Abstract
Objective To evaluate the effectiveness of cognitive therapy for post-traumatic stress disorder related to terrorism and other civil conflict in Northern Ireland.
Design Randomised controlled trial.
Setting Community treatment centre, Northern Ireland.
Participants 58 consecutive patients with chronic post-traumatic stress disorder (median 5.2 years, range 3 months to 32 years) mostly resulting from multiple traumas linked to terrorism and other civil conflict.
Interventions Immediate cognitive therapy compared with a waiting list control condition for 12 weeks followed by treatment. Treatment comprised a mean of 5.9 sessions during 12 weeks and 2.0 sessions thereafter.
Main outcome measures Primary outcome measures were patients' scores for post-traumatic stress disorder (post-traumatic stress diagnostic scale) and depression (Beck depression inventory). The secondary outcome measure was scores for occupational and social functioning (work related disability, social disability, and family related disability) on the Sheehan disability scale.
Results At 12 weeks after randomisation, immediate cognitive therapy was associated with significantly greater improvement than the waiting list control group in the symptoms of post-traumatic stress disorder (mean difference 9.6, 95% confidence interval 3.6 to 15.6), depression (mean difference 10.1, 4.8 to 15.3), and self reported occupational and social functioning (mean difference 1.3, 0.3 to 2.5). Effect sizes from before to after treatment were large: post-traumatic stress disorder 1.25, depression 1.05, and occupational and social functioning 1.17. No change was observed in the control group.
Conclusion Cognitive therapy is an effective treatment for post-traumatic stress disorder related to terrorism and other civil conflict.
Trial registration Current Controlled Trials ISRCTN16228473.
Introduction
Guidance from the National Institute for Health and Clinical Excellence1 recommends trauma focused cognitive behaviour therapy and eye movement desensitisation and reprocessing therapy as the leading evidence based treatments for post-traumatic stress disorder. These recommendations are largely based on randomised controlled trials that focus on non-terrorism related traumatic events, such as road traffic crashes and rape. Little is known about how to successfully treat trauma resulting from events such as the bombings in London in 2005, the attack on the World Trade Center in New York, and the train bombings in Madrid. The only published evaluation of treatment after a terrorist bomb is an open trial of cognitive therapy for post-traumatic stress disorder (a form of cognitive behaviour therapy) with survivors of the car bomb that exploded in Omagh, Northern Ireland, in 1998. In this uncontrolled study2 cognitive therapy delivered three months to two years after the bombing was associated with improvements in post-traumatic stress disorder as large as those normally observed with cognitive therapy in randomised controlled trials of non-terrorism related post-traumatic stress disorder. In response to these results the Victims Liaison Unit of the Northern Ireland Office established a new treatment centre (the Northern Ireland Centre for Trauma and Transformation) with a Northern Ireland wide remit that would offer trauma focused cognitive therapy to people affected by terrorism and other civil conflict over the past four decades. We evaluated the effectiveness of cognitive therapy provided by the centre.
Methods
The Northern Ireland Centre for Trauma and Transformation was a new initiative that aimed to provide a treatment option that had not been generally available. The service was brought to the attention of potential referrers and the wider community in several ways. An information leaflet and a letter were sent to all general practitioners in Northern Ireland as well as to health authorities and trusts, mental health teams, voluntary and community organisations, self help groups, the clergy, and other community care professionals. A website and several newspaper articles also mentioned the service.
Patients referred to the centre between August 2003 and September 2004 were assessed by mental health clinicians for post-traumatic stress disorder and other psychiatric disorders using the semi-structured clinical interview for the Diagnostic and Statistical Manual of Mental Disorders, (DSM-IV)3 and the clinician administered post-traumatic stress disorder scale for DSM-IV.4 Referrals came from a wide range of sources: community mental health teams (39%), primary care (22%), self referral (21%), voluntary sector and victims' groups (10%), and occupational health (7%). We invited patients meeting diagnostic criteria for post-traumatic stress disorder after traumatic events in adulthood to participate in the trial unless they had another disorder that required immediate treatment. After consent had been obtained patients were randomly allocated to immediate cognitive therapy or to a 12 week wait followed by cognitive therapy. Treatment entailed up to one therapy session a week for 12 weeks, followed by a review and additional therapy sessions if these were indicated by the therapist.
