Abstract
Thirty percent of acute liver graft rejection episodes are resistant to steroids. As interleukin-1 (IL-1) is an important target of steroid therapy, we examined the possible involvement of reduced sensitivity of IL-1 production to steroids or defective production of its antagonist, IL-1Ra. Patients were assessed during steroid-sensitive or -resistant rejection and 2 years later. In situ IL-1β and IL-1Ra expression was evaluated by immunohistochemistry; their production was assayed by enzyme-linked immunosorbent assay and the gene polymorphisms by reverse transcriptase-polymerase chain reaction on blood cells. Hepatic IL-1β and IL-1Ra expression were enhanced during rejection. IL-1 production and its inhibition by steroids were similar in steroid-responsive and steroid-resistant rejection. However, IL-1Ra production was lower in steroid-resistant than in steroid-responsive rejection, and this difference was still observed 2 years after rejection. IL-1β and IL-1Ra gene polymorphisms did not differ between patients with and without steroid resistance. Low IL-1Ra production is associated with steroid resistance of acute rejection and is due to a constitutional defect. The early identification of such patients might qualify them for stronger anti-rejection therapy, including IL-1Ra.
After liver transplantation, ∼50% of patients experience at least one episode of acute rejection. 1,2 This can be reversed in many cases by high doses of steroids, but 20 to 30% of patients do not respond and need additional therapy. 2-8
Interleukin-1 (IL-1) plays a key role in inflammatory and immune-mediated diseases. 9 During allograft rejection, IL-1 production precedes allograft dysfunction and injury. 10-12 Inhibition of IL-1 production is an important mechanism by which corticosteroids suppress immune response. 13-16
A natural antagonist of the IL-1 receptor (IL-1Ra) has recently been identified. 17-21 Soluble IL-1Ra can counteract the proinflammatory properties of IL-1 by competitively binding to the cell-surface receptor without inducing signal transduction. 22-25 Its role as an anti-inflammatory protein has been reported both in vitro and in vivo. 26-28 IL-1Ra production is also enhanced in stable human kidney graft recipients, and could thus be a key factor in early down-regulation of the allogeneic immune response. 29
The mechanisms of steroid resistance after organ transplantation are unknown. We explored the possible roles of a reduced sensitivity of IL-1 production to corticosteroid therapy, or defective IL-1Ra production. Our results indicate that both IL-1 production and its inhibition by corticosteroids are normal in patients whose acute rejection is steroid-resistant whereas, in contrast, IL-1Ra secretion is consistently reduced, pointing to a constitutional defect of IL-1Ra production in such patients.
Patients and Methods
Patients
The study population consisted of adult liver transplant recipients. After liver transplantation, patients were treated initially with corticosteroids, azathioprine, and cyclosporine. The dose of cyclosporine was adjusted to maintain whole-blood levels between 150 and 250 μg/L. Azathioprine was discontinued after 3 months, and steroids were tapered to 5 to 10 mg/day.
Acute rejection was defined by both biochemical and histological criteria, including at least two of the following: portal inflammatory infiltrate, endothelial inflammation, and biliary damage. Rejection was considered resistant when liver function tests improved by <50% of the highest values after three steroid boluses, in addition to persistent histological features of acute rejection on control liver biopsy. Episodes of acute rejection were initially treated for 3 days with a 1-g bolus of intravenous methylprednisolone daily. Cases of steroid-resistant acute rejection were treated with the monoclonal antibody OKT3 (Ortho Pharmaceutical Corp., Raritan, NJ).
Blood Sampling and Liver Biopsy
Blood and liver biopsy specimens were obtained, with their informed consent, from 29 patients with suspected rejection (Table 1) ▶ . Histological confirmation of acute rejection was obtained in 21 of these cases. Nine episodes responded to steroids whereas 12 resisted. The remaining eight patients had no histological evidence of acute rejection, either initially or during follow-up. Transplant recipients without acute rejection were assessed at approximately day 15, so as to be as close as possible to the median time of acute rejection in the two other groups. A portion of each biopsy specimen was immediately fixed and embedded in paraffin. Sections were stained with hematoxylin-eosin-safran for histological diagnosis. The remaining portion was snap-frozen in liquid nitrogen and stored at −80°C for immunohistochemistry. Blood and liver samples were obtained on days 14.5 ± 2.5, 15.1 ± 3.1, and 14.7 ± 2.8, respectively, from patients without rejection and patients with steroid-responsive and steroid-resistant rejection. In the latter two subgroups, samples were obtained before anti-rejection therapy. Blood and liver biopsy specimens were also obtained from the same patients, with their informed consent, during a routine work-up, a mean of 2 years posttransplantation. At that time, the patients were clinically stable and receiving minimal doses of steroids. Moreover, the total doses of steroids received since liver transplantation, as well as the cyclosporine dose and blood concentrations, were similar in the three groups of patients (Table 1) ▶ . Blood samples were also obtained, with their informed consent, from 44 healthy volunteers.
Table 1.
