Abstract
Strong traditions of basic research, clinical innovation, teaching and integrating science and evaluation of outcomes into clinical practice have characterized University of Iowa orthopaedics for ninety years. These traditions were brought to Iowa City from Vienna when Iowa City was a town of fewer than 10,000 people in a sparsely populated rural state. In the last third of the 19th century, surgeons at the University of Vienna, led by Theodore Billroth (1829-1894), helped transform the practice of surgery. They developed new more effective procedures, analyzed the results of their operations, promoted the emergence and growth of surgical specialties and sought understanding of tissue structure, physiology and pathophysiology. Their efforts made Vienna one of the world's most respected centers for operative treatment, basic and clinical research and surgical education. Two individuals who followed Billroth, Eduard Albert (1841-1900) and Adolf Lorenz (1854-1946) focused their research and clinical practice on orthopaedics. Their successes in the study and treatment of musculoskeletal disorders led one of their students, Arthur Steindler (1878-1959), a 1902 graduate of the Vienna Medical School, to pursue a career in orthopaedics. Following medical school, he worked in Lorenz's orthopaedic clinic until 1907 when he joined John Ridlon (1852-1936) at the Chicago Home for Crippled Children. In 1910, Steindler became Professor of Orthopaedics at the Drake Medical School in Des Moines, Iowa, and, in 1913, John G. Bowman, the President of the University of Iowa, recruited him to establish an orthopaedic clinical and academic program in Iowa City. For the next third of a century he guided the development of the University of Iowa Orthopaedics Department, helped establish the fields of orthopaedic biomechanics and kinesiology and tirelessly stressed the importance of physiology, pathology and assessment of the outcomes of operations. From the legacy of Billroth, Albert and Lorenz, Arthur Steindler created an internationally recognized center for orthopaedic care, research and teaching in Iowa City.
In my conception of scientific work, history and research are so indivisibly linked that I cannot even conceive of one without the other.-
Theodore Billroth26
INTRODUCTION
For most of the past twenty-five centuries, surgeons who attempted to correct skeletal deformities, improve mobility of patients suffering from stiff dysfunctional joints and treat injuries of the limbs and spine, did so with little or no understanding of structure and function of the musculoskeletal tissues or the pathophysiology of diseases and injuries of the musculoskeletal system8. Even in the nineteenth and early twentieth centuries, most orthopaedists took little or no interest in seeking new knowledge that would improve understanding of diseases and injuries or in critically evaluating the results of their operations and manipulations. Although exercise, bracing and gentle manipulations were part of orthopaedic practice in the 1800s, many of the non-operative treatments consisted of applying brute force that corrected deformities or mobilized stiff joints by crushing and rupturing tissues8,11; an approach summarized by the motto of a group of European orthopaedists in the early 1800s, "That which cannot be bent must be broken26." Operative treatments were bloody, often ill-conceived and frequently complicated by loss of limbs and death8,11. Patients who did not exsanguinate during surgery commonly died later of surgical infections. Although most 19th century surgeons had little interest in collecting data on the results of their operations, they knew that opening a joint or exposing a fracture had a much greater risk of leading to an infection than opening the abdomen, bladder or skull. When open reduction and internal fixation of a closed patellar fracture or removal of a loose body from a joint had mortality rates that approached fifty percent, few surgeons were eager to perform the procedures, and patients suffering from these disorders, who understood the risk, avoided surgeons if at all possible. Understandably, orthopaedic surgery, the most physical of the healing arts, did not enjoy even the level of respect accorded to other medical specialties.
In the early and mid 1800s, to gain recognition and attract patients, surgeons needed considerable technical skill and unshakable self confidence, if not arrogance and theatrical talent. More than a few possessed these qualities including Robert Liston of London and Samuel Gross of Philadelphia.
ROBERT LISTON (1794-1847)
Before the development of inhalation anesthesia in the 1840s, no patient could tolerate meticulous dissection: speed was the measure of a surgeon's skill-few operations short or long produced good results, but shorter operations caused less pain8. Robert Liston, Professor of clinical surgery at London's University College, earned a well deserved reputation as one of England's greatest surgeons for his masterful knowledge of anatomy, willingness to attempt the most difficult and dangerous procedures and displays of dexterity, physical strength, speed and dramatic talent in the operating theater8. His operations and lectures attracted students and physicians from throughout the United Kingdom, Europe and America and his papers on surgical procedures were widely read and quoted29–31. Liston routinely performed leg amputations in less than three minutes, performances marked by flashing steel and spurting blood18,38,54. In his efforts to perform above knee amputations and hip disarticulations with speed and panache, Liston occasionally injured observers who stood too close to the operating table and amputated more than he had originally planned. On at least one occasion, he simultaneously performed an accidental orchiectomy and an intentional above knee amputation. Another of his leg amputations led to a 300% mortality. A distinguished spectator died after he was slashed during the operation, the patient died of sepsis several days later and Liston's assistant died of sepsis as a result of losing several of his fingers during the operation18.
SAMUEL GROSS (1805-1884)
The rapid adoption of inhalation anesthesia in the late 1840s decreased the need for surgeons to operate with blazing speed, but it almost certainly increased the frequency and number of surgical complications including death8. Inhalation anesthesia made surgeons more willing to operate and patients more willing to have an operation. Yet, surgeons did not know how to prevent infections, they had difficulty controlling bleeding during operations and they had no way to restore blood volume in patients who had suffered massive hemorrhage.
Samuel Gross (Figure 1), the pre-eminent North American surgeon of the mid and late 1800s19–22, known for his expertise in treating disorders of the extremities, listed the qualities of a good surgeon, " . . . a firm and steady hand, a keen eye, and the most unflinching courage, which can disregard alike the sight of blood and the cries of the patient 22." He was among the surgeons who believed that a chance to cut is a chance to cure, and no surgeon should pass up a chance to cure. He stressed that " . . . as long as the various tissues of the body are subjected to disease and accident, so long will they require removal by the knife 22." Gross felt that surgeons had been unnecessarily reluctant to resect diseased or injured joints, but that his encouragement and their "intelligence, zeal and skill22" would soon increase the use of the procedure and extend it to every joint in the body.
Figure 1.
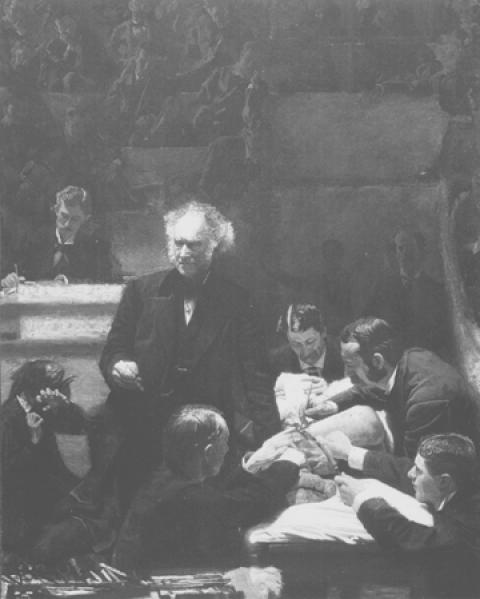
The Gross Clinic, Thomas Eakins' 1875 painting showing Samuel Gross, age 70, debriding the femur of a patient with osteomyelitis.
