Abstract
Medial collateral ligament (MCL) injury is one of the most common knee injuries, especially in young athletic patients. Most MCL injuries can be managed conservatively with good results. However, a complete understanding of knee anatomy and the involved structures is necessary to make intelligent treatment decisions. We will review the anatomy and biomechanics of the MCL, classification systems for MCL injuries, and operative and nonoperative treatment for acute and chronic MCL injuries.
INTRODUCTION
The medial collateral ligament (MCL) is one of the most commonly injured ligamentous structures of the knee joint.1–3 The popularity of sports, particularly those involving valgus knee loading such as ice hockey, skiing, and football, has contributed to the frequent occurrence of MCL injuries.3–5 The role of prophylactic bracing has been biomechanically and clinically studied, and in the majority of studies was of limited benefit.3,5,7 Other preventive measures such as skill training, rule modifications, proper equipment, and promotion of fair play have been proposed, but the efficacy of these changes is not known.2,5,8
The majority of patients who sustain MCL injuries of varying severity can achieve pre-injury activity level with nonoperative treatment alone.9–18 The most severe injuries, especially those with multiple ligament involvement, may require operative repair or augmentation on an acute basis. In addition, surgical reconstruction is indicated for isolated symptomatic chronic MCL laxity. We will discuss the functional anatomy, clinical evaluation, and treatment of MCL injuries. We will review the original work by James, which still applies today in understanding the functional anatomy of medial knee structures, and our approach to the treatment of acute and chronic medial-sided knee injuries. The authors' preferred surgical techniques for ligamentous repair, augmentation, and reconstruction, as well as postoperative care and complications, will be discussed.
ANATOMY
The anatomy of the medial side of the knee is complex, being composed of three tissue layers and multiple components with interconnections to the joint capsule, the muscle-tendon units, and the medial meniscus. The ligamentous sleeve spans the entire medial side of the knee from the medial aspect of the extensor mechanism to the posterior aspect of the knee adjacent to the posterior cruciate ligament (Figure 1A). The majority of the basic anatomy has been described by James,19–21 Warren,22,23 Hughston,24 and others. In particular, Figures 1B, 2B, and 3B are from dissections James performed at the University of Iowa during the 1970s.
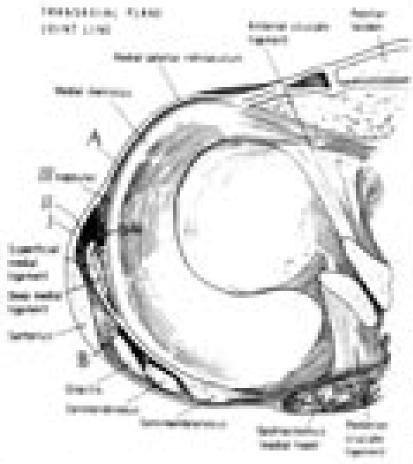
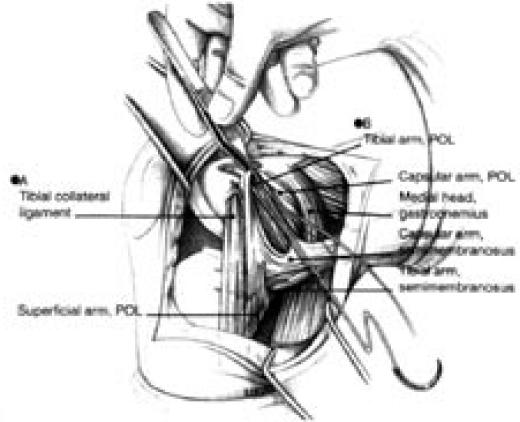
Figure 1A.
Layer I is the deep crural fascia which is in continuity with the medial patellar retinaculum and the sartorial fascia. The fascia spans from the patellar tendon anteriorly to the midline of the popliteal fossa posteriorly. (From Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee, an anatomic analysis. J Bone Joint Surg Am 1979;61:58, permission granted.)
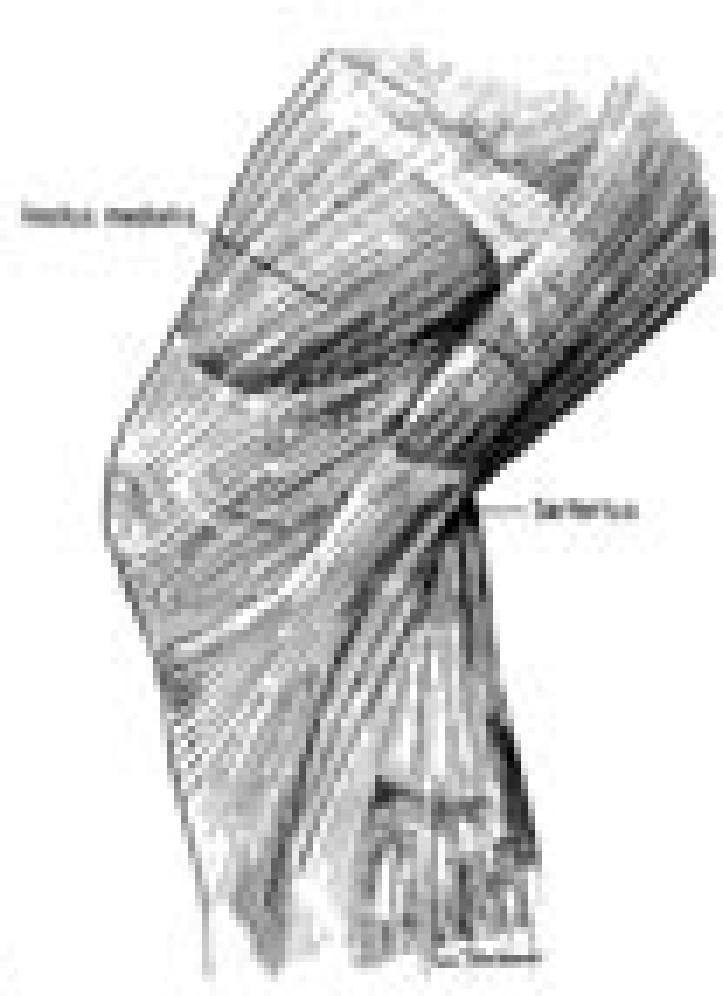
Figure 1B.
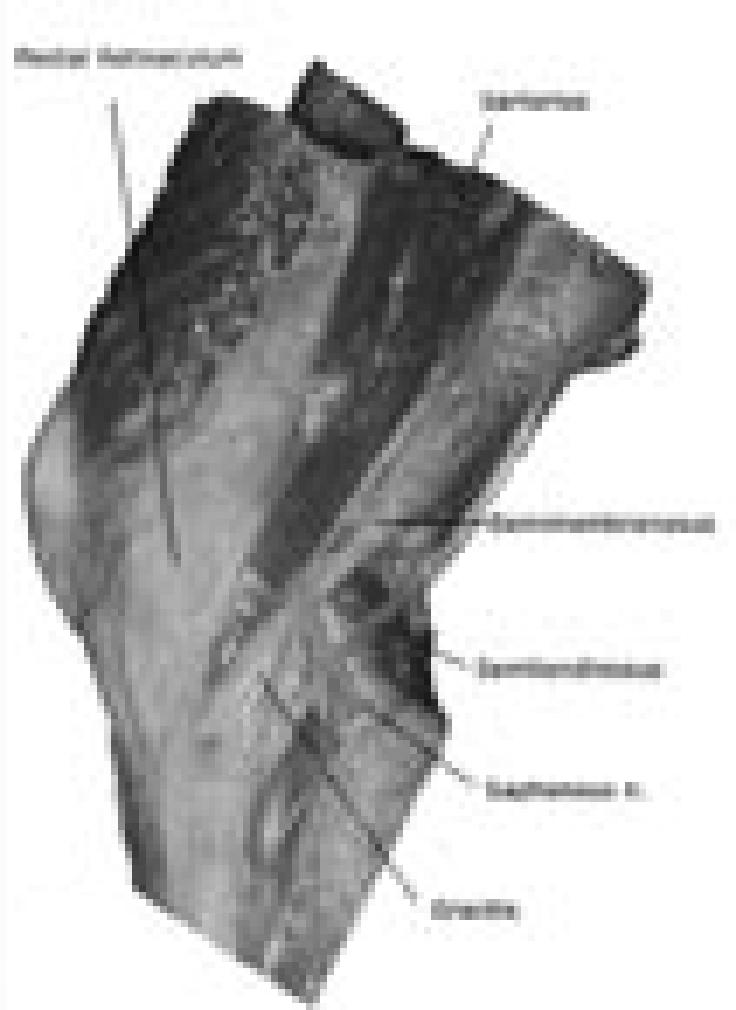
A cadaver dissection reveals the relationship of the medial retinaculum, the pes anserinus tendons, the semimembranosus tendon, and the saphenous nerve.
