SYNOPSIS
The National Drug Abuse Treatment Clinical Trials Network conducted this study to determine the availability of and factors associated with infection-related health services in substance abuse treatment settings. In a cross--sectional descriptive design, state policies, reimbursement for providers, state level of priority, and treatment program characteristics were studied via written surveys of administrators of substance abuse treatment programs and of state health and substance abuse departments.
Data from health departments and substance abuse agencies of 48 states and from 269 substance abuse treatment programs revealed that human immunodeficiency virus/acquired immunodeficiency syndrome-related services are more frequent than hepatitis C virus or sexually transmitted infection-related services, and that nonmedical services are more frequent than medical services. While the availability of infection-related health services is associated with medical staffing patterns, addiction pharmacotherapy services, and state priorities, reimbursement was the most significant determining factor.
These findings suggest that greater funding of these health services in substance abuse treatment settings, facilitated by supportive state policies, represents an effective response to the excess morbidity and mortality of these substance use-related infections.
In the aftermath of the 25th anniversary since the first case report of acquired immunodeficiency syndrome (AIDS), there is recognition of significant progress in prevention and treatment. Yet, some features of the AIDS landscape in the U.S. have not changed. Substance use remains among the three most frequent mechanisms of transmission of the human immunodeficiency virus (HIV), the cause of AIDS.1–4 Substance use also plays a significant role in the transmission of hepatitis C virus (HCV) infection5–9 and in the acquisition of sexually transmitted infections (STIs).10–15
Infected individuals who actively use or abuse substances have significant challenges accessing care and adhering to care, which contributes to disease progression.16–20 For these reasons, increased attention has been paid to the role of the substance abuse treatment system in responding to the excess morbidity and mortality associated with these infections. Other reasons include the fact that a substantial portion of substance abusers are enrolled in the substance abuse treatment system and many published reports document the benefits of substance abuse treatment in reducing transmission of substance use-related infections.21–24 These reports have focused primarily on changes in infection-related behaviors and/or infection rates among enrollees in substance abuse treatment programs.
Similar to other health-care providers, substance abuse treatment programs are diverse in setting, types of services (i.e., some are directly focused on unhealthy behaviors, while others focus on ameliorating the consequences of these behaviors), types and number of staff, and patient characteristics. And like other health-care settings, the provision of services is related to many external factors, such as financing and state guidance (i.e., policies, regulations, and priorities).
Although reports exist of infection-related health services in substance abuse treatment settings,25,26 very few explore features of substance abuse treatment programs or state policies, funding, or priorities that may affect the availability of health services responsible for infection-related benefits. This information represents an important public health need, given the pivotal role of substance abusers in the transmission of these infections in society and the fact that substance abuse treatment programs represent an important point of access to substance abusers.
The primary objective of Characteristics of Screening, Evaluation, and Treatment of HIV/AIDS, Hepatitis C Viral Infection and Sexually Transmitted Infections in Substance Abuse Treatment Programs—referred to as the Infections and Substance Abuse Study—was to describe the availability of health services for HIV/AIDS, HCV infection, and STIs among substance abuse treatment programs participating in the National Drug Abuse Treatment Clinical Trials Network (CTN). While we previously published an overview of the study design, methods, and processes,27 in this article, we examine the availability of these health services and their association with factors integral to and external to the substance abuse treatment programs participating in the CTN.
METHODS
Study population
The CTN was established to improve the quality of drug abuse treatment throughout the country using science as the vehicle. A full description of the CTN is available at http://www.nida.nih.gov/CTN/about.html and in previously published reports.28,29
This article is limited to information derived from state substance abuse and health department administrators and substance abuse treatment program administrators. We received responses to a survey from 48 states (96% response rate). From 21 states, we received two surveys (one from the health department and one from the substance abuse department). Of the more than 20,000 questions among the submitted state surveys, a discrepancy within a state's response occurred in less than 10% of the responses, and we selected the response most consistent with the jurisdiction of the relevant agency.
A survey was provided to the administrator of each of the 319 treatment programs in the CTN, distributed across 26 states. Eighty-four percent (269 of 319) of substance abuse program administrators returned a survey. No portion of the country or the CTN was overrepresented among the 50 nonresponding program administrators.