Gross knew that the complications of joint operations included "excessive suppuration, pyemia, and erysipelas22," conditions that he treated with bleeding, leeches, purgatives and blistering22. Despite these treatments, pyemia proved " . . . fatal in nine out of ten cases22." He regarded these complications as part of the risk of surgical treatment and disparaged Joseph Lister's 1867 report8,28 that anti-sepsis cut the mortality following elective surgery from forty-five percent to fifteen percent. Nearly ten years after Lister's publication, Gross commented, "Little, if any faith, is placed by any enlightened or experienced surgeon on this side of the Atlantic in the so-called carbolic acid treatment of Professor Lister," and in 1882 he added " . . . demonstration of living, disease-producing germs is wanting 39." Gross was certain that the increased skill and enthusiasm of surgeons for resecting tissues damaged by disease or accident would insure that surgery would no longer be " . . . regarded merely as a kind of handicraft, fit to be exercised only by men of inferior attainment, ability and skill 22."
In 1875, Thomas Eakens painted Samuel Gross at age 70 debriding the femur of a patient with osteomyelitis (Figure 1). Gross and his assistants wear their street clothes, splattered with blood and pus, and incise and retract the wound with their unwashed bare hands. The anesthetist sedates the patient with opendrop ether anesthesia. Lighting is poor and unsterile surgical instruments lie scattered where the surgeons can easily grab and discard them. The artist sits in the first row of spectators observing the procedure, making a drawing or taking notes. Other observers stand in an open entry way behind the anesthetist. A woman, possibly the sister, mother or wife of the patient, covers her face and recoils from the dissection and Gross's bloody hand.
THEODORE BILLROTH (1829-1894)
The transformation of surgery from a dangerous, dramatic and often ineffective handicraft into a safe effective method of treatment did not result not from increased zeal and technical skill of surgeons, but from a growing appreciation of the importance of scientific investigation and evaluation of the outcomes of surgical practice. No institution did more to bring about this change than the University of Vienna where the faculty stressed the importance of the sciences as a basis for surgical practice26. They contributed to progress in almost every currently recognized surgical specialty and taught physicians from throughout the world, including approximately 10,000 Americans who studied at the University of Vienna between 1870 and 191433.
In 1867, recognizing the limitations of surgical practice, the medical faculty of the University of Vienna, demanded that the University appoint a professor of surgery "of whom the greatest promotion of science may be expected, a man who is not only famous in the field of practical surgery, but also in the areas of physiological and pathological research who has demonstrated a special genius as a teacher, a surgeon and a writer, who is still in the prime of his life, from whom it may be expected that he will represent the most modern trends in surgery in relation to physiology and pathological anatomy and who is able to establish a surgical school in Vienna which will bring fame to the University and the greatest benefit to the country26." The University of Vienna found a man who exceeded all of these expectations: Theodore Billroth (Figure 2), the first child of Johanna and Karl Theodor Billroth, the pastor of a Lutheran church in Rugen, Germany's largest island in the Baltic Sea.
Figure 2.
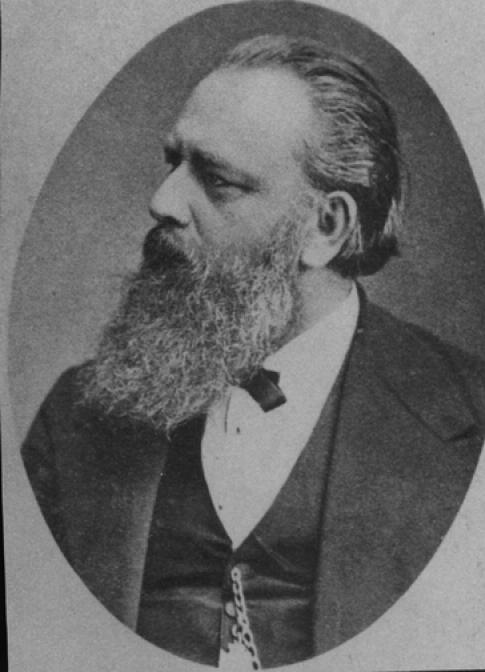
Theodore Billroth
Billroth's medical education in Gottigen, Berlin and Zurich had focused on science and surgery 33. He performed animal experimentation as well as microscopic examination of normal and diseased tissues and was recognized for his work in experimental physiology and pathology. Billroth enjoyed the study of pathology, but he chose to become a surgeon because "Observation at the sickbed is so much more interesting than microscopy26." In 1853, he started working as an assistant to the prominent German surgeon Bernhard Langenbeck (1810-1887)26. Although he did not limit himself to orthopaedics, Langenbeck treated patients with osteomyelitis and clubfoot deformities. He performed subcutaneous osteotomies to correct skeletal deformities caused by rickets and ankylosis of the hip and knee and developed the idea of stabilizing femoral neck fractures by driving a nail through the greater trochanter27. While working with Langenbeck, Billroth rapidly gained recognition for his talent as a surgeon and investigator and in 1860 was named to the position of Professor of Surgery in Zurich. In 1863 he published his most well known work, Die allgemeine chirurgische Pathologie und Therapie (English Edition: General Surgical Pathology and Theraputics. 1871)4, a book that illustrated the relationships between symptoms and abnormalities in tissues and demonstrated the importance of understanding pathophysiology for surgical practice.
Although he devoted much of his time to science and surgery, Billroth enjoyed history and music 33. In his study on the history of treatments for gun shot wounds he commented, "Only the man who is familiar with the art and science of the past is competent to aid in its progress in the future33." He had initially intended to pursue a career in music and demonstrated talent as a pianist, but his mother convinced him to enter medical school. To some extent his passion for music was fulfilled through his relationship with Johannes Brahms. The two men met in 1865, and began a close friendship that continued until Billroth's death2. Brahms arranged to perform many of his works in Billroth's home and dedicated two of his string quartets to Billroth.
Like Joseph Lister, Billroth recognized that as long as more than 40% of patients suffered wound infections or sepsis following technically successful operations, surgeons should only operate to save lives or relieve unbearable pain. Under these conditions, elective operations to improve limb function or correct deformity were difficult to justify and progress in orthopaedic surgical practice was impossible. In 1855 Billroth began a series of investigations directed toward finding the cause of post operative infections. In 1864, the year before Lister first used carbolic acid in a patient with an open fracture to kill the "unseen vital particles" that caused putrification and blood poisoning8, 11,28, Billroth proposed that substances formed in wounds caused fevers and sepsis26.
When Billroth joined the University of Vienna medical faculty in 1867, he continued his efforts to find the cause of wound infections. In the same year, Lister reported the efficacy of his carbolic acid antiseptic method in a consecutive series of patients8,28, an event that stimulated Billroth to start new investigations of the role of microorganisms in wound infections and methods of antisepsis. He concluded that Lister's method needed further development, but he started using it in 187826. Because of complications caused by carbolic acid Billroth switched to using iodoform as an antiseptic in the 1880s and in 1891 began the practice of asepsis for surgery.
