Abstract
Alcoholics with depressive symptoms score ≥ 10 on the Beck Depression Inventory (A. T. Beck, C. H. Ward, M. Mendelson, J. Mock, & J. Erbaugh, 1961) received 8 individual sessions of cognitive–behavioral treatment for depression (CBT-D, n = 19) or a relaxation training control (RTC; n =16) plus standard alcohol treatment. CBT-D patients had greater reductions in somatic depressive symptoms and depressed and anxious mood than RTC patients during treatment. Patients receiving CBT-D had a greater percentage of days abstinent but not greater overall abstinence or fewer drinks per day during the first 3-month follow-up. However, between the 3- and 6-month follow-ups, CBT-D patients had significantly better alcohol use outcomes on total abstinence (47% vs. 13%), percent days abstinent (90.5% vs. 68.3%), and drinks per day (0.46 vs. 5.71). Theoretical and clinical implications of using CBT-D in alcohol treatment are discussed.
The co-occurrence of alcoholism and depression is well documented (e.g., Regier et al., 1990). In the general population, results from the Epidemiological Catchment Area (ECA) survey reveal the occurrence of the combined disorders to be almost two times higher (odds ratio [OR ] = 1.9) than would be expected by chance associations alone (Helzer & Pryzbeck, 1988; Regier et al., 1990). Among alcoholics from patient samples, rates of comorbidity are even greater. In an alcohol treatment-seeking sample, 22.6% of those surveyed had a lifetime history of major depressive disorder (MDD), whereas 35.9% of patients with both alcohol and drug use disorders had lifetime MDD (Ross, Glaser, & Germanson, 1988). Rates of comorbidity based on depressive symptom rating scales are generally higher than those from structured diagnostic criteria (Hesselbrock, Hesselbrock, Tennen, Meyer, & Workman, 1983; Keeler, Taylor, & Miller, 1979), with clinically significant levels of depressive symptoms being reported in as many as 65–85% of patients entering alcohol treatment (e.g., Dorus, Kennedy, Gibbons, & Ravi, 1987). Taken together, data from both community and clinical samples reveal a strong association between depression and alcoholism.
Comorbid depression has been associated with poorer prognosis after alcoholism treatment. This impact of depression on patient outcomes in alcoholism treatment extends to depressive disorders, as well as to subsyndromal depressive symptoms. When assessed at pretreatment, patients with lifetime MDD (compared with those without MDD) have evidenced elevated drinking rates and alcohol-related problem behaviors (Hesselbrock, 1991; Rounsaville, Dolinsky, Babor, & Meyer, 1987), more frequent relapses and subsequent addiction treatment (O'Sullivan et al., 1988), more medical problems (Rounsaville et al., 1987), and elevated rates of depressive symptoms and disorders at extended follow-up (Hesselbrock, 1991; O'Sullivan et al., 1988; Rounsaville et al., 1987). Pretreatment depressive symptoms have been associated with premature dropout from alcohol treatment (Baekland, Lundwall, & Shanahan, 1973), and posttreatment depressive symptoms have been associated with greater risk of suicide (Berglund, 1984). Cross-sectionally, relapse has been associated with greater depressive symptoms after alcohol treatment (Hatsukami & Pickens, 1982).
Depressed mood may also be an important trigger of alcoholic relapse. Situations involving negative mood states are among the most frequently cited precipitants of relapse across several types of addictive substances (Marlatt & Gordon, 1985; Shiffman, 1982). Mariatt and Gordon (Mariatt & Gordon, 1985) identified negative mood state situations as the most frequent precipitant of relapse in their sample of alcoholics, accounting for 38% of all relapse episodes. In a similar report (Pickens, Hatsukami, Spicer, & Svikis, 1985), depressed mood was cited as the most important reason for relapse by 22% of alcoholics who relapsed after residential treatment for substance abuse. Alcoholics with lifetime MDD report drinking to relieve depressive symptoms more frequently than those without lifetime MDD (Hesselbrock, Hesselbrock, & Workman-Daniels, 1986), suggesting an increased vulnerability to situations involving negative affect.
Evidence from a number of sources suggests that depression is associated with poorer outcome in alcohol treatment. It is surprising that only two studies have evaluated the use of cognitive-behavioral treatment of depression (CBT-D) for alcoholics, particularly given the demonstrated efficacy of CBT-D for unipolar depression (Brown & Lewinsohn, 1984a; Hollon & Najavits, 1988; Jarrett & Rush, 1994; U.S. Department of Health and Human Services, 1993). The first study (Turner & Wehl, 1984) found that adding CBT-D for alcoholics with significant depressive symptoms was more effective on mood and alcohol use measures than standard treatment alone within an individual but not a group treatment modality. However, interpretation of these findings is limited because of the lack of control for contact time in the standard treatment condition, leaving open the possibility that treatment effects were due to the added therapist contact in the individual condition. The second study (Monti et al., 1990) found that mood management training was less effective than communications skills training on alcohol use outcomes. However, in this study patients were not selected on the basis of depression criteria, depressive symptoms were not assessed, and two of the three components of their mood management training (relaxation training and “changing personal behavior using stimulus control”) have little or no demonstrated efficacy in the treatment of depression. Thus neither study provided an adequate test of the efficacy of CBT-D with alcoholics. An integrated cognitive–behavioral intervention that targets the unique needs of alcoholics with comorbid depressive symptomatology holds the promise of improved treatment outcomes (Lehman, Myers, & Corty, 1989).
The present study evaluated the comparative efficacy of adding CBT-D versus a relaxation training control (RTC) to standard partial hospital alcohol treatment for alcoholics with elevated levels of depressive symptoms. The cognitive-behavioral treatment applied in this study was an adaptation of the Coping With Depression Course, which has been shown to be effective in the treatment of unipolar depression (Brown & Lewinsohn, 1984a; Lewinsohn, Antonuccio, Breckenridge, & Teri, 1984). We expected that the addition of CBT-D to standard alcohol treatment would result in decreased levels of depressive symptoms and in reduced quantity and frequency of alcohol use over a 6-month follow-up, relative to the addition of the relaxation control condition. We further expected that the predicted reductions in drinking in the CBT-D group would be mediated by the decrease in depressive symptoms, which would, in turn, be mediated by decreases in dysfunctional beliefs and increases in pleasant activities. Finally, we predicted that reductions in drinking among CBT-D patients would also be mediated by increases in drinking self-efficacy.
Method
Participants
The participants were 35 men and women recruited from the Alcohol and Drug Treatment Services (ADTS) day partial hospital program at Butler Hospital, a private, university-affiliated psychiatric hospital located in Providence, Rhode Island. Patients were included in the study if they met Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev.; DSM–III–R; American Psychiatric Association, 1987) criteria for alcohol dependence as determined by the patient version of the Structured Clinical Interview for DSM–III–R (SCID-P; Spitzer, Williams, Gibbon, & First, 1989) and had a Beck Depression Inventory (BD1; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) total score of 10 or greater. Participants are referred to throughout this article as “alcoholics with elevated depressive symptoms” (Kendall & Flannery-Schroeder, 1995), rather than as “depressed alcoholics,” as the latter term would incorrectly suggest that participants had met diagnostic criteria for a depressive disorder. Patient exclusion criteria were active suicidal or homicidal risk, acute psychosis, or current opiate abuse or dependence. Information about prospective participants was initially screened through review of the medical record as to the diagnostic inclusion–exclusion criteria. Thereafter, a total of 113 patients were considered for participation in the study. Of those, 17 were excluded because of psychiatric symptomatology (i.e., psychotic symptoms or active suicidal–homicidal risk), 19 refused participation in the study, 3 had BDI scores < 10, and 39 were ineligible for administrative reasons (e.g., non-English speaking, not recruited during washout period, attending psychiatrist did not allow participation, administratively discharged from partial hospital treatment).
