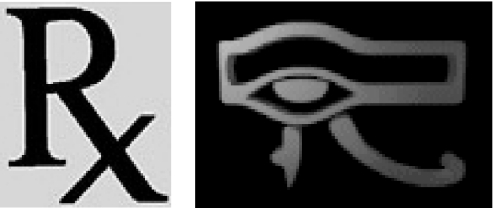
No-one knows the origin of the well-known prescription sign (Figure 1), but an attractive hypothesis is that it is derived from the utchat, or Eye of Horus, the symbol of good fortune and healing used by the ancient Egyptians and others (Figure 1) [1]. The sign of the utchat was worn by Egyptians to give them the strength of the sun and to maintain their good health, and it was inscribed in documents to ensure their success. When we inscribe its modern equivalent on a prescription we symbolically give the prescription the seal of success. But are our prescriptions always successful?
Figure 1.
The prescription sign (left) and the Eye of Horus (right).
Unsuccessful prescribing takes several forms: underprescribing, overprescribing, inappropriate prescribing, irrational prescribing, and prescribing errors.
Underprescribing is perhaps the most common of these, and we are again reminded of it in this issue of the Journal. In one of a series of four thorough reviews of various drug treatments in elderly patients, Mangoni and Jackson remind us that only a proportion of elderly patients with stable heart failure receive ACE inhibitors, despite good evidence of efficacy, and that those who are treated often receive inappropriately low doses [2]. In another of their articles they suggest that elderly patients should be given a statin regardless of their serum LDL cholesterol concentrations [3]; but we have previously published evidence that although prescribing of statins is increasing they are still being underprescribed [4].
‘Postcode prescribing’, as it is known in the UK, refers to variable prescribing in different parts of the country. Muller et al. in this issue of the Journal present evidence that suggests that there may be international variability of this kind [5]. They discovered marked discrepancies in a French hospital between the WHO-defined daily doses of antimicrobial drugs and the doses that were actually prescribed. This suggests that there are wide differences between prescribing habits in different countries. It would be interesting to know if such differences correlate with international differences in reporting adverse drug reactions [6].
Prescribing errors are also common. Headlines like ‘Hospital makes 135 drug errors a week’[7] (and of those 135 errors 34 were potentially serious [8]) have highlighted this, and we have previously published information about prescribing errors, including, for example, an epidemiological assessment of predictors of such errors in hospital [9]. Inappropriate prescribing and irrational prescribing also feature from time to time in the Journal[10].
The UK General Medical Council's document Tomorrow's Doctors[11] states that ‘graduate [doctor]s must know about and understand the principles of treatment, including … the effective and safe use of medicines as a basis for prescribing, harmful interactions … [and] be able to … write safe prescriptions for different types of drugs’. Of course they must. So must any prescriber.
But both in the UK [12] and elsewhere [13] medical students have said that they feel that not enough time is devoted to therapeutics teaching. Our first prescription should be to expose them and other prescribers to more.
Before prescribing
The word prescribe comes from a Latin word meaning to write in advance [of giving a medicine]. But the actual writing is a late event in the prescribing process. It must be preceded by a number of other processes.
First, the diagnosis must be accurately made and underpinned by an understanding of the basic pathophysiology. If a drug is not appropriately matched to the pathophysiology of the disease the wrong choice may be made. For example, one would not use digoxin to treat atrial fibrillation if thyrotoxicosis was the cause – a beta-blocker would be preferred; and although some forms of hypokalaemia respond to spironolactone, others do not [10].
Secondly, the prescriber must assess the balance of benefit to harm of a particular form of treatment (i.e. whether to treat at all).
Thirdly, practical matters related to the choice of drug must be addressed; these include picking the right drug from a range of alternatives (for example, an ACE inhibitor vs a beta-blocker, atenolol vs bisoprolol), designing the dosage regimen, considering the susceptibilities of a patient that might lead to adverse drug reactions, and remembering possible interactions with other drugs, including herbal formulations, and foods.