Samuel Gross watched Billroth perform an operation in 1868 and described him as, "fearless and bold, almost to the point of rashness33." Given Gross's evaluation, it is reasonable to assume that Billroth did not lack confidence when he was operating, but he also carefully planned each operation and performed and tested new operations on animals to evaluate their efficacy and refine his techniques26. Among his most well-recognized achievements were successful esophageal resection in 1871, laryngectomy in 1873 and gastrectomy, the Billroth I, in 188126.
Billroth also had an interest in the pathophysiology and treatment of musculoskeletal diseases and injuries. He studied and treated club foot deformities, developmental dislocations of the hip, sarcomas of the extremities, fractures, malunions, pseudarthroses, bone and joint infections, joint injuries, joint dislocations, joint ankylosis and arthritis deformans (osteoarthritis)1,4. His description of the abnormalities of the acetabulum in patients with developmental dysplasia of the hip show that he understood the problem, ". . . not only is the head of the bone out of the socket, but the socket is irregularly formed-too shallow; later in life, in adults, it is greatly compressed and filled with fat." In Billroth's experience, treatment of developmental dislocations of the hip in older individuals was difficult if not impossible4. He commented, ". . . when you read in orthopedic pamphlets of the frequent cure of congenital luxations, you may be sure that in most cases there have been errors of diagnosis, or there is intentional deception4."
Throughout his career in Vienna, Billroth stressed the importance of the natural sciences in medical education5, and devoted time to making sure that younger surgeons understood that acquisition of technical surgical skills must be combined with scientific investigations and understanding of physiology and pathology. He also taught that statistical comparisons of the outcomes of different operations should be used to determine which operations were most effective26.
In 1890, Adelbert Seligmann painted Theodore Billroth at age 61 operating in the Allgemeines Krankenhous (General Hospital of the University of Vienna) (Figure 3). Although Seligmann's portrayal of Billroth as a commanding figure surrounded by assistants and spectators resembles Eakins depiction of Gross (Figure 1), there are differences. In Seligmann's painting surgeons and the anesthetist wear frocks resembling modern surgical gowns, the lighting from the windows is excellent and no one covers their face in horror. Billroth's expression and posture suggests that, at least on this day, he approached the performance of an operation with more thought and less drama than Gross, and the scene more closely resembles a current operating room than a theater.
Figure 3.

Adelbert Seligmann's 1890 painting showing Theodore Billroth, age 61, operating in the Allgemeines Krankenhous (General Hospital of the University of Vienna).
Billroth was a skillful teacher and surgeon, and a dominating leader, a surgical Geheimrat33. He was also an unreservedly committed German nationalist and a man of his time, family and culture 1,33. The decisiveness and confidence that made him a great surgeon may have contributed to his willingness to voice his opinions concerning the importance of establishing and maintaining order in medical education and of the fitness of different students for the study of medicine. In his book, "The Medical Sciences in the German Universities: A Study in the History of Civilization 5" he expressed concern that " . . . there are many studying at Vienna who are not of the elect and who are trying to force themselves into the medical profession." He was concerned that accommodating these students would "reduce the German method of university instruction to the level to which the lay surgeons were formerly restricted, expressly for the sake of these elements that are piling up in Vienna, or to organize separate schools in which to transform stupid, ignorant, starving students into stupid, ignorant and starving physicians5."
Billroth argued that to avoid the degradation of German university medical education the academic hierarchy must be maintained and only the most desirable students should be selected for medical education. He believed that the rules of academic conduct and advancement should be enforced by the state, "no faculty can exist without a definite code for both students and professors" and "it is the duty of the state to see to that such a code exists5." Commenting on the aspirations of some individuals for a career in medicine he said, "No profession except, perhaps, the clergy, is so often exploited by uneducated families who aim to climb into the cultured classes on the shoulders of the younger generation, as is the medical profession. For the Jews a medical career offers comparatively fewer difficulties than any other5." He also expressed concern over the composition of the medical student body in Vienna, "Among the non-Germans studying in Vienna a lack of money is often coupled with the lack of talent and of decent home training . . ." and "I have repeatedly pointed out that the undesirable elements are not German, but Galacian and Hungarian Jewish elements5." Other members of the University of Vienna faculty in the late 1800s and early 1900s may not have been as willing as Billroth to record their views of the Germanic academic hierarchy and the desirability of Jewish students, but it is likely that many of them would have agreed with him. In this environment, students who were "not of the elect" faced multiple barriers and frustrations if they attempted to pursue a career in medicine.
EDUARD ALBERT (1841-1900)
While Billroth achieved widespread recognition for developing methods of resecting the stomach, esophagus and larynx, a younger Viennese surgeon, Eduard Albert (Figure 4) focused his practice and research on joint diseases and skeletal deformities26, 27,32,36. Albert, a watchmaker's son from Senftenberg, Bohemia, graduated from the Vienna Medical School in 1867, the year that Billroth was named professor of surgery. Following graduation Albert became a disciple of Billroth's arch rival, a prominent aristocrat and surgeon, Johann Heinrich Baron Dumreicher von Osterreicher (1815-1880). Dumreicher, a talented surgeon and excellent teacher, had a strong interest in surgery of the extremities. Unlike Billroth, he believed that surgery should be based on established facts and that introduction of scientific questions did nothing but create confusion. In addition, he had feuded with Billroth's teacher, Langenbeck, so the hostility between Billroth and Dumreicher was intense and long standing. Perhaps for this reason, as well as the desire to advance the career of one of his own disciples, Vincenz Czerny, Billroth bitterly opposed the appointment of Albert as head of the First Department of Surgery at the University of Vienna. Billroth considered it his greatest defeat when Albert was given the position in 1881.
Figure 4.
