Abstract
The dislocated hip in a non-ambulatory child with spastic paresis tends to be a painful interference to sleep, sitting upright, and perineal care. Proximal femoral resection-interposition arthroplasty is one method of treatment for this condition. We reviewed eight hips, two bilateral cases, with a mean follow-up of 30 months. Clinical improvement was observed in all except one case, with respect to pain relief and sitting tolerance. Some proximal migration was observed in three cases, despite routine post-operative skeletal traction in all cases and careful soft tissue interposition. One case showed significant heterotopic ossification which restricted prolonged sitting. This patient needed some occasional medication for pain.
INTRODUCTION
Quadriplegia in cerebral palsy patients is commonly associated with hip dislocation and subluxation,2,5,8,11,18 with its incidence ranging from 2.6 to 75%.4,6,18 Several factors have been related to this complication including absence of normal gait and excessive femoral anteversion, as well muscle imbalance and spasticity. 3 The age of presentation for this complication is variable, but represents the end stage of a progressively subluxating hip in juveniles.5 Some procedures may be effective in preventing this devastating problem at an early age, such as soft-tissue releases and femoral or pelvic osteotomies.22
Hip dislocation in patients with spastic quadriplegia may be associated with several problems such as difficulties with perineal hygiene and sitting position, decubitus ulcerations in the lateral aspect of the greater trochanter, pathologic fractures in the ipsilateral distal femoral metaphysis, pelvic obliquity, and scoliosis.2,18 Probably the most serious and severe problem for the patient and family is pain. Pain is significantly associated with spastic hip dislocation in as many as 70% of these patients.2,10,18
Different approaches have been used to treat painful spastic hip dislocation, depending, in part, on the presence or absence of degenerative arthritis in the hip joint. These include femoral resection with subtrochanteric valgus osteotomy,13 open reduction with various osteotomies, 14,17 prosthetic interposition arthroplasty,7,10 arthrodesis,16 and resection-interposition arthroplasty.4 We review our experience and results in treating painful hip dislocations in patients with spastic quadriplegia.
MATERIALS AND METHODS
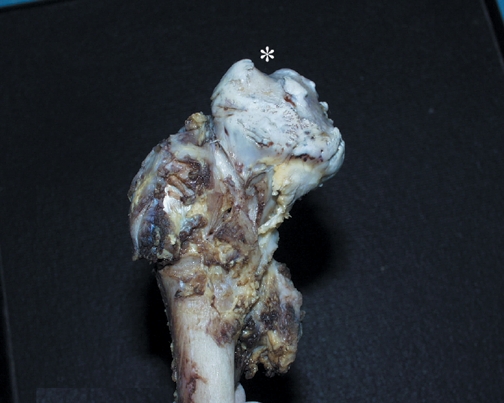
We reviewed patients treated in our hospital with spastic quadriplegia and an associated painful hip dislocation. We found the charts and radiographs of six patients (eight hips) who had undergone resection interposition arthroplasty described by Castle4 for the treatment of a chronic dislocated painful hip (Figure 1). Average age at the time of surgery was 14 years and 4 months (range from 9 years and 6 months to 17 years). There were four males and two females. None of the patients had ever been ambulatory. The right side was involved in four cases and the left in another four. All patients were mentally impaired with spastic quadriplegia. None had any previous surgical procedure. The average follow-up was 30 months (range 8 months to 90 months).
Figure 1.

AP radiograph, left hip dislocation. Impingement (asterisk) of superolateral aspect of the acetabulum against proximal femoral epiphysis.
Patients were treated surgically with a resection-interposition arthroplasty of the dislocated hip, as described by Castle and Schneider.4 The procedure consisted of an extraperiosteal dissection and resection of the proximal femur at the level of the lesser trochanter. A straight lateral approach was used. Post-operatively, patients were placed in skeletal traction for three weeks. No routine heterotopic ossification prophylaxis was used postoperatively.
