INTRODUCTION
The use of free fibular grafts has been well reported for the treatment of various conditions. These include reconstruction of bony defects and nonunions, osteomyelitis, bone loss after resection of tumors, spinal surgery fusions, and congenital pseudarthrosis of the tibia among many others.4,8,9,16 It is an ideal graft in many circumstances because a vascular inflow can be obtained if needed. A fibular graft has excellent strength due to the cortical bone present, and has the potential for remodeling with loading.4,10 Several studies have looked specifically at the resultant donor site morbidity following free fibular grafting.1,2,3,7,12,19,23 The resultant morbidity at the donor site has occasionally been referred to as insignificant or inconsequential.1,9 However, several reports have found significant functional changes following partial fibulectomy, including decreased range of motion and strength at the knee and ankle, gait alteration, and contracture, stiffness and weakness of the great toe.2,7,12,19,22 Several other immediate and long-term complications of the free fibular graft donor site have been documented as well. Donor-site wound-healing complications, osteomyelitis and wound infection, transient peroneal nerve palsy, donor-site pain, edema, hematoma, ankle valgus deformity, and distal fibular osteoporosis are among the complications cited in the literature.2,3,7,8,12,16,19 Only eight previous cases of tibial stress fracture following partial free fibular graft harvest have been reported.6,8,10,22 Two of the eight cases involved a vascularized fibular graft, whereas the remaining six did not.
We present the case of a patient who underwent vascularized free fibular graft harvest for mandibular reconstruction. After six months this patient suffered a stress fracture and subsequent complete fracture of the tibia immediately adjacent to the fibular donor-site prompting referral to our institution. The patient's presenting complaints, physical exam findings, radiographic findings and treatment course are discussed.
CASE REPORT
An eighty-two year-old female presented to the Otolaryngology department on referral from a local oral surgeon due to a mass in the anterior gingival buccal region causing difficulty with denture fitting. She was diagnosed with stage T4N0 squamous cell carcinoma of the left anterior floor of the mouth. She subsequently underwent surgical anterior alveolar ridge resection and neck dissection. The mandible was reconstructed with the use of a vascularized fibular free flap with skin paddle harvested from the right leg without apparent difficulty. The graft taken measured approximately eighteen centimeters in length by radiographs of the donor leg taken post-operatively (Figure 1). Approximately six months post-operatively, she developed pain in the donor leg. Radiographs of the involved leg were again taken (Figure 2). An MRI was obtained revealing increased signal in the tibial region adjacent to the donor site. She was referred to a local Orthopaedic Surgeon and diagnosed with tibial osteomyelitis. Treatment at an outside institution consisted of a four-week course of intravenous antibiotics and limited weight bearing on the right extremity. Radiographs following antibiotic completion revealed increased sclerosis and the beginning of lucency in the diaphysis of the right tibia (Figure 3). Her pain had improved and she began physical therapy with the leg in a boot immobilizer. The antibiotics were discontinued. The patient was ambulating at physical therapy when a loud snap occurred with immediate pain in the right leg. She was referred the next day to Orthopaedic Surgery at our facility with a pathologic fracture through the area of presumed osteomyelitis(Figure 4).
Figure 1.

Anteroposterior radiograph of right leg one month following harvest of vascularized fibular graft for mandible reconstruction.
Figure 2.

Anteroposterior radiograph five months after surgery with onset of leg pain.
Figure 3.

Six months after fibulectomy and one month after onset of leg pain, anteroposterior and lateral radiographs reveal sclerosis, periosteal reaction and lucency in the diaphyseal tibia consistent with a stress fracture.
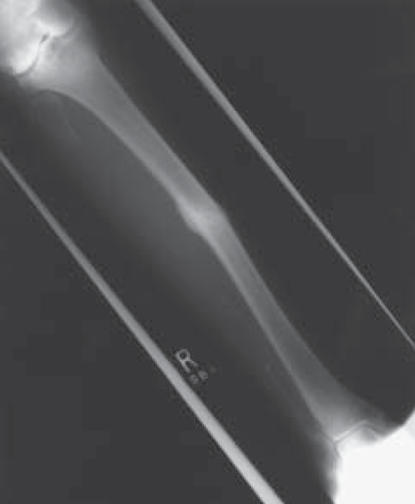
Figure 4.

