Abstract
Patients with lower back or buttock pain that radiates into the posterior or lateral leg are often referred to physical therapy with a diagnosis of sciatica. Often the physical exam does not reveal neurologic findings indicative of radiculopathy. Instead, there is hip abductor muscle pain and weakness. This syndrome involves muscle imbalances that result in overuse strain of the gluteus medius and gluteus minimus muscles, myofascial trigger points, and trochanteric bursitis. This paper describes hip abductor pain syndrome and provides a rationale for the diagnosis and treatment.
INTRODUCTION
Low back pain is widely recognized as a common reason for health care visits. However, frequently the main complaint is not back pain per se, but "hip" or buttock pain, often extending to the lateral thigh or calf. Patients with these complaints are commonly referred to physical therapy with a diagnosis of "sciatica," which connotes nerve root irritation or pressure causing pain in the distribution of the sciatic nerve.16 However, when the physical exam for this type of presentation reveals no neurologic deficits or neural tension signs, perhaps the more appropriate terminology would be "pseudosciatica." This paper provides a rationale and guide for explaining diagnostic conclusions, as well as symptom control for patients with this type of presentation. Rationale and treatment recommendations are based on physical exam and basic neuromuscular principles relating to problems with muscle length, strength, and motor recruitment. These patients typically complain of predominant hip and buttock pain, which worsens with prolonged standing or sitting, long bouts of walking, and with lying on the involved side. Physical exam for suspected spine problems usually focuses on lumbar spine mechanical findings, neurologic findings, and the absence or presence of tension signs. It is important to be thorough in this examination as radiculopathy involves a much different diagnostic and treatment process than referred pain. Patient history as well as the physical exam can often help to rule out serious pathology (infection, tumor, neurologic deficit, etc). However, when the neurologic exam is negative, further examination is required. There is often palpation tenderness in the gluteal muscles lateral to the posterior superior iliac spine (PSIS) and/or out toward the trochanter. In fact, studies indicate that as many as 20% of patients seen in a spine specialty clinic actually have trochanteric bursitis.21 Manual muscle testing usually reveals hip abduction using tensor fascia lata (TFL) is normal. However, testing hip abduction with extension using the posterior gluteus medius (PGM) is very weak, testing no more than 3/5. It may be painful as well.
RATIONALE
Muscle performance is a critical aspect of movement that can influence tissue stress.14 A commonly observed muscle imbalance present in those with posterior pelvic pain involves abnormal length, strength and motor recruitment of the PGM and TFL. The posterior portion of the gluteus medius muscle performs hip abduction with extension as well as some lateral rotation.11 Often, a motor pattern fault involving habitual preference of the tensor fascia lata (TFL) in performing hip abduction movements can result in posterior gluteus medius disuse weakness and atrophy.19,23 Specifically, this muscle imbalance presents as a lengthened/weakened PGM and a shortened/strong TFL, with preferred recruitment of TFL over PGM for hip abduction. For many, this imbalance may exist without any symptoms. However, when the PGM is overloaded/overused a strain may occur. This can be due to several factors involving overuse. Injury may occur by either high magnitude stress over a brief time, low magnitude stress over a long time, or moderate stress repeated many times.14 For instance, weight gain greatly increases the demand on the PGM during gait and standing, which may explain the prevalence of this problem in pregnant women.6,17 In fact, one study indicated posterior pelvic pain to be four times more prevalent than lumbar pain in pregnant women.17 Postural habits such as standing on one leg with the pelvis dipped to the other side or side lying with the top leg flexed and adducted over the other leg can result in adaptive lengthening of the PGM.19 A Trendelenburg gait pattern results in both adaptive lengthening of the PGM and trochanteric bursal irritation.
Muscle strain injury is painful and is usually the predominant symptom. Persistent muscle guarding due to injury may cause relative ischemia due to muscle tension.1,2 The "vicious cycle" of pain, increased muscle tension, decreased capillary fill, lactic acid build up, and pain is often self-perpetuating. This is thought to be the mechanism for myofascial "trigger points" and pain referral patterns.22 The pain referral patterns for the gluteal muscles are well mapped out by Travell and others (Figure 1).7,9,10
Figure 1.

Trigger points (TP) with pain referral patterns (arrows) into the low back, sacrum, buttock, and leg that mimic S1 and L5 radiculopathy.