We chose a waiting list control rather than a comparison with another psychological or pharmacological treatment. We did this because we anticipated that many of the patients referred to the centre would be those who had failed more commonly available psychological treatments (such as counselling or debriefing) or pharmacotherapy, and a design that compared cognitive therapy with alternative treatments would have excluded such people. Also, cognitive behaviour therapy had already been shown to be superior to supportive counselling in non-terrorism related post-traumatic stress disorder.5
To determine whether cognitive therapy is effective, at 12 weeks we compared the immediate cognitive therapy and waiting list groups' scores for post-traumatic stress disorder, depression, and functioning (work related disability, social disability, and family related disability). To determine the overall improvement that could be obtained with cognitive therapy, we compared scores before treatment and after treatment, combining the immediate treatment and delayed treatment groups. Patients were followed up 1, 4, and 12 months after treatment to assess maintenance of gains.
An independent office allocated patients to immediate therapy or to wait followed by therapy on a stratified random basis using the minimisation method of Pocock.6 Assessors were not aware of the allocation algorithm. Stratification variables were severity of post-traumatic stress disorder, severity of depression, and presence or absence of continuing physical problems related to the traumatic event (for example, chronic pain, burns requiring multiple surgery). Continuing physical problems had predicted a less favourable outcome in our study of cognitive therapy after the Omagh bomb.2
Measures and assessments
Primary outcome measures were severity of post-traumatic stress disorder, assessed by the post-traumatic stress diagnostic scale,7 and severity of depression, assessed by the Beck depression inventory.8 The secondary outcome measure was the Sheehan disability scale,9 which has separate items for different aspects of functioning (work, social, and family). Each of these self report measures has been validated against interviewer administered measures of the same construct.7 10 11 We obtained scores for each measure before treatment or wait, after 12 weeks (end of wait), after treatment, and at 1, 4, and 12 months' follow-up. Patients also completed the post-traumatic stress diagnostic scale and Beck depression inventory before each treatment session, providing a clinical endpoint measurement for all patients, even if they dropped out. To estimate the magnitude of the changes in scores before and after treatment we calculated effect sizes using the formula: effect size=(mean score before treatment−mean score after treatment)/pooled standard deviation. Cohen12 classified effect sizes as small if 0.20-0.49, medium if 0.50-0.79, and large if 0.8 or more. To investigate possible predictors of improvement we calculated residualised before to after treatment gain scores, which control for variation in baseline levels. We used one way analysis of covariance to compare the therapists' on these scores.
Treatment, therapists, and supervision
The cognitive therapy programme is described in detail elsewhere2 13 and was based on Ehlers and Clark's model of persistent post-traumatic stress disorder.14 The model identifies three factors thought to prolong the disorder, with therapy targeting each factor. The three factors are excessively negative appraisals of the traumatic event or its sequelae, a disturbance in autobiographical memory, and dysfunctional cognitive and behavioural strategies. We used behavioural activation early in therapy to lift mood when initial levels of depression interfered with trauma processing.
Five therapists (one psychiatrist, one social worker, and three nurse therapists) delivered the treatment. Allocation to therapist was based on available slots. Three of the therapists had been trained to diploma level in Beckian cognitive therapy, and the remaining two had completed ENB 650 style cognitive behaviour therapy courses for nurses. Although three of the therapists had four or five years' experience of treating patients using the Ehlers and Clark model,14 the other two had modest experience. The therapists attended a two day workshop on the application of the model, delivered by MD and KG.