Anteroposterior and lateral radiographs of right leg reveal complete fracture through previous stress fracture site.
On presentation to our facility she had a main complaint of pain in the afflicted extremity. She denied any history of fevers, chills, night sweats or other systemic manifestations of infection during the course of her leg discomfort. Her laboratory results on presentation included a C-Reactive Protein of 1.9 mg/dl, WBC of 8.9 K/mm3 and Sedimentation rate of 49mm/Hr. Physical exam was consistent with a fracture through the diaphysis of the tibia. There was minimal warmth, swelling and erythema consistent with a minimally displaced tibia fracture. The skin was intact. Radiographs revealed a complete fracture through the diaphysis of the tibia adjacent to the donor site for the fibular graft. The area of the fracture showed increased bony sclerosis and significant periosteal reaction consistent with a stress fracture. There were no bony erosions present. Retrospective review of prior radiographs sent with the patient from her local physicians revealed a gradual appearance of bony sclerosis and stress fracture lucency at the region of the eventual complete fracture.
The patient was placed into a long leg plaster cast after minimal closed reduction was performed. She was kept non-weight bearing for two months. This was then changed into a short-leg-cast with partial-weight-bearing at two months. At three and one-half months she was placed into a Sarmiento-type fracture brace and allowed weight bearing as tolerated. Her radiographs have shown progressive callus formation toward healing during her recovery (Figure 5).
Figure 5.