Figure 2A.
Cross-section anatomy at the level of the joint line is demonstrated. A split can be seen just in front of the superficial MCL. Layer I and II blend together along a vertical line 1-2 cm anterior to the anterior border of the superficial MCL. At the posteromedial corner of the knee, layers II and III merge forming the posterior oblique ligament, which is augmented by the insertion of the semimembranosus insertions. (From Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee, an anatomic analysis. J Bone Joint Surg Am 1979;61:58, permission granted.)
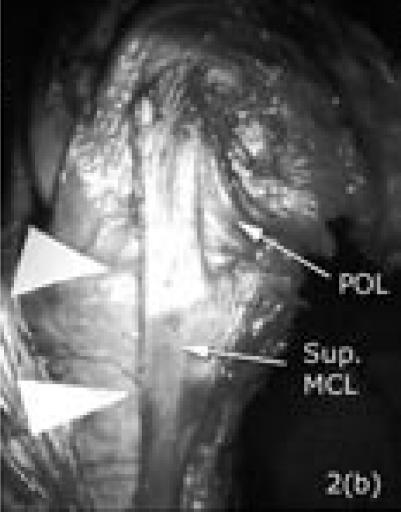
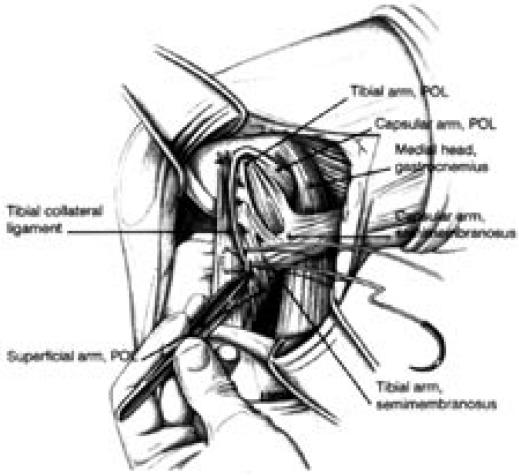
Figure 2B.
A cadaver dissection shows the slit in front of the superficial MCL (two white triangles). The ligament is long and inserts about 5-7 cm below the joint line. The posterior oblique ligament (POL) is clearly shown in continuity with the parallel fibers of the superficial MCL posteriorly.
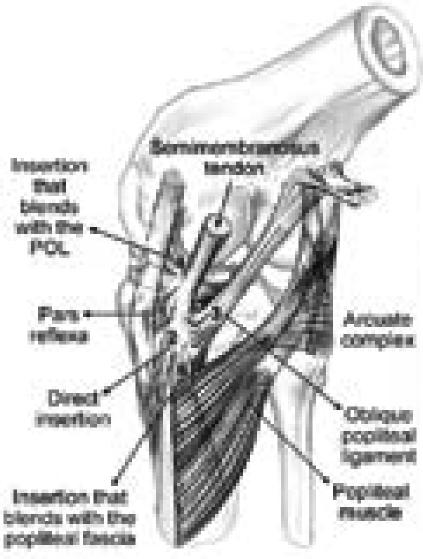
Figure 3A.
The posteromedial structures of the knee are demonstrated. Note the relationship between the posterior oblique ligament, the meniscus, and the insertions of the semimembranosus tendon. The five insertions of the semimembranosus include the: (1) pars reflexa; (2) direct posteromedial tibial insertion; (3) oblique popliteal ligament insertion; (4) expansion to posterior oblique ligament; and (5) popliteus aponeurosis expansion. (From Sims, WF and Jacobson, KE. The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med 2004. 32(2):337-45, permission granted.)
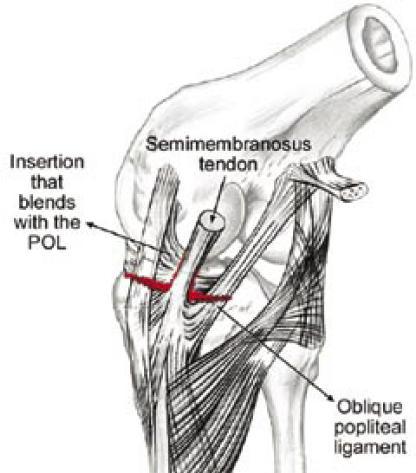
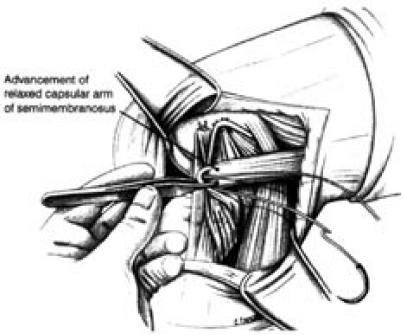
Figure 3B.
Insertions of the semimembranosus (A), with the numbers (1, 4, 3) corresponding to the Figure 3a legend, are shown in a cadaver. The medial gastrocnemius muscle is cut and elevated proximally (B).
The structures that are considered static stabilizers of the medial knee are the superficial MCL, the deep MCL, and the posterior oblique ligament. The superficial MCL is the primary static medial stabilizer of the knee situated in the second layer, according to Warren and Marshall's three-layer concept.22 It is positioned between the superficial sartorial fascia and the deep MCL. Its parallel fibers originate from the center of knee motion on the medial femoral epicondyle and insert on the medial aspect of the proximal tibia five to seven centimeters (cm) below the joint line, with an average length of 11 cm and an average width of 1.5 cm (Figure 1B). The ligament is deep to the crural and sartorial fascia and superficial to the deep MCL. Between the anterior border of the superficial MCL and the confluence of the first and second layers lies a vertical split of varying size and shape (Figures 2A, 2B).
The posterior aspect of the ligament has a continuum of oblique fibers referred to as the "posterior oblique ligament" that arises as a conjoined structure from the second and the third layers forming the posteromedial capsule (Figures 2B, 3A, 3B). Hughston described the anatomy of this structure.24 The posterior oblique ligament arises from the adductor tubercle of the distal femur and has three distal attachments: 1) The prominent tibial arm on the edge of the posterior surface of the tibia; 2) the capsular arm which is continuous with the posterior capsule and the proximal part of the oblique popliteal ligament; and 3) the inferior arm which blends with the sheath covering the semimembranosus tendon and continues on to the tibia just distal to the direct insertion of the semimembranosus tendon. The deep MCL is the thick part of the middle third of the medial capsule, also known as the "middle capsular ligament" (Figure 2A). It lies in the third and deepest layer, extending from the femur to the mid-portion of the peripheral margin of the medial meniscus and inserting just below the tibial articular margin, making meniscofemoral and meniscotibial portions. In a cadaver sectioning study, the superficial MCL limits valgus and external rotation forces. On the other hand, the deep MCL and the posterior oblique ligament failed to show a significant contribution to stability in the described planes.23 However, the posterior oblique ligament was believed to assist the dynamic function of the semimembranosus tendon.24
The dynamic stabilizers of the medial side of the knee are the semimembranosus complex, the quadriceps, and the pes anserinus. The semimembranosus tendon terminates in five different insertions on the posteromedial knee: Two bony insertions on the proximal tibia just below the joint line, one into the posterior oblique ligament, one into the oblique popliteal ligament, and one into the popliteal fascia (Figures 3A, 3B). The semimembranosus plays a significant role in the dynamic stability of the medial side of the knee by tightening the normally lax posterior oblique ligament while posteriorly displacing the posterior horn of the medial meniscus to prevent impingement during knee flexion.25 The quadriceps and pes anserinus have been shown to potentially increase the effective stiffness of the MCL complex of the knee by 164 percent and 108 percent, respectively. However, the reaction time of those muscles has proved to be far too slow to protect against most sports injuries.26
BIOMECHANICS
The biomechanical properties of the MCL have been studied in both human and animal models. Areas of most intense interest include structural properties of the MCL, failure modes and failure location, effects of immobilization, and ligamentous healing.
