Abstract
The Bernese Periacetabular Osteotomy (PAO) is an operation designed to relieve hip pain and improve function in patients with symptomatic dysplastic hips. The short-term results of the Bernese PAO indicate that there is a learning curve but most patients with dysplasia and mild arthritis have excellent pain relief. Outcomes and complications are the primary focus of discussion. Operative data and complications from the first 36 patients undergoing the Bernese PAO at the University of Iowa have been comparable to those reported in the literature.
INTRODUCTION
Development dysplasia of the hip (DDH) is a heterogeneous disorder that can lead to disabling hip pain and degenerative arthritis. The main pathoanatomic component is osteoarticular deficiency of the acetabulum with deficient lateral and anterior coverage of the femoral head. This acetabular deficiency substantially alters force transmission across the hip, subjecting the acetabulum and femoral head to increased and abnormally directed contact stresses1. Chronic abnormal stresses eventually can lead to subluxation and endstage arthritis of the hip.
Patients with DDH who develop hip pain and subluxation are at nearly uniform risk to progress to endstage arthritis. Unfortunately, many of these patients are young adults. Total hip arthroplasty is an outstanding option for elderly patients with disabling hip arthritis, but it is a much less desirable option in young patients. Ganz developed the Bernese periacetabular osteotomy (PAO), an operation designed to improve femoral head coverage by reorienting the shallow acetabulum, to relieve hip pain and slow the progression of arthritis in patients with symptomatic DDH who were young4. In this review, early and medium-term outcomes on Ganz's original patients and results from several other centers are reviewed. Finally, early operative and radiographic results as well as complications from the first 36 cases performed at the University of Iowa are presented.
REVIEW OF CLINICAL LITERATURE
The operation was originally described by Ganz in 1988 and often bears his name4. Ganz et al. reported on the initial 75 patients treated with the Bernese PAO. The authors cited several advantages compared to other innominate osteotomies. They emphasized that the Bernese PAO could achieve greater corrections which was especially advantageous in severely dysplastic hips. Secondly, they emphasized that the structural continuity of the pelvic ring is not disrupted, eliminating necessary postoperative immobilization or traction. Finally, they felt the Bernese osteotomy was technically easier than several of the described spherical osteotomies. However, patient follow-up was too short to report on any outcomes.
The authors emphasized that the operation has a learning curve, with substantial decreases in operative time and blood loss occurring throughout the series. They also noted clinically substantial complications occurred in the first 18 cases including several intraarticular osteotomies, several malpositioned fragments, a transient femoral nerve palsy, several cases of resubluxation of the femoral head, and four cases of heterotopic bone formation. They concluded that there is a significant learning curve but the operation had excellent potential to help young patients with symptomatic acetabular deficiency.
Trousdale et al. reported on 42 patients from Ganz's original series who had a diagnosis of DDH at an average of 4 years (2-8 years) after surgery9. Overall, Harris hip scores improved from 63 to 86 following surgery. The authors noted that the amount of preoperative arthrosis correlated with postoperative outcome. Patients with mild to moderate arthrosis (Tonnis Grades 0-2) had substantial improvements in their hip scores compared to patients with Grade 3 osteoarthrosis which showed little benefit. Five of the 6 patients who progressed to total hip arthroplasty had Grade 3 osteoarthrosis prior to their PAO. The authors reported no major neurovascular complications. One patient required resection of heterotopic bone and one required neurolysis of the lateral femoral cutaneous nerve. Overall, the authors demonstrated that the Bernese PAO provided dramatic pain relief and improved function in selected patients with DDH who had minimal to mild pre-existing arthritic changes in their hips. They cautioned that the osteotomy was not a predictable operation for patients with advanced arthritic changes.