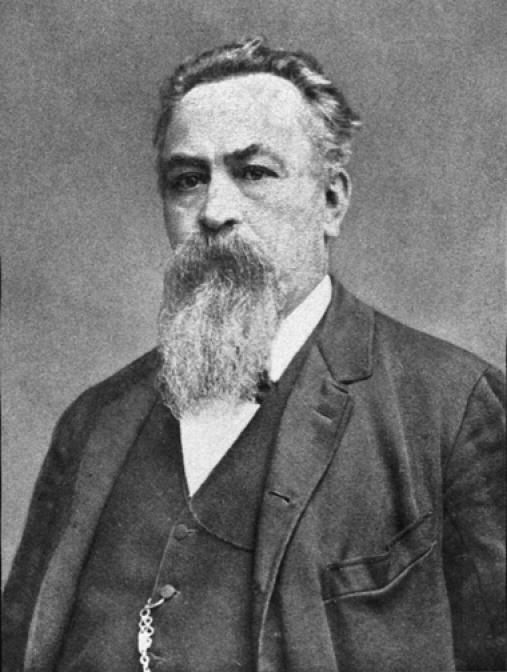
Eduard Albert
Had Billroth known Albert better he might have considered him a worthy choice for the position of Head of Surgery. Albert showed that he recognized the importance of Billroth's emphasis on scientific investigation, not only through his own work, but in an address praising Billroth's academic contributions in 189226. Albert published the first textbook advocating use of antisepsis to prevent post-operative infections in 1880 and during his time as Head of Surgery he proved to be an enthusiastic investigator who performed basic scientific investigations to advance surgical practice. His clinical experience with joint diseases combined with an interest in mathematics and a unique ability to visualize structures and their relationships in three dimensions led him to study joint mechanics, human movement and the mechanical changes in the spine associated with scoliosis. Albert investigated the structure of the synovial membrane and bone autografts3,27. He injected fluid into joints to study the resistance of the capsule and surrounding structures, and conducted a series of studies on the mechanics of the knee joint, the ankle joint, the shoulder girdle and the hip joint26. He was especially interested in the hip and described the function of the hip capsule during joint motion, in particular the movement and torsion of the capsular fibers. His studies of the pathology and therapy of coxitis and his manuscripts and lectures describing surgery of the extremities increased interest in operative treatment of joint diseases.
At the time Albert was conducting his studies of joint structure, function, mechanics, and diseases, other surgeons were treating joint diseases, primarily tuberculosis, by joint resection, often to the detriment of their patients. Albert argued for non-operative treatment of joint diseases, except for patients with the most severe joint deformities, instability or pain, or limb paralysis26. He proved that these patients could be helped by joint fusion, a procedure that he named arthrodesis3, and showed that arthrodesis could eliminate bracing and improve function of otherwise useless extremities3,26,36. He was best known for performing the first successful shoulder arthrodesis in 188127.
ADOLPH LORENZ (1854-1946)
Albert's favorite student, Adolf Lorenz (Figure 5), became one of the most influential orthopaedists of the 20th century3,27, 32,36. Lorenz, the son of an Austrian innkeeper and harness-maker, moved to Vienna in 1878 to study medicine32. To help pay for his medical studies he worked as an assistant in the anatomy department and acquired an encyclopedic knowledge of anatomy and considerable skill in dissection. Following graduation from medical school he sought employment in a surgical clinic. His background in anatomy gave him an advantage over other applicants and he was hired by Dumriecher to work as an assistant surgeon. Within a year, Dumbriecher died and Eduard Albert succeeded him. Lorenz commented later that the only teachers at the University of Vienna who made a lasting impression on him were Billroth and Albert32.
Figure 5. Adolf Lorenz.
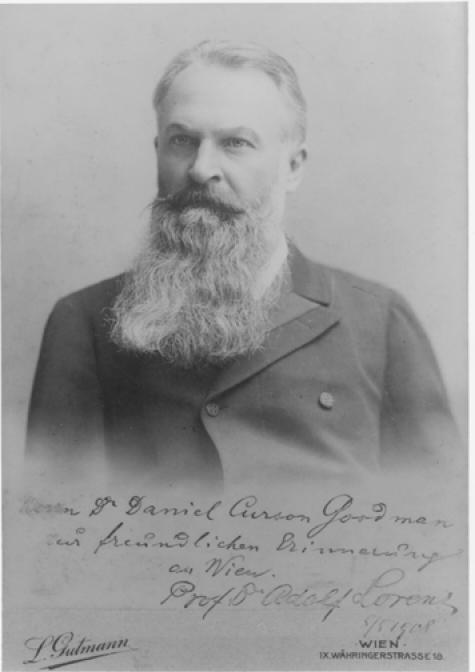
Lorenz autographed this portrait in 1908.
Lorenz's ambition, energy and intellect led Albert to appoint Lorenz as a lecturer in surgery at the University in 188426. Lorenz showed considerable talent as a surgeon, and decided that he wanted to become one of the great Viennese surgeons, like Billroth and Albert. However, an unexpected event forced him to temporarily choose another direction. Albert insisted that all surgeons in his department use Lister's carbolic acid antiseptic techniques. Lorenz developed severe eczema when his hands were exposed to carbolic acid and was unable to continue operating in the presence of carbolic acid. Albert advised him, "if you can't get along with wet surgery, why not try dry surgery26,32"; dry surgery referred to manipulative and casting treatment of diseased or injured limbs and the spine. Albert took this advice and established the "University Outpatient Department for Orthopaedic Surgery." He became interested in the "bloodless" treatment of children's musculoskeletal disorders including clubfoot deformities, bone and joint tuberculosis, paralytic deformities, congenital dislocation of the hip and scoliosis26. His ability to correct a skeletal deformity and maintain the reduction with a plaster dressing led Viennese surgeons and students to call him the "Gipsdozent" or plaster docent, a title that gave him great satisfaction32.
When the enthusiasm for carbolic acid antisepsis waned and other less toxic antiseptics became accepted, Lorenz started operating again using alcohol as an antiseptic; but, it was his experience with non-operative treatment of skeletal deformities that led to his most well known contributions to orthopaedics. Demonstrating that dangerous operations were unnecessary gave him great pleasure32. He showed that his treatment of joint tuberculosis with prolonged plaster immobilization produced better results than traction or joint resection, and he found that plaster bed treatment of spinal tuberculosis improved the general health of the patients and made surgery unnecessary in most cases32. He was correct that prolonged immobilization of an entire limb produced better results than joint resection for many patients with joint tuberculosis, but he apparently did not appreciate that this treatment damaged normal joints.
The best recognized of Lorenz's contributions to nonoperative treatment was his refinement and promotion of modeling redressment (molding reduction) of growing tissues and structures to correct deformity36. Lorenz had learned during his studies with Albert to consider and analyze the effects of mechanical forces on form and function of the musculoskeletal system. He considered it absurd to treat congenital or acquired deformities or loss of motion in such delicate and balanced structures as joints with "redressment force" (brute force), an approach that followed the teaching "if it can't be bent, then it must be broken26." Surgeons using the redressement force approach applied whatever force was necessary to correct a deformity, such as a clubfoot, and then fixed the limb in the reduced position with a cast or a similar appliance. As he described it, Lorenz's modeling redressment consisted of hundreds of successive applications of measured and moderate force until the corrected limb showed no tendency to recoil into the deformed position32. In his studies of clubfoot, he found that his gentle successive manipulations could overcome even resistant deformities if the surgeon was patient. He declared, "that no clubfoot, either in children or adults, of what ever origin could resist the modeling redressment" and that all bone operations on club feet were superfluous and mutilating32.
In his view, his greatest success was molding reduction treatment of developmental dislocation of the hip. He found that with traction and manipulation he could stretch the contracted soft tissues and lower the head of the femur from its displaced position to the level of the acetabulum3,32. Then, holding the femoral head in the reduced position with a plaster dressing caused remodeling of the soft tissues and the flattened acetabulum. He realized that the presence of the femoral head influenced the growth and development of the acetabulum and stressed that it was necessary to achieve reduction of the hip at an early stage to give the defective upper rim of the acetabulum "unhindered expression to its intrinsically normal growth tendencies26" thereby deepening the acetabulum and permanently stabilizing the hip in a reduced position. Lorenz's work with molding reduction of hip dysplasias led to a nomination for the Nobel Prize. He reported that he fell one vote short of receiving the award26,32.