In cadaver knees, the superficial MCL provided 57 percent of the restraining valgus moment at five degrees of knee flexion, and provided 78 percent of the moment at 25 degrees of knee flexion due to decreased contribution from the posterior capsule.27 The ultimate strength of the human MCL has been shown to be approximately equal to that of the anterior cruciate ligament (ACL).28 When testing different components separately, the maximum load was found to be 534 N for the superficial MCL, 194 N for the deep MCL, and 425 N for the posterior oblique ligament. Failure occurred at a mean elongation of 10.2 mm, 7.1 mm, and 12.0 mm respectively.29 The location of maximum strain of the entire medial collateral complex from cadaver studies was found to be near the femoral insertion when the knee was in full extension. This correlates well with a few clinical and laboratory findings that suggest the femoral insertion as the most common location for MCL injury.15,30–34 However, when considering each component separately, a cadaver study showed that the femoral attachment was the most common site of failure for the superficial MCL, but interstitial failure was more common for the deep MCL and the posterior oblique ligament.29 In contrast, operative findings in clinical series by Sims and O'Donoghue localized the tibial attachment as the most common injury site for the superficial MCL, and the femoral attachment as the most common injury site for the deep MCL and the posterior oblique ligament.25,35 A clinical series by Hughston demonstrated that the tibial insertion was the most common site of injury for all the components of the MCL complex.36
With continued displacement after MCL rupture, the ACL may also tear, producing a more extensive injury. In one study of MCL injuries, Fetto and Marshall reported the incidence of ACL tears to be 20 percent when there is no valgus laxity on clinical exam, 53 percent with laxity only in 30 degrees of knee flexion, and 78 percent with valgus laxity in full extension.1 Therefore, if the knee opens medially in extension, one must suspect that an ACL injury is likely present.
Several studies have shown that immobilization has detrimental effects on the mechanical properties of the MCL, such as disorganization of collagen fibrils, decrease in the structural properties of the bone-ligament- bone complex, and resorption of bone at ligament insertion sites.37 On the other hand, controlled motion has positive effects on healing in both animal models and clinical settings.9,20,37 Early controlled motion has become a part of standard nonoperative treatment protocols in most current series.9,10,38,39
In contrast to the ACL, the MCL has shown excellent healing capability in both animal and clinical studies.39–41 Nevertheless, the biomechanical and biochemical properties of the healing MCL fail to return to normal, making up for the deficiency by an increased mass of healing tissue.40 Attempts to improve the quality of the healing ligament have included motion and immobilization, NSAIDS, hyperbaric oxygen, energy application, and growth factors.42 From the promising results of short half-life growth factors, focus has been placed on gene transfer as a method of delivering growth factors produced by host cells over an extended treatment period.43–48 Lastly, the likelihood of satisfactory healing decreases with associated cruciate injury, valgus alignment of the knee, or injury to the deeper capsular ligament, the posterior oblique ligament, or oblique popliteal extensions from the semimembranosus.40,41,49–51
CLINICAL EVALUATION
The mechanism of injury can be obtained either from direct observation of the injury or by careful history taking. Valgus stress is the most common mechanism of injury. However, due to the position of the knee and the force vectors, a combined flexion/valgus/external rotation injury is usually the end result.52,53 The vast majority of MCL injuries are from a direct blow to the outer aspect of the lower thigh or upper leg, although non-contact valgus external rotation injuries are common in skiing.51,54
Other important information from the clinical history includes the location of pain, the ability to ambulate after the injury, time and onset of swelling, the sensation of a pop or tear, the presence of deformity, and the immediate site of tenderness.55 The absence of swelling may indicate a severe tear that allows fluid to extravasate into the surrounding tissue outside the joint. An acute effusion, within two hours of injury, indicates hemarthrosis, whereas swelling that appears 12-24 hours after injury usually indicates a synovial effusion. Seventy-six percent of patients with complete MCL tears could walk into the office unaided without any support, and pain was found to be worse in incomplete tears than complete tears.36
In Hughston's series, the location of edema and tenderness accurately localized the injury site of the superficial collateral ligaments in 64 and 76 percent of cases respectively.36 The exact location of injuries of the deep MCL and the posterior oblique ligament were found to be difficult to palpate because of their deep-seated position, but pain and tenderness in this area may at least indicate the presence of injury to these posteromedial structures, including the semimembranosus attachments.25
The best time for examination of the knee is immediately after the injury before muscle spasm occurs. Unfortunately, many times this opportunity is only available to team physicians present at the time of injury. In those patients with severe muscle spasms, a 24-hour period of immobilization is usually sufficient for relaxation, and examination under anesthesia is rarely necessary.36 While keeping the patient relaxed, a valgus stress test should be performed with the knee in 30 degrees of flexion, and compared to the contralateral knee as a control. The examination is then repeated with the knee in 0 degrees of flexion to recruit the function of remaining posteromedial structures. Any laxity appreciated from the latter test indicates a complete medial-sided injury and should lead the examiner to suspect associated injuries to the secondary restraints such as the cruciate ligaments and the posterior capsule (Figure 4).1,27 The degree of joint opening in millimeters and the quality of the end point both contribute to the overall assessment of the severity of instability.
Figure 4.
In complete medial-sided knee injuries, the injury completely tears the superficial and deep MCL, as well as the semimembranosus attachments to the femur as shown here. If the knee opens in valgus in extension, usually the posterior oblique and the oblique popliteal ligament extensions from the semimembranosus tendon are ruptured, leaving the semimembranosus attached to the tibia only. These should be repaired at the time of surgery. (Modified from Sims, WF and Jacobson, KE. The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med 2004. 32(2):337-45, permission granted.)