Recently, several other centers have reported short-term results on patients treated with the Bernese PAO2,5,7,10. Matta et al. reported on 66 hips treated with the Bernese PAO in 58 patients with an average followup of 4 years5. They had a similar experience in that patients with minimal to moderate preoperative arthritic changes (Grade 0 - 2) had 78% to 85% good or excellent results, and patients with Grade 3 arthritic changes had 33% good or excellent results. Three of the 5 patients who eventually required total hip arthroplasty had grade 3 osteoarthritic changes. Overall, the authors' results supported the Bernese PAO as an excellent option for symptomatic young patients with mild to moderate arthritic changes resulting from DDH. Crockarell et al. reviewed 21 patients treated with the Bernese PAO with an average follow-up of 3.2 years 2. Overall, Harris Hip scores improved from 68 preoperatively to 86 postoperatively. Trumble et al. reported results on 124 Bernese PAO's performed on 115 patients with an average follow-up of 4.3 years 10. Overall, Harris Hip scores improved from 65 preoperatively to 89 postoperatively. The authors' noted that preoperative arthrosis correlated with outcome. Patients with grades 0, 1, and 2 arthritic changes achieved Harris Hip scores of 89 - 92. Patients with grade 3 changes had an average Harris Hip score of 77. Murphy et al. reported on 135 Bernese PAO's performed on 130 patients with an average follow-up of 3.9 years7. Five hips, all with grade 3 arthrosis preoperatively, progressed to total hip arthroplasty. The authors did not specify outcomes for the remaining 130 hips.
Davey and Santore specifically reviewed complications occurring in the senior author's first 35 cases compared to his second 35 cases3. They categorized complications as major, moderate, and trivial. Major complications included 2 bleeding complications, reflex sympathetic dystrophy in 2 patients, one sciatic nerve palsy, one pulmonary embolus, and one ileum nonunion. Most notably, major complications decreased from 17% in the first group to 2.9% in the second group. Of note, none of the major complications had any substantial long-term sequela. Moderate complications included 3 ischial fractures, 2 superficial wound problems, 1 posterior column fracture, and 3 peroneal neuropraxias, none of which had any sequela. Matta et al. reported no major complications 5. One patient underwent excision of symptomatic heterotopic ossification. Crockarell reported two intraarticular osteotomies in 21 patients that affected their ability to correct the dysplasia and two peroneal nerve palsies2. In Trumble's series, 3 patients had major arterial thromboses (2 femoral and 1 iliac) that required emergent intervention10. All of these occurred in patients treated through an ilioinguinal approach and the authors subsequently have abandoned this approach. They reported 2 deep infections requiring multiple debridements and they also had to evacuate 5 postoperative hematomas.
In summary, short-term outcomes from multiple centers have remarkably consistent results. Patients with minimal to moderate arthritic changes usually achieve substantial pain relief and improved function. Conversely, patients with advanced radiographic arthritic changes had much less predictable success. There is a substantial learning curve in performing the operation. Major complications tended to occur early in all authors' series and this was shown to be statistically significant by Davey and Santore3. Infection rates are uniformly low. Vascular problems in patients operated through an anterior approach are minimal. The most clinically significant complications have been intraarticular osteotomies. Finally, surgical corrections were markedly consistent (Table 1). The operation allows substantial three-dimensional improvement of femoral head coverage.
TABLE 1. Magnitude of Correction.
Magnitude of correction of the Lateral Center Edge Angle, Anterior Center Edge Angle, Acetabular Index, and Femoral Head Medialization for four previously reported series and the current series at the University of Iowa. Values represent differences between preoperative and postoperative values.
| Lateral Center Edge Angle (Degrees) | Anterior Center Edge Angle (Degrees) | Acetabular Index (Degrees) | Femoral Head Medialization (millimeters) | |
|---|---|---|---|---|
| Siebenrock | 28 | 22 | 20 | 6 |
| Matta | 28 | 28 | 22 | 6 |
| Crockarell | 22 | 44 | N/A | N/A |
| Trumble | 23 | 25 | 17 | 5 |
| McKinley | 24 | 26 | 19 | 4 |
Siebenrock et al. were the first to report longer-term results on 71 of the original 75 patients operated on by Ganz8. Fifty-eight of 71 (82%) hips had been preserved over a mean follow-up period of 11.3 years. Hip reconstruction was performed at a mean of 6.1 years after the PAO in the 13 patients who did not preserve their hips. Fifty-two of the 71 hips (73%) were graded good or excellent by the Harris hip score and the D̕Aubigne hip score. Eighty percent of preserved hips had grade 0 or 1 osteoarthritis. Again the authors found that advanced radiographic preoperative arthritis was a strong predictor of poor outcome.