As Lorenz's fame and clinical practice increased, an increasing number of surgeons from Europe and United States came to Vienna to learn his techniques32. His success convinced him that he needed an appropriate house, " . . . like a small castle on the slopes of Wiener wald, overlooking the broad valley of the Danube, the Tullnerfeld, and rising out of a nice garden with beautiful old trees32." He selected a site with a commanding view of the Danube and designed an imposing structure, Lorenz Hall, with impressive terraces and gardens (Figure 6). Above the entrance he had a sentence from Horace cut in stone: "Lucro appone quem fors dierum cumque dabit." (Consider as gain whatever chance may bring)32.
Figure 6. Lorenz Hall.
A. Exterior.

B. Lion Gate entrance.
C. Entry hall.

In 1902 and 1903, Lorenz traveled extensively in the United States32,36. During an extended stay in Chicago he performed a series of consultations and operations and reportedly collaborated with the prominent American Orthopaedist and Professor of Orthopaedic Surgery at Northwestern University John Ridlon (1852-1936)34,36,49. Figure 7 shows Lorenz performing a procedure, possibly a closed reduction of the hip, before a large audience in Chicago32. Ridlon subsequently challenged Lorenz's claim that the Lorenz method of closed reduction of the hip produced perfect reductions in fifty percent of treated hips and good results in eighty percent49. In 1904, at the New York Academy of Medicine, Ridlon stated that anatomic reductions using the Lorenz method were rare and did not exceed ten percent. Ridlon also reported that the method promoted by Lorenz had been developed previously by Agostino Paci (1845-1902)3,35,36 and that the extreme force used by Lorenz gave deplorable results49.
Figure 7. Adolf Lorenz in Chicago in 1902.
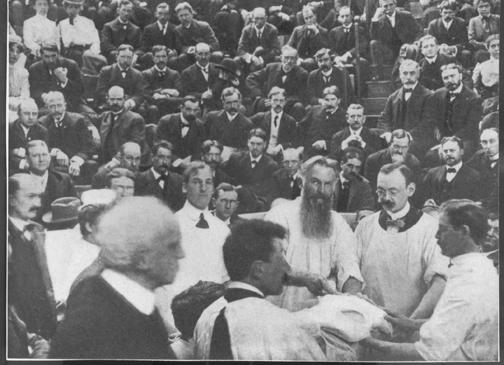
A large audience watches him perform a procedure.
World War I devastated Vienna and made Lorenz's investments worthless. Partially because of his difficult financial situation he continued to practice well into his 70s. Although he was generally complimentary concerning the United States, he was "stricken from the roles" of the American Orthopaedic Association, apparently during World War I32. When he asked to be reinstated in 1924, his request was refused. The reasons for these decisions are unknown. He completed his autobiography at age 8032, and noted, "I always enjoy the thought that excellent California wine will take the place of ice water upon my table," and "Moderate drinking, moderate eating, and moderate smoking will help you reach an average age of 80." He died at age 92.
ARTHUR STEINDLER (1878-1959)
Arthur Steindler, the son of Leopold Steindler (1849-1906) and Caroline (Goldberg) Steindler (1851-1936), was born in Graslitz, a town near Prague in the Austria-Hungarian province of Bohemia9,10,12,37. Shortly thereafter his family moved to Vienna (Figure 8). His father was a lawyer who valued rigorous classical education. In Arthur's early years he studied literature, language, philosophy and music. He eventually mastered five languages which enabled him to follow the world orthopaedic and scientific literature, translate manuscripts for others, write for foreign publications, and teach students from other countries. As a young man he enjoyed music and expressed interest in becoming a professional musician. However, his father strongly recommended that he choose a career in medicine. As a result, Steindler entered medical school at the University of Vienna in 1896 and graduated in 1902. Although Billroth had been dead for two years when Steindler started medical school, many of his former students were still present: Albert was 55, a prime age for a department head, teacher, surgeon and scientist, and Lorenz was only 42.
Figure 8.

Steindler Family in Vienna. Arthur (1878-1959) stands in the back in the center of the photograph. His younger brother Julius (1890-1970) is seated in front. His sisters Olga (1879-1933) and Irma (1876-1935) are to his right and his parents Leopold (1849-1906) and Caroline (Goldberg) (1851-1936) to his left.
Albert was regarded as one of the greatest teachers at the University of Vienna. Students never missed his lectures and he had an exceptional ability to explain complex clinical problems and make them interesting32. Steindler was among the students who found Albert's work exciting and he decided to work and study in University Outpatient Department for Orthopaedic Surgery directed by Lorenz following graduation from medical school13. Attitudes like those expressed by Billroth were common in Vienna in the early 1900s, and Jewish physicians, including Steindler, found that they had little chance for advancement13. After five years in Lorenz's clinic, Steindler left Vienna to join John Ridlon at the Chicago Home for Crippled Children in 1907. He later stated that he left Vienna because, "It was plain what was going to happen in Europe. There was nothing but privilege and preference. The working man had no chance. And nothing but aggression could come out of the politics of the government17".
It seems probable that Steindler became aware of Ridlon's work as a result of Lorenz's previous stay in Chicago and the subsequent controversy stimulated by Ridlon over the Lorenz method of closed reduction of the hip. Ridlon received his medical and orthopaedic education in New York, but he also studied with Hugh Owen Thomas (1834-1891), a leading British Orthopaedist. During his years in Chicago, Ridlon advocated and practiced Thomas's methods of treating deformities with bracing and manipulation rather than surgery. In addition to learning the American and Liverpool approaches to orthopaedic practice in Chicago, Arthur Steindler met Louise Junk, a young woman from a small town in Iowa53, and one of Ridlon's surgical nurses49.
In 1909 or 1910, John Ridlon was offered the position of Professor of Orthopaedics at the Drake Medical School in Des Moines, Iowa. Ridlon was well established in Chicago and had no interest in moving to Des Moines. In the short time Steindler had been in Chicago he had impressed Ridlon with his ambition, knowledge and clinical skill, and Ridlon suggested that Drake offer the position to his younger associate. He encouraged Steindler to take the opportunity to establish his own program. Drake seemed like a good choice. Des Moines, the state capital and largest city in the state, had good prospects for future growth, and Drake was a respected private University. Furthermore, there were no orthopaedists in the state. After moving to Des Moines in 1910, Steindler built a large clinical practice at Iowa Methodist and Lutheran hospitals17.
While Arthur Steindler was starting his orthopaedic program in Des Moines, a former high school principal, Abraham Flexner 14, was reviewing medical education in the United States and Canada. Between January of 1909 and April of 1910, Flexner visited all of the medical schools in the United States and Canada, in one 90 day period he visited 69 medical schools7. By June of 1910, Flexner had submitted and published a blistering critique revealing the dismal quality of North American medical education and exposing multiple instances of fraud 15,39.