In addition, the examiner must perform a complete exam to rule out associated injuries to the knee. Injuries commonly seen in combination with MCL injuries include bone bruises, ACL tears, lateral collateral ligament (LCL) tears, medial meniscus tears, lateral meniscus tears, and posterior collateral ligament (PCL) tears.56 Fetto and Marshall found ACL disruption to be the most common ligamentous damage associated with MCL injuries, especially high-grade MCL tears.1 Physical examination is the most reliable method to diagnose anteromedial rotatory instability, which can occur with or without an associated ACL injury.25,57 Anteromedial rotatory instability is detected by performing the anterior drawer test while holding the tibia in external rotation.58 Any evidence of anterior subluxation of the medial tibial plateau during a valgus stress test with the knee in 30 degrees of flexion might also indicate the presence of anteromedial rotatory instability.25 Anterior instability should be carefully evaluated. Laxity with Lachman's testing, especially when the end-point is absent, is a reliable indicator of ACL rupture even in the face of MCL injury.59 The pivot shift test should be interpreted vigilantly since loss of medial pivot might cause false negative results.59 As stated earlier, the presence of a hemarthrosis is also suggestive of an associated ACL rupture. Posterior cruciate ligament injuries, meniscus injuries, and bone contusions on the lateral femoral condyle and posterolateral tibia are not unusual and should be ruled out as well.52
CLASSIFICATION
The American Medical Association (AMA) classification of MCL injuries has caused confusion and difficulty in comparison of treatment results.1,13,60 In 1976, Hughston standardized MCL injury classification, with further clarification in 1994, into two related systems: The severity system (grade I, II, III) and the laxity system (grade 1+, 2+, 3+).51 Under this combined classification system, grade I, a first-degree tear, involves a few fibers resulting in localized tenderness but no instability. Grade II, a second-degree tear, is a disruption of more fibers, with more generalized tenderness but still no instability. Grade III, a third-degree tear, is a complete disruption of the ligament, with resultant instability. Grade III injuries are subdivided according to the extent of laxity as determined by the amount of absolute joint separation from valgus stress with the knee in 30 degrees of flexion. Grade 1+, 2+, and 3+ laxities indicate 3-5 mm, 6-10 mm, and more than 10 mm of absolute medial separation respectively. The location of a tear, the presence or absence of a firm end-point, and other modifications have been added to the AMA classification system.15,53,61,62
Fetto and Marshall defined their grade I injuries as those without valgus laxity in both 0 and 30 degrees of flexion, grade II injuries as those with valgus laxity in 30 degrees of flexion but stable in 0 degrees of flexion, and grade III as those with valgus laxity in both 0 and 30 degrees of flexion.1 Of note, the authors emphasized the importance of performing the test in 0 degrees of flexion, which is different from in full extension. In full extension, there is recruitment of ACL function that can mask the laxity of the complete medial-sided injury. There is a high incidence of associated ligamentous injuries with ACL injuries in grade III cases using this classification system. We prefer this classification because it documents the instability from loss of all medial-sided structures, which may affect the treatment options. Unfortunately, the validity and reliability of any of the classification systems have not been described in the English literature. As the treatment trend moves toward conservative treatment for all grades of isolated MCL injuries, interest in classifying this ligamentous injury has declined.25 We believe that MCL injuries should, at the minimum, be classified as isolated or combined with other pathologies, which will help with treatment planning.
IMAGING STUDIES
The need for knee radiographs after injury should be determined according to the Ottawa knee rules.63 If indicated, anteroposterior, lateral, and merchant views are obtained. Stress x-rays are helpful in adolescents to exclude physeal plate injuries.64 Efforts have been made to evaluate laxity using combined stress radiographs and stress machines, but this technique has failed to become common practice, possibly due to the size and complexity of the machine.65,66
The role of MRI in the classification and treatment planning of medial-sided knee injuries has been increasing. Hayes et al. classified complex knee injuries into ten types based on the mechanism of injury.52 Recognition of these patterns may help assess the full extent of knee injuries, particularly those involving the posterolateral and posteromedial corners of the knee. A study by Nakamura et al. showed that the location of the injury in the superficial layer on MRI could help predict the outcome after conservative treatment of grade III MCL lesions combined with ACL injuries.33 After six weeks of immobilization in a knee brace, six out of 17 patients presented with residual valgus laxity on examination under anesthesia and were indicated for a medial collateral advancement or reconstruction at the time of the ACL reconstruction. Five out of the six patients had evidence of injury "over the whole length of the superficial layer."33 Indelicato recommended either a routine MRI or an arthroscopic study in all patients with laxity >10 mm to diagnose intraarticular injuries, because a capsular tear might mask a significant effusion. 55 The authors' preference is generally to use MRI only to rule out any other associated injury. In isolated Fetto and Marshall's grade I or II injuries, an MRI is not indicated. In grade III injuries, we recommend MRI evaluation to completely assess the extent of the injury and for preoperative planning.
ACUTE INJURY: TREATMENT RATIONALE AND NONOPERATIVE TREATMENT
Nonoperative care has been proposed as the mainstay treatment for the majority of isolated MCL injuries regardless of severity. Treatment with early protected range of motion exercises and progressive strengthening has been shown to produce excellent results and a high rate of return to sports.9–18 However, the current treatment recommendations have been confused by the conflicting and overlapping classification schemes. For example, Hughston's grade III injuries include different degrees of laxity from 1+ to 3+, derived from the examination of the knee in 30 degrees of flexion.36 In contrast, Fetto and Marshall's grade III injuries are unstable in 0 degrees of flexion, indicating failure of all posteromedial structures with or without ACL disruption.1
From a literature review of successful nonoperative treatment, we have found that all series claimed that "complete" or "grade III" injuries did not include patients with instability in 0 degrees of flexion, with only two exceptions.9,10,13,16,67,68 This data has given the impression that nonoperative treatment is routinely successful for even the most severe grade of isolated medial-sided knee injury. Good results have been achieved with Fetto and Marshall's grade II or Hughston's grade III injuries, with most reports uniformly supporting nonoperative treatment.15,17,18 However, for Fetto and Marshall's grade III injuries, Kannus showed that the long-term outcome of nonoperative treatment was much worse than grade I and II, with a high frequency of persistent medial instability, secondary dysfunction of the ACL, muscle weakness, and post-traumatic osteoarthritis of the injured knee.69 This supports the recommendation from Fetto and Marshall for operative treatment of all isolated type III injuries based on slightly better results in their small series.
With MRI now able to pinpoint the exact location of injury, treatment decisions are being based on the anatomic location of the MCL failure. Operative treatment has been recommended for situations where there is injury over the whole length of the superficial layer, or a complete injury of both the superficial and deep MCL from the tibia.33,70 With the exception of those injuries with laxity in extension, we treat all lesser grades of MCL injuries in a hinged knee brace with weight bearing as tolerated and crutches for initial pain relief. The patient can start isometric and range of motion exercises immediately. Crutches are discontinued when the patient can walk without limping. Anti-inflammatory medication appears to be beneficial for soft-tissue healing, but results are still inconclusive.71 For athletes, we recommend the goal-oriented rehabilitation program proposed by Reider et al. which was shown to facilitate early return to sports while having an acceptable rate of re-injury (Table 1).38 When the athlete is ready to return to practice, use of a hinged brace is encouraged initially until the athlete feels completely confident about their knee. After associated cruciate ligament injuries have been ruled out by MRI, we treat those patients with laxity at 0 degrees of flexion conservatively, as previously described. The exception is those patients with valgus knee alignment and laxity in 0 degrees of flexion. In those patients, early operative repair should be considered.
TABLE 1. Goal-oriented rehabilitation program for isolated collateral ligament sprains in athletes38 .
Initial treatment
Subsequent treatment
Goal one: Walking unassisted without a limp
Goal two: 90 degrees of knee flexion
Goal Three: Full knee motion
Goal four: Complete entire running program in one session
|
ACUTE INJURY: OPERATIVE TREATMENT
Though the majority of isolated medial-sided knee injuries can be managed nonoperatively with good results, surgeons may consider operative interventions in specific situations involving complete ligament disruption. Examples include the presence of intraarticular entrapment of the end of the ligament, a large bony avulsion, a tibial plateau fracture, a complete tibial side avulsion in athletes, or when anteromedial rotatory instability is present on physical examination (Figure 5).25,70,72–74 In addition, valgus-aligned knees with complete medial injury likely would benefit from acute repair, since these knees do not tolerate the valgus laxity well. The authors' summary of operative indications for medial-sided knee injuries is shown in Table 2.
Figure 5.
A MRI study in an acute injury reveals complete rupture of the superficial and deep MCL from the tibia. The medial meniscus is displaced medially with entrapment of the distal part of the avulsed ligament underneath it (small arrow). Severe hemarthrosis is seen. Please note the bone bruise at the lateral aspect of the lateral femoral condyle suggesting a valgus mechanism (large arrow).