Approval was obtained from Institutional Review Boards with jurisdiction over the participating treatment programs. Participants were provided information about the objectives of the study prior to the one-time administration of the survey instruments.
Study design
The Infections and Substance Abuse Study was a cross-sectional, descriptive, and observational examination of the range of available services and related state policies and funding associated with targeted infections in substance abuse treatment settings within the CTN.
This article focuses on two categories of infection-related health services: medical services (medical history and physical examination, biological testing, medical treatment, and medical monitoring) and nonmedical health services (patient education, patient risk assessment, and patient counseling). Definitions for each health service accompanied the paper surveys, as reported previously.27 The state administrator survey sought information about state policies, guidelines, or regulations (yes or no), reimbursement for providers (yes or no), and level of priority (low, medium, or high) for each of the infection-related health services.
For this article, we focused on whether or not state administrators reported that there was a high priority (yes or no) on each of the infection-related health services. The program administrator survey contained questions focused on the treatment program structure, service setting, patient characteristics, staff characteristics, sources of reimbursement, infection-related health practices, treatment program guidelines, barriers to the provision of infection-related services, and their opinions of the importance of services for these infections in treatment programs.
Statistical analysis
Each section of the survey contained mostly yes-no or multiple-choice questions. Consequently, the number and proportion of respondents providing a given answer were used to summarize responses. For questions requiring numerical answers, the mean, median, and standard deviation were used to evaluate the answers. For some questions, responses were collapsed into a broader set of categories (e.g., federal, state, and local funding collapsed to government funding).
Cross-tabulations of the seven health services for each of the three infections (dependent variables) and the treatment program or state attributes (independent variables) were calculated to investigate relationships. The significance of bivariate relationships was assessed by Chi-Square tests. In cases where the Chi-Square test was inappropriate (cases with expected cell counts less than five), the Fisher's exact test was used. While sample size was not based on statistical test considerations, as this was an exploratory study, power calculations were performed using PASS 2002 software30 where indicated. The sample sizes for responses to each survey question are noted below each table and figure.
Figure.
Substance abuse treatment programs providing infection-related health services
NOTE: The sample size varies from 247 to 260. A sample size of 247 achieves 80% power to detect an effect size of 0.18 using a one degree of freedom Chi-Square test with a significance level of 0.05. An effect of 0.18 is the equivalent of at least a 0.10 difference (potentially larger depending on the values) in proportions between groups.
a p<0.01 as compared to HIV/AIDS
b p<0.05 as compared to HIV/AIDS
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
HCV = hepatitis C virus
STI = sexually transmitted infection
As this study's design was observational and exploratory, without a control group, we were not able to ascribe any predictive value to any of the associations. Thus, the study was designed to generate hypotheses to be pursued in future investigations designed to answer critical hypotheses.
RESULTS
Treatment program characteristics
Nearly 80.0% of the treatment programs were private not-for-profit agencies, 5.6% were private for-profit agencies, 13.4% were public agencies, and 2.2% were reported as other. While most treatment programs offered two or more addiction services, patient outreach and support services were the most frequently reported addiction services (offered by 87.6%).
Program size and medical and nonmedical staffing patterns varied considerably (Table 1). More than two-thirds of the treatment programs had eight or more nonmedical staff such as counselors, educators, psychologists, and social workers. Slightly more than one-fifth of the programs had no medical staff (physicians, physician's assistants, nurse practitioners, registered or licensed practical nurses, pharmacists, or medical technicians).
Table 1.
Program and patient characteristics of substance abuse treatment programs (n=269)a
Some categories do not total 100% due to rounding.
Responses for this characteristic are not mutually exclusive.
HIV = human immunodeficiency virus
HCV = hepatitis C virus
STI = sexually transmitted infection
Availability of infection-related health services
Infection-related health services were delivered on-site or via referral agreements with other agencies (Figure). Generally, HIV/AIDS-related health services were more available than services for HCV infection or STIs. The three nonmedical health services (patient education, risk assessment, and counseling) were more available than the four medical services (patient history and physical examination, biological testing, treatment, and clinical monitoring). The provision of at least one of the three types of HIV/AIDS-related, HCV-related, and STI-related nonmedical health services was reported, by 94%, 83%, and 85% of program administrators, respectively. In contrast, the availability of at least one of the medical services related to HIV/AIDS, HCV infection, and STIs was reported, respectively, by only 70%, 59%, and 60% of program administrators. More than one-quarter of the programs provided all seven HIV-related services. None of the HIV-related, HCV-related, or STI-related health services were available in 6%, 17%, and 15% of the treatment programs, respectively. More than half of the programs provided ongoing training for staff in HIV/AIDS and HCV infection, while slightly less than half provided ongoing training in STIs. More than 40% of the administrators reported that their agencies had guidelines pertaining to HIV/AIDS-related medical and nonmedical services. Program guidelines were reported at a lower rate for the other infection groups.
