Abstract
Ulnar shortening osteotomy is a surgical treatment option for patients with symptomatic ulnar positive variance for a variety of reasons. Delayed healing and nonunion of the osteotomized sites have been reported and present problematic complications of this procedure. Studies have shown nonunion rate with transverse cuts ranging from 8-15%. The goal is to achieve parallel cuts, thus maximizing the contacting bony surface area for a better union rate. The senior surgeon attempted using a custom thick blade to insure parallel cuts. The concern is whether the heat generated during such a cut would contribute to non-union. It is our hypothesis that complications with ulnar shortening osteotomy using a thick blade are secondary to excess heat generation. When generated heat surpasses the threshold temperature of bone tissue, the organic matrix is irreversibly damaged and necrosis of the bony ends may occur. The present study measured the heat generation during ulnar osteotomy using different blade thicknesses. Thirty-five fresh turkey femurs, having similar size and cortical thickness of the human ulna, were used. Loading was done at three different speeds of 0.66, 1.0, and 1.5 mm/second corresponding respectively to 30, 20, and 10 seconds for the complete cut. A general linear statistical model was fitted relating temperature rise to three predictive factors: blade thickness, sensor distance, and initial bone temperature. There was a statistically significant relationship between temperature rise and all three predictor variables at the 99% confidence level. There was no statistically significant relationship between temperature rise and the number of cuts with the same blade up to 10 times. Compared with the single microsagital saw blade, the temperature rise for the double thickness blade was 14% higher and for the triple thickness blade was 23% higher. The temperature rise was inversely related to the speed of the cut. The temperature rise for the bone cut in 30 seconds was 1.5 times higher than the temperature rise when the bone was cut in 10 seconds. Complications with ulnar shortening osteotomy may be secondary to excess heat generation. A new thick saw blade design and the use of proper internal/external irrigation may overcome the problem.
INTRODUCTION
Patients with a relatively longer ulna than radius at the wrist (positive ulnar variance) are susceptible to a complex of degenerative changes due to the abnormally high load supported by the ulnar head 16. Positive ulnar variance can be congenital, a result of radial shortening from a malunited distal radial fracture or premature physeal closure, or dynamically produced from repetitive grip pronation3,9,17,20. Ulnar shortening is a surgical procedure to correct length discrepancy between the ulna and radius. Osteotomy at the diaphysis and removing a section of the ulna has been shown to produce good results. Often patients return to pain-free function at previous work levels2,4,6,10,11,13,19.
Problems with delayed healing or nonunion after osteotomy have been reported in the literature and complicate the shortening procedure. Oblique osteotomy was developed when inadequate compression of bone ends was implicated in nonunion cases. The placement of a lag screw across the osteotomy site provides a secondary means of compression in addition to the internal fixation plate. Nonunion rates in oblique osteotomy patients have ranged from 0-4%5 compared to 8-15% in patients with transverse osteotomy where placement of a lag screw is impossible. Though compression appears to be important in adequate healing, it does not address all of the challenges inherent in osteotomy surgery that increase the risk of complications.
Whether a surgeon is able to make parallel cuts during the osteotomy impacts how the bone ends will oppose each other. Even the most skilled surgeons may not be able to make these cuts perfectly using a freehand technique. The resulting surfaces may not match when they are fixed, leading to less bony contact. This may result in delayed healing or a nonunion requiring a bone graft. An unpublished trial by the senior surgeon investigator attempted to ensure parallel cuts by using one cut with a specially designed thick blade. The technique has been proposed by Labosky and Waggy12 who found the single cut to produce a more predictable amount of shortening than the technique of using two parallel cuts. Surprisingly, the results of the aforementioned trial were not encouraging, showing high incidence of delayed and non-union of the ulna following osteotomy and fixation.
We hypothesize that the complications associated with ulnar shortening osteotomy using the thick blade are secondary to excess heat generation. When the heat generated during osteotomy surpasses a threshold temperature, bone tissue is damaged, potentially resulting in malunion or nonunion postoperatively.