The preoperative evaluation included range of motion and resting position of the hip, the presence of pain (pain was quantified based on the number and frequency of analgesic pills per day and subjective assessments by the patients' families), and the radiographic position and anatomy of the proximal femur. The postoperative evaluation consisted of: 1) A standardized telephone questionnaire regarding pain and sitting tolerance (all patients lived at home with their families); 2) A clinical examination of the hip and its range of motion; and 3) An AP radiograph for determining migration of the proximal femur and grade of heterotopic ossification. Grade I was a cap of mushroom-shaped bone, grade II was proximal bone spicule formation, and grade III was diffuse ossification.12
RESULTS
Results are summarized in Table 1. Pain status was improved in all patients except one, who needed one pill of regular analgesic medication every two to three nights (case 2). Preoperatively, all patients routinely needed daily pain medication, had significant difficulty sleeping, and had a restricted sitting tolerance (less than one hour). Post-operatively all patients except case-two improved dramatically, without sitting limitations and with no need for medication. All cases also had improved ease of access for perineal hygiene. Range of motion was increased in both flexion and abduction. Flexion contracture, which had interfered with the sleeping position previously, was resolved after resection arthroplasty.
TABLE 1.
| case | sex | age at surgery | side | preoperative |
postoperative |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| hip pain | perineal hygiene | flexion contracture | passive abduction | hip pain | perineal hygiene | flexion contracture | passive abduction | femur level | heterotopic ossification | ||||
| 1 | m | 17 | R | constant | poor | 30° | 0° | no | good | 0-65° | 0-30° | above | no |
| 2 | m | 14 | R | constant | poor | 50° | 0° | discomfort sitting < 4h/day | better | 60-100° | -10° | below | no |
| 3 | f | 17.4 | L | constant | poor | 40° | 70° | no | good | 0-100° | 0-70° | below | no |
| 4 | f | 14.5 | L | constant | poor | 0° | 0° | no | good | 0-90° | 0-40° | below | grade II |
| 5 | m | 9.5 | R | constant | poor | 30° | 15° | no | good | 0-110° | 0-45° | below | no |
| 6 | m | 9.5 | L | constant | poor | 30° | 15° | no | good | 0-90° | 0-45° | below | no |
| 7 | m | 16.8 | L | constant | poor | 100° | 0° | no | good | 0-30° | 0-50° | acetabulum | grade I |
| 8 | m | 16.8 | R | constant | poor | 100° | 0° | no | good | 0-30° | 0-50° | acetabulum | grade I |
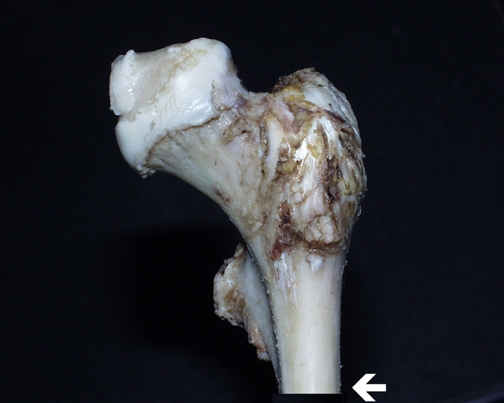
Radiographically, all evaluated hips were dislocated preoperatively. Femoral position was inferior to the acetabulum in five hips, at the level of the acetabulum in two hips, and proximal to the acetabulum in one case. On radiographs, all femoral epiphyses showed a typical triangular shape and a superolateral defect with impingement of the superolateral aspect of the acetabulum (Figure 1). All femoral heads showed a severe articular cartilage defect, especially in the impingement area, even in early cases (Figure 2). Heterotopic ossification was observed in three cases: two hips in a bilateral case showed grade I ossification, and one case had a severe grade II lesion with proportions approaching those of the resected femoral epiphysis (Figure 3). The case with grade II ossification was radiologically diagnosed four months after surgery, at which time she was treated with indomethacin. Both her discomfort and her range of motion improved significantly thereafter.
Figure 2. Gross specimen of the resected femoral head with articular cartilage defect.
A. early stage.
B. late stage (asterisk -acetabular impingement).
Figure 3.
Note the distal level (see arrow).
A.