We then explored the relationships between program characteristics (Table 1) and their provision of the infection-related services. Treatment setting was significantly associated with the delivery of HIV- or HCV-related medical history and physical examination services. HIV-related medical history and physical examination services were available in 79% of programs in a hospital, university, or health center setting, 54% of programs in a social service care setting, and 52% of freestanding substance abuse treatment facilities. HCV-related medical history and physical examination services were available in 68% of programs in a hospital, university, or health center setting, 42% of programs in a social service care setting, and 47% of freestanding substance abuse treatment programs.
When we evaluated the relationship between the provision of each infection-related health service with the provision of the four categories of addiction services (Table 1), each medical and nonmedical service, irrespective of infection, was available more often in treatment programs providing outpatient pharmacotherapy addiction services than in treatment programs that did not provide this type of addiction service (p<0.05). With the exception of STI-related risk assessment services, treatment programs with more medical staff were significantly more likely to provide each of the medical and nonmedical services for each infection group (p<0.01).
At least two-thirds of program administrators reported reimbursement for each infection-related service. As compared to programs reporting the absence of reimbursement for each infection-related health service, programs with reimbursement were more likely to provide the infection-related health service, irrespective of service or infection (p<0.001). When Medicaid was the largest source of funding for substance abuse services, each of the medical (except HIV-related biological testing) and nonmedical services, irrespective of the infection, was significantly more likely to be provided.
While there was no relationship between patient population size and the availability of any of the infection-related health services, programs with greater than 10% patient HIV infection rates were more likely to provide all the HIV-related health services (except medical treatment monitoring) than programs reporting lower HIV infection rates. Similarly, programs with greater than 10% patient HCV infection rates were more likely to provide all the HCV-related health services (except medical treatment monitoring) than programs reporting lower HCV infection rates.
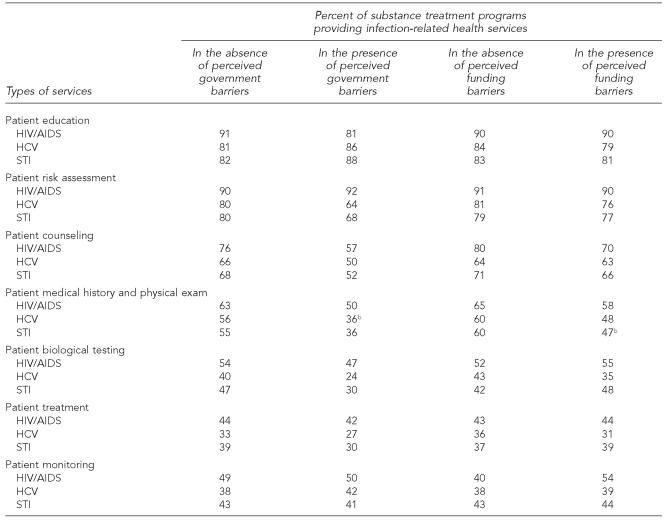
We then explored the existence of any relationships between governmental barriers or funding barriers as reported by program administrators and the availability of infection-related health services in treatment programs (Table 2). While a higher percentage of programs tended to provide infection-related health services when the program administrators reported no government or funding barriers vs. when the program administrators reported the existence of government or funding barriers, the differences were not significant except for two services. HCV-related medical history and physical examination services were available in 56% of the programs reporting no barriers vs. 36% of the programs reporting the existence of such barriers. STI-related medical history and physical examination services were available in 60% of the programs reporting no funding barriers vs. 47% of the programs reporting the existence of such barriers.
Table 2.
