambridge University Press, 1996
- • Skakkebaek NE, Giwercman A, de Kretser D. Pathogenesis and management of male fertility. Lancet 1994;343: 1473-9 [DOI] [PubMed] [Google Scholar]
- • Dunson DB, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod 2002;17: 1399-403 [DOI] [PubMed] [Google Scholar]