Women constituted 29% of the sample; the mean age of participants was 38.0 years (SD = 7.2; range = 27–58). Participants reported a mean education of 13.2 years (SD = 2.5); 31.5% were married or cohabiting, and 100% were Caucasian. Ten participants (28.6%) reported use of antidepressant medication at pretreatment. Participants' mean score on the Alcohol Dependence Scale (ADS; Skinner & Allen, 1982) was 18.1 (SD = 6.5), and their mean number of previous alcohol treatments was 1.7 (SD = 2.4). In the time-line follow-back interview (TLFB; Sobell et al., 1980), participants reported that during the 6 months before treatment, they consumed a mean of 8.6 (SD = 6.6) standard drinks per possible drinking day (i.e., days not in jail or residential treatment), were abstinent 35.8% (SD = 29.8%) of possible drinking days, and drank heavily (more than six standard drinks per day for men and more than five standard drinks per day for women) on 50.1% (SD = 32.6%) of possible drinking days.
Measures
An assessment battery was administered pretreatment within the first 2 to 3 days after admission. Patients were not assessed until withdrawal symptom remission had occurred as determined by chart review and discussion with their attending psychiatrist Pretreatment assessments began, on average, 3.7 ± 2.9 days after the participant's last drink. Follow-up interviews were conducted at posttreatment and at 1, 3, and 6 months after partial hospital discharge. Four types of measures were included in the study: (a) dependent measures of depressive symptoms and depressed and anxious mood, (b) dependent measures of alcohol use, (c) measures intended to provide descriptive and diagnostic information about the participants, and (d) cognitive–behavioral process measures.
Dependent measures of depressive symptoms and depressed and anxious mood
We used the BDI (Beck et al., 1961) and the interviewer-based Modified Hamilton Rating Scale for Depression (HAM-D; Miller, Norman, & Bishop, 1985) to assess depressive symptoms. HAM-D interviewers were aware of treatment condition assignment. The Depression and Anxiety subscales of the Profile of Mood States (POMS; McNair, Lorr, & Droppleman, 1971) were used to assess weekly changes in mood.
Dependent measures of alcohol use
We used the TLFB interview (Sobell et al., 1980) to assess drinking frequency and quantity at baseline and during the follow-up intervals. The reliability and validity of the TLFB interview has been established (Babor, Stephans, & Marlatt, 1987; Sobell, Maisto, Sobell, & Cooper, 1979; Sobell et al., 1980). The TLFB was administered at baseline for the 180 days before admission and at each follow-up interval for the period since its last administration. TLFB data include the number of days abstinent from alcohol, amount consumed during each drinking occasion, and the number of days in jail or in residential treatment. Drinking data were converted to standard-sized drinks (i.e., .48 oz., or 13.6 g of 100% ethanol). The principal dependent measures were percent days abstinent as a measure of drinking frequency and mean number of (standard) drinks per possible drinking day as a measure of drinking intensity (i.e., both variables were calculated only for days not in the hospital, residential treatment, or jail). One family member or close friend (significant other; SO) was interviewed at 3 months and 6 months posttreatment to provide information on the patient's drinking behavior, including quantity and frequency.
Diagnostic and descriptive measures
Participants provided demo-graphic and background information such as age, gender, number of years of education, and number of previous alcohol treatments. We determined current use of antidepressant medication from review of each participant's medical record. The lifetime and current prevalence of DSM–III–R alcohol use and affective disorders and other Axis I syndromes were determined with the SCID-P (Spitzer et al., 1989). We assessed the severity of alcohol dependence using the ADS (Skinner & Allen, 1982).
Cognitive–behavioral process measures
We used the Situational Confidence Questionnaire (SCQ-39; Annis, 1988) to assess drinking self-efficacy. Negative thoughts and dysfunctional attitudes were determined with the Dysfunctional Attitude Scale (DAS; Weissman & Beck, 1978). We used the Pleasant Events Schedule—Mood Related (PES–MR; Lewinsohn & Graf, 1973) to assess the frequency of occurrence and subjective enjoyability of pleasurable events; the cross-product score of frequency and enjoyability is used in all analyses.
Treatments
Elements common to both treatments
After admission to the ADTS partial hospital program, potential participants were informed about the study and their consent was obtained. Eligible patients who consented to participate were then assigned to receive either CBT-D or RTC in addition to the standard treatment program in five sequential, nonoverlapping cohorts, with a washout period between cohorts, thus allowing only one condition to be conducted at a given time in the partial hospital program. The treatment was administered in the following order: CBT-D (n = 6), RTC (n = 5), CBT-D (n = 5), RTC (n = 11), CBT-D (n = 8). This procedure was deemed preferable to random assignment because of concerns about the possibility of treatment contamination should participants compare treatment manuals and procedures if the two conditions were conducted concurrently. Both experimental and control conditions were administered in eight 45-min individual sessions throughout the course of participants' partial hospital treatment. Patient manuals were developed for both conditions and used liberal use of graphics and limited text presentations to enhance readability. Detailed therapist manuals were used to ensure standardized delivery of content in both conditions. Treatment sessions did not interfere with participants' standard care as defined later, but rather were scheduled during patients' free times or during times specifically allotted for individual appointments. Although participation in the study required extra patient effort, both conditions were highly credible and rated favorably by participants.
The two therapists who delivered the treatment protocols were post-doctoral fellows in clinical psychology, whose primary therapeutic orientation was in behavior therapy and who had prior experience in addictive behavior treatment. Therapists were crossed with treatment assignment, so that each therapist provided treatment to an equal number of patients in each treatment condition. Richard A. Brown trained the two therapists and conducted weekly group supervision sessions throughout the study to ensure standardization of protocol delivery.
Standard treatment
All patients participated in the standard partial hospital alcohol treatment program, which served as the background treatment for this study. Inpatient detoxification, when necessary, was provided in an adjacent alcohol and drug inpatient unit. The standard partial hospital treatment is an abstinence-oriented, group treatment-based program that provides treatment daily from 9:00 a.m. to 3:30 p.m., is theoretically grounded in a cognitive social learning model, and includes strong encouragement for participation in 12-step programs. The program has been described in greater detail elsewhere (McCrady, Dean, Dubreuil, & Swanson, 1985).
CBT-D
The Coping With Depression course (Brown & Lewinsohn, 1984a, 1984b), modified for use with alcohol-dependent patients, served as the basis for the CBT-D in the experimental condition. The Coping With Depression course is a multicomponent treatment for depression, incorporating training in several depression-relevant skills including daily mood monitoring, pleasant activities, constructive thinking, and social skills and assertiveness. Brown and Lewinsohn (1984a) demonstrated mat this intervention was superior to a wait-list control; that there were no differences between individual, group, and minimal phone contact modalities; and that treatment gains were maintained at 1- and 6-month follow-ups. Modified versions of the Coping With Depression course have also been successfully applied for depression treatment of adolescents (Lewinsohn, Clarke, Hops, & Andrews, 1990) and Type II diabetics and older adults (Glasgow et al., 1992).
The application of the depression coping skills training to alcoholics involved daily homework assignments applying elements of the skills being taught, and included the following cognitive-behavioral components, which were presented as viable alternatives to drinking that should help combat feelings of depression and replace the perceived void following the loss of drinking as a reinforcing activity.
Treatment rationale: The reciprocal relationship among behavior, thoughts, and mood was explained as an organizing model for the proposed treatment, and examples of how changes in behavior and thoughts can affect mood were provided. The relationship between depressive symptoms and alcohol use was discussed, and the importance of learning coping skills to control depressive symptoms that might otherwise serve as triggers to drink was emphasized.
Daily mood rating: Participants monitored their mood daily on a 9-point Likert-type scale throughout treatment to gain skills in identifying daily mood states and the factors that influence them and to determine the effect of mood-specific coping skills during the intervention.
Increasing pleasant activities: The PES-MR (Lewinsohn & Graf, 1973) was used to help participants create a personalized pleasant activity schedule, with which they monitored pleasant activities daily to establish their baseline rate. Participants then contracted for achievable, systematic increases in pleasant activities to improve their mood and to prevent the onset of depressive symptoms throughout their recovery.