Sometimes the bursal irritation due to the laxity caused by the PGM length and strength problems is the most prominent. Palpation in the bursal area is exquisitely painful. Weakness of PGM resulting in a Trendelenburg sign may also contribute to lumbar pain due to abnormal segmental movement of the lumbar spine if the pelvis is not stable during gait or standing. The lumbar facets can become irritable due to this abnormal movement repeated thousands of times a day.13 There is more wear and tear to the intervertebral discs as well.
In summary, the physical exam for this specific entity involves manual muscle testing for the PGM vs the TFL 11, palpation of the trochanteric bursae and gluteal muscles, and checking for a Trendelenburg sign.18 The Trendelenburg sign is the most sensitive physical exam finding for PGM tendonitis or tear.3 An AP film of the pelvis may be useful to rule out hip dysplasia, DJD, stress fracture, calcific bursitis, or osteonecrosis.
TREATMENT
We propose a treatment algorithm based on the above understanding of this pathology (Figure 2). Treatment for muscular pain is with the use of cold packs for 20 minutes several times a day. The cold pack should reach out to the trochanter. Other soft tissue modalities may also be beneficial, such as ultrasound or iontophoresis. Strengthening exercises are directed specifically to the PGM to decrease the influence of the TFL. The exercises need to be graduated according to the level of strength assessed in the physical exam. Strengthening is done in the shortened position to facilitate normal length. They are done at least twice daily for 4 weeks. It takes at least 4 weeks to actually add sarcomeres to atrophied muscle.15
Figure 2.
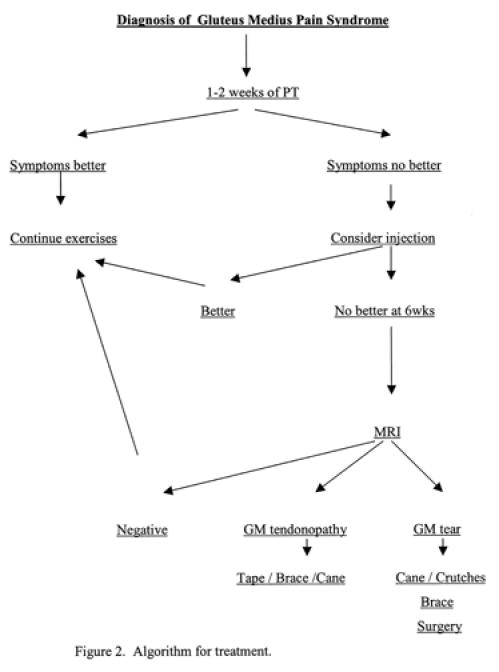
Algorithm for treatment.
Recommendations are given for altering activities of daily living to decrease stretching of the muscle. Specifically, sleeping with pillows between the knees when in side lying, not sitting with the legs crossed, standing with weight evenly distributed to both sides and the pelvis level. Recheck visits are at 1 or 2 weeks to assess improvement and to progress exercises as necessary. At 2 weeks, 20% of muscle strength change is attributed to contractile capacity and 80% to neural training.15 In the 2-4 week time frame, bursal injection or trigger point injections may be considered to facilitate the exercise program. If the muscle strain is severe or too painful, the use of a cane is suggested.19 Taping of the area to lessen forces during weight bearing could also be used.14 If, at 4-6 weeks, there is no improvement in strength assessment, an MRI would be suggested. This would be to determine tendonopathy vs. tendon rupture.12 A recent study reported the MRI findings of 24 people with this syndrome; nine demonstrated gluteus medius tendonitis, five had a tear, six had both evidence of tear and tendonitis, 3 were normal, and one showed avascular necrosis.3 If a tendon rupture is found, treatment could involve surgical repair4,8 and/or bracing in 0° of hip flexion and slight abduction with a hip-spica brace. Tendonitis would continue to be treated in a conservative manner.
SUMMARY
Evidence indicates that an important factor in conservative management involves providing accurate information to patients regarding an explanation of their problems and recommendations on methods of symptom control as well as limiting recurrence. Failure to receive an explanation of the problem results in patient dissatisfaction, increased use of diagnostic tests, and patients seeking treatment from other professionals.5
Often, a reasonable explanation of the probable causes of their pain and expected recovery will relieve anxiety and improve compliance with a home exercise program. The rationale for treatment of this syndrome involves mostly myofascial strain related to muscle imbalance that often mimics a lumbar radiculopathy. When the physical exam is negative for radiculopathy, further physical exam may reveal this syndrome. Recognition of this syndrome may well reduce the number of lumbar MRIs ordered and speed appropriate treatment because a more accurate diagnosis was achieved. We plan further studies involving gait patterns, pain during pregnancy, and acute care and chronic pain prevalence as well as specific interventions as described above.