Lastly, the prescriber and patient need to discuss the proposed treatment and its potential effects, both beneficial and adverse, and the need for careful monitoring and dosage adjustment.
All of this demands a thorough understanding of the pathophysiology of the problem and the pharmacology of the drug, including its pharmaceutical, pharmacokinetic, and pharmacodynamic properties, and how those properties are translated into a therapeutic effect via a chain of biochemical and physiological events [14]. Add to all that a need to understand how to assess the evidence on which drug therapy is based, and a knowledge of, among other things, the effects of co-morbidity, adverse drug reactions, and cost-effectiveness of drug therapy, and it can be seen that the task is formidable for even the best-trained prescriber.
Like marriage, prescribing is not something to be undertaken ‘unadvisedly, lightly, or wantonly’.
Non-medical prescribing
Traditionally, prescribing has been limited to doctors and dentists, but in recent years this right has been extended to nurses, pharmacists, and in some circumstances other health-care workers, as both dependent and independent prescribers [15]. In the UK this has been part of a Governmental effort to give patients readier and more rapid access to medicines, and it has also led to the system known as Patient Group Directions. In this system a nurse or pharmacist, working to a plan described in a written statement formulated by the prescriber, can supply medicines to specific types of patients. This is not, strictly speaking, prescribing by the nurse or pharmacist, but the distinction is a subtle one and we do not yet know what the benefit to harm balance of this system is in different circumstances. However, some evidence comes from a paper by Lewington and Marshall in this issue of the Journal[16].
Since 2000 levonorgestrel-only emergency contraception has been available from UK pharmacists under a Patient Group Direction; the scheme allows pharmacists to supply such contraception to women over 16 years of age without a prescription, and although it is labelled as a form of supply, it can be regarded as a form of self-prescribing, since any young woman of the appropriate age and competence can obtain emergency contraception on demand. Furthermore, since 2001 levonorgestrel has been available to purchase from a pharmacist over the counter, although it is expensive. Lewington and Marshall found that emergency contraception was available much more quickly from pharmacies than from family planning clinics. They calculated that this could mean a 10% increase in the number of prevented pregnancies. However, they did not assess the potential harms of this system. For example, if more young women have unprotected intercourse because they know that emergency contraception is available, the total number of unwanted pregnancies could actually increase. They might also refrain from using barrier methods, exposing themselves to the risk of sexually transmitted diseases. Even appropriate prescribing can cause harm.
Guidelines and computerized prescribing
In recent years many types of guidelines have been formulated to help prescribers choose appropriate therapy for specific conditions. Some have been very successful, such as the British Thoracic Society's asthma guidelines [17] and the UK Resuscitation Council's guidelines on Advanced Life Support [18]. The strength of these guidelines has been that they have been issued with the imprimatur of the learned bodies that have formulated them, often on their own initiative. Other guidelines, such as those formulated by the National Institute for Health and Clinical Excellence (NICE) and the UK's National Service Framework, have been specifically commissioned.
However, a study published in this issue of the Journal has shown discrepant prescribing behaviour in the Netherlands in relation to guidelines on the use of statins; doctors adhered to the European guidelines, which promote the treatment of high-risk individuals whose 10-year risk of nonfatal or fatal coronary heart disease exceeds 20%, and not to the Dutch guidelines, which restricts treatment to men under 70 and women under 75, in whom treatment is not regarded as being cost-effective [19]. Although I would argue that the European guidelines are not liberal enough [4], this result suggests that Dutch doctors prefer to treat patients whom they think merit treatment, irrespective of cost. However, it implies that guidelines by themselves do not necessarily influence prescribing behaviour.
Indeed, there is direct evidence that guidelines are ineffective unless they are accompanied by either education or financial incentives. For example, of 1471 US patients with bipolar disorder, in whom a wide array of psychotropic agents had been used, only one-sixth to one-third were discharged taking medications recommended by expert guidelines [20]. And in a retrospective chart review of Canadian patients with acute stroke the use of antihypertensive medications during the first 7 days was not in accord with recommended expert guidelines, and there was considerable variation in practice [21].