Increasing positive–decreasing negative thoughts: Participants were instructed to monitor their thoughts daily and to characterize thoughts as either positive or negative. Cognitive self-management techniques for reducing negative thoughts such as thought stopping, worrying time, and the blow-up technique and for increasing positive thoughts by priming and using cues, time projection, and self-talk procedures were taught.
ABC technique: This procedure is based on the rational-emotive therapy principles of Albert Ellis (Ellis & Harper, 1961) while incorporating instruction in the identification of cognitive distortions as identified by Beck (Beck, Rush, Shaw, & Emery, 1978) and popularized by Burns (1980). Participants were taught techniques for identifying and disputing distorted, depressive thoughts, and this skill was reinforced through daily practice and homework assignments.
Social skills–assertiveness: These procedures taught participants skills in improving the quality of social interactions and responding more assertively in various situations, including situations involving social pressure to use alcohol. Participants listed situations in which they typically responded unassertively or aggressively and, subsequently, learned more assertive ways to respond in these situations through modeling, role-playing, and homework exercises.
Maintaining gains: To maintain gains in reducing depressed mood after treatment termination, participants were encouraged to monitor their mood periodically, to identify the skills they found to be most effective for them, and to actively use those skills to manage and prevent depressed mood without drinking during the alcohol recovery process.
RTC
We reasoned that a relaxation control condition equated for contact time would provide a stringent test of the incremental efficacy of the CBT-D treatment. In a previous study, adjunctive relaxation training with alcoholics had not been found to have a significant impact on drinking outcome (cf. Klajner, Hartman, & Sobell, 1984). The RTC condition in the present study included components that were presented as viable alternatives to drinking and as coping skills to help combat feelings of stress and anxiety. During each session, participants practiced the specific relaxation skill (or skills) being taught.
Treatment rationale: The relationship between stress and alcohol use was discussed, and the importance of learning coping skills to control tension and anxiety was emphasized.
Daily tension rating: Participants monitored daily tension levels on a 9-point Likert-type scale throughout treatment to gain skills in identifying tense and relaxed states.
The Relaxation Response: This procedure, developed by Benson (1975), taught participants meditative and deep breathing techniques and was offered as a simple and “portable” method of relaxation.
Progressive Muscle Relaxation: This procedure, developed by Jacobsen (1929), provided instruction to participants in alternately tensing and relaxing selected muscle groups to isolate and differentiate feelings of tension versus relaxation, and in so doing, learn to produce a state of deep muscular relaxation.
Guided imagery: Participants were taught to incorporate several active imagery procedures as a means of enhancing the relaxation effects achieved, either alone or in combination with the other procedures.
Results
At pretreatment, t tests and chi-square tests showed that the two groups did not differ on gender, age, number of years of education, use of antidepressant medication, number of previous treatments for alcohol abuse, severity of alcohol dependence on the ADS, quantity and frequency of alcohol use, and measures of depressive symptoms and mood. Likewise, the two groups did not differ on baseline measures of dysfunctional attitudes, pleasant events, and self-efficacy. Ten participants in the CBT-D condition and 9 participants in the RTC condition met DSM–III–R criteria (per SCID-P) for past history of major depression when the organic rule-out (for alcohol involvement) was not applied. However, only 1 participant (in RTC condition) met criterion for past major depressive episode when the organic rule-out was applied (i.e., during a period while not drinking).
Of the 35 participants who completed baseline measures, one participant (in RTC condition) did not complete the posttreatment assessment but was included in all other analyses. Thirty-two participants (91%) completed all follow-assessments (1-, 3-. and 6-month); we were unable to locate 2 participants in the CBT-D condition and 1 participant in the RTC condition. Thus, our follow-up rate at 6 months was 91.4% (32 of 35). Chi-square analyses showed no significant differences between groups in attrition at either interval.
Participants were in partial hospital treatment for an average of 21.2 calendar days (SD = 4.5), and the mean number of days between pre- and posttreatment assessments was 18.9 (SD = 4.4). There were nonsignificant differences between treatment conditions on length of partial hospital treatment and length of time between assessments (ps > .10). Participants attended an average of 7.43 (SD = 1.0) treatment sessions, and there were no significant differences between CBT-D and RTC conditions (p > . 10). Twenty-one patients were prescribed antabuse on discharge, with no significant differences between treatment conditions (p > .10).
Validity of Self-Reported Alcohol Use
Self-report drinking data at follow-up were compared with the reports from the one SO who provided information as to each participant's drinking. Because of attrition and inability to contact several SOs at each follow-up point, 59 pairs of drinking reports were compared. The agreement between participant and SO reports was 80% (47 of 59) for the participant drinking at all during follow-up. Seven SOs claimed that participants were abstinent when the participants claimed they drank, whereas five SOs claimed that participants drank when the participants reported abstinence. If verification is performed only to confirm participants' self-reported abstinence (i.e., cases where participant reported drinking and SO reported abstinence are not included), agreement between SO and participant reports improves to 92% (54 of 59). The agreement between participant and SO reports was 68% (34 of 50) for the classification of the participants' drinking during the 6 months posttreatment as heavy drinking; that is, more than six drinks for men and more than five drinks for women. (An additional nine SOs were unable to report on the extent of patients' drinking, thus the agreement for this heavy drinking analysis was based on 50 pairs of drinking reports.) Tfen SOs claimed that the participant was not drinking heavily when the participant reported he or she was, whereas 6 SOs claimed the participant was drinking heavily when the participant reported they were not. If verification is performed on the participant's claim of not drinking heavily, agreement between SO and participant reports improves to 88% (44 of 50). SO reports significantly correlated with participant reports for number of drinking days during the 6 months post-treatment, r = .43, p < .03. When data from SOs who said they were not very confident about their knowledge of the participant's drinking were eliminated from these analyses (four people), the correlation improved, r = .56, p < .005. The participant reported more drinking days in 12 cases, the SO reported more drinking days in 19 cases, and the reports agreed in 21 cases. Overall, these data provide strong support for the validity of patients' self-reported alcohol use over the follow-up period.
Cohort or Seasonal Effects
Given that treatment was administered in five sequential, non-overlapping cohorts, we examined the possibility of a cohort effect by comparing the three CBT-D cohorts to each other and the two RTC cohorts to each other on both baseline variables (HAM-D, BDI, POMS Depression subscale, POMS Anxiety subscale, DAS, PES-MR, drinking self-efficacy, age, years of education, number of previous treatments for alcohol use, ADS, and age of onset of alcohol dependence) and drinking outcome variables. Nonparametrics, Mann–Whitney U and Kruskal–Wallis one-way analysis of variance (ANOVA) were used because of small sample sizes. No significant differences were found for any of the baseline or outcome variables between either the RTC cohorts or the CBT-D cohorts, all ps > .09.
Because using a sequential, nonoverlapping design also raises the possibility of a seasonal effect, we divided cohorts into seasons on the basis of the date of the first day of treatment. One CBT-D cohort started in the winter, 1 CBT-D and 1 RTC cohort in the spring, 1 RTC cohort in the summer, and 1 CBTD cohort started in the fall. The four groups were compared on the following baseline variables: HAM-D, BDI, POMS Depression subscale, POMS Anxiety subscale, DAS, PES-MR, drinking self-efficacy, age, number of years of education, number of previous treatments for alcohol use, ADS, and age of onset of alcohol dependence. No significant differences were found using the Kruskal–Wallis one-way ANOVA, allps > .20. Thus, we feel confident that there were no biases that were due to either cohort effects or seasonal effects.