Patient Characteristics
| Steroid-responsive acute rejection (n = 9) | Steroid-resistant acute rejection (n = 12) | No rejection (n = 8) | |
|---|---|---|---|
| Age | 55.2 | 45.1 | 52.5 |
| (48–66) | (32–62) | (36–59) | |
| Sex | 4M, 5F | 5M, 7F | 3M, 5F |
| Initial pathology | |||
| Posthepatitic cirrhosis | 5 | 5 | 3 |
| Alcoholic cirrhosis | 2 | 3 | 2 |
| Others | 2 | 4 | 3 |
| Long-term assessment | |||
| Time after transplantation (years) | 2.75 | 2.5 | 2.75 |
| (2–4) | (2–4) | (2–4) | |
| Dose of steroids (mg/d) | 5.5 | 5.75 | 5.6 |
| (5–10) | (3–10) | (3–10) | |
| Total dose of steroids (mg) | 5,585 ± 955 | 5,175 ± 850 | 5,170 ± 835 |
| Cyclosporine dose (mg/d) | 166 ± 45 | 171 ± 51 | 144 ± 52 |
| Cyclosporine trough level (μg/l) | 124 ± 35 | 112 ± 41 | 131 ± 44 |
Detection of IL-1β and IL-1Ra by Immunohistochemistry
Five-micrometer cryostat sections of each biopsy specimen were mounted on polysine-coated slides (CML-CBE, Nemours, France). Serial slides were air-dried, fixed in acetone, and stored at −20°C until staining. Cytokine expression was tested using an indirect immunoenzymatic method. 30 Anti-IL-1β monoclonal antibody (Genzyme, Cambridge, MA) and anti-IL-1Ra polyclonal antibody (Genzyme) were used at a dilution of 1:20. In positive controls, some blood mononuclear cells activated by lipopolysaccharide (LPS) (1 μg/ml) (Sigma Chemical Company, St Louis, MO) expressed IL-1β and IL-1Ra, whereas no inactivated cells expressed IL-1β and IL-1Ra (data not shown). Cryostat sections were refixed in acetone then incubated with Tris-buffered saline, 20% human AB serum (Sanofi Diagnostics Pasteur, Marnes La Coquette, France), then with the primary antibody. Slides treated with the polyclonal primary antibody (anti-IL-1Ra) were incubated with 1:20 mouse anti-rabbit immunoglobulin (DAKO, Dakopatts A/S, Glostrup, Denmark). All slides were then incubated with 1:20 rabbit anti-mouse immunoglobulin (DAKO) and subsequently with alkaline phosphatase-anti-alkaline phosphatase complexes (DAKO). Alkaline phosphatase activity was revealed after incubation in fast-red TR and napthol-phosphate solution containing levamisole. 31 The slides were counterstained with hematoxylin. In negative controls, the primary antibody was replaced by an irrelevant antibody at the same dilution. Anti-CD3 (DAKO) was used as a positive control.
Quantification of Immunohistochemical Staining
The slides were examined by two of the authors (FC and SB), who were blinded to the pathological diagnoses. Positive cells were counted on each slide in a portal and a lobular field at a magnification of ×200. The number of positive cells recorded was a consensus between the two observers.
Assay of IL-1β and IL-1Ra by Enzyme-Linked Immunosorbent Assay (ELISA) in Cultures of Blood Cells
Five milliliters of heparinized blood were obtained from each patient, diluted 1:5 in RPMI 1640 medium containing l-glutamine and penicillin/streptomycin (Gibco-BRL, Cergy-Pontoise, France), then cultured for 24 hours with or without LPS (1 μg/ml), 21 with various concentrations of dexamethasone (0 to 10−5 mol/L). IL-1β and IL-1Ra were measured in duplicate in 24-hour supernatants of blood cells, using an ELISA kit (R&D System Europe Ltd., Abingdon, UK). The detection limits were 4 pg/ml IL-1β and 31 pg/ml IL-1Ra, and the within-run variation was <5% in each case.
Analysis of IL-1Ra and IL-1β Gene Polymorphisms
Twenty-four patients (nine with steroid-responsive, nine with steroid-resistant acute rejection, and six with no rejection) were investigated for IL-1Ra and IL-1β gene polymorphisms. Genomic DNA was isolated from blood by the salting-out method. 32 IL-1Ra exon 2 polymorphism was analyzed as previously described. 33 Oligonucleotides 5′-CTCAGCAACACTCCTAT-3′ and 5′-TCCTGGTCTGCAGGTAA-3′ were used as primers. 34 The polymerase chain reaction products were separated by electrophoresis on 2% agarose gel and stained with ethidium bromide. Allele 1 (four repeats) was 410 bp long and allele 2 (two repeats) was 240 bp long. The region containing the AvaI polymorphic site at position −511 of the IL-1β gene was amplified by polymerase chain reaction. The oligonucleotides 5′-TGGCAATTGATCTGGTTCATC-3′ and 5′-GTTTAGGAATCTTCCCACTT-3′ flanking this region were used as primers. 35 Polymerase chain reaction products were digested with 6 U of AvaI at 37°C for 3 hours. Fragments were analyzed on 2% agarose gel. This revealed products of 190 bp + 114 bp (allele 1) and 304 bp (allele 2). Position +3953 within exon 5 of the IL-1β gene exhibited single bp polymorphism. 36 The polymorphic region containing the TaqI restriction site was amplified using the following primers: 5′-GTTGTCATCAGACTTTGACC-3′ and 5′-TTCAGTTCATATGGACCAGA-3′. TaqI digestion of the 249-bp fragments resulted in products that either remained intact (allele 2) or were cut into two fragments of 135 bp and 114 bp (allele 1).
Statistical Analysis
The immunohistochemical and ELISA results are expressed as means ± SE. Statview IV software (Abacus Concepts, Berkeley, CA) running on a Macintosh computer was used for statistical analyses (analysis of variance followed by Fisher’s exact test).
Results
Immunochemical IL-1β Expression at the Time of Rejection
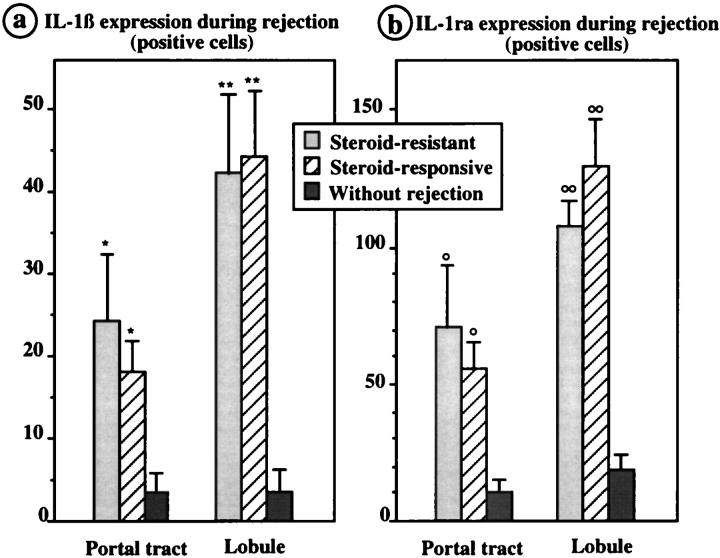
Positive cells were rare in liver grafts without rejection, whereas they were abundant during acute rejection (P < 0.03 in the portal tract and P < 0.01 in the lobule), but there was no difference between patients with steroid-responsive and steroid-resistant acute rejection (Figure 1a) ▶ . Stained cells were mostly endothelial, Kupffer, and inflammatory cells, infiltrating the sinusoids and portal tracts.