Thermal injury in bone is described as irreversible damage to the organic matrix from exposure to an elevated temperature. Early studies described the damage in terms of temperatures in which key proteins were denatured. Matthews and Hirsch found bone alkaline phosphatase was inactivated in vitro at 56°C15. Bonfield and Li attributed mechanical alteration of bone after heating to 50°C to the reorientation of collagen molecules1.
More recent research has focused not only on maximum tolerable temperatures but also on duration of exposure at an elevated temperature. Lundskog demonstrated an exponential increase in inactivity of diaphorase in the osteocyte, dependent both on the exposure temperature and the duration of heat exposure; necrosis was initiated at 50°C14. Rouiller and Majno described necrosis in the long bones of rabbits when exposed to temperatures of 55°C for one minute18. Most recently, Eriksson's microscopic studies of living bone tissue have shown bone to be more sensitive to heat than previously thought. He demonstrated that a temp of 47°C maintained for one minute severely impaired bone regeneration7,8.
Our study seeks to quantify the temperature increase in cortical bone while cutting with microsagittal saw blades of varying thickness. We hypothesize that thicker blades will generate temperature increase above baseline (ΔT≈H 10°C) that would begin to cause damage to the bone matrix if occurring in vivo.
METHODS
Thirty-five fresh turkey femurs, having similar size and thickness of the human ulna, were obtained from a local butcher, stripped of flesh, and frozen until needed. Hours before a testing session the bones were removed and allowed to warm to room temperature. Two cuts were made on each individual bone. Serial bone crosssection revealed an area of uniform thickness on the posterior aspect of the femurs. This area of 3-4 mm thickness was where we embedded the temperature sensors during cutting. Holes for temperature probes were drilled in the bone cortex. The holes were placed as close as possible to the intended line of cut of the saw blade (0.5-2mm). A thermoconductive paste was applied to the holes to rapidly transfer heat generated to the probes.
The bone specimen was held in a custom designed chuck mounted to an 85.8 Bionix System MTS moving load frame. The chuck and bone were lowered onto a Microaire microsagittal 2250 hand piece which inserted the blade, driven by compressed nitrogen at 95 pound per square inch (psi) (Figure 1). The blades were used in the single, double, or triple configuration (Figure 2). Double and triple blades are simply two and three single blades spot-welded together respectively. The hand piece was anchored to the floor of the MTS with a custom built vise (Figure 1). The bone was cut with the single width blade at three different feed rates, 0.66, 1.0, and 1.5 mm/second, corresponding, respectively to 30, 20, and 10 seconds for a complete cut. The double and triple width blades were evaluated only at the 0.66 mm/sec feed rate. Fourteen cuts were made for each combination of blade type and feed rate.
Figure 1.
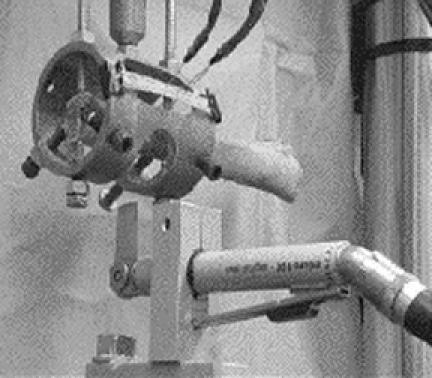
This picture shows the positioning of the bone and the saw blade in the testing machine. The bone specimen was held in a custom designed chuck, which was attached to the moving load frame of MTS. The oscillating saw was fixed to the floor of the MTS load frame and kept stationary. The three thermocouple probes are also shown in the picture.
Figure 2.
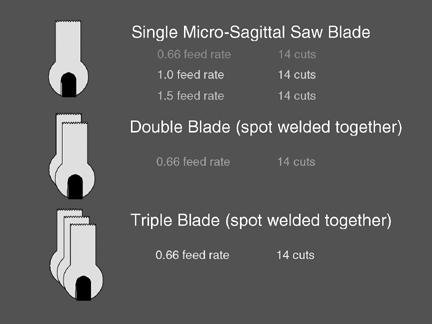
This figure indicates the number of cuts and the associated speed of the cut for single, double, and triple blades used in the study. Double and triple blades are simply two and three single blades spot-welded together, respectively.