Relationship Between Baseline Variables and Drinking Outcomes
Before testing the effects of treatment condition on drinking outcomes (percent days abstinent and drinks per day at both baseline to 3-month follow-up and 3- to 6-month follow-ups), partial correlation coefficients were computed to examine whether the following baseline variables were significantly related to drinking outcomes: HAM-D, BDI, POMS Depression subscale, POMS Anxiety subscale, DAS, PES-MR, drinking self-efficacy, gender, age, number of years of education, number of previous treatments for alcohol use, ADS, age of onset of alcohol dependence, and past history of major depressive disorder (excluding organic rule out). Because of the number of correlations, we used a significance level of p < .01 to control for Type I error. Controlling for the corresponding baseline drinking variable, none of the baseline variables were significantly related to drinking outcomes at either follow-up paint.
In addition, we computed partial correlations to examine whether use of antidepressant medication at admission and at discharge from the partial hospital program was related to drinking outcomes. In the RTC condition, 6 participants were on antidepressant medication on admission and 8 participants were on antidepressant medication at discharge. In the CBT-D condition, 4 participants were on antidepressant medication at admission and 6 were on antidepressant medication when discharged. There were no between group differences at either admission or discharge and antidepressant use was not significantly related to any drinking outcome variables, all ps > .10.
Treatment Effects: Change in Depressive Symptoms and Depressed and Anxious Mood
We used repeated measures analyses of covariance (ANCOVA), with baseline percent days abstinent as the covariate, to investigate the effect of time (pretreatment vs. posttreatment) and treatment condition on measures of depressive symptoms and mood. Separate 2 × 2 (Treatment × Time) analyses were conducted for the three depression measures and for anxious mood.
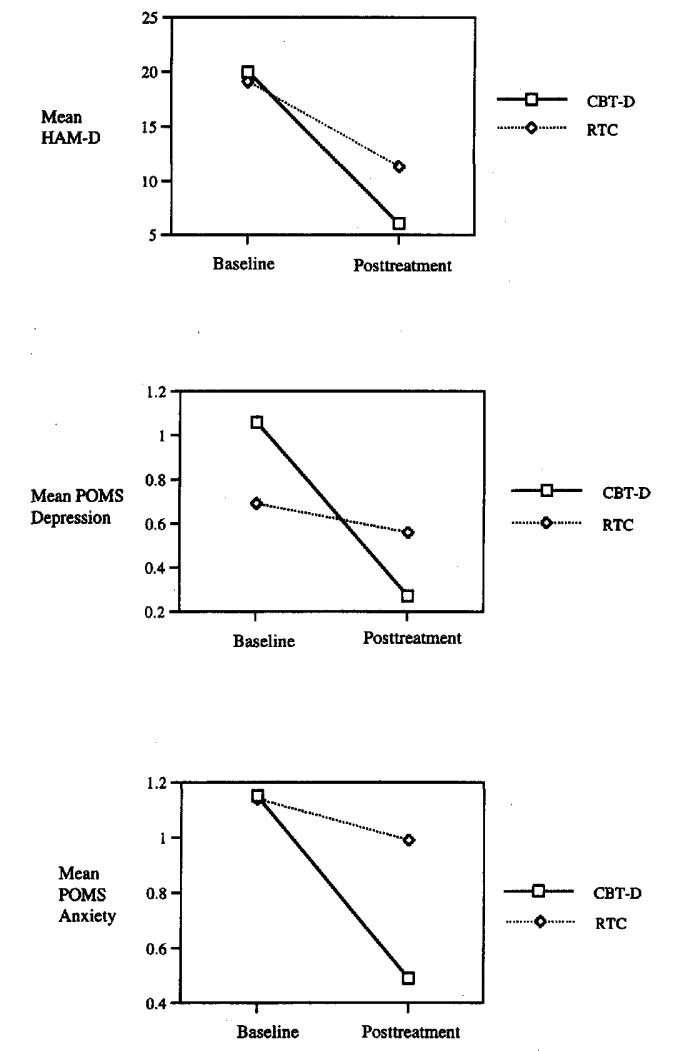
Significant main effects for Time were found on the HAM-D, F(1, 32) = 54.93, p < .001; BDI, F(1, 32) = 42.36, p < .001; POMS Depression subscale, F(1, 30) = 17.04, p < .001; and POMS Anxiety subscale, F(1, 30) = 14.25, p < .01, with participants in both conditions reporting less depressive symptoms and negative mood from pre- to posttreatment. No significant main effects of treatment were found on the HAM-D, BDI, or either POMS subscale. However, a significant Treatment × Time interaction was found on the HAM-D, F(1, 32) = 4.15, p = .05; POMS Depression subscale, F(1, 30) = 8.5, p < .01; and POMS Anxiety subscale, F(1, 30) = 5.68, p < .03; with patients in the CBT-D condition showing a greater decrease in depressive symptoms and negative mood than those in the RTC condition between pre- and posttreatment (see Figure 1). No significant Treatment × Time interaction was found with the BDI.
Figure 1.
Depressive symptoms and negative moods by treatment condition and time. CBT-D = cognitive-behavioral treatment for depression; RTC = relaxation training control; HAM-D = Modified Hamilton Rating Scale for Depression; POMS = Profile of Mood States; Depression = Depression subscale; Anxiety = Anxiety subscale.
Treatment Effects: Change in Cognitive–Behavioral Process Variables
Repeated measures ANCOVAs, with baseline percent days abstinent as the covariate, were used to examine the effects of Time (pretreatment vs. posttreatment) and treatment on cognitive–behavioral process variables for the measurement of dys-functional attitudes, pleasant events, and drinking self-efficacy. The effect of Time was significant for dysfunctional attitudes, F(1, 32) = 10.19, p < .01, and approached significance for drinking self-efficacy, F(1, 24) = 4.06, p < .06, with both treatment conditions showing a decrease in dysfunctional attitudes and an increase in self-efficacy over time. There was a nonsignificant effect of Time for pleasant events (p > .10). No significant effects of Treatment or Treatment × Time interactions were found for any of the three process variables. Given diese results, we did not proceed to test for mediation effects, as significant treatment effects on these variables were a prerequisite condition for mediation (Baron & Kenny, 1986).
Treatment Effects: Changes in Drinking Status, Frequency and Quantity
Drinking status
For both the 0- to 3-month and 3- to 6-month intervals, participants were coded as having drank or not and as having drank heavily or not (i.e., consumed more than six standard alcoholic drinks for men, or five for women on any one day) during that 3-month interval. These results are presented in Table 1. For the first 3 months, both chi-square analyses (Treatment × Any Drinking and Treatment × Heavy Drinking) were nonsignificant. During the second follow-up interval (3 to 6 months posttreatment), the chi-square analysis was significant for any drinking, χ2(1, N = 32) = 4.22, p < .04, with 53% of CBT-D participants drinking (at least once) during this 3-month period compared with 87% of RTC participants. The chi-square analysis for heavy drinking during the second 3-month follow-up interval was nonsignificant.
Table 1.
Means and Standard Deviations of Dependent Variables by Treatment Condition
| CBT-D (n = 19) |
RTC (n = 16)a |
||||
|---|---|---|---|---|---|
| Measure | M | SD | M | SD | Between-group differences |
| Baseline | |||||
| HAM-D | 20.0 | 9.6 | 19.1 | 6.9 | ns |
| BDI | 19.7 | 5.4 | 19.8 | 7.0 | ns |
| POMS-Depression scale | 1.1 | 0.9 | 0.7 | 0.7 | ns |
| POMS-Anxiety scale | 1.2 | 0.7 | 1.1 | 0.6 | ns |
| % days abstinent | 35.1 | 31.8 | 36.6 | 28.4 | ns |
| No. of drinks per day | 8.30 | 4.74 | 8.95 | 8.47 | ns |
| Posttreatmentb | |||||
| HAM-D | 6.1 | 5.3 | 11.3 | 8.1 | F(1,32) = 4.15* |
| BDI | 7.6 | 7.5 | 10.2 | 9.1 | ns |
| POMS-Depression scale | 0.3 | 0.3 | 0.6 | 0.7 | F(1, 30) = 8.50** |
| POMS-Anxiety scale | 0.5 | 0.2 | 1.0 | 0.7 | F(1, 30) = 5.68* |
| 0–3 months | |||||
| % days abstinent | 96.8 | 5.1 | 89.7 | 16.7 | t(30) = 2.25* |
| No. of drinks per day | 0.32 | 0.53 | 1.68 | 5.05 | ns |
| % totally abstinent | 47.1 | 33.3 | ns | ||
| %drinking heavily | 29.4 | 40.0 | ns | ||
| 3–6 months | |||||
| % days abstinent | 90.5 | 21.2 | 68.3 | 36.6 | t(30) = 2.95** |
| No. of drinks per day | 0.46 | 0.75 | 5.71 | 12.59 | t(30) = 2.12* |
| % totally abstinent | 47.1 | 13.3 | χ2(1, N = 32) = 4.22* | ||
| % drinking heavily | 47.1 | 66.7 | ns | ||
Note. CBT-D = cognitive–behavioral treamtent for depression; RTC = relaxation training control; HAM-D = Modified Hamilton Rating Scale for Depression; BDI = Beck Depression Inventory; POMS = Profile of Mood States.