Figure 1.
Semiquantitative analysis of IL-1β (a) and IL-1Ra (b) expression (number of positive cells) in liver grafts, assessed in the portal tracts and lobules. The numbers of positive cells for IL-1β and IL-1Ra were significantly higher during rejection than in patients without rejection, in both the lobule and portal tract (*, P < 0.03; **, P < 0.01; °, P < 0.05; °°, P < 0.02 versus patients without rejection). In contrast, there was no difference between patients with steroid-responsive and steroid-resistant acute rejection.
Immunochemical IL-1Ra Expression at the Time of Rejection
Positive cells were rare in liver transplants without acute rejection (Figure 2A) ▶ and abundant in both steroid-responsive (Figure 2B) ▶ and steroid-resistant acute rejection (Figure 2C) ▶ . The number of cells expressing IL-1Ra was higher in patients with acute rejection than without acute rejection (P < 0.05 in the portal tract and P < 0.02 in the lobule), but there was no difference in this respect between steroid-responsive and -resistant acute rejection (Figure 1b) ▶ . Stained cells were Kupffer and inflammatory cells infiltrating the sinusoids and portal tracts.
Figure 2.
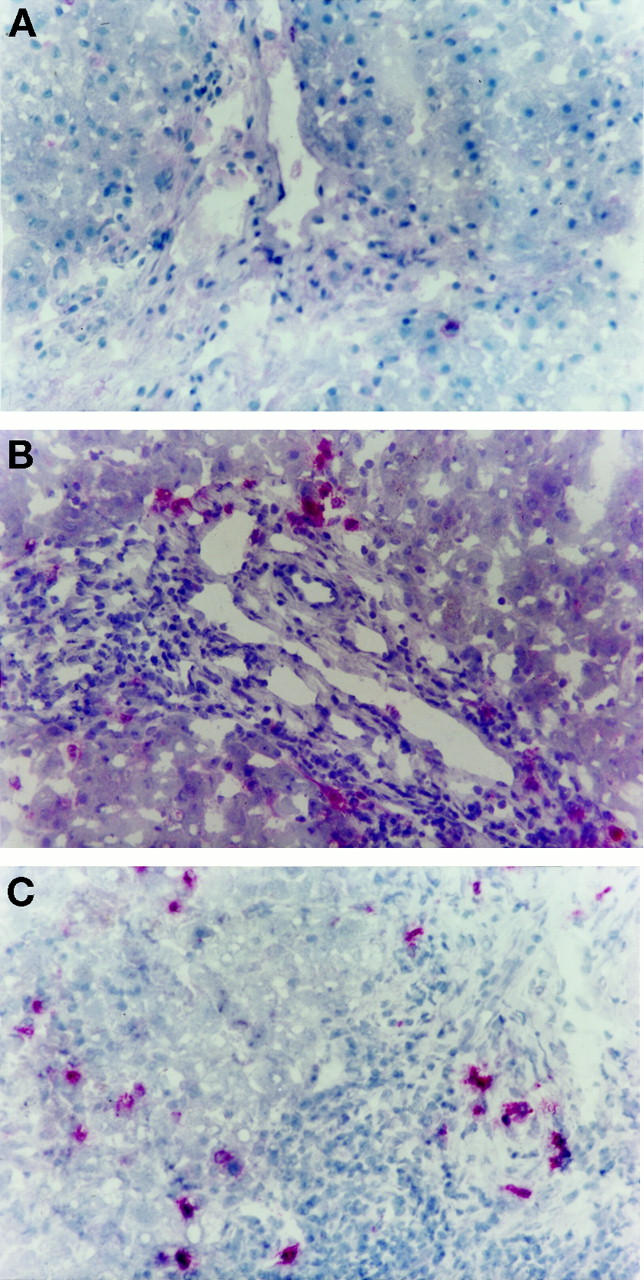
Indirect immunohistochemical staining of cryostat liver biopsy sections. IL-1Ra expression was evaluated in liver transplants without rejection (A), during steroid-responsive acute rejection (B), and during steroid-resistant acute rejection (C). Original magnification, ×200.
IL-1β and IL-1Ra Expression after 2 Years
Few hepatic cells expressed IL-1β and IL-1Ra, with no significant difference between the three groups of patients (data not shown).
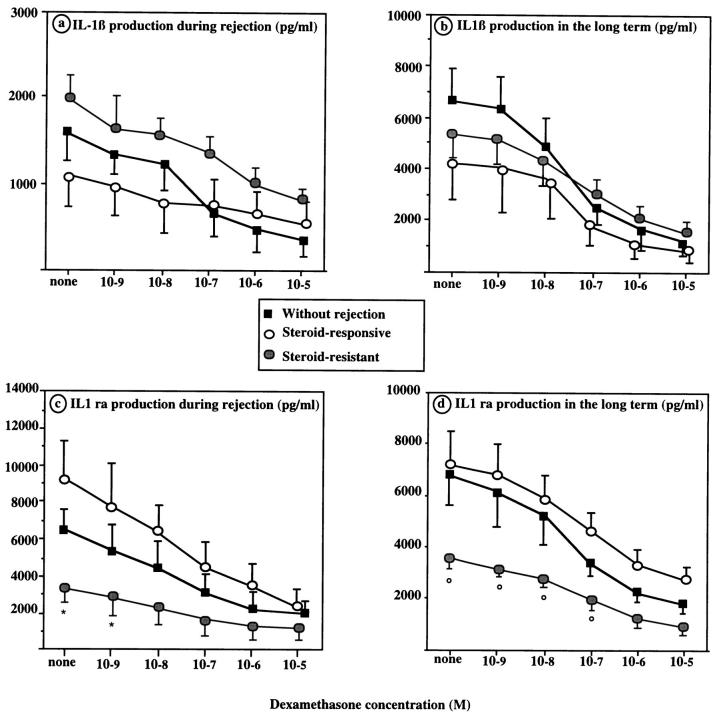
ELISA IL-1β Levels at the Time of Rejection
IL-1β concentrations were low in the supernatants of unstimulated blood cells from patients without acute rejection, with steroid-responsive and with steroid-resistant acute rejection (46 ± 29 pg/ml, 46 ± 29 pg/ml, and 64 ± 46 pg/ml, respectively). After LPS stimulation, the corresponding IL-1β concentrations rose to 1,634 ± 724 pg/ml, 1,027 ± 612 pg/ml, and 1,959 ± 264 pg/ml (NS). IL-1β production was inhibited by dexamethasone in a concentration-dependent manner and to a similar extent in each group (Figure 3a) ▶ .