When Flexner visited Iowa in April of 1909 he found four medical schools: two in Des Moines, Drake University College of Medicine with 106 students, and the Still College of Osteopathy with 115 students, and two in Iowa City, the State University of Iowa College of Medicine with 267 students and the State University of Iowa College of Homeopathic Medicine with 42 students15. Des Moines had a population of 89,113 and Iowa City had a population of 9,007. Flexner concluded that none of the schools in Iowa met minimal standards for medical education and that the state had between two and three times as many doctors as it needed. He regarded the Des Moines osteopathic school as a disgrace to the state that should be summarily suppressed. The Drake Medical School and the Iowa City Homeopathic School he considered "well intentioned but feeble institutions that only a large outlay could convert into acceptable and efficient schools15." His advice to Drake was, "It would be the part of wisdom to retire from a contest to which the institution is clearly unequal 15." He was not much kinder to the State University in Iowa City. His criticisms included a hospital and a patient population that were too small and a weak resident faculty: the Professor of Surgery for the State University of Iowa Medical School lived in Sioux City and the Dean who was also the Professor of Gynecology lived in Dubuque.
Drake University decided to take Flexner's advice and retire from the contest. Soon after this decision, physicians in Des Moines began a campaign to move the state's medical school to their city, arguing that that Des Moines could provide a better clinical experience for the medical students than Iowa City 17. Flexner supported the argument that medical schools should be located in a large cities, " . . . where the problem of procuring clinical material, at once abundant and various, practically solves itself15." However, he also noted that the difficulties in establishing quality medical schools in what he referred to as "out-of-the-way locations" were not insuperable. "At relatively greater expense, it is still possible to develop a medical school in such an environment15." He identified two out-of-the-way locations where "The faculty of medicine in these schools may even turn the defect of the situation to good account: for, freed from distraction, the medical schools at Iowa City and Ann Arbor may the more readily cultivate clinical science15."
John G. Bowman, the ninth president of the University of Iowa from 1911 to 1914, apparently understood Flexner's hint and did not intend to allow the medical school to close or to leave Iowa City. He recognized the urgent need to recruit faculty with clinical expertise who could also integrate science into their teaching and practice. He could not have found an individual who met these criteria better than Arthur Steindler. Steindler could have continued his practice in Des Moines, but he had a strong desire to establish an academic program. On October 6, 1913, President Bowman wrote to Dr. Steindler to tell him that he had been appointed Instructor in Orthopaedic Surgery at the University of Iowa with compensation at the rate of $800 for the academic year6. Bowman noted that, " . . . this appointment is temporary pending the judgment of the permanent surgeon who will shortly be elected . . . the probability seems to me, however, that you will remain with us not only for the present year but for a longer time6."
Although Iowa City and Vienna did not have much in common, the operating theater Steindler used during his first seven years in Iowa City closely resembled the one used by Theodore Billroth (Figure 9). On March 1, 1914, confident that he would be spending a long time in Iowa, Arthur Steindler married Louise Junk (1882-1963) and in the same year he became an American citizen. In 1915, he was appointed to the Chair of Professor of Orthopaedic Surgery at the State University of Iowa24.
Figure 9.
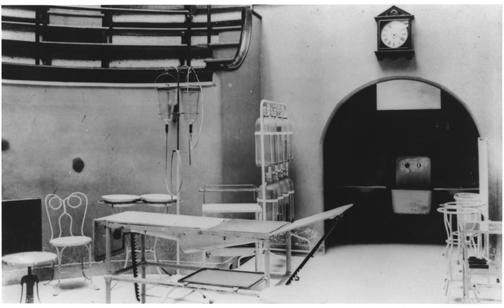
Operating theater in the University Hospital built on the east side of the Iowa River 1898.
By 1916, Steindler had established a large clinical practice in Iowa City and had helped convince the University and the State Legislature to construct a hospital for crippled children and pass legislation that supported the care of these children in Iowa City9,10. The completion of Children's Hospital in 1920 (Figure 10) gave Steindler and the University an exceptional facility that included inpatient areas, outpatient clinics, operating rooms (Figure 11), a brace shop, a large gymnasium, a hydrotherapy unit and laboratories. Many of the children sent to Steindler for treatment lived in the hospital for months while they received medical, surgical and physical treatment 9,10. After 1920 Steindler's orthopaedic program functioned as an autonomous academic and clinical unit and was referred to as the Department of Orthopaedic Surgery24.
Figure 10. Aerial view of Children's Hospital in the late 1920s.

The building was located on a bluff overlooking the Iowa River. The river is visible in the upper right corner of the photograph. Other than the entrance under the cupola, the hospital consisted of a single story with a lower level that was partially underground. All the inpatient wards were on the first floor and every ward had direct access to the outside. In the lower left of the photograph, several patients in their beds who have been moved out on to a patio can be seen. The operating rooms were located on the same floor at the back of the hospital and the brace shop, gymnasium, laboratories and hydrotherapy unit were located on the lower level. The U-shaped roof projecting into the central court yard, covers a ramp connecting the first and lower floors. This ramp made it possible to transport patients from the first floor to the lower level.
Figure 11. Operating room in Children's Hospital in the 1920s.

The operating schedule on the blackboard lists a shoulder arthrodesis, a procedure first described by Eduard Albert. There are no seats for observers, the surgeons wear gowns, gloves and masks, a cheerful nurse observes the operation and a small single electric lamp illuminates the surgical field.
The rapid growth of Steindler's clinical program and his role in promoting legislation that brought patients to Iowa City from all parts of the state were critical for the development of the University of Iowa Hospitals and the College of Medicine. In 1925, Abraham Flexner noted that, "Iowa is now completing an adequate series of clinics16" and in a review of the growth and development of the health sciences at the University of Iowa the Iowa City Press-Citizen noted on October 6, 2002, "It was Arthur Steindler who opened the way for this modern institution [University of Iowa Health Care] by securing a steady flow of patients in the rural Midwest23." His research and the students he attracted earned the College of Medicine national and international respect. On May 10, 1927, Walter Jessup, the fourteenth president of the University of Iowa from 1916-1934, wrote to Dr. Steindler formally appointing Steindler Head of the Department of Orthopaedic Surgery and granting him $3,500 for his research25.
Through his teaching, speaking and writing Steindler encouraged basic research and incorporation of the basic sciences into orthopaedic education. In his 1933 presidential address to the American Orthopaedic Association, he emphasized the value of basic research in orthopaedics pointing out the need for study of anatomy, pathology, physiology and biochemistry48. In addition to encouraging study of the sciences, Steindler immersed himself in the investigation of human mechanics43. He felt that the mechanics of the musculoskeletal system represented a new field with great potential application and observed that "biomechanics is a powerful and indispensable ally of the orthopaedic clinician48." When discussing operative or non-operative treatment of musculoskeletal diseases and injuries he incorporated his knowledge of the biomechanics and biology of the musculoskeletal system. His book "Orthopaedic Operations 46" begins with a chapter titled "The Biology of Functional Restoration" and he states that, "A knowledge of the possibilities and limitation of tissue regeneration, and tissue adaptation is essential equipment for every orthopaedic surgeon; his judgment depends on it." In Steindler's view, orthopaedic progress would occur not through technical perfection of operations, but through advances in the basic sciences.