UNIVERSITY OF IOWA EXPERIENCE
From October 2000 through February 2003, 36 Bernese PAO's have been performed on 30 patients at the University of Iowa by a single surgeon. This report summarizes preoperative and postoperative radiographic corrections, quantifies perioperative data, and details complications of these initial consecutive 36 operations. Patients include 24 women and 7 men with an average age of 33 years (+/- 7.9 years; range 15 -47 years). The typical patient is a young woman with an unexplained, insidious history of progressive buttock or groin pain that has lasted approximately 6 months to several years. The pain is often mistaken for low back pain and a substantial percentage of patients have been treated for mechanical back pain.
Typical physical findings include fairly normal range of motion but substantial exacerbation of pain with flexion, adduction, and internal rotation. Standard radiographic examination begins with a standing AP xray of the pelvis to determine lateral femoral head coverage (lateral center edge angle), determine the slope of the roof of the acetabulum (acetabular index), and judge pre-existing arthritic changes (Figure 1). A false profile view (standing lateral of the affected hip which is rotated approximately 20 degrees anterior to the unaffected hip) is obtained to determine anterior coverage of the femoral head (anterior center edge angle) (Figure 1). An obturator oblique view is obtained to judge posterior coverage of the femoral head. An AP of the pelvis with the affected hip in maximum abduction and internal rotation combined with a false profile view in flexion allow assessment of how the hip joint will appear after correction.
Figure 1.
Preoperative and postoperative AP and false profile x-rays of a 34 year old woman with left hip pain and dysplasia.
Figure 1A.
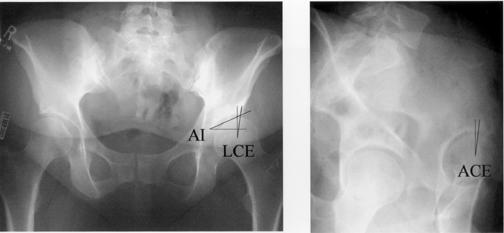
Preoperative lateral center edge angle (LCE) was 7 degrees, anterior center edge angle (ACE) was 5 degrees, and acetabular index (AI) was 28 degrees.
Figure 1B.
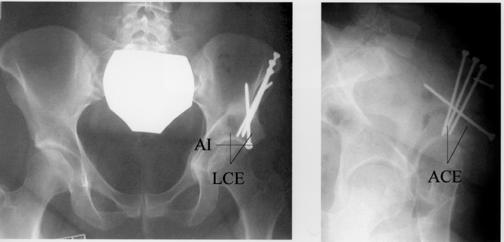
Postoperative x-rays demonstrate an LCE of 36 degrees, an ACE of 30 degrees, and an AI of 0 degrees.
Normal hips have a lateral center edge angle (LCE) and anterior center edge angle (ACE) greater than 25 degrees. The acetabular index (AI) is 8 degrees or less showing a horizontal roof of the acetabulum. In dysplastic hips, radiographs show deficient coverage of the lateral and anterior femoral head due to a shallow acetabulum (Figure 1A). The degree of lateral deficiency compared to anterior deficiency of the acetabulum is highly variable; therefore three-dimensional CT scans are obtained on all patients to aid in planning intraoperartive correction. In the 36 hips in this series, the mean preoperative lateral center edge angle was 8 degrees, anterior center edge angle was 5 degrees, acetabular index was 20 degrees, and Shenton's line was broken in 10 hips.
Surgery is performed through a modified anterior approach5. The acetabulum is mobilized through a series of cuts maintaining the continuity of the pelvic ring 4. Meticulous care is taken to optimize the final position of the acetabulum. The goal is a femoral head that is medialized and well centered under a horizontal roof of the acetabulum. This is judged on AP and false-profile views taken with fluoroscopy and a hard-copy intraoperative AP pelvis radiograph. Care is taken to avoid uncovering to posterior aspect of the femoral head by overcorrecting anterior coverage or retroverting the acetabulum. This is checked with obturator oblique fluoroscopic view and the AP pelvis x-ray. Once the fragment is positioned, it is secured with four screws (Figure 1B). In the 36 hips in this series, the mean postoperative lateral center edge angle was 32 degrees, anterior center edge angle was 31 degrees, acetabular index was 1 degree (Figure 1B).