Figure 3.
IL-1β and IL-1Ra secretion by blood mononuclear cells of liver transplant recipients without rejection, during steroid-responsive acute rejection, and during steroid-resistant acute rejection. a: IL-1β secretion at the time of rejection. b: IL-1β secretion 2 years after transplantation. c: IL-1Ra secretion at the time of rejection. d: IL-1Ra secretion 2 years after transplantation. IL-1Ra secretion was significantly lower during steroid-resistant than during steroid-responsive acute rejection (*, P < 0.01). In the long term, IL-1Ra secretion was lower in patients with a past history of steroid-resistant rejection than in the two other groups (°, P < 0.01).
ELISA IL-1β Levels after 2 Years
Supernatants of unstimulated cells contained 1,824 ± 394 pg/ml, 1,002 ± 583 pg/ml, and 1,422 ± 417 pg/ml IL-1β, respectively, in patients without rejection and those with steroid-responsive and -resistant acute rejection (NS). After LPS stimulation, the corresponding IL-1β concentrations were 6,728 ± 1,497 pg/ml, 4,155 ± 1,231 pg/ml, and 5,149 ± 1,098 pg/ml (NS). IL-1β production was inhibited by dexamethasone to a similar extent in each group (Figure 3b) ▶ .
ELISA IL-1Ra Levels at the Time of Rejection
IL-1Ra concentrations were 565 ± 275 pg/ml, 2,012 ± 1,486 pg/ml, and 1,034 ± 496 pg/ml, respectively, in the supernatants of unstimulated cells from patients without rejection and those with steroid-responsive or steroid-resistant rejection. After stimulation, the corresponding IL-1Ra concentrations rose to 6,461 ± 1,386 pg/ml, 9,010 ± 2,119 pg/ml, and 3,129 ± 349 pg/ml (P < 0.01 between the steroid-responsive and steroid-resistant acute rejection groups). Dexamethasone inhibited LPS-stimulated IL-1Ra production to a similar extent in the three groups (Figure 3c) ▶ .
ELISA IL-1Ra Levels after 2 Years
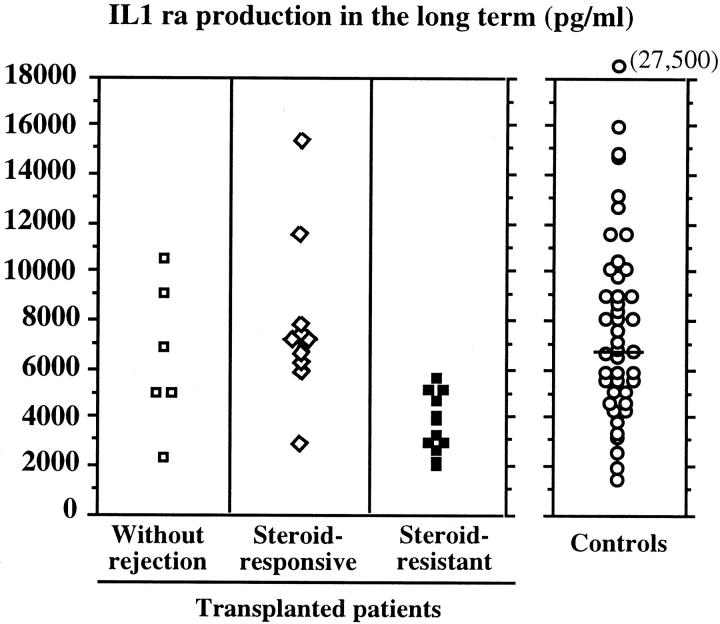
IL-1Ra concentrations were 3,573 ± 573 pg/ml, 3,156 ± 798 pg/ml, and 1,934 ± 250 pg/ml in the supernatants of unstimulated cells from patients without rejection and those with steroid-responsive and -resistant acute rejection, respectively. After stimulation, the corresponding IL-1Ra concentrations rose to 6,331 ± 1,210 pg/ml, 7,269 ± 1,301 pg/ml, and 3,661 ± 366 pg/ml (Figure 3d) ▶ . IL-1Ra secretion was inhibited by corticosteroids to a similar extent in the three groups of patients. IL-1Ra secretion was lower in patients with a history of steroid-resistant rejection than in the other two groups, both in the absence and presence of dexamethasone (P < 0.01). In contrast, IL-1Ra secretion did not significantly differ between patients with a past history of acute rejection (5,208 ± 701 pg/ml) and those with no such history (6,331 ± 121 pg/ml). Taking a cut-off value of 5,750 pg/ml, eight of the nine patients with steroid-responsive acute rejection exhibited IL-1Ra levels above this value, whereas all 12 patients with resistant acute rejection had values below the cut-off (Figure 4) ▶ .
Figure 4.
LPS-stimulated production of IL-1Ra by blood mononuclear cells from liver transplant recipients without rejection, during steroid-responsive acute rejection, and during steroid-resistant acute rejection (2 years after transplantation), and from healthy volunteers.
Analysis of IL-1β and IL-1Ra Gene Polymorphisms
The distribution of IL-1β and IL-1Ra genotypes and corresponding allelic frequencies were similar to those previously reported (Table 2) ▶ . None of the alleles examined was associated with the resistance of acute rejection to steroid therapy in the patients tested. In addition, the association of IL-1Ra allele 2 with IL-1β −511 allele 2 or IL-1β +3,953 allele 2 had no effect on steroid resistance (Table 3) ▶ .