In his study of orthopaedic problems and their treatment, Steindler pointed out the importance of understanding the natural history of diseases and critically reviewing the results of treatment10, and some authors credit him with being the first to report on the long-term outcomes of all of his operations 40. In his publications he presented and critically analyzed his operative experience, even when the results were unsatisfactory. In his book, Orthopaedic Operations: Indications, Technique and End Results, he discussed the indications and surgical techniques for each operation46. He defined four principles that should be used to evaluate operative procedures46: 1) Is the operation rational from the physiological and mechanical point of view? 2) Does the experimental evidence corroborate the expectations of regeneration and repair placed on the operation? 3) Is the operative technique in keeping with our experimental or empirical observations? and 4) Are reliable statistics available to justify the procedure in light of definite end results?
In 1920, Steindler selected a bluff overlooking the Iowa River at the intersection of Riverside Drive and Grand Avenue as the site for a new home (Figure 12). The construction of the house and the terracing of the surrounding land was completed in 192213. Mrs. Steindler planned the landscaping and creation of gardens including stone paths, pools and bridges 13. Their home was large and located in what at the time was an attractive and pleasant location (now the site of the University of Iowa College of Law) over looking the Iowa River and with a view of the Old Capital. Above the entrance to his home, Steindler had a sentence from Horace inscribed: "Ille terrarum mihi praeter omnis anguls ridet" (The corner of the earth that smiles above all others)13, recognition that he had found a place that offered him the opportunities he had sought when he left Vienna.
Figure 12.
The Steindler's home in Iowa City on the bluff overlooking the Iowa River at the intersection of Grand Avenue and Riverside Drive.
A. The appearance of the house from Grand Avenue, the street leading from the Iowa River to the Field House.

B. Path and entrance stairway leading to the house from Riverside Drive.

C. Terraced gardens.

D. Garden paths.

In the 1930s, Steindler monitored political events in Europe closely, and became increasingly concerned about the future of Germany and Austria and the lives of family and friends in Vienna. He started traveling to Austria regularly so that he could bring people to Iowa City where they could start a new life, as he had done. He continued this practice until the political changes in Germany and Austria preceding World War II made it impossible for him to visit Vienna13. Many of these individuals, including Hans Ehrenhaft, one of the most important contributors to the development of cardiothoracic surgery and Steindler's nephew, lived in the Steindler home until they became established in the United States13.
THE VIENNA INFLUENCE
It is not difficult to see the Vienna influence in Arthur Steindler's career or in the department he founded in Iowa City. It is apparent in his research and clinical practice, teaching and in the traditions he established for Iowa orthopaedics. Eduard Albert's interest in the mechanics of joint movement and spinal deformity may have helped stimulate Steindler's studies of biomechanics and kinesiology. Like Albert and Lorenz, Steindler devoted much of his clinical practice to the care of children with developmental and paralytic deformities. Correcting deformities and stabilizing joints by arthrodeses, similar to Albert's operations, in patients crippled by polio and other neuromuscular disorders were an important part of Steindler's clinical work throughout his career44–46,52. Like his teachers, he also investigated the mechanics of scoliosis and devised a non-operative treatment for spinal curvature, compensation-derotation41,42, 50,51.
Steindler learned from Albert and Lorenz, but he did not accept everything they taught and practiced. He agreed with Ridlon's criticisms of Lorenz's treatment of developmental dislocation of the hip and noted that Lorenz's claims of the success of this treatment were exorbitant49. In his discussion of Lorenz's manipulative treatment of clubfoot he makes another rare comment concerning Lorenz, "It is well to recall at this point that the earlier surgeons (Lorenz) went much further with their conservative methods than we do today. They applied a great deal more force, and their attempts of redressement were limited by circulatory embarrassment only. In other words, anything that the circulation could stand in the way of manipulation or mechanical correction was accepted. It is in this sense that Lorenz speaks of modeling redressement. Today we find our ideas of what constitutes the tolerance to manipulation radically changed. We no longer "manipulate" as much as the circulation will stand. Our own attitude is that 90 percent of clubfeet in children can be successfully treated by conservative methods47." Steindler and Lorenz clearly had different views of what constituted modeling redressment and the outcomes of this treatment.
In Iowa City, Arthur Steindler found the opportunity he was seeking when he left Vienna in 1907, but he also created opportunities for others. He helped establish the University of Iowa as a major health science center. He became an international leader in orthopaedics and created an orthopaedic department based on the values and practices that made the University of Vienna one of the most important institutions in the history of orthopaedic surgery. Throughout his career, he emphasized the fundamental principle of the Vienna surgical tradition: excellence and innovation in the techniques of surgery combined with clinical and basic research, critical evaluation of the outcomes of operations and teaching the next generations of surgeons. Although he committed himself to his profession, students and patients, he enjoyed his time with family and friends; and, through the department he founded he enriched the lives of those who followed him.
Figure 13.
Arthur Steindler in the departmental library.
Figure 14. Steindler and his staff and residents in 1945.

Seated (left to right) Ponseti, Thornton, Steindler, Greteman, Kaplan, Leveton. Standing (Left to Right) Salguero, Silensky, Diamond, Hicks, Le Noir, Pugi-Guri, Peidrahita, Nelson, Samaniego.
ACKNOWLEDGMENTS
Arthur Steindler's nephews, Martin Steindler and Hans Ehrenhaft, provided invaluable information and insight into their uncle's life and aspirations. Webster Gelman, Dr. Steindler's colleague and friend, helped me to understand Dr. Steindler's humanity, sense of humor and values.
References
- 1.Absolon KB. The Happy Warrior: Theodore Billroth and the Franco-Prussian War. Rockville, MD: Kabel; 1994. p. 63. [Google Scholar]
- 2.Barkan H, editor. Johannes Brahms & Theodore Billroth: Letters from a Musical Friendship. Norman, OK: University of Oklahoma Press; 1957. p. 264. [Google Scholar]
- 3.Bick EM. Source Book of Orthopaedics. New York: Hafner Publishing; 1968. p. 576. [Google Scholar]
- 4.Billroth T. General Surgical Pathology and Therapeutics. In Fifty Lectures. London: Lewis; 1871. p. 676. [DOI] [PubMed] [Google Scholar]
- 5.Billroth T. The Medical Science in the German Universities: A Study of the History of Civilization. Translated from German. New York: Macmillan; 1924. p. 292. [Google Scholar]
- 6.Bowman JG. Letter to Arthur Steindler. 1913.
- 7.Bowman RC. Flexner's Impact on American Medicine. 2003. http://www.unmc.edu/Community/ruralmed/flexner.htm .