In contrast, education about the use of guidelines on prescribing nutritional supplements in the UK significantly reduced total prescribing by 15% and reduced inappropriate prescribing from 77% to 59%[22] and in Australia the extent of use of antibiotics for upper respiratory tract infections prompted a study of an educational intervention based on prescriber feedback and management guidelines [23]. There was a reduction in antibiotic prescribing for upper respiratory tract infections and a more appropriate choice of antibiotic for tonsillitis or streptococcal pharyngitis. However, it was not clear whether this was the direct result of the educational intervention; other influences on prescribing (such as participation in vocational training for general practice, pressure from patients, and the perceived nonapplicability of general guidelines in individual patients) probably also had important effects.
It is too soon to evaluate the potential impact of computerized methods in prescribing. Computerized reminders to physicians may reduce inappropriate prescribing [24, 25], and cost savings may be possible [26]. However, while some studies have shown reduced prescribing errors [27] others have not [28], and studies have not been powered to detect differences in adverse events [27]. Furthermore, when computers are used to aid in decision making, the warnings that they give may be so numerous that prescribers become immune to them [29, 30]. In one study the computerized provision of patient profiles actually resulted in an increase in the number of prescriptions of two interacting drugs, although the durations of drug-drug interaction episodes were significantly shorter; the authors concluded that prevention of prescribing errors would require an educational or monitoring programme [31].
The main message from all this evidence is that to improve prescribing we should begin with education.
Teaching good prescribing
The results of a study of how well final-year medical students performed in a prescribing exercise suggested that the root cause of prescribing errors was lack of a knowledge base that integrated scientific knowledge with clinical know-how [32]. The clinical section of the British Pharmacological Society has developed a curriculum that lays down guidelines for teaching safe and effective prescribing [33]. It develops the premise that a thorough understanding of basic principles translates into good prescribing, and lists essential attributes for prescribers under three headings concerning the use of drugs: knowledge and understanding, skills, and attitudes. This curriculum should form the basis of teaching better prescribing at all UK medical schools, and elsewhere could be adapted to local needs.
Computerized learning may also have a role. A few years ago, interactive case-based and evidence-based prescribing modules, adapted for computerized learning, were introduced into Australian teaching programmes for senior medical students [34], funded by the National Prescribing Service, and following the tenets of the World Health Organization's ‘Guide to Good Prescribing’[35]. It includes the establishment of local student formularies as a teaching tool, a concept that could be extended to the training of junior hospital doctors and other prescribers. The uses of problem-based, computer-aided, and web-based teaching and learning in other countries have been discussed in detail elsewhere [36].
Teaching prescribing has become increasingly difficult, as drug therapy has become more complex and errors more common [37]. A proper curriculum, taught at the bedside or in the clinic by skilled practitioners (because good prescribing habits should be reinforced by practical example), and supplemented by computer-based material, properly funded, could help to mitigate this. Special study modules in prescribing would allow some students to expand their knowledge. Formal assessment of prescribing ability in final examinations would add incentive to the learning process. And national prescription forms for hospitals would encourage uniform standards; this may come about when electronic prescribing takes root.
Who should undertake such a programme? If you were to ask who should lead the way in teaching electrocardiography, the answer would be cardiologists, even though interpreting the electrocardiogram is a skill that all doctors should acquire and one that all doctors should be prepared to teach. Similarly, where prescribing is concerned, clinical pharmacologists should lead the way. However, despite calls for increased numbers [38, 39], there are still too few of them to undertake the whole burden of undergraduate teaching in practical drug therapy [40]. We should therefore be looking to recruit and train enthusiastic physicians, general practitioners, and specialist nurse prescribers to help. Clinical pharmacists and pharmacist prescribers, in partnership with clinicians, could also make a valuable contribution [11, 41, 42].