Anteroposterior and lateral radiographs five months after complete fracture show healing and minimal residual deformity.
DISCUSSION
The development of a stress fracture of the tibia is not an infrequent occurrence, especially with young and active individuals. The association of tibial stress fractures with athletes and military recruits has been well documented.5,14,15,17 However, the occurrence of tibial stress fracture after free fibular graft harvest from the ipsilateral leg is a rare occurrence. Emery et al reported on five stress fractures among 350 patients who had undergone free fibular graft for use in anterior reconstruction of the spine at two institutions.6 Each of these patients developed pain in the donor leg between ten weeks and sixteen months post-operatively. None of these patients developed a complete fracture of the tibia. Diagnosis was sometimes made retrospectively upon finding resolving periosteal reaction and sclerosis. Ivey et al reported the case of a sixty-two year-old female who developed a stress fracture and subsequent complete tibia fracture four months after she underwent vascularized fibular grafting to the humerus for atrophic non-union.10 This patient healed her tibia fracture uneventfully in a long-leg cast. Han et al reported one "spontaneous" tibia fracture in a diabetic osteopenic patient after vascularized fibular harvest amongst 132 vascularized fibular grafts performed.8 The specifics of this case were not presented in detail, but rather listed as one of the complications encountered in a large series of vascularized graft procedures. Lastly, Westesson reported a tibial stress fracture in an elderly diabetic female patient after vascularized fibular grafting for mandibular reconstruction after tumor resection, similar to our patient.22
The mechanism of stress fracture of the tibia has been postulated to result from excessive tensile forceson the bone at a given location. Tibial stress fractures were demonstrated in a rabbit model and studied histologically. Analysis revealed disruption of the cortical microvasculature causing osteocyte death and subsequent osteoclastic resorption, which weakens the bone.13 The fibula has been shown to carry approximately 6-16% of the load applied to the leg during weight bearing.11,18,20,21 This percentage can be altered by the position of the ankle.22 As shown by Lambert, removal of the fibula results in increased loads on the tibia and alters the fashion in which the tibia carries that load.11 It is unclear whether removing a portion of the tibia's blood supply, as occurs when harvesting a vascularized graft, increases the risk of stress fracture.
The presentation of a stress fracture can be deceiving, especially early in the process. The clinical and radiographic picture can be misleading and misinterpreted as infection or muscle pain amongst other diagnoses. Regardless, it is important to recognize that stress fracture is a potential etiology when donor leg pain occurs. Early recognition likely will prevent progression to a complete fracture, for which the treatment carries additional potential morbidity and significantly greater disability for the patient.
The majority of the reported cases of tibial stress fractures have occurred in patients at higher risk for insufficiency type fractures. Six of the seven case reports where patient age was given, including the case presented here, involved women older than fifty-five. The eighth patient, reported by Han without mention of age, suffered from Diabetes and osteopenia as well. It is likely that more elderly, and possibly osteoporotic, females are at increased risk for such a complication.The likely role of osteoporosis in these fractures was emphasized by Emery et al in their report of five cases.6 Heightened awareness of this potential complication, especially in this high-risk population of elderly, diabetic and osteoporotic patients, is recommended.
References
- 1.Anderson AF, Green NE. Residual functional deficit after partial fibulectomy for bone graft. Clin Orthop. 1991;267:137–140. [PubMed] [Google Scholar]
- 2.Anthony JP, Rawnsley MD, Benhaim P, Ritter EF, Sadowsky SH, Singer MJ. Donor leg morbidity and function after fibula free flap mandible reconstruction. Plast Reconstr Surg. 1995;96:146–152. doi: 10.1097/00006534-199507000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Babovic S, Johnson CH, Finical SJ. Free fibula donor-site morbidity: The Mayo experience with 100 consecutive harvests. J Reconstr Microsurg. 2000;16:107–110. doi: 10.1055/s-2000-7544. [DOI] [PubMed] [Google Scholar]
- 4.Bishop AT. Vascularized bone grafting. In: Green DP, Hotchkiss RN, Pederson WC, editors. In Green's Operative Hand Surgery. Ed 4. Philadelphia: Churchill Livingstone; 1999. pp. 1221–1250. [Google Scholar]
- 5.Blank S. Transverse tibial stress fractures: A special problem. Am J Sports Med. 1987;15:597–602. doi: 10.1177/036354658701500613. [DOI] [PubMed] [Google Scholar]
- 6.Emery SE, Heller JG, Petersilge CA, Bolesta MJ, Whitesides TE. Tibial stress fracture after a graft has been obtained from the fibula. A report of five cases. J Bone and Joint Surg. 1996;78-A:1248–1251. doi: 10.2106/00004623-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Goodacre TEE, Walker CJ, Jawad AS, Jackson AJ, Brough MD. Donor site morbidity following osteocutaneous free fibula transfer. Br J Plast Surg. 1990;43:410–412. doi: 10.1016/0007-1226(90)90004-j. [DOI] [PubMed] [Google Scholar]
- 8.Han CS, Wood MB, Bishop AT, Cooney WP., III Vascularized bone transfer. J Bone and Joint Surg. 1992;74-A:1441–1449. [PubMed] [Google Scholar]
- 9.Hidalgo DA, Rekow A. A review of 60 consecutive fibula free flap mandible reconstructions. Plast Reconstr Surg. 1996;96:585–596. [PubMed] [Google Scholar]
- 10.Ivey M, Hicks CA, Hook JD. Stress fracture of the tibia after harvest of a vascularized fibular graft for repair of nonunion of the humerus. Orthopedics. 1995;18:57–60. doi: 10.3928/0147-7447-19950101-11. [DOI] [PubMed] [Google Scholar]
- 11.Lambert KL. The weight-bearing function of the fibula. A strain gauge study. J Bone and Joint Surg. 1971;53-A:507. [PubMed] [Google Scholar]
- 12.Lee EH, Goh JCH, Helm R, Pho RWH. Donor site morbidity following resection of the fibula. J Bone and Joint Surg. 72-B:129–131. doi: 10.1302/0301-620X.72B1.2298771. [DOI] [PubMed] [Google Scholar]
- 13.Li G, Zhang S, Chen G, Chen H, Wang A. Radiographic and histologic analyses of stress fracture in rabbit tibias. Am J Sports Med. 1985;13:285–294. doi: 10.1177/036354658501300501. [DOI] [PubMed] [Google Scholar]
- 14.Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Stress fractures in athletes: A study of 320 cases. Am J Sports Med. 1987;15:46–58. doi: 10.1177/036354658701500107. [DOI] [PubMed] [Google Scholar]
- 15.Milgrom C, Stein GM, Kashtan H, Margulies JY, Chisin R, Steinberg R, Aharonson Z. Stress fractures in military recruits. J Bone and Joint Surg. 1985;67-B:732–735. doi: 10.1302/0301-620X.67B5.4055871. [DOI] [PubMed] [Google Scholar]
- 16.Minami A, Kasashima T, Iwasaki N, Kato H, Kaneda K. Vascularized fibular grafts: An experience of 102 patients. 2000J Bone and Joint Surg. 82-B:1022–1026. doi: 10.1302/0301-620x.82b7.10332. [DOI] [PubMed] [Google Scholar]
- 17.Rettig AC, Shelbourne KD, McCarroll JR, Bisesi M, Watts J. The natural history and treatment of delayed union stress fractures of the anterior cortex of the tibia. Am J Sports Med. 1988;16:250–255. doi: 10.1177/036354658801600309. [DOI] [PubMed] [Google Scholar]
- 18.Segal D, Pick RY, Klein HA, Heskiaoff D. The role of the lateral malleolus as a stabilizing factor of the ankle joint: preliminary report. Foot Ankle. 1981;2:25–29. doi: 10.1177/107110078100200104. [DOI] [PubMed] [Google Scholar]
- 19.Shpitzer T, Neligan P, Boyd B, Gullane P, Gur E, Freeman J. Leg morbidity and function following fibular free flap harvest. Ann Plast Surg. 1997;38:460–464. doi: 10.1097/00000637-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Skraba JS, Greenwald AS. The role of the interosseous membrane on tibiofibular weightbearing. Foot Ankle. 1984;4:301–304. doi: 10.1177/107110078400400605. [DOI] [PubMed] [Google Scholar]
- 21.Takebe K, Nakagawa A, Minami H, Kanazawa H, Hirohata K. Role of the fibula in weight-bearing. Clin Orthop. 1984;184:289–292. [PubMed] [Google Scholar]
- 22.Westesson PL, Wandtke JC. Stress fracture of the tibai: an unusual complication of reconstructive surgery of the mandible. J Oral Maxillofac Surg. 1999;57:70–74. doi: 10.1016/s0278-2391(99)90638-9. [DOI] [PubMed] [Google Scholar]
- 23.Youdas J W, Wood MB, Cahalan TD, Chao EYS. A quantitative analysis of donor site morbidity after vascularized fibula transfer. J Orthop Res. 1988;6:621–629. doi: 10.1002/jor.1100060502. [DOI] [PubMed] [Google Scholar]