Statistical analysis
We determined sample sizes on the basis of 86% power to detect differences of at least 7 points on the post-traumatic stress diagnostic scale between immediate therapy and wait with a 5% significance level. We carried out analyses on an intention to treat basis and on patients who completed the study, including patients in the waiting list group who subsequently completed cognitive therapy. Patients were classified as having completed the study if they had at least six sessions of treatment or they ended therapy earlier as agreed by the therapist because of noticeable improvement. Comparisons between the immediate treatment and waiting list groups at 12 weeks were based on analyses of covariance, with scores before treatment or wait as covariates. We used t tests to compare scores before treatment, after treatment, and at follow-up. Some trauma related characteristics (number of traumas, years since the traumatic event) were not normally distributed and were transformed before analysis. No patients started drugs while in the study. Preliminary analyses included drug status at intake and several patient characteristics (a civilian, experienced a bombing, or taken hostage) as factors. None of these variables was related to outcome and are not considered further.
To quantify individual differences in symptom change, we followed the Omagh bomb study2 and calculated percentage change in scores for post-traumatic stress disorder (from before to after treatment) for all treated patients.
Results
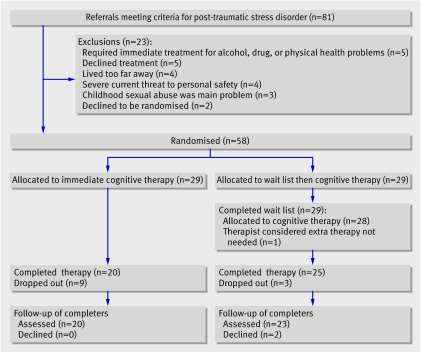
Fifty eight consecutive patients who met the criteria for post-traumatic stress disorder participated in the trial (figure): 29 were allocated to immediate cognitive therapy and 29 to a 12 week wait followed by cognitive therapy.15 The groups were similar at baseline for personal details, psychiatric status, trauma history, and previous treatments (table 1). Most patients had experienced multiple traumatic events. The trauma that was most prominent as an intrusive memory for each patient was identified and described in detail (table 1).
Flow of patients through trial
Table 1.
Baseline characteristics of patients with post-traumatic stress disorder allocated to immediate cognitive therapy or to a waiting list. Values are numbers (percentages) unless stated otherwise
| Variable | Immediate cognitive therapy group (n=29) | Waiting list group (n=29) |
|---|---|---|
| Mean (SD) post-traumatic diagnosis scale | 34.7 (7.8) | 36.8 (6.8) |
| Mean (SD) Beck depression inventory | 35.4 (9.9) | 35.6 (11.3) |
| Mean (SD) Sheehan disability scale | 7.8 (1.4) | 8.6 (1.6) |
| Mean (SD) age (years) | 44.1 (11.3) | 43.7 (12.3) |
| Women | 10 (34) | 13 (45) |
| Civilian | 14 (48) | 21 (72) |
| Police, soldier, or other profession with active involvement | 15 (52) | 8 (28) |
| Experienced multiple traumatic events | 25 (86) | 22 (76) |
| Median (range) No of traumatic events | 3 (1-9) | 3 (1-10) |
| Median (range) years since index event | 8 (0.3-33) | 5.4 (0.2-32) |
| Median (range) duration (years) of post-traumatic stress disorder | 5 (0.3-25) | 5.4 (0.2-32) |
| Characteristics of index trauma event: | ||
| Related to Northern Ireland “troubles” | 24 (83) | 25 (86) |
| Terrorist events outside Northern Ireland | 2 (7) | 1 (4) |
| Bombings | 14 (48) | 9 (31) |
| Shootings and killings | 4 (14) | 9 (31) |
| Taken hostage | 6 (21) | 2 (7) |
| Physical assault | 2 (7) | 6 (21) |
| Road injuries | 3 (10) | 2 (7) |
| Riots | 0 | 1 (3) |
| Experienced event | 19 (66) | 24 (83) |
| Witnessed event | 10 (34) | 5 (17) |
| Injured in event | 4 (14) | 7 (24) |
| Any axis I comorbidity*: | 23 (79) | 19 (66) |
| Major depression | 21 (72) | 16 (55) |
| Panic disorder | 6 (21) | 6 (21) |
| Specific phobias | 2 (7) | 4 (14) |
| Alcohol or substance use disorder | 4 (14) | 4 (14) |
| Generalised anxiety disorder | 2 (7) | 1 (3) |
| Social phobia | 1 (3) | 1(3) |
| Other anxiety disorder | 2 (7) | 0 |
| Bulimia nervosa | 0 | 1 (3) |
| Any psychotropic drugs taken: | 18 (62) | 21 (72) |
| Antidepressants | 15 (52) | 20 (69) |
| Benzodiazepines | 4 (14) | 5 (17) |
| Hypnotics | 1 (3) | 1 (3) |
| Previous psychological treatment for trauma | 18 (62) | 13 (45) |
*Diagnostic and Statistical Manual of Mental Disorders, fourth edition.