Conclusions
Prescribing is difficult. It requires a thorough knowledge and understanding of the pathophysiology of disease, the pharmacological properties of the relevant drugs, and the ways in which the two dovetail. No single intervention can be relied upon to improve prescribing, and a combination of interventions may be required [43]. However, education must be the kingpin. Here is my prescription for teaching undergraduate medical students and doctors and improving their prescribing:
Education, to be taken as often as possible (learning should be lifelong).
Special study modules, to be taken as required.
Proper assessment in the final examination, to be taken once or twice.
A national prescription form for hospitals, to be applied uniformly.
Guidelines and computerized prescribing systems, to be taken as indicated (their roles and proper implementation are currently unclear).
Similar regimens could be devised for other prescribers.
Several institutions are interested in prescribing and are active in different ways. In the UK these include the National Institute for Health and Clinical Excellence (NICE), the National Patient Safety Agency, and the UK Drug Utilization Research Group. However, they have other responsibilities and interests, and there is no overarching structure to focus their efforts on prescribing. A National Prescribing Council, like the National Prescribing Service in Australia, could achieve cohesion.
‘See one, do one, teach one’ runs the old adage. But if we do not increase the amount of time we spend teaching future prescribers, doctors, dentists, nurses, pharmacists, and others, we may soon be saying ‘See one, prescribe one, harm one’.
References
- 1.Aronson JK. X marks the spot. BMJ. 1999;318:1543. doi: 10.1136/bmj.318.7197.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mangoni AA, Jackson SHD. The implications of a growing evidence base for drug use in elderly patients. Part 2. ACE inhibitors and angiotensin receptor blockers in heart failure and high cardiovascular risk patients. Br J Clin Pharmacol. 2006;61:502–12. doi: 10.1111/j.1365-2125.2006.02610.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mangoni AA, Jackson SHD. The implications of a growing evidence base for drug use in elderly patients. Part 1. Statins for primary and secondary cardiovascular prevention. Br J Clin Pharmacol. 2006;61:494–501. doi: 10.1111/j.1365-2125.2006.02609.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aronson JK. Prescribing statins. Br J Clin Pharmacol. 2005;60:457–8. doi: 10.1111/j.1365-2125.2005.02521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muller A, Monnet DL, Talon D, Hénon T, Bertrand X. Discrepancies between prescribed daily doses and WHO defined daily doses of antibacterials at a University hospital. Br J Clin Pharmacol. 2006;61:585–91. doi: 10.1111/j.1365-2125.2006.02605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferner RE, Aronson JK. National differences in publishing papers on adverse drug reactions. Br J Clin Pharmacol. 2005;59:108–11. doi: 10.1111/j.1365-2125.2005.02267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anonymous. Hospital makes 135 drug errors a week. The Guardian. 2002. December 5.
- 8.Dean B, Schachter M, Vincent C, Barber N. Prescribing errors in hospital inpatients: their incidence and clinical significance. Qual Saf Health Care. 2002;11:340–4. doi: 10.1136/qhc.11.4.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fijn R, Van den Bemt PM, Chow M, De Blaey CJ, De Jong-Van den Berg LT, Brouwers JR. Hospital prescribing errors: epidemiological assessment of predictors. Br J Clin Pharmacol. 2002;53:326–31. doi: 10.1046/j.0306-5251.2001.bjcp1558.doc.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aronson JK. Rational prescribing, appropriate prescribing. Br J Clin Pharmacol. 2004;57:229–30. doi: 10.1111/j.1365-2125.2004.02090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.General Medical Council. Tomorrow's Doctors. Recommendations on Undergraduate Medical Education. London: General Medical Council; 2002. [30 March, 2006]. http://www.gmc-uk.org/education/undergraduate/tomdoc.pdf. [Google Scholar]
- 12.Ellis A. Prescribing rights: are medical students properly prepared for them? BMJ. 2002;324:1591. [Google Scholar]
- 13.Wells JL, Borrie MJ, Crilly R, Brymer CD, Hurwitz JS. A novel clinical pharmacy experience for third-year medical students. Can J Clin Pharmacol. 2002;9:7–16. [PubMed] [Google Scholar]
- 14.Grahame-Smith DG, Aronson JK. The Oxford Textbook of Clinical Pharmacology and Drug Therapy. 3. Oxford: Oxford University Press; 2002. The four processes of drug therapy; pp. 3–6. [Google Scholar]
- 15.Leathard HL. Understanding medicines: extending pharmacology education for dependent and independent prescribing (Part II) Nurse Educ Today. 2001;21:272–7. doi: 10.1054/nedt.2001.0554. [DOI] [PubMed] [Google Scholar]
- 16.Lewington G, Marshall K. Access to emergency hormonal contraception from community pharmacies and family planning clinics. Br J Clin Pharmacol. 2006;61:605–8. doi: 10.1111/j.1365-2125.2006.02623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.British Thoracic Society, Scottish Intercollegiate Guidelines Network. [30 March, 2006]; British Guideline on the Management of Asthma. A National Clinical Guideline. Revised Edition November 2005. http://www.sign.ac.uk/pdf/sign63s1.pdf.