Availability of infection-related health services substance abuse treatment programs by government and funding barriersa
As reported by treatment program administrators. The sample size for responses to each survey question varied from 143 to 254. A sample size of 143 achieves 80% power to detect an effect size of 0.23 using a one degree of freedom Chi-Square test with a significance level of 0.05. An effect of 0.23 is the equivalent of at least a 0.12 difference (potentially larger depending on the values) in proportions between groups.
p<0.05 comparing treatment programs offering the service with programs that do not offer the services
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
HCV = hepatitis C virus
STI = sexually transmitted infection
Relationships between infection-related health services in treatment programs and state guidance and funding
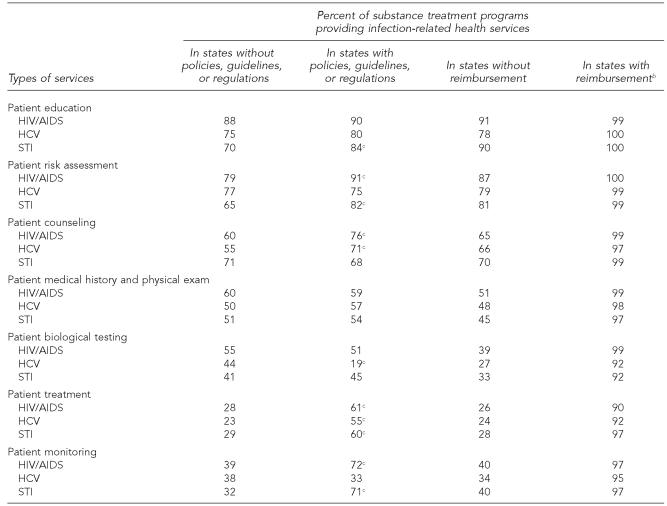
To explore the relationships between the availability of infection-related health services in treatment programs as reported by program administrators and state guidance (policies, guidelines, or regulations) and funding as reported by state administrators, we limited the analysis of the state data to the 26 states represented by the treatment programs in the CTN. We assessed the percentage of treatment programs providing each infection-related health service for the three infections in the presence or absence of two conditions: state guidance and reimbursement (Table 3).
Table 3.
Availability of infection-related health services substance abuse treatment programs by state policies, guidelines, or regulations or by state reimbursementa
As reported by state administrators. The sample size for responses to each survey question varied from 143 to 254. A sample size of 143 achieves 80% power to detect an effect size of 0.23 using a one degree of freedom Chi-Square test with a significance level of 0.05. An effect of 0.23 is the equivalent of at least a 0.12 difference (potentially larger depending on the values) in proportions between groups.
p<0.01 comparing treatment programs offering the service with programs that do not offer the service
p<0.05 comparing treatment programs offering the service with programs that do not offer the service
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
HCV = hepatitis C virus
STI = sexually transmitted infection
In the presence of state guidance, a larger percentage of programs provided HIV-related risk assessment (p=0.02), patient counseling (p=0.02), medical treatment (p<0.01), and medical monitoring (p<0.01) services than programs in states without such guidance. State guidance was also positively associated with HCV-related patient counseling and patient treatment, as well as STI-related patient education, patient risk assessment, patient treatment, and patient monitoring. In contrast, the presence of reimbursement, as reported by state administrators, was significantly associated with the availability of each of the 21 infection-related health services, as reported by program administrators.
State substance abuse and health departments
Seven states had HIV/AIDS-related policies, guidelines, or regulations for all seven health-care services. Four states reported no policies, guidelines, or regulations pertaining to any of the seven HIV-related health-care services. Funding for all seven HIV/AIDS-related services was available in 41 states. All seven HIV/AIDS-related services were a high priority for 16 states. When asked about whether or not certain components are mandated as part of HIV/AIDS-related services in substance abuse treatment program settings, 58% of the states had such mandates for HIV risk assessment, 79% for HIV/AIDS-related education, 27% for HCV risk assessment, and 33% for STI risk assessment.
Four states reported HCV-related policies, guidelines, or regulations for all four medical services, while 10 states reported such guidance for all three nonmedical services. Thirteen states had no policies, guidelines, or regulations pertaining to any of the HCV-related health services. All four HCV-related medical services and all three nonmedical services were high priorities in six and 13 states, respectively.