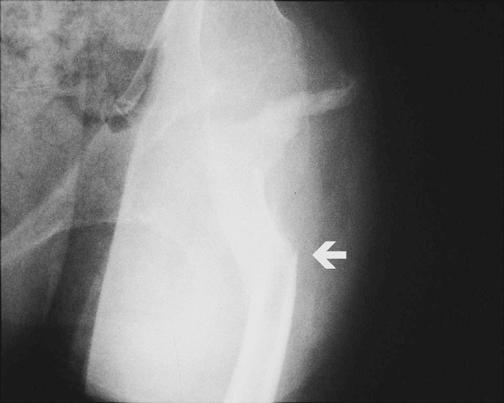
Significant heterotopic ossification, grade II, simulating the previously dislocated femoral epiphysis
B.
gross specimen of femoral resection
Time of surgery ranged from 80 minutes to 3 hours and 30 minutes, including bilateral cases. All patients needed a postoperative blood transfusion, (threshold for transfusion was a hemoglobin less than 7.8 mg/dL).
There were two postoperative complications: Case 3 had skin breakdown at the ischial tuberosity and required surgical debridement. Case 7/8, a bilateral case, developed pneumonia and upper gastrointestinal bleeding.
DISCUSSION
Patients with spastic quadriplegia and associated hip dislocation may often develop significant difficulties with upright sitting and posture, perineal hygiene, and hip pain. The frequency of significant pain in this patient population is quite variable in the reported literature, ranging from 30% to 80%, and even approaching 100% in selected subpopulations.6,10,17,18 Prevention of dislocation is the ideal approach, as with many pediatric orthopaedic conditions. However, when a painful hip dislocation is established, the goal of treatment is to obtain a pain-free mobile hip that will facilitate both a comfortable upright sitting position and ease of hygienic care.18 The definitive optimal treatment still remains controversial.
Open reduction with pelvic and femoral osteotomies14,17,20,22 are extensive approaches indicated for moderate femoral head deformities without osteoarthritic changes in the presence of an open triradiate cartilage. Some possible disadvantages include early femoral physeal closure as a consequence of vascular damage, the need for postoperative casting, and the subsequent risk of femoral and/or tibial fractures.17,21
Resection of the femoral head with subtrochanteric osteotomy has been done in an attempt to avoid proximal migration (by placing the lesser trochanter into the acetabulum), and heterotopic ossification (by a less extensile procedure).13 We fear that this alternative would require a second operation for removal of the fixation hardware. Also, the change in muscle vectors after a valgus osteotomy could direct the remaining femur into the acetabulum, which could compromise free range of motion.
The third option is prosthetic interposition arthroplasty.7,10,16 Gabos 7 described 14 patients treated with a humeral prosthesis, with or without the glenoid component. Although 70% had complete pain relief, almost one-third had a recurrent dislocation by radiographs. The author concluded that the implant stability does not affect the clinical outcome, as the implant acts as a spacer avoiding direct bone-to-bone contact. Koffman 10 reviewed four patients treated with total hip replacement with poor results: one was dislocated, another two had poor clinical results and subsequent revision surgeries, and the remaining patient died five months postoperatively. The author concluded that bone deformities, pelvic obliquity and poor bone stock are significant factors preventing optimal positioning of the implants in these patients. Root16 described good results in 13 of 15 patients with unilateral total hip replacement in spastic patients, but most of them had previously been ambulatory.
Arthrodesis has been mentioned by Bleck2 in one case, with improvement in discomfort and position of the lower limb. Root16 described good results in six of eight patients with a successful arthrodesis. Two cases had pseudarthrosis and needed a revision surgery. The procedure involved taking a muscle-pedicle graft from the iliac crest. They concluded that in unilateral cases, hip fusion was their treatment of choice, and in bilateral cases, total hip replacement was preferred.
Resection of the dislocated femoral head is the most common surgical treatment for most non-ambulatory patients. Kalen9 described 18 hips, most of them with significant pain relief. However, three patients had proximal migration of the femur that required a second operation. Koffman10 showed poor results related to pain, and almost all had heterotopic ossification. Five of six patients improved their sitting tolerance. The level of resection seems important in avoiding proximal migration of the femur that can result in unwanted articulation with the acetabulum and possibly new bone formation after resection. Studies by Perlmutter15 and Sherk19 show significantly different results between the Girdlestone resection and a more extensive distal resection. Closure of the capsulotomy was attempted in most of their cases. They concluded that patients treated with a girdlestone resection continued to have pain postoperatively.