The mean (standard deviation) number of treatment sessions was 7.8 (5.1), with 5.9 (2.5) sessions in the first 12 weeks and 2.0 (3.2) sessions thereafter. Twelve patients (21%) dropped out. The mean (standard deviation) numbers of sessions for those who dropped out and those who completed the study were 2.8 (1.2) and 9.2 (4.9).
Comparison between immediate treatment and waiting list groups at 12 weeks after randomisation
No significant differences were found between the groups at intake on scores for post-traumatic stress disorder, depression, and social functioning, but at 12 weeks the scores were significantly lower in the immediate therapy group (table 2). Paired t tests showed that at 12 weeks the waiting list group did not improve on any measure whereas the immediate therapy group improved on all measures (P<0.001).
Table 2.
Comparisons between immediate cognitive therapy group and waiting list group at 12 weeks after randomisation on primary and secondary outcome measures
| Variable | Immediate therapy group | Waiting list group | Mean (95% CI) difference between adjusted means* | P value | |||
|---|---|---|---|---|---|---|---|
| No | Mean (SD) | No | Mean (SD) | ||||
| All randomised patients: | |||||||
| Post-traumatic diagnosis scale | 29 | 21.8 (14.4) | 29 | 33.4 (11.6) | 9.6 (3.6 to 15.6) | 0.002 | |
| Beck depression inventory | 29 | 22.6 (14.1) | 29 | 32.7 (14.9) | 10.1 (4.8 to15.3) | <0.001 | |
| Sheehan disability scale | 29 | 5.3 (2.8) | 25 | 7.4 (2.6) | 1.3 (0.3 to 2.5) | 0.045 | |
| Completers†: | |||||||
| Post-traumatic diagnosis scale | 20 | 15.1 (9.9) | 25 | 33.1 (9.9) | 16.9 (10.9 to 23.0) | <0.001 | |
| Beck depression inventory | 20 | 17.9 (12.1) | 25 | 33.6 (15.0) | 13.2 (7.2 to 19.3) | <0.001 | |
| Sheehan disability scale | 20 | 4.2 (2.4) | 22 | 7.4 (2.8) | 2.4 (1.0 to 3.8) | <0.001 | |
*Based on one way analysis of covariance with scores before immediate therapy or wait as covariates.
†Patients who had at least six sessions of therapy or stopped therapy early because of noticeable improvement. For completers' analysis, waiting list group includes only patients who subsequently completed therapy.
Overall effectiveness of cognitive therapy
Table 3 shows the scores before and after treatment and at follow-up for all patients who received cognitive therapy. The immediate therapy and delayed therapy groups were combined as the latter group showed no improvement during wait and did not differ in improvement during treatment from the immediate therapy group. Therapists had the option of offering a few additional sessions after 12 weeks if clinically indicated. Twenty seven of 57 patients (47%) had additional sessions. The overall improvements in scores for post-traumatic stress disorder, depression, and social functioning were greater than those observed at 12 weeks. Paired t tests showed highly significant reductions between the scores before and after treatment. The observed effect sizes for post-traumatic stress disorder, depression, and social functioning for patients who completed the study were 1.74, 1.24, 1.08, 1.36, and 0.96, with respective values for the intention to treat sample of 1.25, 1.05, 0.97, 1.03, and 0.70. Most of the effect sizes were large and one was medium.12
Table 3.