Temperature measurements were made through three Exacon type T-N0605 thermocouple probes mated with a computer workstation. The probes were held in the bone cortex by a length of surgical tubing stretched to provide some forward pressure on the probes (Figure 1). The computer interface measured temperature input from the probes versus time. Recording began before cutting commenced and continued for 1-1.5 min after cut was complete to allow bone to cool back to room temperature. After each cut, calipers were used to measure the distance of each probe from the line of cut. Major and minor diameters of the femur were recorded at the cut site, as well as the number of cuts that were made with each blade to gauge any effect of blade wear on temperature.
A general linear statistical model was fitted relating temperature rise to three predictive factors: blade thickness, sensor distance from the cut, and initial bone temperature. Other variables included, number of cuts per blade, and speed of the cut. A p-value less than 0.05 was considered as statistically significant.
RESULTS
Figure 3 shows the temperature rise as a function of time for three different speeds of 0.66, 1.0, and 1.5 mm/second corresponding, respectively, to 30, 20, and 10 second for the complete cut. Figure 4 shows the average temperature rise and its standard variation as a function of blade thickness.Figure 5 represents a three-dimensional configuration of temperature rise as a function of both sensor distance from the cut and the initial bone temperature. Figure 6 represents a threedimensional configuration of temperature rise as a function of both the speed of cut and the sensor distance from the cut. There was a statistically significant relationship between temperature rise and all three predictor variables at the 99% confidence level. Compared with the single micro-sagittal saw blade, the temperature rise for the double thickness blade was 14% higher and for the triple thickness blade was 23% higher. The temperature rise was inversely related to the speed of the cut. The temperature rise for the bone cut in 30 seconds was 1.5 times higher than the temperature rise when the bone was cut in 10 seconds. There was no statistically significant relationship between temperature rise and the number of cuts with the same blade up to ten times.
Figure 3.
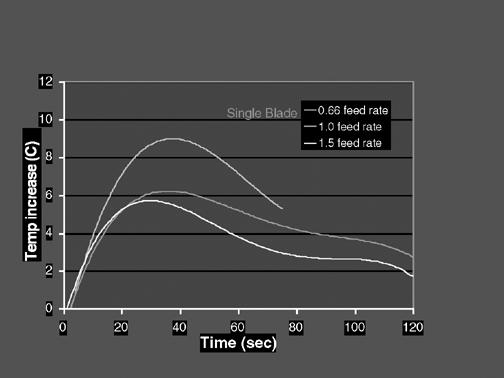
This figure shows the temperature rise as a function of time for three different speeds of 0.66, 1.0, and 1.5 mm/second, corresponding respectively to 30, 20, and 10 seconds for the complete cut.
Figure 4.
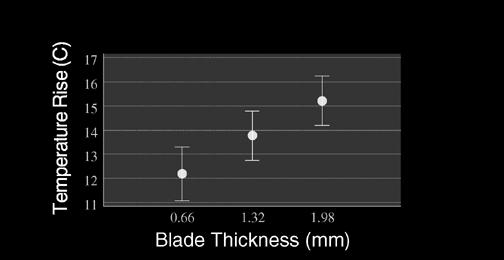
This figure shows the overall average temperature rise and its standard variation as a function of blade thickness.
Figure 5.
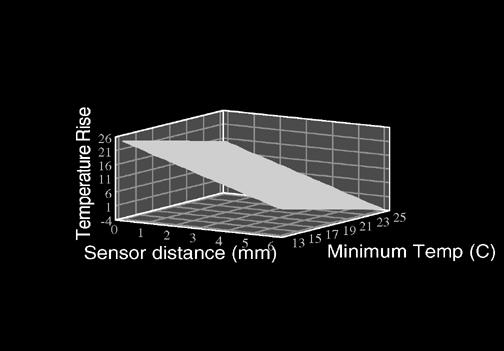
This figure represents a three-dimensional configuration of temperature rise as a function of both sensor distances from the cut and the initial bone temperature.