References
- 1.Anrep GV, Von Saalfeld E. Blood flow through muscle in relation to contraction. J Physiol. 1935;85:375–399. doi: 10.1113/jphysiol.1935.sp003326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barcroft H, Millen JLE. Blood flow through muscle during sustained contraction. J Physiol. 1939;97:17–31. doi: 10.1113/jphysiol.1939.sp003789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bird PA, et al. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arth and Rheum. 2001 Sep;44(9):2138–2145. doi: 10.1002/1529-0131(200109)44:9<2138::AID-ART367>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 4.Bunker TD, et al. Rotator cuff tear of the hip. JBJS. 1997 Jul;79-B(4):618–620. doi: 10.1302/0301-620x.79b4.7033. [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Diehl AK. Patient satisfaction with medical care for low back pain. Spine. 1986;11:43–47. doi: 10.1097/00007632-198601000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Foti T, et al. A Biomechanical Analysis of Gait During Pregnancy. JBJS. 2000 May;A(5):625–632. [PubMed] [Google Scholar]
- 7.Kagan A. Rotator Cuff Tears of the Hip. Clin Ortho and Related Research. 1999;368:135–140. [PubMed] [Google Scholar]
- 8.Good MG. Muscular sciatica. Clin J. 1943;72:66–71. [Google Scholar]
- 9.Kellgren JH. Observations on referred pain from muscle. Clin Sci. 1938;3:175–190. [Google Scholar]
- 10.Kelly M. Treatment of fibrositis and allied disorders by local anesthesia. Med J Aust. 1941;1:294–298. [Google Scholar]
- 11.Kendall F P. Muscles: Testing and Function. Williams & Wilkins; 1983. [Google Scholar]
- 12.Kumagai M, et al. Functional Evaluation of Hip Abductor Muscle with use of Magnetic Resonance Imaging. J of Clin Research. 1997;15:888–893. doi: 10.1002/jor.1100150615. [DOI] [PubMed] [Google Scholar]
- 13.Maluf KS, Sahrmann SA, Van Dillen LR. Use of a classification system to guide nonsurgical management of a patient with chronic LBP. Physical Therapy. 2000;80:1097–1111. [PubMed] [Google Scholar]
- 14.Mueller MJ, Maluf KS. Tissue Adaptation to Physical Stress: A Proposed "Physical Stress Theory" to Guide Physical Therapist Practice, Education, and Research. Physcial Therapy. 2002 Apr;82(4):383–403. [PubMed] [Google Scholar]
- 15.Mortani H, Devries HA. Neural factors versus hypertrophy in the time course of muscle strength gain. Am J Phys Med. 1979;58:115. [PubMed] [Google Scholar]
- 16.Mosby's Medical, Nursing, and Allied Health Dictionary. Fourth Edition 1994.
- 17.Ostgaard HC, et al. Reduction of Back and Posterior Pelvis pain in Pregnancy. Spine. 1994;19(8):894–900. doi: 10.1097/00007632-199404150-00005. [DOI] [PubMed] [Google Scholar]
- 18.Peltier LF. Trendelenburg's Test: 1895. Clin Ortho and Related Research. 1998 Oct;355:3–7. [PubMed] [Google Scholar]
- 19.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. Mosby, Inc; 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slawski DP, Howard RF. Surgical Management of Refractory Trochanteric Bursitis. Amer J of Sports Med. 1997;25:1. doi: 10.1177/036354659702500117. [DOI] [PubMed] [Google Scholar]
- 21.Tortolini MD, et al. Greater trochanteric pain syndrome in patients referred to orthopedic spine specialists. The Spine Journal. 2002;2:251–254. doi: 10.1016/s1529-9430(02)00198-5. [DOI] [PubMed] [Google Scholar]
- 22.Travell JG, Simons DG. Myofascial Pain Dysfunction: The Trigger Point Manual. Williams & Wilkins; 1983. [Google Scholar]
- 23.Williams P, Goldspink G. Effect of immobilization on longitudinal growth of striated muscle fibers. J Anat. 1973;116:45. [PMC free article] [PubMed] [Google Scholar]