- 8.Buckwalter JA. Advancing the science and art of orthopaedics. Lessons from history. J Bone Joint Surg. (Am) 2000;82-A(12):1782–1803. doi: 10.2106/00004623-200012000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Buckwalter JA. Arthur Steindler. Orthopaedic scholar, teacher, and clinician. Clin Orthop. 2000;374:171–182. [PubMed] [Google Scholar]
- 10.Buckwalter JA. Arthur Steindler: Founder of Iowa Orthopaedics. Iowa J Orthop. 1981;1:5–12. [Google Scholar]
- 11.Buckwalter JA. Integration of science into orthopaedic practice: Implications for solving the problem of articular cartilage repair. J Bone Joint Surg. (Am) 2003;85-A(2):1–7. [PubMed] [Google Scholar]
- 12.Buckwalter JA, Brand RA. Arthur Steindler and orthopaedic research. J Ortho Res. 1999;17:1–2. doi: 10.1002/jor.1100170102. [DOI] [PubMed] [Google Scholar]
- 13.Ehrenhaft JL. Personal Communication. 2003. Iowa City.
- 14.Flexner A. Abraham Flexner: An Autobiography. New York: Simon and Schuster; 1960. p. 302. [Google Scholar]
- 15.Flexner A. Medical Education in the United States and Canada: A Report to the Carnegie Foundation for the Advancement of Teaching. New York: Carnegie Foundation; 1910. p. 346. [Google Scholar]
- 16.Flexner A. Medical Education: A Comparative Study. New York: Macmillan; 1925. p. 334. [Google Scholar]
- 17.Gerber JC. A Pictorial History of the University of Iowa. Iowa City: University of Iowa Press; 1988. p. 273. [Google Scholar]
- 18.Gordon E. Great Medical Disasters. New York: Dorset Press; 1983. p. 220. [Google Scholar]
- 19.Gross SD. The Anatomy, Physiology and Diseases of Bones and Joints. Philadelphia: John Grigg; 1830. p. 389. [Google Scholar]
- 20.Gross SD. Autobiography of Samuel D Gross. Philadelphia: G Barrie; 1887. p. 842. [Google Scholar]
- 21.Gross SD. Excision of the Bones and Joints. In: Gross SD, editor. A System of Surgery. Philadelphia: Blanchard and Lee; 1859. pp. 657–662. [Google Scholar]
- 22.Gross SD. A System of Surgery. Philadelphia: Blanchard and Lee; 1859. p. 1160. [Google Scholar]
- 23.Hibbs B. Iowa City Press-Citizen. Iowa City: 2002. Steindler Children's Hospital; p. 11A. [Google Scholar]
- 24. (Iowa University). Department of Orthopaedic Surgery. Medical Bulletin. 1941. p. 55.
- 25.Jessup WA. Letter to Arthur Steindler. 1927.
- 26.Lesky E. In: The Vienna Medical School of the 19th Century. Lesky E, editor. Baltimore: Johns Hopkins University Press; 1967. p. 604. [Google Scholar]
- 27.LeVay D. The History of Orthopaedics. Park Ridge, NJ: Parthenon Publishing Group; 1990. p. 693. [Google Scholar]
- 28.Lister J. The Collected Papers of Joseph, Baron, Lister. Oxford: Clarendon Press; 1909. p. 1018. [Google Scholar]
- 29.Liston R. Elements of Surgery. Philadelphia: EL Carey and A Hart; 1837. p. 540. [Google Scholar]
- 30.Liston R. Lectures on the Operations of Surgery. Philadelphia: Lea and Blanchard; 1846. p. 32. [Google Scholar]
- 31.Liston R. Practical Surgery. Philadelphia: Adam Waldie; 1838. p. 374. [Google Scholar]
- 32.Lorenz A. My Life and Work: The Search For A Missing Glove. New York: Charles Scribner; 1936. p. 362. [Google Scholar]
- 33.Nuland SB. The Masterful Spirit - Theodor Billroth. Delran, NJ: The Classics of Surgery Library; 1991. p. 44. [Google Scholar]
- 34.Orr HW. On the Contributions of Hugh Owen Thomas, Sir Robert Jones, John Ridlon. Springfield IL: Charles C Thomas; 1949. p. 253. [Google Scholar]
- 35.Paci A. Lussazione iliaca comune congenita del femore. Arch Ortop. 1890;7:191–197. [Google Scholar]
- 36.Peltier LF. Orthopedics: A History and Iconography. San Francisco: Norman Publishing; 1993. p. 304. [Google Scholar]
- 37.Ponseti IV. Arthur Steindler. Clin Orthop. 1959;19:1–8. [Google Scholar]
- 38.Porter R. The Greatest Benefit to Mankind. New York: 1998. –Norton.pp. 831 [Google Scholar]
- 39.Rutkow IM. American Surgery. Philadelphia: Lippincott-Raven; 1998. p. 638. [Google Scholar]
- 40.Steindler A. The classic: The biology of functional restoration. Clin Ortho Rel Res. 1983;177:4–8. [PubMed] [Google Scholar]
- 41.Steindler A. Compensation vs correction in the treatment of structural scoliosis. J Bone Joint Surg. 1926;VIII:570–586. [Google Scholar]
- 42.Steindler A. The compensation-derotation treatment in scoliosis. J Bone Joint Surg. 1939;21:51–58. [Google Scholar]
- 43.Steindler A. Mechanics of Normal and Pathological Motion in Man. Springfield IL: Thomas; 1935. [Google Scholar]
- 44.Steindler A. Operative methods and end-results of disabilities of shoulder and arm. J Orthopaedic Surg. 1921;3:652–666. [Google Scholar]
- 45.Steindler A. Operative treatment of paralytic conditions of the upper extremity. J Orthopaedic Surg. 1919;1:608–619. [Google Scholar]
- 46.Steindler A. Orthopaedic Operations: Indications- Technique and End Results. Springfield IL: Thomas; 1940. p. 766. [Google Scholar]
- 47.Steindler A. Post-Graduate Lectures of Orthopedic Diagnosis and Indications. Vol. 1. Springfield IL: Charles C Thomas; 1950. p. 285. [Google Scholar]
- 48.Steindler A. Presidential address. J Bone Joint Surg. 1933;15:567–573. [Google Scholar]
- 49.Steindler A. Ridlon and His Share in Molding Orthopedic Surgery. In: Orr HW, editor. On the Contributions of Hugh Owen Thomas, Sir Robert Jones, John Ridlon to Modern Orthopedic Surgery. Springfield IL: Charles C Thomas; 1949. pp. 215–233. [Google Scholar]
- 50.Steindler A. The treatment of scoliosis. JAMA. 1909;52:1572–1573. [Google Scholar]
- 51.Steindler A. The treatment of scoliosis by the socalled compensation method. Lancet. 1926. Jul 1, pp. 3–11.
- 52.Steindler A. The treatment of the flail ankle; panastragaloid arthrodesis. J Bone Joint Surg. 1923;5:284–293. [Google Scholar]
- 53.Steindler M. Personal Communication. 2003.
- 54.Thorwald J. The Century of the Surgeon. London: Thames and Hudson; 1957. p. 416. [Google Scholar]