Average operative time was 217 minutes and blood loss averaged 956 ml for all 36 patients. Average operative time for the first 18 patients was 237 minutes ( +/- 40 minutes; range 195 - 348 minutes) compared to 197 minutes (+/- 36 minutes; range 144 - 287 minutes) for the second 17 patients (p = 0.003) (Figure 2). Average blood loss for the first 18 patients was 1147 ml (+/- 681 ml; range 600 - 2800 ml) compared to 766 ml (+/- 353 ml; range 300 - 1500 ml) for the second 17 patients (p = 0.04) (Figure 3). Patients are allowed touch-down weightbearing for the first eight postoperative weeks and then progress as tolerated. The vast majority of patients are full weightbearing by three months after surgery and have returned to laboring occupations by six months. Patients with sedentary occupations are usually back to work within two months.
Figure 2. Operative Time.
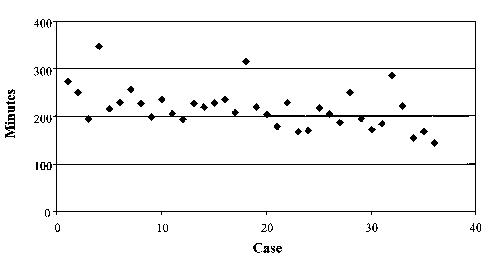
Operative time for 36 patients undergoing the Bernese PAO at the University of Iowa.
Figure 3. Blood Loss.
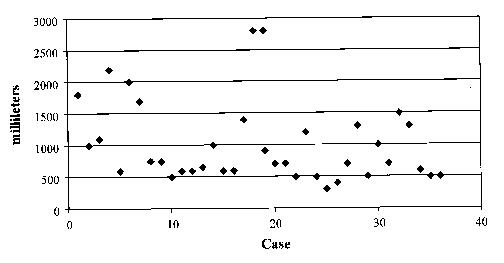
Estimated blood loss for 36 patients undergoing the Bernese PAO at the University of Iowa.
There have been six major complications in the whole series. These include four poor corrections, one peroneal nerve palsy, and one case of post-operative pulmonary edema. Minor complications include seven cases of superficial wound problems and one case of asymptomatic heterotopic bone.
Two cases with poor corrections occurring early in the series (cases 1 and 4) were overcorrected with excessive anterior coverage. Both patients have had substantial clinical improvement but have not had complete resolution of pain. Two cases later in the series (cases 28 and 32) were undercorrected. One of the cases of undercorrection involved a 47 year old woman with severe dysplasia and preoperative hip subluxation. Radiographs taken two months after surgery showed her hip had resubluxated, however her acetabular fragment appeared well healed and unchanged in position. Her acetabulum was undercorrected, and her substantial femoral valgus deformity had been ignored. She is currently scheduled for a varus proximal femoral osteotomy. The second case of undercorrection (case 32) was a difficult case in a 41 year old male with moderate to advanced arthritic changes. This patient had a prolonged operation and suffered postoperative pulmonary edema requiring four days of mechanical ventilation. Review of preoperative abduction with internal rotation radiographs demonstrated poor improvement of joint space. In retrospect, the patient was a poor candidate for acetabular realignment.
There has been one postoperative peroneal nerve palsy (case 8). This patient had a proximal femoral osteotomy concurrent with her PAO. The patient has subsequently recovered some ankle and great toe dorsiflexion but still requires a shoe insert for persistent footdrop. Most patients have experienced transient numbness in the distribution of the lateral femoral cutaneous nerve, which typically resolves. No patients have had any ongoing complaints due to dysfunction of the lateral femoral cutaneous nerve.
There have been no intraarticular osteotomies or inadvertent fractures during surgery. There has been a substantial incidence (7 of 36 cases) of superficial wound dehiscence at the apex of the curved incision in the region of the ASIS. This problem has occurred only in obese patients. One patient did not respond to local wound care and required an operative debridement and repeat wound closure 6 weeks postoperatively. She has subsequently healed with no sequela. The other 6 patients responded to wet-to-dry dressing changes and a 10 day course of cephalexin. Obese patients now have their skin closed with monofilament, interrupted sutures, avoiding subcuticular techniques.
Only 13 patients have at least two years follow-up making it too early to report outcomes from this series. However, the majority of patients have had complete to nearly complete pain relief. Radiographic corrections are detailed in Table 1. Values compare well with other reports in the literature demonstrating the substantial correction of acetabular dysplasia which can be achieved with the Bernese PAO.