Table 2.
IL-1Ra and IL-1β Genotypes (Base Exchange Polymorphisms at Positions −511 and +3,953) and the Corresponding Allele Frequencies
| Genotype | Allele | ||||
|---|---|---|---|---|---|
| 1.1 | 1.2 | 2.2 | 1 | 2 | |
| IL-1Ra | |||||
| No rejection (n = 6) | 5 | 1 | 0 | 0.91 | 0.09 |
| Steroid-responsive acute rejection (n = 9) | 7 | 1 | 1 | 0.83* | 0.17 |
| Steroid-resistant acute rejection (n = 9) | 5 | 4 | 0 | 0.77*† | 0.23 |
| IL-1β (−511) | |||||
| No rejection (n = 6) | 5 | 0 | 1 | 0.83 | 0.17 |
| Steroid-responsive acute rejection (n = 9) | 6 | 2 | 1 | 0.78* | 0.22 |
| Steroid-resistant acute rejection (n = 9) | 4 | 4 | 1 | 0.67*† | 0.33 |
| IL-1β (+3,953) | |||||
| No rejection (n = 6) | 2 | 2 | 2 | 0.50 | 0.50 |
| Steroid-responsive acute rejection (n = 9) | 5 | 2 | 2 | 0.67* | 0.33 |
| Steroid-resistant acute rejection (n = 9) | 4 | 3 | 2 | 0.61*† | 0.39 |
*NS versus patients without rejection.
†NS versus patients with steroid-responsive acute rejection.
Table 3.
The Effect of IL-1Ra and IL-1β Genotypes on Steroid Response
| Genotype | Steroid-responsive acute rejection (n = 9) | Steroid-resistant acute rejection (n = 9) |
|---|---|---|
| IL-1Ra-2+ | 2 | 4 |
| IL-1Ra-2− | 7 | 5 |
| IL-1Ra-2+/IL-1β-511-2+ | 1 | 2 |
| IL-1Ra-2−/IL-1β-511-2+ | 2 | 3 |
| IL-1Ra-2+/IL-1β-511-2− | 1 | 2 |
| IL-1Ra-2−/IL-1β-511-2− | 5 | 2 |
| IL-1Ra-2+/IL-1β+3,953-2+ | 0 | 2 |
| IL-1Ra-2−/IL-1β+3,953-2+ | 4 | 3 |
| IL-1Ra-2+/IL-1β+3,953-2− | 2 | 2 |
| IL-1Ra-2−/IL-1β+3,953-2− | 3 | 2 |
ELISA IL-1Ra Levels in Ungrafted Controls
To determine whether the low IL-1Ra levels observed in transplant patients with steroid resistance were also found in the general population, IL-1Ra production was measured in blood samples from 44 healthy volunteers. Large interindividual differences were found in IL-1Ra secretion (Figure 4) ▶ . Low IL-1Ra production (<5,750 pg/ml) by LPS-stimulated mononuclear cells, similar to that found in the steroid-resistant acute rejection group, was observed in 34% of healthy volunteers.
Discussion
This is the first report suggesting that the steroid resistance of acute rejection is associated with low levels of IL-1Ra production by blood cells.
In all of the patients with acute rejection, whatever their response to steroid therapy, a high level of IL-1β production was found by immunohistochemistry on liver biopsies and by ELISA in the supernatants of stimulated blood cells. These data are in agreement with those previously obtained by reverse transcriptase-polymerase chain reaction in the same clinical setting. 11,12 Because steroid-resistant and steroid-responsive acute rejection did not differ in terms of IL-1β production by blood mononuclear cells, a defect in IL-1β sensitivity to steroid therapy is probably not involved in steroid resistance, although a lower sensitivity of hepatocytes and sinusoidal endothelial cells to steroids could not be excluded.
IL-1Ra expression in the liver grafts was also increased in patients with acute rejection relative to patients without rejection. To our knowledge, this is the first clear evidence that hepatic IL-1Ra production is enhanced during acute liver graft rejection. This IL-1Ra overexpression may result from an increased stimulation through the local production of cytokines, and may restrict the rejection process by inhibiting the effects of IL-1. 37,38 In those patients, IL-1Ra was only expressed by the inflammatory cells infiltrating the sinusoids and portal tracts. In our study, hepatocytes, which may secrete IL-1Ra, especially when stimulated by IL-1 and IL-6, 37 were consistently found to be negative for IL-1Ra expression by immunohistochemistry. It is noteworthy that the number of the infiltrating cells expressing IL-1Ra was similar during steroid-responsive and -resistant episodes of acute rejection. In contrast, IL-1Ra production by blood cells was lower in steroid-resistant than in steroid-sensitive patients, both at the time of acute rejection and throughout the long term.
To determine whether this difference reflected the existence of high and low IL-1Ra producers within the general population, we compared LPS-stimulated IL-1Ra production by blood cells from the transplant patients with that of healthy volunteers, and found the same broad range of responses in both groups. All steroid-resistant patients exhibited IL-1Ra levels <5,750 pg/ml, as did ∼30% of the healthy volunteers, who may therefore be at risk of steroid resistance. It remains to be determined if this distinction between weak and strong IL-1Ra producers could be used to predict an increased risk of steroid resistance in other transplant settings, as well as in other inflammatory or autoimmune diseases.
We then investigated whether the variability in IL-1Ra production could be explained by the recently described IL-1β and IL-1Ra gene polymorphisms. Indeed, certain IL-1β or IL-1Ra alleles are associated with severe forms of inflammatory or autoimmune diseases. 35,36,39-43 In addition, allele 2 of the IL-1Ra gene is associated with higher concentrations of the molecule in plasma. 34 We found no link between the known IL-1β and IL-1Ra polymorphisms and steroid resistance. The number of patients tested was however small, and this result needs to be confirmed. Other polymorphisms of IL-1Ra gene should also be investigated.