TABLE 2. Summary of surgical indications for medial-sided injuries of the knee.
| Operations | Surgical Indications |
|---|---|
| Acute repair |
|
| Delayed repair |
|
| Augmentation |
|
| Reconstruction |
|
| Distal femoral varus osteotomy |
|
= Anteromedial rotary instability
Primary repair of the MCL is usually performed within seven to ten days after the injury. Location of the tear and the quality of the tendon as assessed by MRI or arthroscopic examination help guide surgical planning. 33 Femoral avulsion of the ligament leaves the best tissue for repair and the ligament can be approximated using suture anchors, staples, or a screw and washer. However, repair in this location may lead to the most problems with postoperative motion because of capsular adhesions and dysfunction of the extensor mechanism.75 Acute complete injuries with avulsion of the superficial and deep components off of the tibia can be repaired directly as well. Repair can be performed using either suture anchors or staples to secure the ligament back to its anatomic location on the proximal medial tibia after tension has been restored.70 Often mid-substance, and occasionally tibial-sided injuries, require augmentation or an allograft reconstruction due to the quality of the remaining tendon.
SURGICAL TECHNIQUE
Examination under anesthesia is performed to completely assess the scope of the injury preoperatively. Arthroscopy is performed to rule out any other associated injuries. In addition, arthroscopy can help determine the site of the deep MCL injury, either above or below the meniscus (Figure 6). In an acute setting, arthroscopy should be performed quickly and efficiently to minimize fluid extravasation. Alternatively, the surgeon may choose to do any extended arthroscopic procedures after the exposure is made, allowing it to serve as a channel for the drainage of arthroscopic fluid.
Figure 6.
The arthroscopic picture in a case of complete medial-sided knee injury demonstrates pathologic widening of the medial compartment and elevation of the meniscus from the medial tibial articular surface indicating a rupture of the meniscotibial ligament. In this case, the loose fibers of the superficial MCL are seen (arrow). With combined valgus stress and probing, we were able to identify the loose part distally so as to localize the site of the injury. Arthroscopy can also be used in chronic cases to direct the surgeon to the area of laxity below or above the joint.
An incision is made on the medial side of the knee over the suspected site of injury. To expose the entire MCL, an incision is made from the medial proximal tibia to the medial femoral epicondyle, curving posteriorly in line with the medial intermuscular septum of the thigh. For isolated repairs either distally or proximally, a more limited approach is used. In the case of combined treatment of acute complete MCL tear and an ACL tear, we have found exposure of the MCL easier if approached through a separate medial incision as opposed to extending the tibial incision for the ACL reconstruction. Care is necessary to preserve the infrapatellar branch of the saphenous nerve if possible.
The sartorial fascia is identified without undermining of the subcutaneous tissue sleeve. The crural and sartorial fascia is incised longitudinally. If dealing with a distal injury, the ruptured ends of the superficial MCL are identified beneath the gracilis and semitendinosus tendons (Figure 8A). Hematoma may be encountered in this plane and should be removed to allow direct visualization of all the injuries. The deep MCL is identified, and the tear is examined. The opening to the joint created by the tear and any injury to the meniscal attachment is inspected. We tend to use Hughston's concept of repairing all of the injured structures in anatomic position.24 The repair should begin from the deepest structure outward. A peripheral tear of the medial meniscus is commonly seen (33 percent) and nearly all of these are repairable.76 This can be done using an open technique under direct visualization. The suture knots should be placed on the outside aspect of the posterior oblique ligament in order to recreate the dynamic function of the meniscus.61 A meniscofemoral ligament tear can be directly repaired using sutures alone, or suture anchors if necessary. Suture anchor fixation into the tibial plateau is preferred for the meniscotibial ligament tear (Figures 7, 8B). If it is injured, the posterior oblique ligament is repaired by direct suture back to the femur.
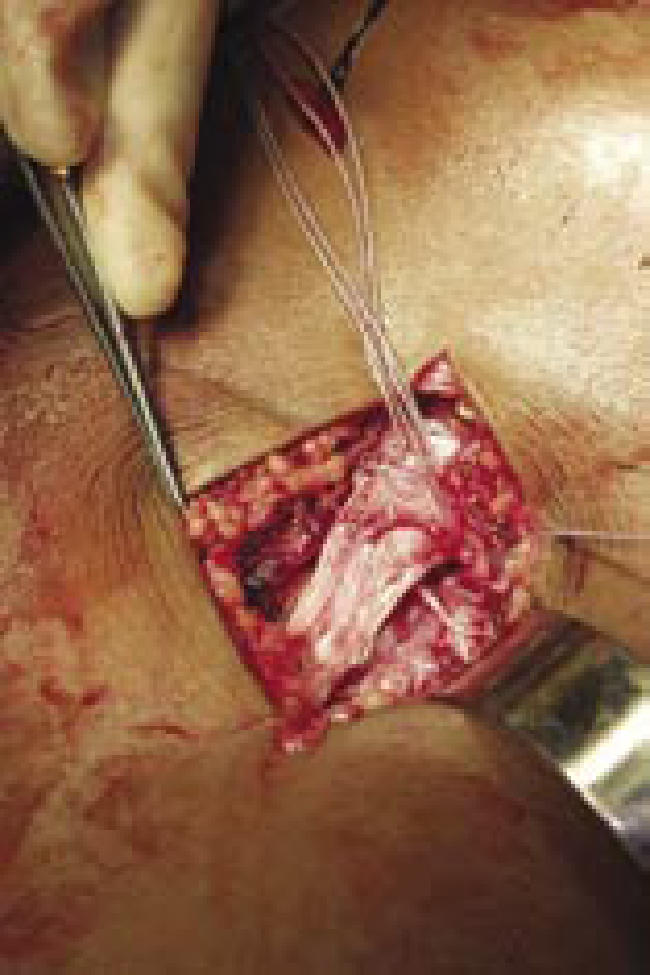
Figure 8A.

The torn end of the superficial and deep MCL is elevated demonstrating the medial joint space and the medial meniscus.
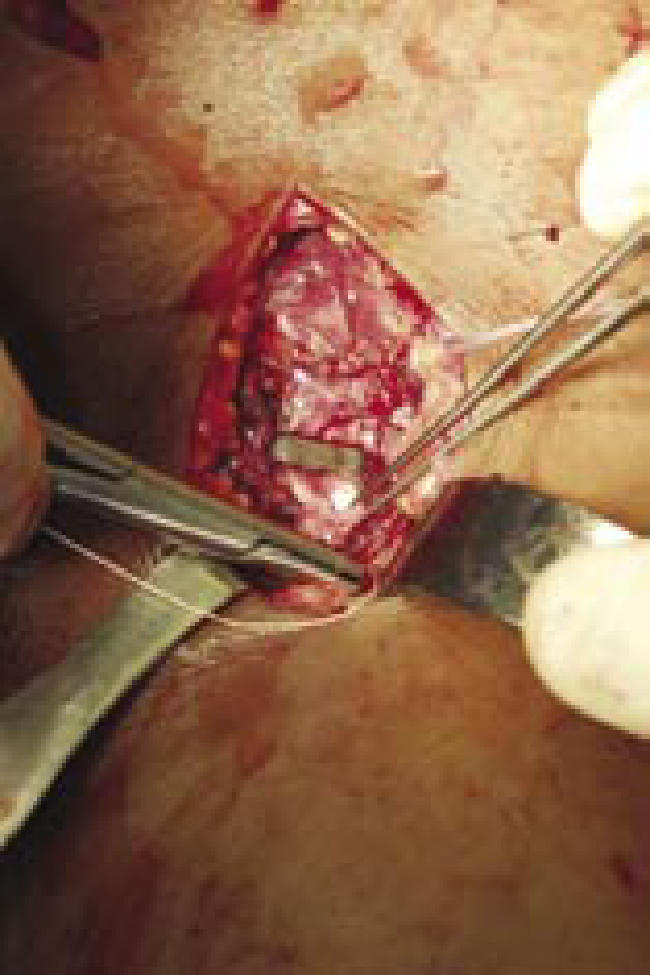
Figure 8B.