Mean (standard deviation) scores before treatment, after treatment, and at follow-up (immediate and delayed cognitive therapy groups combined)
| Measure | Completers (n=45)* | All patients (n=57)† | ||||
|---|---|---|---|---|---|---|
| Before treatment | After treatment | Follow-up | Before treatment | After treatment | ||
| Post-traumatic diagnosis scale | 33.9 (10.1) | 14.6 (12.0) | 12.6 (11.1) | 34.3 (9.6) | 18.9 (14.5) | |
| Beck depression inventory | 33.3 (12.4) | 17.5 (13.0) | 14.9 (12.9) | 34.6 (12.1) | 20.8 (14.2) | |
| Work related disability | 7.8 (2.6) | 4.6 (3.3) | 3.6 (3.2) | 8.1 (2.4) | 5.3 (3.3) | |
| Social life related disability | 7.7 (2.5) | 4.1 (2.8) | 3.6 (3.1) | 7.7 (2.4) | 4.9 (3.0) | |
| Family related disability | 6.8 (2.7) | 4.1 (2.9) | 3.1 (3.0) | 6.8 (2.7) | 4.8 (3.0) | |
*43 patients completed at least one follow-up assessment. Post-treatment scores were carried forward for remaining two patients.
†Treatment drop-outs were not followed up. One patient showed substantial improvement during wait and declined subsequent treatment.
Maintenance of treatment gains
Only patients who completed treatment were offered follow-up appointments. Most attended at least one follow-up appointment and completed the outcome measures at that time. Those who did not were asked to return completed questionnaires by post. Overall 43 patients (96%) provided follow-up data. Table 3 shows the mean scores for the latest available follow-up (at four or 12 months for all but two patients, who were assessed at one month). Paired t tests comparing patients' scores after treatment and at follow-up indicated that treatment gains were well maintained. No significant difference was found in scores from after treatment to follow-up for post-traumatic stress disorder, depression, and social disability. Further significant improvement was evident at follow-up for work related disability (P<0.05) and family related disability scales (P<0.01). Effect sizes from before treatment to follow-up were large for post-traumatic stress disorder, depression, work related disability, social disability, and family related disability: 2.10, 1.45, 1.44, 1.46, and 1.30.
Predictors of treatment response
Percentage change in scores from before to after treatment for post-traumatic stress disorder showed that four patients had deteriorated (change <0%), four showed no change, and the remaining 49 (88%) showed various degrees of improvement: 1-24% (n=10), 25-49% (n=7), 50-74% (n=18), and 75-100% (n=14). Deterioration occurred more often in the wait period (38%) than in therapy (7%).
The presence or absence of a comorbid psychiatric disorder was not related to degree of improvement. This may have been because patients with comorbidities had significantly (P<0.05) more treatment sessions than those who did not: 8.6 v 5.9 sessions. Contrary to the findings of the Omagh bomb study2 degree of improvement was also unrelated to the presence or absence of enduring physical health problems as a consequence of the trauma. However, higher scores for depression at baseline (P<0.05) and a longer time since the trauma (P<0.05) were associated with less improvement.
A significant therapist effect was found when residualised gain scores were compared between therapists. Paired comparisons indicated significant differences (P<0.05) between each of the two therapists whose patients had improved most and one therapist whose patients had improved least.t tests indicated that the patients treated by these two sets of therapists did not differ in symptoms of initial post-traumatic stress disorder, initial depression, or time since the trauma, but patients treated by the therapist with poorer outcomes were significantly older (P<0.01) and had significantly fewer treatment sessions (P<0.01). The therapist effect remained significant (P<0.05) after patient age and number of treatment sessions were entered before the therapist's identity in a multiple regression analysis, indicating that the effect cannot be entirely explained by patient age or number of sessions.