The mechanisms of steroid resistance are still poorly understood. In steroid-resistant asthma, neither altered steroid metabolism nor an abnormality of the hypothalamic-pituitary-adrenal axis seems to be involved. 44-47 Impaired liver graft function might result in reduced conversion of methylprednisolone to its active form, without a corresponding reduction in its rate of elimination. 48 However, we found no difference in the conversion rate of prednisolone to its active form among our patients (V. Furlan, manuscript in preparation). A relative insensitivity of T lymphocytes to corticosteroids has also been suspected. 46,47,49,50 The present study suggests that the clinical resistance of acute liver rejection to steroids is at least partly due to an IL-1Ra defect. Clinical steroid resistance was probably not related to a stronger inhibition of IL-1Ra production by steroids in the clinically resistant group, as the inhibition curves ran parallel in all groups. The use of the term “steroid resistance” in the transplant setting may thus be misplaced, as it does not correspond to true steroid resistance at the cellular level. IL-1 production is incompletely inhibited by corticosteroids during acute rejection, as substantial amounts of IL-1 can be found in the graft. IL-1Ra may prevent residual IL-1 from binding to its receptor. The inability of some individuals to mount an adequate IL-1Ra response may result in the so-called steroid resistance. Clinical resistance to steroids is probably potentiated by the inhibitory effect of steroids on IL-1Ra production.
This study defines a new concept in the pathophysiology of steroid resistance and suggests IL-1Ra as a potential treatment. Indeed, IL-1Ra could be used to treat steroid-resistant acute rejection in humans, as in experimental models. 51-53 The use of IL-1Ra to treat rheumatoid arthritis and graft-versus-host disease has proved to be safe and effective. 54-56 Moreover, constitutively low IL-1Ra production can be detected before transplantation, so that IL-1Ra could be included in the immunosuppressive regimen of such patients.
Acknowledgments
We thank Mrs. Voltoury and the Blood Transfusion Center at Hôpital Saint-Vincent de Paul (Paris) (Etablissement de Transfusion Sanguine de l’AP-HP), who collected the blood samples from normal volunteers; François Durand and Christophe Duvoux, who collected samples from liver transplant recipients; and Pierre Thomopoulos, Françoise Russo-Marie, and David Young for their help in preparing the manuscript.
Footnotes
Address reprint requests to Yvon Calmus, Service de Chirurgie, Hôpital Cochin, 75674 Paris Cedex 14, France. E-mail: yvon.calmus@cch.ap-hop-paris.fr.
Supported by a grant from Novartis Pharma France. F. C. is the recipient of a fellowship from the Association Française pour l’Etude du Foie.
References
- 1.Adams DH, Neuberger JM: Patterns of graft rejection following liver transplantation. J Hepatol 1990, 10:113-119 [DOI] [PubMed] [Google Scholar]
- 2.Klintmalm G, Nery J, Husberg B, Gonwa T, Tillery G: Rejection in liver transplantation. Hepatology 1989, 10:978-985 [DOI] [PubMed] [Google Scholar]
- 3.Wiesner R, Wahlstrom H, Gores G, Kamath P, Krom R: Early cellular rejection treated with high-dose intravenous corticosteroid therapy is associated with a decrease in the incidence of steroid-resistant rejection and graft failure from rejection. Transplant Proceed 1993, 25:1791-1793 [PubMed] [Google Scholar]
- 4.Adams D, Neuberger J: Treatment of acute rejection. Semin Liver Dis 1992, 12:80-87 [DOI] [PubMed] [Google Scholar]
- 5.Wagner F, Reichenspurner H, Uberfuhr P, Kur F, Kaulbach H, Meuser B, Ziegler U, Reichart B: How successful is OKT3 rescue therapy for steroid-resistant acute rejection episodes after heart transplantation? J Heart Lung Transplant 1994, 13:438-442 [PubMed] [Google Scholar]
- 6.Portela D, Patel R, Larson-Keller J, Ilstrup D, Wiesner R, Steers J, Krom R, Paya C: OKT3 treatment for allograft rejection is a risk factor for cytomegalovirus disease in liver transplantation. J Infect Dis 1995, 171:1014-1018 [DOI] [PubMed] [Google Scholar]
- 7.Hosenpud J, Norman D, Pantely G, Cobanoglu A, Starr A: OKT3-induced hypotension in heart allograft recipients treated for steroid-resistant rejection. J Heart Transplant 1989, 8:159-165 [PubMed] [Google Scholar]
- 8.Freese DK, Snover DC, Sharp HL, Gross CR, Kay Savick S, Payne WD: Chronic rejection after liver transplantation: a study of clinical, histopathological and immunological features. Hepatology 1991, 13:882-891 [PubMed] [Google Scholar]
- 9.Dinarello C: Biologic basis for interleukin-1 in disease. Blood 1996, 87:2095-2147 [PubMed] [Google Scholar]
- 10.Salom R, Maguire J, Hancock W: Endothelial activation and cytokine expression in human acute cardiac allograft rejection. Pathology 1998, 30:24-29 [DOI] [PubMed] [Google Scholar]
- 11.Mannon R, Sundar S, Sanfilippo F, Coffman T: Alterations in renal interleukin-1 production during kidney transplant rejection in the rat. The effects of high-dose methylprednisolone. Transplantation 1993, 56:1157-1162 [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann MW, Wonigeit K, Steinhoff G, Herzbeck H, Flad HD, Pichlmayr R: Production of cytokines (TNF-alpha, IL-1-beta) and endothelial cell activation in human liver allograft rejection. Transplantation 1993, 55:329-335 [DOI] [PubMed] [Google Scholar]