At posttreatment, n = 15.
Statistical tests reflect Treatment Condition × Time interactions.
p ≤ .05.
p < .01.
Drinking frequency and quantity
Because of skewness, all variables involving percent abstinent days were normalized using log transformations and mean number of drinks per day using inverse transformations, and the transformed variables were used in all analyses. However, raw scores were used in all figures for ease of interpretation. Separate 2 × 2 (Treatment × Time) repeated measures ANCOVAs were conducted for percent days abstinent and mean number of drinks per day. We entered both the 0- to 3-month and 3- to 6-month follow-up values as the repeated measure, with the corresponding variable at base-line (for past 180 days) serving as the covariate.
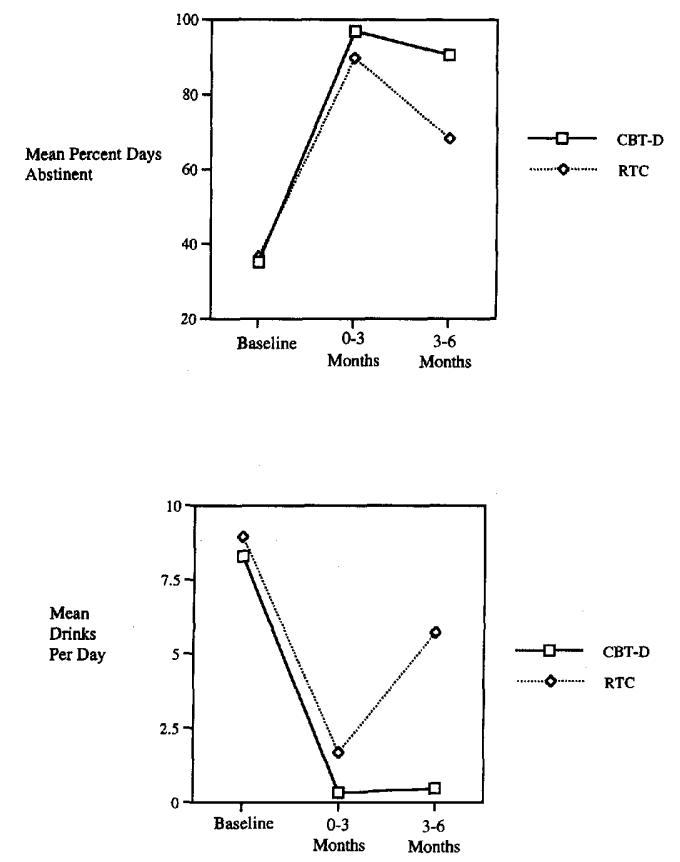
The repeated measures ANCOVA for percent days abstinent revealed a significant main effect for Time, F(1, 30) = 8.64, p < .01, as percent abstinent days at follow-up declined over time in both conditions. More relevant to the study hypotheses, the analysis revealed a significant effect of Treatment, F(1, 29) = 8.21, p < .01, and a Treatment × Time interaction that approached significance, F(1, 30) = 2.85, p = .10. Examination of Figure 2 reveals that the overall percentage of days abstinent is higher in the CBT-D condition than in the RTC and that the decrease in percent days abstinent from the first to the second follow-up interval is greater in the RTC condition than in the CBT-D. A simple effects test across groups at each time point revealed a significantly greater percent days abstinent at 0- to 3-month follow-up, t(30) = 2.25, p = .03, and at 3- to 6-month follow-up, t(30) = 2.95, p < .01, in the CBT-D condition relative to the RTC. In addition, a simple effects test within groups across time showed that, whereas the RTC condition had a significant decrease in percent days abstinent, t(14) = 2.48, p < .03, from the first to the second 3 months of follow-up, the CBT-D condition did not change significantly (p > .10).
Figure 2.
Drinking frequency and quantity at follow-up by treatment condition and time. CBT-D cognitive–behavioral treatment for depression; RTC = relaxation training control.
On the mean number of drinks per day, the repeated measures ANCOVA revealed a significant main effect of Time, F(1, 30) = 8.64, p < .01; a nonsignificant effect of Treatment, F( 1, 29) = 2.67, p > . 10; and a significant Treatment × Time interaction, F(1, 30) = 4.10, p = .05. Examination of Figure 2 shows that mean number of drinks per day is lower in the CBT-D group between 3- and 6-month follow-up and that RTC patients had a greater increase in mean number of drinks per day than patients receiving CBT-D. A simple effects test between groups at each time point indicated that the two groups did not differ significantly at 0- to 3-month follow-up but that CBT-D patients drank significantly fewer drinks per day than RTC patients at 3- to 6-month follow-up, t(30) = 2.12, p < .05. A simple effects test within groups across time confirmed that, although the CBT-D condition did not change significantly from the first to the second 3 months (p > .10), the RTC condition's mean number of drinks per day increased significantly, t(14) = 2.62, p < .03.
Relationship Between Depressive Symptoms and Drinking Outcome
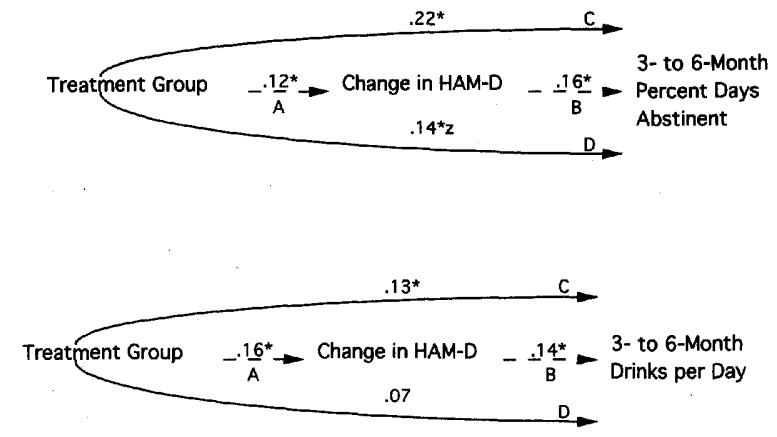
Given our findings that CBT-D intervention resulted in greater decreases in depressive symptoms during treatment and in improved drinking frequency and quantity at longer term followup, we examined whether change in depressive symptoms mediated the relationship between treatment condition and these drinking outcomes from 3- to 6- months after treatment; that is, did patients in the CBT-D condition drink less at follow-up because of improved levels of depressive symptoms? For change in depressive symptoms to be a mediator, the following conditions must be met: (a) treatment condition is significantly related to change in depressive symptoms; (b) change in depressive symptoms is significantly related to drinking outcome; (c) treatment is significantly related to drinking outcome; and (d) after controlling for change in depressive symptoms, either treatment is no longer significantly related to drinking outcome or the relationship between treatment and outcome is significantly reduced (Baron & Kenny, 1986).