- 18.Resuscitation Council (UK) Trading Ltd. [30 March, 2006]; Resuscitation Guidelines 2005. http://www.resus.org.uk/pages/guide.htm.
- 19.Mantel-Teeuwisse AK, Klungel OH, Hofman A, Verschuren WMM, Trienekens PH, Porsius AJ, Stricker BHCh, de Boer A. Prescribing behaviour according to Dutch and European guidelines on the management of hypercholesterolaemia (1992–1999) Br J Clin Pharmacol. 2006;61:596–600. doi: 10.1111/j.1365-2125.2006.02634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lim PZ, Tunis SL, Edell WS, Jensik SE, Tohen M. Medication prescribing patterns for patients with bipolar I disorder in hospital settings: adherence to published practice guidelines. Bipolar Disord. 2001;3:165–73. [PubMed] [Google Scholar]
- 21.Kanji S, Corman C, Douen AG. Blood pressure management in acute stroke: comparison of current guidelines with prescribing patterns. Can J Neurol Sci. 2002;29:125–31. [PubMed] [Google Scholar]
- 22.Gall MJ, Harmer JE, Wanstall HJ. Prescribing of oral nutritional supplements in primary care: can guidelines supported by education improve prescribing practice? Clin Nutr. 2001;20:511–15. doi: 10.1054/clnu.2001.0479. [DOI] [PubMed] [Google Scholar]
- 23.Zwar N, Henderson J, Britt H, McGeechan K, Yeo G. Influencing antibiotic prescribing by prescriber feedback and management guidelines: a 5-year follow-up. Fam Pract. 2002;19:12–17. doi: 10.1093/fampra/19.1.12. [DOI] [PubMed] [Google Scholar]
- 24.Tamblyn R, Huang A, Perreault R, Jacques A, Roy D, Hanley J, McLeod P, Laprise R. The medical office of the 21st century (MOXXI): effectiveness of computerized decision-making support in reducing inappropriate prescribing in primary care. CMAJ. 2003;169:549–56. [PMC free article] [PubMed] [Google Scholar]
- 25.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices. Arch Intern Med. 2000;160:2741–7. doi: 10.1001/archinte.160.18.2741. [DOI] [PubMed] [Google Scholar]
- 26.Kawahara NE, Jordan FM. Influencing prescribing behavior by adapting computerized order-entry pathways. Am J Hosp Pharm. 1989;46:1798–801. [PubMed] [Google Scholar]
- 27.Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review. Arch Intern Med. 2003;163:1409–16. doi: 10.1001/archinte.163.12.1409. [DOI] [PubMed] [Google Scholar]
- 28.Gandhi TK, Weingart SN, Seger AC, Borus J, Burdick E, Poon EG, Leape LL, Bates DW. Outpatient prescribing errors and the impact of computerized prescribing. J Gen Intern Med. 2005;20:837–41. doi: 10.1111/j.1525-1497.2005.0194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ferner RE. Computer aided prescribing leaves holes in the safety net. BMJ. 2004;328:1172–3. doi: 10.1136/bmj.328.7449.1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weingart SN, Toth M, Sands DZ, Aronson M, Davis RB, Phillips RS. Physicians’ decisions to override computerized drug alerts in primary care. Arch Intern Med. 2003;163:2625–31. doi: 10.1001/archinte.163.21.2625. [DOI] [PubMed] [Google Scholar]