Castle4 described a more extensive resection with selected capsular and fascial closure over the acetabulum and resected end of the femur in 14 hips. Sitting tolerance, motion and pain improved in all patients. The author concluded that adequate soft tissues coverage was extremely important in achieving such results.
Baxter1 also advocated an extensive resection, as described by Castle, in order to avoid poor results after a Girdlestone-type resection. He treated 4 patients with this approach, using skeletal traction post-operatively for three to six weeks, with minimal blood loss, a rapid rehabilitation, and without postoperative complications.
McCarthy12 found good results in almost all of 34 patients, based on pain relief, sitting position and perineal care, although he concluded that prior to skeletal maturity, this procedure could produce proximal migration of the proximal femur and heterotopic ossification. He also indicated that six weeks of postoperative traction was essential.
Widdman23 treated 18 hips with this procedure. Significant improvement was noted in pain, range of motion and sitting tolerance after surgery. The degree of proximal migration was not related to the type of postoperative traction used (skin vs. skeletal).
Our series demonstrated substantial clinical improvements. Pain relief was achieved in all cases but one. Sitting tolerance was globally improved, range of motion significantly increased, and perineal hygiene was eased.
Radiographically, some migration was observed in three cases, but without any resultant limitations in range of motion. Migration has been reported to cause flexion and adduction contractures, yet this was not the case in our patients. It seems reasonable that an adequate soft tissue interposition can prevent a progressive loss in range of motion, although some proximal migration can still take place. It is not clear whether the issue of proximal migration always results in clinical problems. A McHale procedure redirects the lesser trochanter into the acetabulum with relatively good preservation of range of motion. (Proximal migration could also be avoided by using skeletal traction for a longer period of time, or with distraction across the resection with an external fixator.)
Heterotopic ossification is another significant problem that occurred in one patient. Perioperative indomethacin and/or radiotherapy could be prophylactically administrated in cases with painful dislocated hips, in the presence of osteoarthritic changes and an open physis.23
With no other significant complications observed in our series, this resection-arthroplasty procedure is a promising treatment alternative for the patient with spastic quadriplegia and an associated painful hip dislocation. We would recommend this for most cases of dislocation with no previous history of surgical intervention.
References
- 1.Baxter M, D̕Astous J. Proximal femoral resection interposition arthroplasty: salvage hip procedure for the severely disabled child with cerebral palsy. J Pediatr Orthop. 1986;6:681–685. [PubMed] [Google Scholar]
- 2.Bleck EE. Orthopaedic Management In Cerebral Palsy. Philadelphia: JB Lippincott; 1987. [Google Scholar]
- 3.Carr C, Gage JR. The fate of the nonoperated hip in cerebral palsy. J Pediatr Orthop. 1987;7:262–267. doi: 10.1097/01241398-198705000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Castle ME, Schneider C. Proximal femoral resection-interposition arthroplasty. J Bone Joint Surg. (Am) 1978;60:1051–1054. [PubMed] [Google Scholar]
- 5.Cooke PH, Cole WG, Carey RPL. Dislocation of the hip in cerebral palsy: natural history and predictability. J Bone Joint Surg. (Am) 1989;71:441–446. doi: 10.1302/0301-620X.71B3.2722938. [DOI] [PubMed] [Google Scholar]