To test these conditions, we performed a series of regression analyses. We controlled for the appropriate baseline drinking variable by entering it first in all regression analyses. First, change in depressive symptoms was regressed onto treatment condition (Figure 3, Line A). Second, drinking outcome was regressed onto change in depressive symptoms (Figure 3, Line B). Third, drinking outcome was regressed onto treatment condition (Figure 3, Line C). Fourth, drinking outcome was regressed onto treatment condition after controlling for change in depressive symptoms (Figure 3, Line D). According to the aforementioned criteria, evidence suggests that change in HAM-D is a mediator of the relationship between treatment condition and 3- to 6-month drinking outcomes. The only possible exception was that the relationship between treatment condition and percent days abstinent was still statistically significant after controlling for change in depressive symptoms and the decrease in the strength of the relationship between treatment and drinking required to show mediation only approached significance (p <.08; Meng, Rosenthal, & Rubin, 1992).
Figure 3.
The mediating effect of change in depressive symptoms on the relationship between treatment and drinking outcome. A series of regression analyses were performed with the appropriate baseline drinking variable controlled for by entering it first in all regression analyses. First, change in depressive symptoms was regressed onto treatment condition (A). Second, drinking outcome was regressed onto change in depressive symptoms (B). Third, drinking outcome was regressed onto treatment condition (C). Fourth, drinking outcome was regressed onto treatment condition after controlling for change in depressive symptoms (D). Numbers represent squared correlations, z = the decrease from .22 to .14 approached significance, p < .08. HAM-D = Modified Hamilton Rating Scale for Depression. *p < .05.
Posttreatment Alcoholics Anonymous (AA) Participation
The standard partial hospitalization treatment for alcohol-dependent patients includes strong encouragement for participation in AA programs. Therefore, patients were asked at 1-, 3-, and 6-month follow-ups whether they had attended any AA meetings and if so, how many meetings they had attended at each followup interval. At 1 month, 94% of CBT-D and 64% of RTC patients had attended one or more AA meetings since posttreatment, χ2 (1 ,N = 27) = 3.92, p < .05; at 3 months, 87% of CBT-D and 42% of RTC patients had attended AA meeting (or meetings) since the 1-month follow-up, χ2 (1, N = 27) = 6.08, p < .02; and at 6 months, 81% of CBT-D and 27% of RTC patients had attended AA meetings since the 3-month follow-up, χ2 (1, N = 31) = 9.31, p < .01. There were also significant differences in the number of AA meetings attended by the CBT-D versus those attended by the RTC patients between posttreatment and 1 month (Mdns = 11 and 0, respectively), between 1 and 3 months (Mdns = 27 and 0, respectively), and between 3 and 6 months (Mdns = 31 and 0, respectively); Mann–Whitney tests, all ps < .005. Although patients were not asked directly if they had attended AA meetings before treatment, they were asked how many days they had received treatment in an outpatient setting, including AA, in the 30 days before starting treatment. No significant pretreatment difference was found between treatment conditions; CBT-D, M = 1.05, RTC, M = 2.38 (p > .10).
AA Participation and Drinking Outcome
Because there were treatment group differences on AA attendance during follow-up, we reexamined the relationship between treatment group and drinking outcomes after covarying the number of AA sessions attended. Specifically, using regression analyses, we examined the relationship between treatment group and drinking outcomes between 3- and 6-month follow-ups, with and without covarying the number of AA sessions attended from 0- to 3-months. As expected, without covarying AA sessions, treatment group significantly predicted 3- to 6-month percent days abstinent (r = .47, p = .006), number of drinks per day (r = .36, p = .04), and drinking status (i.e., totally abstinent vs. any drinking), model χ2 (1, N = 32) = 4.46, p = .03. After covarying me number of AA sessions attended from 0- to 3-months, we found that treatment group continued to significantly predict 3- to 6-month percent days abstinent (r2 change = .18, p = .01) and number of drinks per day (r2 change = .18, p = .01), and the prediction of 3- to 6-month drinking status approached significance, model χ2(1, N = 27) improvement = 2.69, p = .10.
Discussion
Alcoholics with elevated levels of depressive symptoms who received CBT-D in addition to standard alcohol treatment had significantly greater reductions in somatic depressive symptoms and in depressed and anxious mood at posttreatment than did patients in standard alcohol treatment who received a relaxation training control. Patients receiving CBT-D had a greater percentage of days abstinent but not greater overall abstinence or fewer drinks per day during the first 3-month follow-up period. However during the second 3 months, CBT-D patients drank significantly less on all three measures compared to patients in the RTC condition. From 3 to 6 months after treatment, 47% of patients receiving CBT-D were completely abstinent, compared with 13% of RTC patients, and CBT-D patients reported a higher percentage of days abstinent (90.5% vs. 68.3%) and fewer drinks per day (0.46 vs. 5.71) than RTC patients. These differences appear to be due to the fact that the CBT-D group maintained improvement in drinking outcomes during the second 3 months of follow-up, whereas the RTC group did not. Finally, there was suggestive evidence that the decrease in somatic depressive symptoms functioned as a mediator of the treatment effect on percent days abstinent and mean drinks per day during the 3- to 6-month follow-up period.
The results of this study confirm the basic premise that adding CBT-D to standard alcohol treatment is an effective means of reducing depressive symptoms and improving drinking outcomes for alcoholics with elevated depressive symptoms, relative to adding an RTC condition. Patients seemed to gain a better understanding of depression and the factors that affected their moods, and they viewed the depression coping skills as useful and relevant to their recovery from alcohol dependence. These results confirm and extend those of Turner and Wehl (Turner & Wehl, 1984) by including an active control condition equated for contact time. The finding that CBT-D patients had greater decreases in somatic depressive symptoms than RTC patients during treatment is particularly striking, given that the CBT-D group had to “outperform” the depressive symptom reduction (of 41%) in the RTC condition. It is notable that initial depression severity scores in this study were lower than those generally seen in depression treatment outcome studies, because this would predispose the data against finding a significant treatment by time interaction. This provides an additional reason to place confidence in this finding.
During the first 3 months after treatment, patients receiving depression coping skills training plus standard treatment drank less frequently but did not drink less in amount. A possible explanation is that the coping skills training in the CBT-D condition may have served to decrease slips or the onset of drinking episodes; however, once drinking was initiated, this training may have had no effect on the amount of alcohol consumed. This interpretation is consistent with findings that depressed mood or negative affect situations are important triggers for drinking lapses (Marlatt & Gordon, 1985; Pickens et al., 1985). However, once drinking is initiated, mood may have less of an impact on drinking quantity, and factors such as decreased self-efficacy and the abstinence violation effect (Marlatt & Gordon, 1985) may be more potent determinants of the amount of alcohol consumed.
It is interesting to note that the treatment groups diverged more during the second 3 months of follow-up, and that treatment effects were demonstrated across all three drinking measures (frequency, quantity, and complete abstinence) during this longer term follow-up. One possibility, although not directly assessed in this study, is that patients receiving CBT-D maintained treatment gains on mood and depressive symptoms over time relative to RTC patients and that maintenance of these gains resulted in improved drinking outcomes. Although speculative with regard to this study, this idea is consistent with findings in the depression treatment outcome literature of a general maintenance of treatment gains among patients receiving CBT-D (Brown & Lewinsohn, 1984a; Jarrett & Rush, 1994; Paykel, 1989).
The evidence from this study suggesting that reductions in somatic depressive symptoms served to mediate the relationship between treatment condition and drinking outcomes is of interest. To our knowledge, no other studies have fully examined the question of whether depressive symptoms have mediated the relationship between treatment and drinking outcomes. It is important to note that, as might be expected with abstinence during standard treatment alone (Brown & Schuckit, 1988), patients in the RTC condition experienced a considerable decrease in depressive symptoms, albeit significantly less so than patients in the CBT-D condition. Therefore, the mediating mechanism suggested by our data may be a function of the magnitude of the reductions in somatic depressive symptoms or of the means by which the reductions were brought about (i.e., as a result of depression coping skills training), or both. For instance, one may wonder whether effects on depressive symptoms achieved through a placebo-controlled trial of antidepressant medication would show the same type of mediation of drinking outcomes. Nonetheless, although these findings await replication, this preliminary evidence for mediation appears to confirm the importance of the role of depressive symptoms in recovery from alcohol dependence and the need to address depression as a signifi-cant factor in alcohol treatment.