The drop-out rate (20%) was higher than that in the two previous randomised controlled trials16 17 of cognitive therapy for post-traumatic stress disorder (0%-5%), both of which focused on non-terrorism related trauma. The case notes for the 12 patients who dropped out in the present trial were reviewed. Four were related to the unique context of Northern Ireland (threats to self or family linked to the civil conflict), four were associated with non-adherence to the therapy protocol in relation to imaginal reliving and behavioural experiments (not tackling beliefs, inadequate or inappropriate preparation), two were due to illness or trauma in the family, and two were unknown.
Discussion
Cognitive therapy is an effective treatment for post-traumatic stress disorder related to terrorism and other civil conflict. Patients allocated to immediate therapy showed significant and substantial reductions in the symptoms of post-traumatic stress disorder and depression and noticeable improvements in self reported work related disability, social disability, and family related disability. In contrast, patients allocated to a no treatment (waiting list) control condition showed no change.
The trial builds on and extends the findings of our uncontrolled study2 of cognitive therapy for post-traumatic stress disorder after the Omagh bomb. Both studies had minimal exclusion criteria and so are probably best conceptualised as effectiveness, rather than efficacy, studies. However, patients in the Omagh study were treated between three months and two years after the bombing, whereas patients in the current study were treated up to 33 years after trauma (median 6 years). Half had failed other treatments and many had high levels of concurrent depression.
A high proportion of patients in the present study had experienced multiple traumas. The Omagh bomb study2 focused on a single recent trauma, with only a few patients reporting a multiple trauma history. Similarly, the two randomised controlled trials16 17 of cognitive therapy for non-terrorism related post-traumatic stress disorder were restricted to patients who had experienced no more than two major traumas. In contrast, 59% of patients in the present study had experienced more than two traumas. Such patients improved as much as those who had experienced fewer traumas.
Although cognitive therapy was effective overall, the degree of improvement varied considerably. Analysis of this variability suggested several important lessons for future research and clinical practice. Firstly, the presence or absence of another psychiatric disorder did not influence the extent of a patient's reduction in symptoms of post-traumatic stress disorder. This was also reported in the Omagh bomb study.2 In that, as well as in the present study, therapists were given flexibility in the number of sessions that they could offer and were also allowed to use cognitive behaviour therapy techniques for other conditions requiring treatment. Patients with comorbidities received more sessions than those without comorbidities. This flexibility may have been responsible for the similarly good results of treatment in patients with comorbidities.
Secondly, unlike in the Omagh bomb study,2 ongoing physical problems resulting from the trauma did not predict poorer outcome. This may be because patients had longer to adapt to the problem. In addition, the team may have become better at dealing with this problem as a result of treating people affected by the Omagh bombing.
Thirdly, high levels of depression at intake were associated with poorer outcome. This finding was not observed in the Omagh bomb study2 or in the two randomised controlled trials16 17 of cognitive therapy for non-terrorism related post-traumatic stress disorder. However, the average scores for depression at intake were noticeably higher in the present study (average score 35) than in the Omagh bomb study (28) or the randomised controlled trials (19 and 24). Furthermore, mean scores at intake were as high as for published trials of severe major depression.18 We included behavioural activation in the treatment protocol to help reduce high levels of initial depression but it would seem that further development of the protocol is required for severely depressed patients. In our study, patients whose initial depression score was over 35 were particularly difficult to engage in the treatment, although notable exceptions occurred.