- 31.Koepsell TD, Gurtel AL, Diehr PH, Temkin NR, Helfand KH, Gleser MA, Tompkins RK. The Seattle evaluation of computerized drug profiles: effects on prescribing practices and resource use. Am J Public Health. 1983;73:850–5. doi: 10.2105/ajph.73.8.850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boreham NC, Mawer GE, Foster RW. Medical students’ errors in pharmacotherapeutics. Med Educ. 2000;34:188–93. doi: 10.1046/j.1365-2923.2000.00510.x. [DOI] [PubMed] [Google Scholar]
- 33.Maxwell S, Walley T. Teaching safe and effective prescribing in UK medical schools: a core curriculum for tomorrow's doctors. Br J Clin Pharmacol. 2003;55:496–503. doi: 10.1046/j.1365-2125.2003.01878.x. Downloadable from http://www.bps.ac.uk/coreCPTCurricula.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith AJ, Tasioulas T. Education on prescribing can be improved. BMJ. 2002;325:776. doi: 10.1136/bmj.325.7367.776/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Vries TPGM, Henning RH, Hogerzeil HV, Fresle DA. Guide to Good Prescribing. A Practical Manual. Geneva: World Health Organization Action Programme on Essential Drugs; 1994. [30 March, 2006]. WHO/DAP/94.11. http://whqlibdoc.who.int/hq/1994/WHO_DAP_94.11.pdf. [Google Scholar]
- 36.Herzig S, Jakobs KH. Michel MC, editor. Novel teaching techniques in pharmacology. Naunyn Schmiedeberg's Arch Pharmacol. 2002;366(1) doi: 10.1007/s00210-002-0568-4. [DOI] [PubMed] [Google Scholar]
- 37.Audit Commission. London: Audit Commission; 2001. [30 March, 2006]. A Spoonful of Sugar–[Improving (subsequently deleted)] Medicines Management in Hospitals. http://www.audit-commission.gov.uk/reports/NATIONAL-REPORT.asp?CategoryID=&ProdID=E83C8921-6CEA-4b2c-83E7-F80954A80F85. [Google Scholar]
- 38.Royal College of Physicians of London. [30 March, 2006]; Clinical Pharmacology and Therapeutics in a Changing World. Report of a Working Party, May 1999. http://www.rcplondon.ac.uk/pubs/brochures/pub_print_clinph.htm. [PMC free article] [PubMed]
- 39.US Food and Drug Administration. [30 March, 2006]; Innovation or Stagnation. Challenge and Opportunity on the Critical Path to New Medical Products. US Department of Health and Human Services, March 2004. http://www.fda.gov/oc/initiatives/criticalpath/whitepaper.html.
- 40.Maxwell SR, Webb DJ. Clinical pharmacology – too young to die? Lancet. 2006;367:799–800. doi: 10.1016/S0140-6736(06)68316-5. [DOI] [PubMed] [Google Scholar]
- 41.Scobie SD, Lawson M, Cavell G, Taylor K, Jackson SH, Roberts TE. Meeting the challenge of prescribing and administering medicines safely: structured teaching and assessment for final year medical students. Med Educ. 2003;37:434–7. doi: 10.1046/j.1365-2923.2003.01492.x. [DOI] [PubMed] [Google Scholar]
- 42.National Prescribing Centre. [30 March, 2006]; http://www.npc.co.uk.
- 43.Technology Evaluation Center Staff and Blue Cross and Blue Shield Association Medical Advisory Panel. Special report: the efficacy of interventions to change physician prescribing behavior. Technol Eval Cent Asses Program Exec Summ. 2004;19:1–2. [PubMed] [Google Scholar]