Despite our expectation that patients in the CBT-D group would experience greater pre- to posttreatment changes in dys-functional attitudes, pleasant activities, and drinking self-efficacy than RTC patients, no treatment effects were found on these variables. It is possible that involvement in the strong background treatment precluded differential change in the process variables that improved in both conditions (i.e., dysfunctional attitudes and self-efficacy). Both groups received an active standard partial hospital alcohol program and the relaxation training “control” group received an intervention that offered a relevant and useful skill. Increased self-efficacy and decreased dysfunctional attitudes may have been due to participation in treatment generally and to reductions in depressive and mood symptoms occurring with abstinence in both conditions. There-fore, the lack of between-group differences may best be construed as the failure of the CBT-D group to outperform the considerable changes in these two process variables occurring in the RTC group.
The finding that patients receiving CBT-D attended AA meetings more frequently than RTC patients over the 6-month followup interval is of particular interest. As the groups did not differ on any pretreatment variables including outpatient and AA participation, there is no compelling reason to suspect a priori that one group would attend AA more frequently than the other. Rather, it may be that the increased AA participation among CBT-D patients was related to and facilitated by the specific treatment elements of the CBT-D treatment in combination with the standard alcohol treatment program. This could have taken place as a function of the decreased depressive symptoms and mood levels experienced in the CBT-D condition or by specific training received in assertiveness, increasing the quality of social interactions or cognitive restructuring. Interestingly, in analyses covarying number of AA sessions attended, significant between group differences on percent days abstinent and drinks per day (from 3 to 6 months) suggest that the improved drinking out-comes on these measures in the CBT-D group were not a function of increased AA participation but rather of the specific CBT-D treatment that was added to standard treatment. Results from the third dependent variable, drinking status, were suggestive but did not attain statistical significance, thus leaving open the possibility that greater abstinence achieved in the CBT-D group was due to increased AA participation. Unfortunately, the limited sample size of the present study precludes drawing more definitive conclusions on this issue. Future studies applying CBT-D interventions in alcoholism should further explore the possibility of intervention effects on AA participation, as well as the effects of AA participation on drinking outcomes.
The use of CBT-D plus standard alcohol treatment for alcohol-dependent patients can serve as a viable alternative to treatment with antidepressant medication. Results of studies examining the usefulness of antidepressant medications in alcoholism treatment have been equivocal (e.g., McGrath et al., 1996), and issues regarding which patients should receive pharmacological interventions and when these treatments should be initiated continue to be the topic of intense debate (Brown & Schuckit, 1988; Brown et al., 1995). These questions are of concern considering that aggressive antidepressant treatment may expose patients to needless expense and potential medication toxicity and may encourage patients to attribute mood improvement to medication rather than to sobriety. A major advantage of CBTD is that it can be initiated early in alcoholism treatment with little or no risk to the patient and without some of the inherent problems and confusion surrounding the use of antidepressant medication.
The present study was somewhat limited by its modest sample size. Failure to detect treatment effects on process variables and to identify predictors of treatment outcome may have been due to insufficient power. Nonetheless, significant treatment effects were found on depressive and mood symptoms and on alcohol use outcomes, particularly at longer term follow-up, suggesting that the size of these effects were large. Because of the use of a design involving successive cohort assignment, HAM-D interviewers were aware of participants' treatment condition. However, future studies should endeavor to remove this potential bias. Given that this study was conducted in a private hospital setting with well-educated, Caucasian patients, caution is advised in generalizing these findings to populations with substantially different characteristics. On the positive side, the sample was reasonably representative in terms of addiction severity, alcohol consumption, and gender representation. Generalizability of our findings may also be limited by the nature of the group treatment-based, partial hospital alcohol program to which the two treatments in this study were added. The extent to which results would be similar if added to a strictly individual treatment-based program or any other program of differing characteristics remains to be determined.
Future, large-scale studies testing the use of CBT-D in alcoholics with elevated depressive symptoms appear warranted. These studies may serve to elucidate process-to-outcome relationships by incorporating a broader range of process measures (e.g., measures of positive and negative thoughts, and assertiveness) and by including measures of depressive symptoms at follow-up intervals. Future studies might also evaluate the comparative efficacy of individual versus group CBT-D treatment, given the equivalence of these modalities demonstrated in the original work on the Coping With Depression course (Brown & Lewinsohn, 1984a). Finally, provided the findings from this study withstand replication, future studies on the efficacy of combination treatments with antidepressant medication would be of interest, particularly given the demonstrated efficacy of combining antidepressant and cognitive–behavioral therapies in the treatment of unipolar depression (Miller & Keitner, 1996; Wright & Thase, 1992).
Footnotes
This study was supported in part by a developmental research grant from the Department of Psychiatry and Human Behavior, Brown University. We thank Peter M. Lewinsohn, Raymond Niaura, and Susan Ramsey for their helpful comments on an earlier draft of the manuscript. We also gratefully acknowledge the research assistance of Virginia Smith, Michelle Ricci, Jessica Whiteley, Thomas Aguiar, and Suzanne Sales. Thanks also to Mary Dubreuil, who provided assistance in accessing study participants, and to James Hittner, who served as a therapist in the study and provided helpful suggestions in the development of treatment manuals.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed. Author; Washington, DC: 1987. [Google Scholar]
- Annis HM. Situational Confidence Questionnaire. Addiction Research Foundation; Toronto, Ontario, Canada: 1988. [Google Scholar]
- Babor TF, Stephans RS, Marian GA. Verbal report methods in clinical research on alcoholism: Response bias and its minimization. Journal of Studies on Alcohol. 1987;48:410–424. doi: 10.15288/jsa.1987.48.410. [DOI] [PubMed] [Google Scholar]
- Baekland F, Lundwall L, Shanahan TJ. Correlates of patient attrition in the outpatient treatment of alcoholism. The Journal of Nervous and Mental Disease. 1973;157:99–107. doi: 10.1097/00005053-197308000-00002. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford Press; New York: 1978. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benson H. The relaxation response. William Morrow; New York: 1975. [Google Scholar]
- Berglund M. Suicide in alcoholism. Archives of General Psychiatry. 1984;41:888–891. doi: 10.1001/archpsyc.1984.01790200070009. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lewinsohn PM. Coping with depression: Course workbook. Castalia Press; Eugene, OR: 1984a. [Google Scholar]
- Brown RA, Lewinsohn PM. A psychoeducational approach to the treatment of depression: Comparison of group, individual, and minimal-contact procedures. Journal of Consulting and Clinical Psychology. 1984b;52:774–783. doi: 10.1037//0022-006x.52.5.774. [DOI] [PubMed] [Google Scholar]