DISCUSSION
This consecutive series clearly demonstrates the significant learning curve associated with the Bernese PAO. Surgical complications have occurred throughout the entire case series, including two poor corrections later in the series (cases 28 and 32). The poor surgical corrections are likely the most significant complications in this series of patients. Fortunately, other serious complications including vascular injuries, neurologic injuries, and deep infections are rare in the current series and in other reports. Operative time and blood loss showed a significant improvement in the second 18 cases and figures 2 and 3 suggest they have not plateaued.
Outcomes from the current series are unknown. However, the majority of patients have enjoyed dramatic pain relief and have substantially improved their daily function. Outcomes from other authors reporting early results (mean postoperative periods of 3.2 - 4.3 years) have been consistently good, especially in patients who meet ideal indications. Siebenrock et al. have shown that the consistent early success reported by several institutions held up for greater than ten years, casting optimism for longer-term success of the Bernese PAO.
The literature strongly suggests that young patients with dysplastic hips and minimal to mild arthritic changes are ideal candidates for this operation. Patients with moderate arthritic changes have also consistently fared well. The operation becomes less predictable with advanced preoperative arthritic changes. However, the literature demonstrates that even a substantial percentage of patients with advanced arthritic changes (grade 2 and 3) have good short-term and medium term outcomes. The difficult patient becomes increasingly clear from the literature: a young patient with dysplasia with advanced arthritic changes. The PAO is less predictable but arthroplasty in a 20 to 40 year old active patient is undesirable. Murphy and Deshmukh have shown that patients with advanced arthrosis that improved their joint space with functional radiographs predictably improved with the PAO, even with advanced arthrosis. Functional radiographs included comparing anterior/posterior views with the hip in neutral position compared to the hip in maximum abduction and internal rotation. They also looked at false-profile radiographs with the hip extended compared to the hip flexed. Improvements in joint space on both views correlated with good outcomes in patients with advanced preoperative arthritic changes.
As with any major elective intervention, careful consideration of the ratio of benefits and risks dictate proper indications. Davey and Santore demonstrated complication rates significantly decrease with experience. More importantly they found that the major complications encountered by their patients left no long-term sequela. In general, patients undergoing the Bernese PAO are young and healthy, allowing them to tolerate and recover from predictable perioperative complications. While only one-half the size of Davey and Santore's series, the current series had similar findings. Complications with this operation occur but patients tend to overcome them and enjoy substantial benefits from acetabular realignment.
In conclusion, the Bernese PAO remains a technically demanding operation that has potential to profoundly improve patient function and prolong the useful life of dysplastic hips. The ideas conceived, executed, and taught by Ganz have now achieved reproducible short-term success, and in one report, continued longerterm success. While complications should be expected, they decrease with experience and usually cause minimal long-term sequela. Fortunately, patient outcomes have justified expected complications.
References
- 1.Brand RA. Hip Osteotomies: A Biomechanical Consideration. J Am Acad Orthop Surg. 1997;5(5):282–291. doi: 10.5435/00124635-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Crockarell J, Jr, Trousdale RT, Cabanela ME, Berry DJ. Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop. 1999;363:45–53. [PubMed] [Google Scholar]
- 3.Davey JP, Santore RF. Complications of periacetabular osteotomy. 1999Clin Orthop. 363:33–37. [PubMed] [Google Scholar]
- 4.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop. 1988;232:26–36. [PubMed] [Google Scholar]
- 5.Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop. 1999;363:21–32. [PubMed] [Google Scholar]
- 6.Murphy S, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop. 2002;405:168–174. [PubMed] [Google Scholar]
- 7.Murphy SB, Millis MB, Hall JE. Surgical correction of acetabular dysplasia in the adult. A Boston experience. Clin Orthop. 1999;363:38–44. [PubMed] [Google Scholar]
- 8.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop. 1999;363:9–20. [PubMed] [Google Scholar]
- 9.Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg. (Am) 1995;77(1):73–85. doi: 10.2106/00004623-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy. Minimum 2 year follow-up in more than 100 hips. Clin Orthop. 1999;363:54–63. [PubMed] [Google Scholar]