Policies, guidelines, or regulations for at least one of the STI-related medical services and at least one of the STI-related nonmedical services existed in 73% and 69% of the states, respectively. Funding was available for at least one of the STI-related medical services in 94% of the states and for at least one of the nonmedical services in 87% of the states. Funding for all the STI-related health services existed in 47% of the states, while no funding existed for any of the health services in 6% of the states. At least one of the STI-related medical services was a high priority in 79% of the states, while at least one of the nonmedical services was a high priority in 70% of the states.
We then assessed relationships between the 21 infection-related health services and (1) state policies, guidelines, or regulations, (2) treatment program funding, and (3) high level of priority as reported by state administrators (Table 4). There were no significant differences between the proportion of states reporting policies, guidelines, or regulations for HIV-related medical services and the proportion of states reporting such guidance for HCV- or STI-related medical services. However, 60% to 83% of the states reported such guidance for HIV-related nonmedical services vs. 40% to 53% of the states reporting guidance for the HCV-related nonmedical services and 35% to 56% for STI-related nonmedical services.
Table 4.
State policies, guidelines or regulations, funding, and priority level by infection-related health services in substance abuse treatment programs
The sample size varies from 44 to 48. A sample size of 44 produces 80% power to detect an effect size of 0.42 using a one degree of freedom Chi-Square test with a significance level of 0.05. An effect of 0.42 is the equivalent of at least a 0.22 difference (potentially larger depending on the values) in proportions between groups.
p<0.01 as compared to HIV/AIDS
p<0.05 as compared to HIV/AIDS
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
HCV = hepatitis C virus
STI = sexually transmitted infection
A significantly larger proportion of states reported funding for each of the seven HIV-related services as compared to HCV- or STI-related medical or nonmedical services. Also, a larger proportion of the states reported a high priority for HIV-related nonmedical services than for HCV- or STI-related nonmedical services. A high priority for the HIV-related medical services was reported by a larger proportion of states than states reporting a high priority for HCV-related medical services.
DISCUSSION
Substance abuse treatment programs represent a unique setting in the American health-care system, providing an important point of access to health care for the 9.4% of American adults diagnosed with a substance use disorder.29 Substance abuse treatment has been studied extensively, not only with respect to its impact on reducing substance use,31–33 but also its impact on reducing transmission of HIV, HCV infection, and STIs.21–24,33 There have been two published multisite reports of infection-related health services available in substance abuse treatment.25,26 These prior reports were limited to a focus on HIV/AIDS or HCV infection and did not examine the impact of state policy, funding, and priority setting on the ability of substance abuse treatment programs to deliver infection-related health services. This article addresses these unanswered questions for a wide array of health services and includes three infection groups with excess morbidity and mortality among substance users in the U.S. today.
Among the main findings from the current study is the fact that more states place a high priority on, and report policies, guidelines, regulations, and funding for HIV/AIDS-related health services as compared to HCV- or STI-related services and for the nonmedical infection-related services as compared to the medical services. Similarly, in substance abuse treatment programs, HIV/AIDS-related health services of all types were more frequently available than health services for either HCV infection or STIs. Irrespective of the infection, nonmedical services were more available than medical services. Even though funding exists for these health-care services, treatment programs reported funding and government regulatory barriers to their delivery more frequently for medical services than for nonmedical services. These observations suggest a relationship between the availability of infection-related services in substance abuse treatment programs and funding, state policies, and state priority settings.
Other major findings of this study were the varied substance abuse treatment settings delivering infection-related services and the program and patient characteristics most commonly observed among these health-care institutions. Substance abuse treatment programs with the following attributes—providing outpatient pharmacotherapy (such as methadone); with robust medical staffing; reporting Medicaid as their largest revenue source; reporting the availability of reimbursement of any type for the infection-related services; or reporting higher HIV, HCV, or STI infection rates or risk behaviors—were more likely to provide infection-related medical or nonmedical services.
Some of these relationships were intuitive and had high face validity; reimbursement and medical staff were crucial ingredients in the delivery of infection-related health services. Consistent with prior reports, infection-related services were more prevalent in treatment programs providing addiction-related pharmacotherapy services (which tend to require more robust medical staffing) than treatment programs that did not provide pharmacotherapy services. The greater availability of infection-related health services in substance abuse treatment programs with pharmacotherapy services may explain why opiate agonist therapies are associated with reduced infection-related drug use behaviors, reduced HIV transmission, and a lower probability of HIV disease progression.34–37
The finding that Medicaid is the largest revenue source for treatment programs providing these services may be explained by the fact that patients receiving care from these agencies are not likely to be Medicare-eligible, and private insurance is not a significant contributor to the revenues of treatment programs. Also, some states have enhanced reimbursement schedules for the infection-related medical services via Medicaid.