- 6.Cooperman DR, Bartucci E, Dietrick E, Millar E. Hip dislocation in spastic cerebral palsy: long-term consequences. J Pediatr Orthop. 1987;7:268–276. doi: 10.1097/01241398-198705000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Gabos PG, Miller F, Galban MA, Gupta GG, Dabney K. Prosthetic interposition arthroplasty for the palliative treatment of end-stage spastic hip disease in nonambulatory patients with cerebral palsy. J Pediatr Orthop. 1999;19:796–804. [PubMed] [Google Scholar]
- 8.Howard CB, MacKibbin B, Williams LA, Mackie I. Factors affecting the incidence of hip dislocation in cerebral palsy. J Bone Joint Surg. (Am) 1985;67:530–532. doi: 10.1302/0301-620X.67B4.4030844. [DOI] [PubMed] [Google Scholar]
- 9.Kalen V, Gamble JG. Resection arthroplasty of the hip in paralytic dislocations. Dev Med Child Neurol. 1984;26:341–346. doi: 10.1111/j.1469-8749.1984.tb04451.x. [DOI] [PubMed] [Google Scholar]
- 10.Koffman M. Proximal femoral resection or total hip replacement in severely disabled cerebral-spastic patients. Orthop Clin North Am. 1981;12:91–100. [PubMed] [Google Scholar]
- 11.Lonstein JE, Beck K. Hip dislocation and subluxation in cerebral palsy. J Pediatr Orthop. 1986;6:521–526. doi: 10.1097/01241398-198609000-00001. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy RE, Simon S, Douglas B, Zawacki R, Reese N, et al. Proximal femoral resection to allow adults who have severe cerebral palsy to sit: management. J Bone Joint Surg. (Am) 1988;70:1011–1016. [PubMed] [Google Scholar]
- 13.McHale KA, Bagg M, Nasson SS. Treatment of the chronically dislocated hip in adolescents with cerebral palsy with femoral head resection and subtrochanteric valgus osteotomy. J Pediatr Orthop. 1990;10:504–509. [PubMed] [Google Scholar]
- 14.Mubarak SJ, Valencia SG, Wenger DR. One-stage correction of the spastic dislocated hip: use of pericapsular acetabuloplasty to improve coverage. Bone Joint Surg. (Am) 1992;74:1347–1357. [PubMed] [Google Scholar]
- 15.Perlmutter MM, Synder M, Miller F, Bisbal R. Proximal femoral resection for older children with spastic hip disease. Dev Med Child Neurol. 1993;35:525–531. doi: 10.1111/j.1469-8749.1993.tb11683.x. [DOI] [PubMed] [Google Scholar]
- 16.Root L, Gross JR, Mendes J. The treatment of the painful hip in cerebral palsy by total hip replacement or hip arthrodesis. J Bone Joint Surg. (Am) 1986;68:590–598. [PubMed] [Google Scholar]
- 17.Root L, Laplaza FJ, Brourman SN, Angel DH. The severely unstable hip in cerebral palsy: treatment with open reduction, pelvic osteotomy, and femoral osteotomy with shortening. J Bone Joint Surg. (Am) 1995;77:703–712. doi: 10.2106/00004623-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Samilson RL, Tsou P, Aamoth G, Green WM. Dislocation and subluxation of the hip in cerebral palsy: pathogenesis, natural history and management. J Bone Joint Surg. (Am) 1972;54:863–873. [PubMed] [Google Scholar]
- 19.Sherk HH, Pasquariello PD, Doherty J. Hip dislocation in cerebral palsy. Selection for treatment. Dev Med Child Neurol. 1983;25:738–746. doi: 10.1111/j.1469-8749.1983.tb13842.x. [DOI] [PubMed] [Google Scholar]
- 20.Song HR, Carroll N. Femoral varus derotation osteotomy with or without acetabuloplasty for unstable hips in cerebral plasy. J Pediatr Orthop. 1998;18:62–68. [PubMed] [Google Scholar]
- 21.Stasikelis PJ, Lee DD, Sullivan CM. Complications of osteotomies in severe cerebral palsy. J Pediatr Orthop. 1999;19:207–210. doi: 10.1097/00004694-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Valenciano I, Dopazo JA, AlbiÒana J, Martinez I. Osteotomias en la cadera de la paralisis cerebral. Rev Ortop Traum. 2001;1:40–45. [Google Scholar]
- 23.Widmann RF, Do TT, Doyle SM, Burke SW, Root L. Resection arthroplasty of the hip for patients with cerebral palsy: an outcome study. J Pediatr Orthop. 1999;19:805–810. [PubMed] [Google Scholar]