- Brown SA, Inaba RK, Gillin JC, Schuckit MA, Stewart MA, Irwin MR. Alcoholism and affective disorder: Clinical course of depressive symptoms. American Journal of Psychiatry. 1995;152:45–52. doi: 10.1176/ajp.152.1.45. [DOI] [PubMed] [Google Scholar]
- Brown SA, Schuckit MA. Changes in depression among abstinent alcoholics. Journal of Studies on Alcohol. 1988;49:412–417. doi: 10.15288/jsa.1988.49.412. [DOI] [PubMed] [Google Scholar]
- Burns DD. Feeling good. William Morrow; New York: 1980. [Google Scholar]
- Dorus W, Kennedy J, Gibbons RD, Ravi SD. Symptoms and diagnosis of depression in alcoholics. Alcoholism: Clinical and Experimental Research. 1987;11:150–154. doi: 10.1111/j.1530-0277.1987.tb01279.x. [DOI] [PubMed] [Google Scholar]
- Ellis A, Harper RA. A guide to rational living. Wilshire; Hollywood, CA: 1961. [Google Scholar]
- Glasgow RE, Toobert DJ, Hampson SE, Brown JE, Lewinsohn PM, Donnelly J. Improving self-care among older patients with Type II diabetes: The “Sixty Something …” study. Patient Education and Counseling. 1992;19:61–74. doi: 10.1016/0738-3991(92)90102-o. [DOI] [PubMed] [Google Scholar]
- Hatsukami D, Pickens RW. Posttreatment depression in an alcohol and drug abuse population. American Journal of Psychiatry. 1982;139(12):1563–1566. doi: 10.1176/ajp.139.12.1563. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. Journal of Studies on Alcohol. 1988;49:219–224. doi: 10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- Hesselbrock MN. Gender comparison of antisocial personality disorder and depression in alcoholism. Journal of Substance Abuse. 1991;3:205–219. doi: 10.1016/s0899-3289(05)80037-9. [DOI] [PubMed] [Google Scholar]
- Hesselbrock MN, Hesselbrock VM, Tennen H, Meyer RE, Workman KL. Methodological considerations in the assessment of depression in alcoholics. Journal of Consulting and Clinical Psychology. 1983;51:399–405. doi: 10.1037//0022-006x.51.3.399. [DOI] [PubMed] [Google Scholar]
- Hesselbrock VM, Hesselbrock MN, Workman-Daniels KL. Effects of major depression and antisocial personality on alcoholism: Course and motivational factors. Journal of Studies on Alcohol. 1986;47:207–212. doi: 10.15288/jsa.1986.47.207. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Najavits L. Review of empirical studies on cognitive therapy. In: Frances AJ, Hales R, editors. Review of psychiatry. Vol. 7. American Psychiatric Press; Washington, DC: 1988. pp. 643–666. [Google Scholar]
- Jacobsen E. Progressive relaxation. University of Chicago Press; Chicago: 1929. [Google Scholar]
- Jarrett RB, Rush AJ. Short-term psychotherapy of depressive disorders: Current status and future directions. Psychiatry. 1994;57:115–132. doi: 10.1080/00332747.1994.11024675. [DOI] [PubMed] [Google Scholar]
- Keeler MH, Taylor CI, Miller WC. Are all recently detoxified alcoholics depressed? American Journal of Psychiatry. 1979;136:586–588. [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder EC. Rigor, but not rigor mortis, in depression research. Journal of Personality and Social Psychology. 1995;68(5):892–894. doi: 10.1037//0022-3514.68.5.892. [DOI] [PubMed] [Google Scholar]
- Klajner P, Hartman LM, Sobell MB. Treatment of substance abuse by relaxation training: A review of its rationale, efficacy and mechanisms. Addictive Behaviors. 1984;9:41–55. doi: 10.1016/0306-4603(84)90006-6. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Myers CP, Corty E. Assessment and classification of patients with psychiatric and substance abuse syndromes. Hospital Community Psychiatry. 1989;40:1019–1025. doi: 10.1176/ps.40.10.1019. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Antonuccio DO, Breckenridge JS, Teri L. The Coping with Depression Course: A psychoeducational intervention for unipolar depression. Castalia; Eugene, OR: 1984. [Google Scholar]
- Lewinsohn PM, Clarke GN, Hops H, Andrews J. Cognitive-behavioral treatment for depressed adolescents. Behavior Therapist. 1990;21:385–401. [Google Scholar]
- Lewinsohn PM, Graf M. Pleasant activities and depression. Journal of Consulting and Clinical Psychology. 1973;41:261–268. doi: 10.1037/h0035142. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention. Guilford Press; New York: 1985. [Google Scholar]
- McCrady BS, Dean L, Dubreuil E, Swanson S. The Problem Drinker's Project: A programmatic application of social-learning-based treatment. In: Marlatt GA, Gordon JR, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York: 1985. pp. 417–471. [Google Scholar]
- McGrath PJ, Nunes EV, Stewart JW, Goldman D, Agosti V, Ocepek-Welikson K, Quitkin FM. Imipramine treatment of alcoholics with primary depression: A placebo-controlled clinical trial. Archives of General Psychiatry. 1996;53:232–240. doi: 10.1001/archpsyc.1996.01830030054009. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. BITS manual for the Profile of Mood States. Educational and Industrial Testing Service; San Diego, CA: 1971. [Google Scholar]
- Meng X, Rosenthal R, Rubin DB. Comparing correlated correlation coefficients. Psychological Bulletin. 1992;111:172–175. [Google Scholar]
- Miller IW, Keitner GI. Combined medication and psychotherapy in the treatment of chronic mood disorders. The Psychiatric Clinics of North America. 1996;19:151–171. doi: 10.1016/s0193-953x(05)70279-3. [DOI] [PubMed] [Google Scholar]
- Miller IW, Norman WH, Bishop SB. The Modified Hamilton Rating Scale for Depression. Psychiatry Research. 1985;14:131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- Monti PM, Abrams DB, Binkoff JA, Zwick WR, Liepman MR, Nirenberg TD, Rohsenow DJ. Communication skills training, communication skills training with family and cognitive-behavioral mood management training for alcoholics. Journal of Studies on Alcohol. 1990;51:263–270. doi: 10.15288/jsa.1990.51.263. [DOI] [PubMed] [Google Scholar]
- O'Sullivan K, Rynne C, Miller J, O'Sullivan S, Fitzpatrick V, Hux M, Cooney J, Clare A. A follow-up study on alcoholics with and without co-existing affective disorder. British Journal of Psychiatry. 1988;152:813–819. doi: 10.1192/bjp.152.6.813. [DOI] [PubMed] [Google Scholar]
- Paykel ES. Treatment of depression: The relevance of research for clinical practice. British Journal of Psychiatry. 1989;155:754–766. doi: 10.1192/bjp.155.6.754. [DOI] [PubMed] [Google Scholar]
- Pickens RW, Hatsukami DK, Spicer JW, Svikis DS. Relapse by alcohol abusers. Alcoholism: Clinical and Experimental Research. 1985;9:244–247. doi: 10.1111/j.1530-0277.1985.tb05744.x. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Ross HE, Glaser FB, Germanson T. The prevalence of psychiatric disorders in patients with alcohol and other drug problems. Archives of General Psychiatry. 1988;45:1023–1031. doi: 10.1001/archpsyc.1988.01800350057008. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Archives of General Psychiatry. 1987;44:505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Relapse following smoking cessation: A situational analysis. Journal of Consulting and Clinical Psychology. 1982;50:71–86. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Allen BA. Alcohol dependence syndrome: Measurement and validation. Journal of Abnormal Psychology. 1982;47:189–191. doi: 10.1037//0021-843x.91.3.199. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers' self-reports of drinking behavior. Behaviour Researach and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Maisto SA, Sobell LC, Cooper AM, Cooper TC, Sanders B. Developing a prototype for evaluating alcohol treatment effectiveness. In: Sobell LC, Sobell MB, Ward E, editors. Evaluating alcohol and drug abuse treatment effectiveness: Recent advances. Pergamon Press; New York: 1980. pp. 129–150. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R. New York State Psychiatric Institute; New York: 1989. [Google Scholar]
- Turner RW, Wehl CK. Treatment of unipolar depression in problem drinkers. Advances in Behavior Research and Therapy. 1984;6:115–125. [Google Scholar]
- U.S. Department of Health and Human Services . Depression in primary care: Vol. 1. Detection and diagnosis. Agency for Health Care Policy and Research, Public Health Service; Rockviile, MD: 1993. [Google Scholar]
- Weissman A, Beck A. Development and validation of the Dysfunctional Attitudes Scale; Paper presented at the 12th annual meeting of the Association for the Advancement of Behavior Therapy; Chicago, IL. Nov, 1978. [Google Scholar]
- Wright J, Thase M. Cognitive and biological therapies: A synthesis. Psychiatric Annuals. 1992;22:451–458. [Google Scholar]