Figure 6.
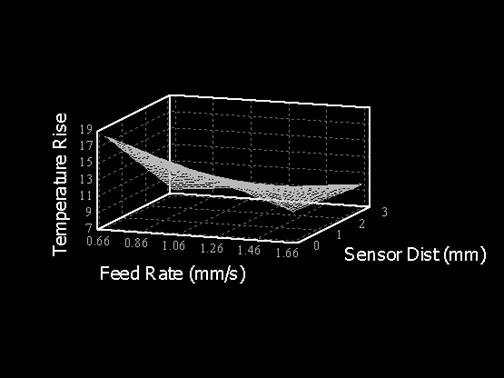
This figure represents a three-dimensional configuration of temperature rise as a function of both the speed of cut and the sensor distance from the cut.
DISCUSSION
For a variety of reasons, ulnar shortening osteotomy is a surgical treatment option for patients with symptomatic ulnar positive variance. The ulnar osteotomy is technically challenging using either free-hand techniques or guided systems to ensure parallel cuts. Oblique osteotomy fixed with lag screws, although more technically challenging, can improve clinical outcome. The placement of a lag screw across the osteotomy site provides a secondary means of compression in addition to the internal fixation plate. Nonunion rates in oblique osteotomy patients have ranged from 0-4%5 compared to 8-15% in patients with transverse osteotomy where placement of a lag screw is impossible. For the case of transverse osteotomy, the goal is to achieve parallel cuts, thus maximizing the contacting bony surface area. Union rates should increase with greater bony contact.
Using thick saw blades for the osteotomy greatly reduces the technical challenge of the procedure as parallel cuts are assured each time with a free-hand technique. Unfortunately, delayed union and nonunion are a common complication with this procedure. Thermal injury to bone may occur during the osteotomy, thus increasing the risk for poor healing. Our study found the temperature rise for the double thickness blade was 14% higher than the single, and 23% higher for the triple thickness blade. We also found the speed of the cut to be a significant factor. The higher the speed, the lower the temperature rise.
Ulnar shortening osteotomy presents many challenges technically, yet provides great benefit clinically for many patients. This is a useful surgical option, and developing ways to minimize the complications of delayed union and nonunion would make it an even more appealing one as well. Limitations of the current study included the following: lack of in vivo study, initial bone temperature did not match body temperature, and the effect of irrigation on heat removal was not studied.
CONCLUSION
Complications with ulnar shortening osteotomy may be secondary to excess heat generation. A new thick saw blade design and use of proper internal/external irrigation my overcome the problem.
ACKNOWLEDGMENT
The study was supported by George E. Omer, Jr., MD, Research foundation. Statistical analysis was provided by Dan Tandberg, MD.
Footnotes
This study was supported, in part, by the Dedicated Health Research Funds of the University of New Mexico School of Medicine
Part of this study was presented at the 20th Annual University of New Mexico Orthopaedic Alumni Conference June 8-9, 2001
References
- 1.Bonfield W, Li CH. The Temperature Dependence of the Deformation of Bone. J Biomechanics. 1968;1:323–329. doi: 10.1016/0021-9290(68)90026-2. [DOI] [PubMed] [Google Scholar]
- 2.Boulas HJ. Ulnar shortening for tears of the triangluar fibrocartilage complex. Journal of Hand Surgery. 1990;15A:415–420. doi: 10.1016/0363-5023(90)90052-s. [DOI] [PubMed] [Google Scholar]
- 3.Bowers WH. Distal radioulnar joint. In: Green DP, editor. Operative hand surgery. 4th Edition. New York: Churchill Livingstone; 1997. pp. 1015–1019. [Google Scholar]
- 4.Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. Journal of Hand Surgery. 1993;18A:46–53. doi: 10.1016/0363-5023(93)90243-V. [DOI] [PubMed] [Google Scholar]
- 5.Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG. Comparison of ulnar shortening osteotomy and the wafer resection procedure as treatment for ulnar impaction syndrome. Journal of Hand Surgery. 2000;25A:55–60. doi: 10.1053/jhsu.2000.jhsu025a0055. [DOI] [PubMed] [Google Scholar]
- 6.Dos Reis FB, Katchburn MV, Faloppa F, Albertoni WM, Filho JL. Osteotomy of the radius and ulna for the Madelung deformity. 1998;80-B(5):817–824. doi: 10.1302/0301-620x.80b5.8691. [DOI] [PubMed] [Google Scholar]
- 7.Eriksson AR. Heat induced bone tissue injury. Dissertation, University of Gothenburg, Goteborg. 1984.