Two anchors were placed and sutures were brought through the peripheral part of the meniscus to repair the deep capsular ligament.
Figure 8C.
The torn end of the superficial MCL was secured with a staple. The very distal part of the ligament is sutured to the remaining tissue.
Figure 7.
The intraoperative fluoroscopic picture of a combined ACL reconstruction and a medial-sided knee repair is shown. The two anchors are used to hold the meniscus down to the tibia and the staple is for superficial MCL stabilization.
For tibial avulsion injuries, we prefer suture anchor fixation down to the tibial plateau just distal to the subchondral bone. Repair is completed while the knee is held in varus and full extension. A gentle valgus test should not gap open the medial joint space if the repair is adequate. The avulsed superficial MCL ends can be repaired with anchors, staples, or a screw and washer (Figure 8C). This can be aided by placing a locking suture into the substance of the torn end of the ligament that allows either proximal or distal traction to be placed on the ligament as fixation is applied. The semimembranosus portion of the posterior oblique ligament is repaired using interrupted absorbable sutures. If possible, the anterior border of the torn posterior oblique ligament can be sutured to the posterior border of the repaired MCL in a pants-over-vest fashion (Figure 9A–C). Avulsion of medial patellofemoral ligament and tearing of the vastus medialis muscle have been found in association with proximal injuries of the MCL and should be repaired if identified.57
Figure 9a.
Technique of posteromedial plication demonstrated in a case with proximal avulsion of the superficial MCL and the posterior oblique ligament. Point A demonstrates the location for suture fixation of the superficial MCL to restore tension. With the knee in 60 degrees of flexion and the hip externally rotated, the posterior oblique ligament is pulled anteriorly and proximally to point B where it is being reattached. (From Hughston, JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the ACL. Results of long-term follow-up. J Bone Joint Surg Am 1994. 76(9):1328-44, permission granted.)
Figure 9b.
The anterior aspect of the posterior oblique ligament is plicated over the superficial MCL in a pants-over-vest fashion. (From Hughston, JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the ACL. Results of long-term follow-up. J Bone Joint Surg Am 1994. 76(9):1328-44, permission granted.)
Figure 9c.
The lax capsular arm of the semimembranosus tendon is plicated over the restored posterior oblique ligament. (From Hughston, JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the ACL. Results of long-term follow- up. J Bone Joint Surg Am 1994. 76(9):1328-44, permission granted.)
If injury to the superficial MCL is extensive, augmentation of the repair may be required.77 We prefer the figure- of-eight reconstruction technique described by Gorin using autologous gracilis tendon.78 This construct has two bundles, does not interfere with the original insertion, and requires no tunnels. The augmentation can be performed through the previously described operative approach. The gracilis tendon is harvested using a tendon stripper while keeping the tibial insertion attached. The knee is brought to full extension and the deep limb of the figure-of-eight is secured with a suture anchor placed in a bony trough at the posterior aspect of the medial epicondyle. The tendon is stabilized at another anchor fixation point just anterior to the femoral footprint. With the knee in 30 degrees of flexion, the superficial limb of the reconstruction is fixed to the tibia with a suture anchor approximately 2 cm posterior and deep to the pes anserinus insertion. Finally, the tourniquet is deflated and inspection and control of potential excessive bleeding from the inferior medial geniculate artery and its branches is performed. A compressive dressing is applied postoperatively.
POSTOPERATIVE CARE
The patient is kept non-weight bearing for three weeks in a long hinged knee brace allowing 30-90 degrees of motion. At 3 weeks the patient is allowed to do full range of motion and weight bearing as tolerated. Progressive activities are started at about six weeks and the brace is gradually weaned off.
CHRONIC INJURY
Although rare, chronic valgus instability has been described following MCL injury alone or in combination with ACL tears.49,77,79–81 This combination has been found to seriously compromise joint stability, and patients with this injury are more likely to experience symptoms of giving way than those with isolated ACL deficiency.1,57,82 Slocum defined "late" or "chronic" as three months or more after the acute injury.83 By that time, the ligaments have lost their healing potential and the anatomic restoration of the traumatized tissue is no longer possible due to the contracture of the ligament ends and the formation of scar tissue. Multiple reconstruction techniques have been described focusing mainly on reconstruction of the superficial MCL with quadriceps tendon autograft, hamstring autograft, hamstring allograft, or Achilles allograft. 77,79,81 Patients with valgus deformity of the knee should have hip-to-ankle radiographs and may need a distal femur varus-producing osteotomy prior to ligament reconstruction in order to move the mechanical axis into slight varus. Persistent valgus malalignment will cause graft stretching and recurrence of the instability if not corrected.49,84 For chronic medial instability we prefer the technique modified from Toth and Warren's description, using Achilles allograft for reconstruction of the superficial MCL.85
SURGICAL TECHNIQUE
Examination under anesthesia is performed to document all deficient structures. Arthroscopy can be done to rule out and treat intra-articular pathologies if indicated. The surgical exposure is performed using a hockey-stick approach as described above. The soft tissue flaps are mobilized with a larger inferior flap, allowing exposure of the fascia over the MCL. The sartorial/crural fascia is incised and reflected anteriorly and posteriorly. The native superficial MCL is identified and dissected. The soft spot between the posterior aspect of the superficial MCL and the posterior oblique ligament is sharply developed for future possible plication. The center of rotation of the knee joint is identified using a pin technique. A guide pin is drilled into the medial epicondyle parallel to the joint line along the epicondylar axis. One end of suture is fixed to the tibia at the approximate insertion of the superficial MCL. The other end is looped over the pin and the knee is taken through its range of motion. The length of the suture should not change more than 2 mm if the center axis is correct. An approximately 10 mm reamer is used to make a tunnel 2.5-3 cm in depth, carefully avoiding penetration into the intercondylar notch. We have found allograft bone plugs smaller than 10 mm in diameter to be less reliable and more apt to break during preparation and fixation. An Achilles allograft is prepared so that the calcaneal bone plug can fit into the 10 mm sizer with preservation of the tendon insertion and periosteum on one side. The 10 mm x 10 mm x 25 mm bone plug is inserted into the tunnel, either freely or using traction sutures and a Beath pin, and fixed with an interference screw on the cancellous side of the bone plug.
The tendinous part of the graft can be fixed to the tibia in two ways. The first method, described next, involves drilling a tunnel in the tibia. The soft tissue expanse of the Achilles graft is whip-stitched for 4-6 cm with #2 Ticron sutures and then sizing is performed. Using a 10-mm reamer, a tibial tunnel is made approximately 5 cm distal to the joint line and just posterior to the gracilis insertion. The graft is pre-tensioned, and the knee is moved through a range of motion several times. A Beath pin is then inserted freehand into the tunnel aiming about one centimeter lateral to the tibial crest to avoid injury to the peroneal nerve. The graft is pulled into the tunnel and fixed with a soft tissue interference screw while the knee is held in 30 degrees of flexion, valgus, and internal rotation. Alternatively, the broad expanse of the Achilles graft is drawn distally with locking traction sutures. It then can be fixed in place with two staples or with suture anchors at its anatomic location. Again, the leg should be held in varus at 30 degrees of flexion during fixation.
We then evaluate the posterior oblique ligament. With the knee in 60 degrees of flexion and hip in external rotation, the posterior oblique ligament is advanced anteriorly and proximally. It is then fixed to the adductor tubercle using suture anchors. The sutures are tied when the knee is brought to near-full extension. The anterior border of the posterior oblique ligament is sutured over the reconstructed MCL in a pants-over-vest fashion. The wound is closed and a compressive dressing is applied.
POSTOPERATIVE CARE
Generally, we use the same protocols previously described for postoperative care after an acute repair.