- 13.Barnes P, Adcock I: Anti-inflammatory actions of steroids: molecular mechanisms. Trends Pharmacol Sci 1993, 14:436-441 [DOI] [PubMed] [Google Scholar]
- 14.Kern J, Lamb R, Reed J, Daniele R, Nowell P: Dexamethasone inhibition of interleukin 1 beta production by human monocytes. Post-transcriptional mechanisms. J Clin Invest 1988, 81:237-244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang D-M, Baptiste P, Schur P: The effect of antirheumatic drugs on interleukin 1 (IL-1) activity and IL-1 and IL-1 inhibitor production by human monocytes. J Rheumatol 1990, 17:1148-1157 [PubMed] [Google Scholar]
- 16.Bleeker M, Netea M, Kullberg B, Van der Ven-Jongekrijg J, Van des Meer J: The effects of dexamethasone and chlorpromazine on tumour necrosis factor-alpha, interleukin-1 beta, receptor antagonist and interleukin-10 in human volunteers. Immunology 1997, 91:548-552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eisenberg S, Evans R, Arend W, Verderber E, Brewer M, Hannum C, Thompson R: Primary structure and functional expression from complementary DNA of human interleukin-1 receptor antagonist. Nature 1990, 343:341-346 [DOI] [PubMed] [Google Scholar]
- 18.Arend W, Joslin F, Thompson R, Hannum C: An IL-1 inhibitor from human monocytes. Production and characterization of biologic properties. J Immunol 1989, 143:1851-1858 [PubMed] [Google Scholar]
- 19.Carter D, Diebel M, Dunn J, Tomich C-S, Laborde A, Slightom J, Berger A, Bienkowski M, Sun F, McEwan R, Harris P, Yem A, Waszak G, Chosay J, Sieu L, Hardee M, Zurcher-Neely H, Reardon I, Heinrikson R, Truesdell S, Shelly J, Eessalu T, Taylor B, Tracy D: Purification, cloning, expression, and biological characterization of an interleukin-1 receptor antagonist protein. Nature 1990, 344:633-637 [DOI] [PubMed] [Google Scholar]
- 20.Hannum C, Wilcox C, Arend W, Joslin F, Dripps D, Heimdal P, Armes L, Sommer A, Eisenberg S, Thompson R: Interleukin-1 receptor antagonist activity of an interleukin-1 inhibitor. Nature 1990, 344:336-341 [DOI] [PubMed] [Google Scholar]
- 21.Dinarello C: Interleukin-1 and interleukin-1 antagonism. Blood 1991, 77:1627-1652 [PubMed] [Google Scholar]
- 22.Granowits E, Clark B, Mancilla J, Dinarello C: Interleukin-1 receptor antagonist competitively inhibits the binding of interleukin-1 to the type II interleukin-1 receptor. J Biol Chem 1991, 266:14147-14150 [PubMed] [Google Scholar]
- 23.Seckinger P, Williamson K, Dayer J, McDonald H: A urine inhibitor of interleukin-1 activity that blocks ligand binding. J Immunol 1987, 139:1546-1553 [PubMed] [Google Scholar]
- 24.Dripps D, Brandhuber J, Thompson R, Eisenberg S: Interleukin-1 (IL-1) receptor antagonist binds to the 80-kDa IL-1 receptor but does not initiate IL-1 signal transduction. J Biol Chem 1991, 266:10331-10336 [PubMed] [Google Scholar]
- 25.Lukacs N, Kunkel S, Burdick M, Lincoln P, Strieter R: Interleukin-1 receptor antagonist blocks chemokine production in the mixed lymphocyte reaction. Blood 1993, 82:3668-3674 [PubMed] [Google Scholar]
- 26.Arend W, Malyak M, Guthridge C, Gabay C: Interleukin-1 receptor antagonist: role in biology. Annu Rev Immunol 1998, 16:27-55 [DOI] [PubMed] [Google Scholar]
- 27.Cominelli F, Nast C, Clark B, Schindler R, Lerena R, Eysselem V, Thompson R, Dinarello C: Interleukin 1 (IL-1) gene expression, synthesis, and effect of specific IL-1 receptor blockade in rabbit immune complex colitis. J Clin Invest 1990, 86:972-980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dinarello C, Thompson R: Blocking IL-1: interleukin-1 receptor antagonist in vivo and in vitro. Immunol Today 1991, 19:404-410 [DOI] [PubMed] [Google Scholar]
- 29.Oliveira J, Xavier P, Neto S, Mendes A, Guerra L: Monocytes-macrophages and cytokines/chemokines in fine-needle aspiration biopsy cultures. Enhanced interleukin-1 receptor antagonist in rejection-free kidney transplant patients. Transplantation 1997, 63:1751-1756 [DOI] [PubMed] [Google Scholar]
- 30.Cordell JL, Falini B, Erber WN, Ghosh AK, Abdulaziz A, MacDonald S, Pulfpord KAF, Stein H, Mason DY: Immunoenzymatic labelling of monoclonal antibodies using immune complex of alkaline phosphatase and monoclonal anti-alkaline phosphatase. J Histochem Cytochem 1984, 32:219-229 [DOI] [PubMed] [Google Scholar]
- 31.Gaulard P, Kanavaros P, Farcet J, Rocha F, Haioun C, Divine M, Reyes F, Zafrani E: Bone marrow histologic and immunohistochemical findings in peripheral T-cell lymphoma: a study of 38 cases. Hum Pathol 1991, 22:331-338 [DOI] [PubMed] [Google Scholar]
- 32.Miller K, Anderson J: Human monocyte/macrophage activation and interleukin 1 generation by biomedical polymers. J Biomed Mater Res 1988, 22:713-731 [DOI] [PubMed] [Google Scholar]
- 33.Tarlow J, Blakemore A, Lennard A, Solari R, Hughes H, Strenkasserer A, Duff G: Polymorphism in human IL-1 receptor antagonist gene intron 2 is caused by variable numbers of an 86-bp tandem repeat. Hum Genet 1993, 91:403-404 [DOI] [PubMed] [Google Scholar]
- 34.Hurme M, Santtila S: IL-1 receptor antagonist (IL-1Ra) plasma levels are co-ordinately regulated by both IL-1Ra and IL-1beta genes. Eur J Immunol 1998, 28:2598-2602 [DOI] [PubMed] [Google Scholar]