Fourthly, the drop-out rate in the present study (20%) was higher than those reported in the previous three studies of this cognitive therapy programme, but is not unusually high for trauma focused cognitive behaviour therapy programmes in general (average drop-out rate 23%, see NICE guidance,1 appendix 15a). Some patients seem to have dropped out of the study as a result of problems in running a treatment centre that serves communities where terrorism and other civil conflict related fears and suspicions are still present. However, other patients seem to have dropped out because of suboptimal delivery of the treatment protocol, in particular omitting to use cognitive techniques to tackle some patients' extreme beliefs about the adverse effects of imaginal reliving. This observation, and the finding of a therapist effect, suggests that greater attention may be needed to ensure that therapists dealing with chronic and severe post-traumatic stress disorders have sufficient training and ongoing supervision. The variation in outcome associated with different therapists (14%) was much larger than that observed in a randomised controlled trial of the same treatment (<1%), which was run in a university research clinic with therapists who had received extensive training to protocol.16
Recent NICE guidelines1 19 20 21 22 recommend cognitive behaviour therapy as a treatment of choice (alone or in conjunction with drugs) for many psychiatric disorders. In view of this guidance, and other recent developments, such as the Layard initiative,23 NHS trusts are increasingly likely to make cognitive behaviour therapy available to a variety of populations, some of which will not have been represented in the randomised controlled trials that led to a particular guideline. In such instances, NHS providers will wish to determine rapidly whether the treatment is effective in the new setting. When the Northern Ireland Centre for Trauma and Transformation was established, evidence was not available to indicate whether the positive results that have been observed with randomised controlled trials of cognitive behaviour for non-terrorism post-traumatic stress disorder would generalise to chronic, terrorist and civil conflict related violence. The centre took the decision to establish its treatment programme as a randomised controlled trial, with all referred adults with post-traumatic stress disorder being invited to participate in the trial. In this way it was possible to determine in a relatively short time that treatment does generalise to a different population and setting.
Limitations
Because of financial constraints the study relied on self report measures of post-traumatic stress disorder and associated symptoms. The absence of independent assessor ratings is a limitation. We do not think this is likely to have seriously compromised the study because in our two previous trials16 17 of cognitive therapy for post-traumatic stress disorder, and in several trials of cognitive behaviour therapy for other anxiety disorders,24 25 independent assessor ratings and self report scores have been similar. In addition, if there was any demand effect with respect to self reported symptoms it might be more in the direction of under-reporting of improvement at the end of the controlled phase of the study (12 weeks). This is because patients who had reported only modest improvement were offered further treatment.
Civil conflict occurs in a community context. In Northern Ireland the historic ceasefires that started in 1997 have had numerous effects on the community and there have been many positive community based initiatives, not least in Omagh, where the Northern Ireland Centre for Trauma and Transformation is located. Such societal changes applied equally to the waiting list and immediate therapy groups in our study and hence do not compromise the design. It is, however, our impression that recent community initiatives have had a role in helping people to come to terms with civil conflict related trauma as well as making treatment more acceptable. Evaluation of such influences was beyond the scope of our investigation.
What is already known on this topic
Trauma focused cognitive behaviour therapy and eye movement desensitisation and reprocessing therapy are recommended by NICE for non-terrorism related post-traumatic stress disorder
What this study adds
Cognitive therapy is effective in the treatment of post-traumatic stress disorder related to terrorism and other civil conflict
The therapists were Sean Collins, MD, KG, Susan McGandy, and John McLaren. Tracy McCrossan assisted with data collection. DMC is supported by the Wellcome Trust. We thank David Bolton, director of the Northern Ireland Centre for Trauma and Transformation, for supporting the research.
Contributors: All authors contributed to the design, execution, analysis, and writing up of the trial. MD is guarantor.
Funding: Northern Ireland Victims Liaison Unit.
Competing interests: None declared.
Ethical approval: This study was approved by the ethics committee of Queen's University of Belfast School of Medicine.