Limitations
Although this report is based on information from a nonrandom and not necessarily representative sample of substance abuse treatment programs, findings are consistent in areas in which the current study and two previous multisite treatment program studies sought similar information.25,26 Randomized controlled clinical trial design may not always capture many contextual or clinical factors critical to informing clinical practice or public health policy, especially for behavioral health issues.38
Another limitation is that this study is based on self-reports of individuals and that this information may be biased or inaccurate, especially since the study contained no data to validate information from the surveys. To limit any motivation by respondents to misrepresent information, respondents were informed that their personal, treatment program, and state identities would be kept confidential, and they completed their surveys at their own pace.
The current study captured information on many more infection-related services as well as information about state policies and priorities related to these services. It did not target information on costs or effectiveness of, or patient or staff satisfaction with, infection-related health services in substance abuse treatment settings, which should be pursued in the future.
Reimbursement for the infection-related services was the single factor most significantly associated with service availability. Nonetheless, it is troubling to note the absence of infection-related health services even when funding for these services is available or when state policies and priorities exist in support of these health services. These health services contribute to the infection-related benefits of substance abuse treatment. As states make crucial decisions about how to prevent and respond to the excess morbidity and mortality of these infections, it is important to address both the availability of reimbursement and to develop mechanisms to assure that providers are trained and that reimbursable services are offered in this unique health-care setting.
While there is continued debate about the appropriate role of substance abuse treatment in the American health-care system—including how it should be financed—and many questions remain about the relative benefits of various features of substance abuse treatment, there can be little doubt of the benefit of this health-care sector in reducing transmission of these preventable infections. The benefit is not only for people who abuse drugs, but also for populations that acquire these infections from those who do.
Acknowledgments
The authors are indebted to the efforts of administrators, clinicians, and investigators of the 17 universities and medical centers along with the participating community-based substance abuse treatment programs of the National Drug Abuse Treatment Clinical Trials Network. The authors are also grateful for the assistance of the National Association of State Alcohol and Drug Abuse Directors, the National Alliance of State and Territorial AIDS Directors, and the Association of State and Territorial Health Officers.
Footnotes
This article was supported by the National Institute on Drug Abuse/National Institutes of Health via the National Drug Abuse Treatment Clinical Trials Network (2 U10 DA13046).
REFERENCES
- 1.Epidemiology of HIV/AIDS—United States, 1981–2005. MMWR Morb Mortal Wkly Rep. 2006;55(21):589–92. [PubMed] [Google Scholar]
- 2.Francis H. Substance abuse and HIV infection. Top HIV Med. 2003;11:20–4. [PubMed] [Google Scholar]
- 3.National Institute on Drug Abuse (US) HIV/AIDS. National Institute on Drug Abuse Research Report Series. 2006. National Institutes of Health Publication Number 06-5760.
- 4.National Institute on Drug Abuse (US) Principles of HIV prevention in drug-using populations: a research-based guide. 2002. National Institutes of Health Publication Number 02-4733.