- 8.Eriksson AR, Albrektsson T. The effect of heat on bone regeneration: an experimental study in the rabbit using the bone growth chamber. J Oral Maxillofac Surg. 1984;42:705–711. doi: 10.1016/0278-2391(84)90417-8. [DOI] [PubMed] [Google Scholar]
- 9.Friedman SL, Palmer AK. The ulnar impaction syndrome. Hand Clinics. 1991;7(2):295–310. [PubMed] [Google Scholar]
- 10.Hulsizer D, Weiss AC, Akelman E. Ulna-shortening osteotomy after failed arthroscopic debridement of the triangular fibrocartilage complex. Journal of Hand Surgery. 1997;22A:694–698. doi: 10.1016/S0363-5023(97)80130-X. [DOI] [PubMed] [Google Scholar]
- 11.Koppel M, Hargreaves IC, Herbert TJ. Ulnar shortening osteotomy for ulnar carpal instability and ulnar carpal impaction. [Journal of Hand Surgery]. 1997;22B:451–456. [Google Scholar]
- 12.Labosky DA, Waggy CA. Oblique ulnar shortening osteotomy by a single saw cut. Journal of Hand Surgery. 1996;21A:48–59. doi: 10.1016/S0363-5023(96)80153-5. [DOI] [PubMed] [Google Scholar]
- 13.Loh YC, Van Den Abbele K, Stanley JK, Trail IA. The results of ulnar shortening for ulnar impaction syndrome. Journal of Hand Surgery. 1999;24B:316–320. doi: 10.1054/jhsb.1999.0062. [DOI] [PubMed] [Google Scholar]
- 14.Lundskog J. Heat and bone tissue. An experimental investigation of the thermal properties of a bone tissue and threshold levels for thermal injury. Scand J Plast Reconstr Surg. pp. 1–80. [PubMed]
- 15.Matthews LS, Hirsch C. Temperatures measured in human cortical bone when drilling. J Bone and Joint Surgery. 1972;54:297–308. [PubMed] [Google Scholar]
- 16.Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clinical Orthopaedics and Related Research. 1984;187:26–35. [PubMed] [Google Scholar]
- 17.Richards RR. Chronic disorders of the forearm. Journal of Bone and Joint Surgery. 1996;78-A(6):916–930. doi: 10.2106/00004623-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Rouiller M, Majno G. Morphologische und chemische untersuchungen an Knochen nach Hitzeeinwirkung. Beitr Path Anat. 1953;113:100–120. [PubMed] [Google Scholar]
- 19.Salon A, Serra M, Pouliquen JC. Long-term follow-up of surgical correction of Madelung's deformity with conservation of the distal radioulnar joint in teenagers. Journal of Hand Surgery. 2000;25B:22–25. doi: 10.1054/jhsb.1999.0304. [DOI] [PubMed] [Google Scholar]
- 20.Tomaino MM. Ulnar impaction syndrome in the ulnar negative and neutral wrist. Journal of Hand Surgery. 1998;23B:754–757. doi: 10.1016/s0266-7681(98)80090-9. [DOI] [PubMed] [Google Scholar]