References
- 1.National Institute for Health and Clinical Excellence. Post-traumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care (clinical guideline 26). London: NICE, 2005
- 2.Gillespie K, Duffy M, Hackmann A, Clark DM. Community based cognitive therapy in the treatment of post-traumatic stress disorder following the Omagh bomb. Behav Res Ther 2002;40:345-57. [DOI] [PubMed] [Google Scholar]
- 3.First BM, Spitzer RL, Gibbon M, Williams JBW. User's guide for the structured clinical interview for DSM-IV axis I disorders: SCID-I clinician version Washington DC: American Psychiatric Press, 1995
- 4.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. J Trauma Stress 1995;8:75-90. [DOI] [PubMed] [Google Scholar]
- 5.Blanchard EB, Hickling EJ, Devineni T, Veazey CH, Galovski TE, Mundy E, et al. A controlled evaluation of cognitive behavioral therapy for posttraumatic stress in motor vehicle accident survivors. Behav Res Ther 2003;41:79-96. [DOI] [PubMed] [Google Scholar]
- 6.Pocock SJ. Clinical trials Chichester: Wiley, 1984
- 7.Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the posttraumatic diagnostic scale. Psychol Assess 1997;9:445-51. [Google Scholar]
- 8.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression New York: Guilford Press, 1979
- 9.Sheehan DV. The anxiety disease New York: Scribner, 1983
- 10.Beck AT, Steer RA, Brown GK. Beck depression inventory. 2nd ed. San Antonio: Psychological Corporation, 1996
- 11.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan disability scale. Int J Psychiatry Med 1997;27:93-105. [DOI] [PubMed] [Google Scholar]
- 12.Cohen J. Statistical power analysis for the behavioral sciences 2nd ed. Hillside, NJ: Lawrence Erlbaum Associates, 1988
- 13.Clark DM, Ehlers A. Posttraumatic stress disorder: from theory to therapy. In: Leahy RL, ed. Contemporary cognitive therapy New York: Guilford, 2004:141-60.
- 14.Ehlers A, Clark DM. A cognitive model of persistent posttraumatic stress disorder. Behav Res Ther 2000;38:319-45. [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association. Diagnostic and statistical manual of mental disorders 4th ed. Washington DC: APA, 1994
- 16.Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M, Herbert C, et al. A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Arch Gen Psychiatry 2003;60:1024-32. [DOI] [PubMed] [Google Scholar]
- 17.Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M. Cognitive therapy for post-traumatic stress disorder: development and evaluation. Behav Res Ther 2005;43:413-31. [DOI] [PubMed] [Google Scholar]
- 18.DeRubeis RJ, Gelfand LA, Tang TZ, Simons AD. Medications versus cognitive behavior therapy for severely depressed outpatients: mega-analysis of four randomized comparisons. Am J Psychiatry 1999;156:1007-13. [DOI] [PubMed] [Google Scholar]
- 19.National Institute for Health and Clinical Excellence. Anxiety: management of anxiety (panic disorder, with and without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care (clinical guideline 22). London: NICE, 2004 [PubMed]
- 20.National Institute for Health and Clinical Excellence. Depression: management of depression in primary and secondary care (clinical guideline 23). London: NICE, 2004
- 21.National Institute for Health and Clinical Excellence. Obsessive-compulsive disorder: core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder (clinical guideline 31). London: NICE, 2005 [PubMed]
- 22.National Institute for Health and Clinical Excellence. Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders (clinical guideline 9). London: NICE, 2004 [PubMed]
- 23.Layard R. The case for psychological treatment centres. BMJ 2006;332:1030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark DM, Salkovskis PM, Hackmann A, Middleton H, Anastasiades P, Gelder MG. A comparison of cognitive therapy, applied relaxation and imipramine in the treatment of panic disorder. Brit J Psychiatry 1994;164:759-69. [DOI] [PubMed] [Google Scholar]
- 25.Clark DM, Ehlers A, Hackmann A, McManus F, Fennell MJV, Waddington L, et al. Cognitive therapy versus exposure plus applied relaxation in social phobia: a randomised controlled trial. J Consult Clin Psychol 2006;74:568-78. [DOI] [PubMed] [Google Scholar]