- 5.Recommendations for prevention and control of hepatitis C virus (HCV) infection and HCV-related chronic disease. MMWR Recomm Rep. 1998;47(RR-19):1–39. [PubMed] [Google Scholar]
- 6.Broers B, Junet C, Bourquin M, Deglon JJ, Perrin L, Hirschel B. Prevalence and incidence rate of HIV, hepatitis B and C among drug users on methadone maintenance treatment in Geneva between 1988 and 1995. AIDS. 1998;12:2059–66. doi: 10.1097/00002030-199815000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Lorvick J, Kral AH, Seal K, Gee L, Edlin BR. Prevalence and duration of hepatitis C among injection drug users in San Francisco, Calif. Am J Public Health. 2001;91:46–7. doi: 10.2105/ajph.91.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas DL, Vlahov D, Solomon L, Cohn S, Taylor E, Garfein R, et al. Correlates of hepatitis C virus infections among injection drug users. Medicine (Baltimore) 1995;74:212–20. doi: 10.1097/00005792-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Garfein RS, Doherty MC, Monterroso ER, Thomas DL, Nelson KE, Vlahov D. Prevalence and incidence of hepatitis C virus infection among young adult injection drug users. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(Suppl 1):S11–9. doi: 10.1097/00042560-199802001-00004. [DOI] [PubMed] [Google Scholar]
- 10.Belongia EA, Danilia RN, Angamuthu V, Hickman CD, DeBoer JM, MacDonald KL, et al. A population-based study of sexually transmitted disease incidence and risk factors in human immunodeficiency virus-infected people. Sex Transm Dis. 1997;24:251–6. doi: 10.1097/00007435-199705000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Fortenberry JD, Brizendine EJ, Katz BP, Wools KK, Blythe MJ, Orr DP. Subsequent sexually transmitted infections among adolescent women with genital infection due to Chlamydia trachomatis, Neisseria gonorrhoeae, or Trichomonas vaginalis. Sex Transm Dis. 1999;26:26–32. doi: 10.1097/00007435-199901000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Poulin C, Alary M, Bernier F, Ringuet J, Joly JR. Prevalence of Chlamydia trachomatis, Neisseria gonorrhoeae, and HIV infection among drug users attending an STD/HIV prevention and needle-exchange program in Quebec City, Canada. Sex Transm Dis. 1999;26:410–20. doi: 10.1097/00007435-199908000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Plitt SS, Garfein RS, Gaydos CA, Strathdee SA, Sherman SG, Taha TE. Prevalence and correlates of chlamydia trachomatis, neisseria gonorrhoeae, trichomonas vaginalis infections, and bacterial vaginosis among a cohort of young injection drug users in Baltimore, Maryland. Sex Transm Dis. 2005;32:446–53. doi: 10.1097/01.olq.0000154567.21291.59. [DOI] [PubMed] [Google Scholar]
- 14.Bachmann LH, Lewis I, Allen R, Schwebke JR, Leviton LC, Siegal HA, et al. Risk and prevalence of treatable sexually transmitted diseases at a Birmingham substance abuse treatment facility. Am J Public Health. 2000;90:1615–8. doi: 10.2105/ajph.90.10.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep. 2002;51(RR-6):1–78. [PubMed] [Google Scholar]
- 16.Tobias C, Brown K, Rajabiun S, Drainoni ML, Young SR. A kaleidoscope of care for HIV-infected substance users. J HIV/AIDS & Social Services. 2005;4:27–43. [Google Scholar]
- 17.Mehta SH, Thomas DL, Sulkowski MS, Safaein M, Vlahov D, Strathdee SA. A framework for understanding factors that affect access and utilization of treatment for hepatitis C virus infection among HCV-mono-infected and HIV/HCV co-infected injection drug users. AIDS. 2005;19(Suppl 3):S179–89. doi: 10.1097/01.aids.0000192088.72055.90. [DOI] [PubMed] [Google Scholar]
- 18.Poundstone KE, Chaisson RE, Moore RD. Differences in HIV disease progression by injection drug use and by sex in the era of highly active antiretroviral therapy. AIDS. 2001;15:1115–23. doi: 10.1097/00002030-200106150-00006. [DOI] [PubMed] [Google Scholar]
- 19.Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, et al. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. J Gen Intern Med. 2002;17:377–81. doi: 10.1046/j.1525-1497.2002.10644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore RD, Keruly JC, Chaisson RE. Differences in HIV disease progression by injecting drug use in HIV-infected persons in care. J Acquir Immune Defic Syndr. 2004;35:46–51. doi: 10.1097/00126334-200401010-00006. [DOI] [PubMed] [Google Scholar]