- 35.Di Giovine F, Takhsh E, Blakemore A, Duff G: Single base polymorphism at -511 in the human interleukin-1 beta gene (IL1 beta). Hum Mol Genet 1992, 1992:450-451 [DOI] [PubMed] [Google Scholar]
- 36.Pociot F, Molvig J, Wogesen L, Worsaae H, Nerup J: A TaqI polymorphism in the human interleukin-1 beta (IL-1 beta) gene correlates with IL-1 beta secretion in vitro. Eur J Clin Invest 1992, 22:396-402 [DOI] [PubMed] [Google Scholar]
- 37.Gabay C, Smith M, Eidlen D, Arend W: IL-1 receptor antagonist (IL-1Ra) is an acute-phase protein. J Clin Invest 1994, 99:2930-2940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arend W, Dayer J: Inhibition of the production and effects of interleukin 1 and tumor necrosis factor alpha in rheumatoid arthritis. Arthritis Rheum 1995, 38:151-160 [DOI] [PubMed] [Google Scholar]
- 39.Santtila S, Savinainen K, Hurme M: Presence of the IL-1Ra allele 2 (IL1RN*2) is associated with enhanced IL-1 beta production in vitro. Scand J Immunol 1998, 47:195-198 [DOI] [PubMed] [Google Scholar]
- 40.Chang D: Interleukin-1 and interleukin-1 receptor antagonist in systemic lupus erythematosus. Immunol Invest 1997, 26:649-659 [DOI] [PubMed] [Google Scholar]
- 41.Andus T, Daig R, Volg D, Aschenbrenner E, Lock G, Hollerbach S, Kollinger M, Scholmerich J, Gross V: Imbalance of the interleukin 1 system in colonic mucosa-association with intestinal inflammation and interleukin 1 receptor antagonist genotype 2. Gut 1997, 41:651-657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heresbach D, Alizadeh M, Dabadie A, Le Berre N, Colombel J, Yaouanq J, Bretagne J, Semana G: Significance of interleukin-1beta and interleukin-1 receptor antagonist genetic polymorphism in inflammatory bowel diseases. Am J Gastroenterol 1997, 92:1164-1169 [PubMed] [Google Scholar]
- 43.Roussomoustakaki M, Satsangi J, Welsh K, Louis E, Fanning G, Targan S, Landers C, Jewell D: Genetic markers may predict disease behavior in patients with ulcerative colitis. Gastroenterology 1997, 112:1845-1853 [DOI] [PubMed] [Google Scholar]
- 44.Lane S, Atkinson B, Swaminathan R, Lee T: Hypothalamic-pituitary-adrenal axis in corticosteroid-resistant bronchial asthma. Am J Respir Crit Care Med 1996, 153:557-560 [DOI] [PubMed] [Google Scholar]
- 45.Lane S, Palmer B, Skidmore I, Lee T: Corticosteroid pharmacokinetics in asthma. Lancet 1990, 336:1265-1266 [DOI] [PubMed] [Google Scholar]
- 46.Corrigan C, Brown P, Barnes N, Szefler S, Tsai J, Frew A, Kay A: Glucocorticoid resistance in chronic asthma: glucocorticoid pharmacokinetics, glucocorticoid receptor characteristics, and inhibition of peripheral blood T cell proliferation by glucocorticoids. Am Rev Respir Dis 1991, 144:1016-1025 [DOI] [PubMed] [Google Scholar]
- 47.Alvarez J, Surs W, Leung D, Ikle D, Gelfand E, Szefler S: Steroid-resistant asthma: immunologic and pharmacologic features. J Allergy Clin Immunol 1992, 89:714-721 [DOI] [PubMed] [Google Scholar]
- 48.Lawson G, Chakraborty J, Tredger J, Baylis E: Methylprednisolone-hemisuccinate and its metabolites in serum, urine and bile from two patients with acute graft rejection. Br J Clin Pharmacol 1995, 39:176-178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wilkinson J, Lane S, Lee T: Effects of corticosteroids on cytokine generation and expression of activation antigens by monocytes in bronchial asthma. Int Arch Allergy Appl Immunol 1991, 94:220-221 [DOI] [PubMed] [Google Scholar]
- 50.Schlaghecke R, Beuscher D, Kornely E, Specker C: Effects of glucocorticoids in rheumatoid arthritis. Diminished glucocorticoid receptors do not result in glucocorticoid resistance. Arthritis Rheum 1994, 37:1127-1131 [DOI] [PubMed] [Google Scholar]
- 51.Sandberg J-O, Eizirik D, Sandler S, Tracey D, Anderson A: Treatment with an interleukin-1 receptor antagonist protein prolongs mouse islet allograft survival. Diabetes 1993, 42:1845-1851 [DOI] [PubMed] [Google Scholar]
- 52.Shiraishi M, Csete M, Yasunaga C, McDiarmid S, Vannice J, Busuttil R, Shaked A: The inhibitor cytokine interleukin-1 receptor antagonist synergistically augments cyclosporine immunosuppression in a rat cardiac allograft model. J Surg Res 1995, 58:465-470 [DOI] [PubMed] [Google Scholar]
- 53.Abhyankar S, Gilliland D, Ferrara J: Interleukin-1 is a critical effector molecule during cytokine dysregulation in graft versus host disease to minor histocompatibility antigens. Transplantation 1993, 56:1518-1523 [DOI] [PubMed] [Google Scholar]
- 54.Campion G, Lebsack M, Lookabaugh J, Gordon G, Catalano M: Dose-range and dose-frequency study of recombinant human interleukin-1 receptor antagonist in patients with rheumatoid arthritis. The IL-1Ra arthritis study group. Arthritis Rheum 1996, 39:1092-1101 [DOI] [PubMed] [Google Scholar]
- 55.Antin J, Weinstein H, Guinan E, McCarthy P, Bierer B, Gilliland D, Parsons S, Ballen K, Rimm I, Falzarano G, Bloedow D, Abate L, Lebsack M, Burakoff S, Ferrara J: Recombinant human interleukin-1 receptor antagonist in the treatment of steroid-resistant graft-versus-host disease. Blood 1994, 84:1342-1348 [PubMed] [Google Scholar]
- 56.McCarthy P, Williams L, Harris-Bacile M, Yen J, Przepiorka D, Ippoliti C, Champlin R, Fay J, Blosch C, Jacobs C, Anasetti C: A clinical phase I/II study of recombinant human interleukin-1 receptor in glucocorticoid-resistant graft-versus-host disease. Transplantation 1996, 62:626-631 [DOI] [PubMed] [Google Scholar]