COMBINED INJURY
Treatments for combined ACL and MCL injuries are still developing. Early reconstruction of both the ACL and MCL may lead to motion loss postoperatively.86 Reconstructing only the medial-sided structures is supported only by limited groups.50,57 Many authors recommend ACL reconstruction after a period of rehabilitation to allow the MCL to heal.54,76,87 Surgery is performed after achieving full range of motion and adequate strength, and after resolution of the knee effusion, which typically occurs approximately six weeks after the injury. The caveat to this method is that the severity of the knee injuries is not totally clear in studies supporting this technique. Such variation in the original injury would definitely impact the outcome. For example, a knee with grade 3+ laxity in 30 degrees of flexion that is stable in extension is different from a knee that opens medially in extension. Therefore, at the time of ACL reconstruction, examination under anesthesia must be performed to determine the residual laxity to valgus stress. We use a residual difference between legs of more than 3-4 mm with valgus stress at full extension as an indication for MCL reconstruction.33,76 The techniques of MCL repair, augmentation, and reconstruction are the same as previously described in isolated injuries.
COMPLICATIONS
The most common complications from the medial-sided knee repair or reconstruction are knee stiffness and residual laxity.61 Knee stiffness can be associated with the timing of repairs, non-anatomic repairs, and problems with postoperative rehabilitation.61 Stabilizing the superficial MCL too close to the joint line can capture the knee. Residual instability generally stems from failure to address all the components of the injury, especially the meniscus and posteromedial structures. Repeated examinations during the various stages of repair are important to provide optimal stability. In addition, awareness of the restraining structures for various knee flexion angles is crucial to correct repair or reconstruction.27 Pellegrini-Stieda lesions are sometimes painful, and if nonoperative treatments fail, a resection with a repair may be required.88 In general, most complications can be avoided using the appropriate surgical and postoperative strategies as previously described.
SUMMARY
MCL and medial-sided knee injuries are still major problems in the modern era of sports medicine. With advances in imaging techniques and refined grading of injuries, surgical treatment for medial-sided knee injuries, once popularized by Hughston, may have a role in many cases.
Long-term studies of the most severe category of MCL injuries are needed to define the best treatment. Nonetheless, most medial-sided injuries are best treated nonoperatively, with proven great success.
References
- 1.Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop. 1978;132:206–218. [PubMed] [Google Scholar]
- 2.Peterson L, et al. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28(5 Suppl):S51–S57. doi: 10.1177/28.suppl_5.s-51. [DOI] [PubMed] [Google Scholar]
- 3.Najibi S, Albright JP. The use of knee braces, part 1: Prophylactic knee braces in contact sports. Am J Sports Med. 2005;33(4):602–611. doi: 10.1177/0363546505275128. [DOI] [PubMed] [Google Scholar]
- 4.Warme WJ, et al. Ski injury statistics, 1982 to 1993, Jackson Hole Ski Resort. Am J Sports Med. 1995;23(5):597–600. doi: 10.1177/036354659502300514. [DOI] [PubMed] [Google Scholar]
- 5.Lorentzon R, Wedren H, Pietila T. Incidence, nature, and causes of ice hockey injuries. A three-year prospective study of a Swedish elite ice hockey team. Am J Sports Med. 1988;16(4):392–396. doi: 10.1177/036354658801600415. [DOI] [PubMed] [Google Scholar]
- 6.Tegner Y, Lorentzon R. Evaluation of knee braces in Swedish ice hockey players. Br J Sports Med. 1991;25(3):159–161. doi: 10.1136/bjsm.25.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paulos LE, et al. The biomechanics of lateral knee bracing. Part I: Response of the valgus restraints to loading. Am J Sports Med. 1987;15(5):419–429. doi: 10.1177/036354658701500501. [DOI] [PubMed] [Google Scholar]
- 8.Koehle MS, Lloyd-Smith R, Taunton JE. Alpine ski injuries and their prevention. Sports Med. 2002;32(12):785–793. doi: 10.2165/00007256-200232120-00003. [DOI] [PubMed] [Google Scholar]
- 9.Reider B, et al. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994;22(4):470–477. doi: 10.1177/036354659402200406. [DOI] [PubMed] [Google Scholar]
- 10.Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop. 1990;256:174–177. [PubMed] [Google Scholar]
- 11.Pforringer W, Beck N, Smasal V. Conservative therapy of ruptures of the medial collateral ligament of the knee. Results of a comparative follow-up study. Sportverletz Sportschaden. 1993;7(1):3–7. doi: 10.1055/s-2007-993477. [DOI] [PubMed] [Google Scholar]
- 12.Petermann J, von Garrel T, Gotzen L. Non-operative treatment of acute medial collateral ligament lesions of the knee joint. Knee Surg Sports Traumatol Arthrosc. 1993;1(2):93–96. doi: 10.1007/BF01565459. [DOI] [PubMed] [Google Scholar]
- 13.Ballmer PM, Jakob RP. The nonoperative treatment of isolated complete tears of the medial collateral ligament of the knee. A prospective study. Arch Orthop Trauma Surg. 1988;107(5):273–276. doi: 10.1007/BF00451505. [DOI] [PubMed] [Google Scholar]
- 14.Sandberg R, et al. Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. J Bone Joint Surg Am. 1987;69(8):1120–1126. [PubMed] [Google Scholar]
- 15.Ellsasser JC, Reynolds FC, Omohundro JR. The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56(6):1185–1190. [PubMed] [Google Scholar]
- 16.Jones RE, Henley MB, Francis P. Nonoperative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop. 1986. pp. 137–140. [PubMed]
- 17.Holden DL, Eggert AW, Butler JE. The nonoperative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med. 1983;11(5):340–344. doi: 10.1177/036354658301100511. [DOI] [PubMed] [Google Scholar]
- 18.Derscheid GL, Garrick JG. Medial collateral ligament injuries in football. Nonoperative management of grade I and grade II sprains. Am J Sports Med. 1981;9(6):365–368. doi: 10.1177/036354658100900605. [DOI] [PubMed] [Google Scholar]
- 19.Buckwalter J. Iowa and Eugene, Oregon, Orthopaedics. Iowa Orthopaedic Journal. 2003;23:123–129. [PMC free article] [PubMed] [Google Scholar]
- 20.Tipton CM, et al. Influence of exercise on strength of medial collateral knee ligaments of dogs. Am J Physiol. 1970;218(3):894–902. doi: 10.1152/ajplegacy.1970.218.3.894. [DOI] [PubMed] [Google Scholar]
- 21.James SL. Surgical anatomy of the knee. Fortschr Med. 1978;96(4):141–146. 166. [PubMed] [Google Scholar]
- 22.Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: An anatomical analysis. J Bone Joint Surg Am. 1979;61(1):56–62. [PubMed] [Google Scholar]
- 23.Warren LA, Marshall JL, Girgis F. The prime static stabilizer of the medical side of the knee. J Bone Joint Surg Am. 1974;56(4):665–674. [PubMed] [Google Scholar]
- 24.Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55(5):923–940. [PubMed] [Google Scholar]
- 25.Sims WF, Jacobson KE. The posteromedial corner of the knee: Medial-sided injury patterns revisited. Am J Sports Med. 2004;32(2):337–345. doi: 10.1177/0363546503261738. [DOI] [PubMed] [Google Scholar]
- 26.Pope MH, et al. The role of the musculature in injuries to the medial collateral ligament. J Bone Joint Surg Am. 1979;61(3):398–402. [PubMed] [Google Scholar]
- 27.Grood ES, et al. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am. 1981;63(8):1257–1269. [PubMed] [Google Scholar]