- 21.Hubbard RL, Marsden ME, Cavanaugh E, Rachal JV, Ginzburg HM. Role of drug-abuse treatment in limiting the spread of AIDS. Rev Infect Dis. 1988;10:377–84. doi: 10.1093/clinids/10.2.377. [DOI] [PubMed] [Google Scholar]
- 22.Metzger DS, Navaline H, Woody GE. Drug abuse treatment as AIDS prevention. Public Health Rep. 1998;113(Suppl 1):S97–106. [PMC free article] [PubMed] [Google Scholar]
- 23.Sorensen JL, Copeland AL. Drug abuse treatment as an HIV prevention strategy: a review. Drug Alcohol Depend. 2000;59:17–31. doi: 10.1016/s0376-8716(99)00104-0. [DOI] [PubMed] [Google Scholar]
- 24.Farrell M, Gowing L, Marsden J, Ling W, Ali R. Effectiveness of drug dependence treatment in HIV prevention. Intern J Drug Policy. 2005;16:67–75. [Google Scholar]
- 25.Strauss SM, Falkin GP, Vassilev Z, Des Jarlais DC, Astone J. A nationwide survey of hepatitis C services provided by drug treatment programs. J Subst Abuse Treat. 2002;22:55–62. doi: 10.1016/s0740-5472(01)00213-6. [DOI] [PubMed] [Google Scholar]
- 26.Substance Abuse and Mental Health Services Administration, Office of Applied Studies (US) Data on substance abuse treatment facilities. Rockville (MD): 2005. National Survey of Substance Abuse Treatment Services (N-SSATS): 2004. DASIS Series: S-28, DHHS Publication No. (SMA) 05-4112. [Google Scholar]
- 27.Brown LS, Jr., Kritz SA, Goldsmith J, Bini EJ, Rotrosen J, Baker S, et al. Characteristics of substance abuse treatment programs providing services for HIV/AIDS, hepatitis C virus infection, and sexually transmitted infections: The National Drug Abuse Treatment Clinical Trials Network. J Subst Abuse Treat. 2006;30:315–21. doi: 10.1016/j.jsat.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rotrosen J, Leshner A, Tai B, Greenlick M, Pencer E, Trachtenberg R, et al. The national drug abuse treatment clinical trials network—challenges and opportunities. National Institute on Drug Abuse Research Monograph Series. 2002;182:12–7. [Google Scholar]
- 29.Substance Abuse and Mental Health Services Administration (US) Rockville (MD): SAMHSA; 2005. Results from the 2004 National Survey on Drug Use and Health: national findings. (Office of Applied Studies, NSDUH Series H-28, DHHS Publication No. SMA 05-4062) [Google Scholar]
- 30.NCSS. PASS: 2002 for Windows. Kaysville (UT): NCSS; 2002. [Google Scholar]
- 31.Simpson DD, Sells SB. Effectiveness of treatment for drug abuse: an overview of the DARP research program. Adv Alcohol Subst Abuse. 1982;2:7–29. [Google Scholar]
- 32.Hubbard RL, Rachal JV, Craddock SG, Cavanaugh ER. Treatment outcome prospective study (TOPS): client characteristics and behaviors before, during, and after treatment. In: Tims FM, Ludford JP, editors. Drug abuse treatment evaluation: strategies, progress and prospects. Research Monograph. Vol. 51. Rockville (MD): Department of Health and Human Services (US), National Institute on Drug Abuse; 1984. pp. 42–68. [PubMed] [Google Scholar]
- 33.Hubbard RL, Craddock SG, Flynn PM, Anderson J, Etheridge RM. Overview of 1-year follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychol Addict Behav. 1997;11:261–78. [Google Scholar]
- 34.Cooper JR. Methadone treatment and acquired immunodeficiency syndrome. JAMA. 1989;262:1664–8. [PubMed] [Google Scholar]
- 35.Hartel DM, Schoenbaum EE. Methadone treatment protects against HIV infection: two decades of experience in the Bronx, New York City. Public Health Rep. 1998;113(Suppl 1):S107–15. [PMC free article] [PubMed] [Google Scholar]
- 36.Brown LS, Jr., Chu A, Nemoto T, Ajuluchukwu D, Primm BJ. Human immunodeficiency virus infection in a cohort of intravenous drug users in New York City: demographic, behavioral, and clinical features. NY State J Med. 1989;89:506–10. [PubMed] [Google Scholar]
- 37.O'Connor PG, Selwyn PA, Schottenfeld RS. Medical care for injection-drug users with human immunodeficiency virus infection. N Engl J Med. 1994;331:450–9. doi: 10.1056/NEJM199408183310707. [DOI] [PubMed] [Google Scholar]
- 38.Tucker JA, Roth DL. Extending the evidence hierarchy to enhance evidence-based practice for substance use disorders. Addiction. 2006;101:918–32. doi: 10.1111/j.1360-0443.2006.01396.x. [DOI] [PubMed] [Google Scholar]