INTRODUCTION
Congenital vertical talus (CVT), or "rocker-bottom" foot, describes the most severe form of congenital flatfoot. It is characterized by a rigid dislocation of the talonavicular joint, in which the navicular articulates with the dorsal aspect of the talus.11 The term "congenital convex pes valgus" is also frequently used.4,5,11 To make a definite diagnosis, it is important to demonstrate that the navicular is dislocated dorsally on the neck of the talus when the foot is maintained in extreme plantar flexion.3
The etiology of this entity remains unknown. It is associated with certain central nervous system defects, multiple malformation syndromes, in-utero deformation, and some aneuploidy states.1 Only two groups have reported on the familial occurrence of this condition.9,10 We describe vertical transmission of isolated CVT in four separate families and confirm that autosomal dominant inheritance should be considered in the differential diagnosis of isolated CVT.
CASE REPORTS
Case 1
The pedigree for this family is shown in Figure 1. The proband (II-2) was noted to have severe rocker-bottom deformities in both feet at birth. No other clinical abnormalities were noted. There was no evidence of flexion contractures or ulnar deviation of the fingers, limitation of motion at other joints or an underlying neuromuscular disease. The diagnosis of CVT was confirmed by radiographs demonstrating persistent dorsal dislocation of the navicular on the talus and no change with a maximum plantar flexion view (Figure 2A). There was no radiographic evidence of tarsal coalition or other malformation. The patient underwent open reduction of the talona vicular joints with posterior releases at two years of age. She developed increasing hind foot pain and underwent triple arthrodesis at the age of 13 years. She is now 52 years old and asymptomatic.
Figure 1.
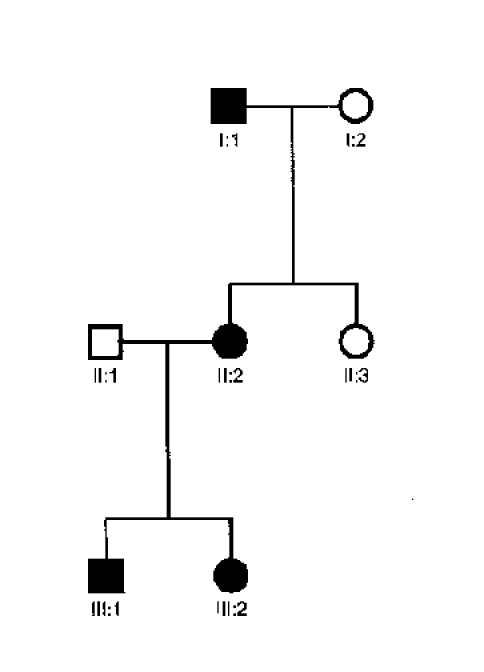
This three-generation pedigree is compatible with autosomal dominant inheritance.
The patient's daughter (III-2) was noted to have rocker-bottom deformities in both feet at birth (Figure 2B). No other clinical abnormalities were noted. She was initially treated with serial corrective casts without improvement and underwent open reduction of the talonavicular joints with posterior ankle releases at 2 1/2 years of age. She is now 26 years old and has no complaints with regard to her feet.
The patient's son (III-1) was also found to have rocker-bottom deformity in his right foot at birth. Clinical evaluation at the age of 5 months demonstrated talipes equinovarus deformity of the left foot, and congenital vertical talus of the right foot (Figure 2C). Serial corrective casts were applied to both feet. Open reduction of the right vertical talus was performed at 8 months of age. Surgical correction of his clubfoot was also performed at that time.
All immediate members of this family underwent physical and roentgenographic examination, with the exception of I-1, who was deceased at the time of this investigation. According to family members, I-1 had life-long difficulty with his feet and was treated as a young adult with triple arthrodeses for advanced degenerative arthritis. Upon review of his medical records, it was found he had bilateral CVT deformities as a child as well.
Case 2
A 2-year-old female was seen at our institution and diagnosed with CVT bilaterally. No other abnormalities were found. The deformities were initially treated by open reduction of the talonavicular dislocations followed by delayed posterior releases. At the age of 33, her right foot is asymptomatic without deformity; however, the left foot shows marked rocker-bottom deformity with moderate amount of pain.
This patient's younger brother was found to have a rocker-bottom deformity of his right foot at birth. The parents noticed this because the boy's sister had the same deformity. No other abnormalities were noted. He was treated with serial casting without success. He underwent open reduction at 5 months of age. We were able to examine both parents and no foot abnormalities were noted.
Case 3
A 10-month-old female was treated with serial casting followed by open reduction of a right-sided CVT deformity. No other abnormalities were noted on physical examination. The patient's mother was also treated at our institution as a child with open reduction of an isolated unilateral CVT deformity. We were able to examine all immediate family members and noted flexible flatfeet in several members, but there was no evidence of rigid foot deformities.
Case 4
A 9-month-old female presented to our hospital for evaluation of a rigid flatfoot deformity on the right. After obtaining plantar-flexion radiographs of both feet, she was diagnosed with CVT on the right. She is currently undergoing serial casting. Both parents were examined and there was no evidence of foot abnormalities in either. However, the family history was remarkable for the child's grandmother being treated for CVT as a child.
DISCUSSION
Lamy and Weisman,8 who were the first to provide an extensive review of congenital vertical talus, reported one familial case, a mother and child. Ogata et al.9 reported on two families in which there was familial occurrence of CVT. These included an affected mother whose son and daughter also had CVT, and another family in which a brother and sister were affected. Stern et al.10 reported on a three generation family with 9 total affected members and suggested that CVT can be inherited as an autosomal dominant trait. We report the occurrence of familial CVT in four separate pedigrees, in which the disorder is inherited in an autosomal dominant fashion with variable expression and incomplete penetrance. This explains those cases in which affected siblings were born to clinically normal parents.
When evaluating a patient with apparent isolated CVT, it is important to rule out systemic neurological, muscular or skeletal disorders, such as arthrogryposis, spina bifida, Down syndrome, and Trisomy 18, since approximately half of all cases of CVT will be associated with one of these abnormalities.2,6,7 Another entity that is important to keep in the differential is autosomal dominantly inherited digitotalar dysmorphism. This disorder is characterized by flexion deformity and ulnar deviation of the fingers, short stature and rocker-bottom feet due to vertical talus. Therefore, examination of the hands is crucial before making the diagnosis of isolated CVT.
Based on our report of vertical transmission of isolated CVT in four separate pedigrees and other cases of familial isolated CVT in the literature, we support the theory that isolated CVT can be transmitted as an autosomal dominant trait with variable expression and incomplete penetrance. In all patients with isolated CVT, a family history should be obtained to look for affected family members. Appropriate counseling should be provided to families in regard to the inheritance pattern.
Since this disorder follows a Mendelian inheritance pattern, it is likely that a single gene is responsible; this makes a search for this gene an attractive proposition. We are currently performing a genome-wide scan to localize the gene for this disorder. Once chromosomal localization is made, candidate genes will be identified in that area based on their known or probable role in limb development. Mutational analysis studies will then be performed on these chosen genes in the hopes of identifying the one responsible for this disorder.
Figure 2.
Figure 2A.

Lateral radiograph of proband II-2's foot at 19 months of age.
Figure 2B.

Lateral radiograph of proband III-2's foot at 12 months of age.
Figure 2C.

Lateral radiographs of proband III-1's foot at 5 months of age.
References
- 1.Coleman SS, Stelling FH, III, Jarrett J. Pathomechanics and treatment of congenital vertical talus. Clin Orthop. 1970;70:62–72. [PubMed] [Google Scholar]
- 2.Dodge LD, Ashley RK, Gilbert RJ. Treatment of the congenital vertical talus: a retrospective review of 36 feet with long-term follow-up. Foot Ankle. 1987;7:326–332. doi: 10.1177/107110078700700602. [DOI] [PubMed] [Google Scholar]
- 3.Drennan JC. Congenital vertical talus. Instr Course Lect. 1996;45:315–322. [PubMed] [Google Scholar]
- 4.Drennan JC, Sharrard WJ. The pathological anatomy of convex pes valgus. J Bone Joint Surg. (Br) 1971;53:455–461. [PubMed] [Google Scholar]
- 5.Ellis JN, Scheer GE. Congenital convex pes valgus. Clin Orthop. 1974;99:168–174. doi: 10.1097/00003086-197403000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Hamanishi C. Congenital vertical talus: classification with 69 cases and new measurement system. J Pediatr Orthop. 1984;4:318–326. [PubMed] [Google Scholar]
- 7.Jacobsen ST, Crawford AH. Congenital vertical talus. J Pediatr Orthop. 1983;3:306–310. doi: 10.1097/01241398-198307000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Lamy L, Weissman L. Congenital convex pes valgus. J Bone Joint Surg. 1939;21:79–81. doi: 10.1302/0301-620x.81b2.8980. [DOI] [PubMed] [Google Scholar]
- 9.Ogata K, Schoenecker PL, Sheridan J. Congenital vertical talus and its familial occurrence: an analysis of 36 patients. Clin Orthop. 1979. pp. 128–132. [PubMed]
- 10.Stern HJ, Clark RD, Stroberg AJ, et al. Autosomal dominant transmission of isolated congenital vertical talus. Clin Genet. 1989;36:427–430. [PubMed] [Google Scholar]
- 11.Tachdjian MO. Congenital convex pes valgus. Orthop Clin North Am. 1972;3:131–148. [PubMed] [Google Scholar]