- 28.Kennedy JC, et al. Tension studies of human knee ligaments. Yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone Joint Surg Am. 1976;58(3):350–355. [PubMed] [Google Scholar]
- 29.Robinson JR, Bull AM, Amis AA. Structural properties of the medial collateral ligament complex of the human knee. J Biomech. 2005;38(5):1067–1074. doi: 10.1016/j.jbiomech.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 30.Gardiner JC, Weiss JA, Rosenberg TD. Strain in the human medial collateral ligament during valgus loading of the knee. Clin Orthop. 2001. pp. 266–274. [DOI] [PubMed]
- 31.Gardiner JC, Weiss JA. Subject-specific finite element analysis of the human medial collateral ligament during valgus knee loading. J Orthop Res. 2003;21(6):1098–1106. doi: 10.1016/S0736-0266(03)00113-X. [DOI] [PubMed] [Google Scholar]
- 32.Kawada T, et al. Analysis of strain distribution in the medial collateral ligament using a photoelastic coating method. Med Eng Phys. 1999;21(5):279–291. doi: 10.1016/s1350-4533(99)00051-x. [DOI] [PubMed] [Google Scholar]
- 33.Nakamura N, et al. Acute grade III medial collateral ligament injury of the knee associated with anterior cruciate ligament tear. The usefulness of magnetic resonance imaging in determining a treatment regimen. Am J Sports Med. 2003;31(2):261–267. doi: 10.1177/03635465030310021801. [DOI] [PubMed] [Google Scholar]
- 34.Bergfeld J. Symposium: functional rehabilitation of isolated medial collateral ligament sprains. First-, second-, and third-degree sprains. Am J Sports Med. 1979;7(3):207–209. doi: 10.1177/036354657900700317. [DOI] [PubMed] [Google Scholar]
- 35.O'Donoghue DH. Surgical treatment of fresh injuries to the major ligaments of the knee. Clin Orthop. 1991. pp. 3–8. [PubMed]
- 36.Hughston JC, et al. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58(2):159–172. [PubMed] [Google Scholar]
- 37.Woo S, et al. The response of ligaments to injury: Healing of the collateral ligaments. In: D DM, A WH, OC JJ, editors. Knee Ligaments: Structure, Function, Injury, and Repair. New York: Raven Press; 1990. pp. 351–364. [Google Scholar]
- 38.Reider B. Medial collateral ligament injuries in athletes. Sports Med. 1996;21(2):147–156. doi: 10.2165/00007256-199621020-00005. [DOI] [PubMed] [Google Scholar]
- 39.Indelicato PA. Isolated medial collateral ligament injuries in the knee. J Am Acad Orthop Surg. 1995;3(1):9–14. doi: 10.5435/00124635-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Anderson DR, et al. Healing of the medial collateral ligament following a triad injury: a biomechanical and histological study of the knee in rabbits. J Orthop Res. 1992;10(4):485–495. doi: 10.1002/jor.1100100404. [DOI] [PubMed] [Google Scholar]
- 41.Woo SL, Vogrin TM, Abramowitch SD. Healing and repair of ligament injuries in the knee. J Am Acad Orthop Surg. 2000;8(6):364–372. doi: 10.5435/00124635-200011000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Creighton R, Spang J, Dahners L. Basic science of ligament healing: medial collateral ligament healing with and without treatment. Sports Med Arthrosc Rev. 2005;12(3):145–150. [Google Scholar]
- 43.Woo SL, et al. Functional tissue engineering for ligament healing: potential of antisense gene therapy. Ann Biomed Eng. 2004;32(3):342–351. doi: 10.1023/b:abme.0000017551.93144.1a. [DOI] [PubMed] [Google Scholar]
- 44.Day CS, et al. Myoblast-mediated gene transfer to the joint. J Orthop Res. 1997;15(6):894–903. doi: 10.1002/jor.1100150616. [DOI] [PubMed] [Google Scholar]
- 45.Nakamura N, et al. Decorin antisense gene therapy improves functional healing of early rabbit ligament scar with enhanced collagen fibrillogenesis in vivo. J Orthop Res. 2000;18(4):517–523. doi: 10.1002/jor.1100180402. [DOI] [PubMed] [Google Scholar]
- 46.Nakamura N, et al. A comparison of in vivo gene delivery methods for antisense therapy in ligament healing. Gene Ther. 1998;5(11):1455–1461. doi: 10.1038/sj.gt.3300765. [DOI] [PubMed] [Google Scholar]
- 47.Shimomura T, et al. Antisense oligonucleotides reduce synthesis of procollagen alpha1 (V) chain in human patellar tendon fibroblasts: potential application in healing ligaments and tendons. Connect Tissue Res. 2003;44(3-4):167–172. doi: 10.1080/03008200390215872. [DOI] [PubMed] [Google Scholar]
- 48.Hildebrand KA, Frank CB, Hart DA. Gene intervention in ligament and tendon: current status, challenges, future directions. Gene Ther. 2004;11(4):368–378. doi: 10.1038/sj.gt.3302198. [DOI] [PubMed] [Google Scholar]
- 49.Cameron JC, Saha S. Management of medial collateral ligament laxity. Orthop Clin North Am. 1994;25(3):527–532. [PubMed] [Google Scholar]
- 50.Frolke JP, Oskam J, Vierhout PA. Primary reconstruction of the medial collateral ligament in combined injury of the medial collateral and anterior cruciate ligaments. Short-term results. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):103–106. doi: 10.1007/s001670050081. [DOI] [PubMed] [Google Scholar]
- 51.Hughston JC. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76(9):1328–1344. doi: 10.2106/00004623-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 52.Hayes CW, et al. Mechanism-based pattern approach to classification of complex injuries of the knee depicted at MR imaging. Radiographics. 2000;20 Spec No:S121–S134. doi: 10.1148/radiographics.20.suppl_1.g00oc21s121. [DOI] [PubMed] [Google Scholar]
- 53.Perryman JR, Hershman EB. The acute management of soft tissue injuries of the knee. Orthop Clin North Am. 2002;33(3):575–585. doi: 10.1016/s0030-5898(01)00003-7. [DOI] [PubMed] [Google Scholar]
- 54.Pressman A, Johnson DH. A review of ski injuries resulting in combined injury to the anterior cruciate ligament and medial collateral ligaments. Arthroscopy. 2003;19(2):194–202. doi: 10.1053/jars.2003.50054. [DOI] [PubMed] [Google Scholar]
- 55.Indelicato P, Linton R. Medial ligament injuries in the adult. In: Delee J, Drej JD, Miller M, editors. DeLee & Drez's Orthopaedic Sports Medicine. Philadelphia, PA: Saunders; 2003. pp. 1938–1949. [Google Scholar]
- 56.Garvin GJ, Munk PL, Vellet AD. Tears of the medial collateral ligament: magnetic resonance imaging findings and associated injuries. Can Assoc Radiol J. 1993;44(3):199–204. [PubMed] [Google Scholar]
- 57.Hughston JC, Barrett GR. Acute anteromedial rotatory instability. Long-term results of surgical repair. J Bone Joint Surg Am. 1983;65(2):145–153. doi: 10.2106/00004623-198365020-00002. [DOI] [PubMed] [Google Scholar]
- 58.Kurimura M, et al. Factors for the presence of anteromedial rotatory instability of the knee. J Orthop Sci. 2004;9(4):380–385. doi: 10.1007/s00776-004-0797-0. [DOI] [PubMed] [Google Scholar]
- 59.Donaldson WF, 3rd, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations. Initial versus examination under anesthesia. Am J Sports Med. 1985;13(1):5–10. doi: 10.1177/036354658501300102. [DOI] [PubMed] [Google Scholar]
- 60.Chicago: American Medical Association; 1968. Standard nomenclature of athletic injuries. [Google Scholar]
- 61.Jacobson KE. Technical pitfalls of collateral ligament surgery. Clin Sports Med. 1999;18(4):847–882. doi: 10.1016/s0278-5919(05)70188-5. [DOI] [PubMed] [Google Scholar]
- 62.Cox JS. Symposium: functional rehabilitation of isolated medial collateral ligament sprains. Injury nomenclature. Am J Sports Med. 1979;7(3):211–213. doi: 10.1177/036354657900700319. [DOI] [PubMed] [Google Scholar]
- 63.Stiell IG, et al. Use of radiography in acute knee injuries: need for clinical decision rules. Acad Emerg Med. 1995;2(11):966–973. doi: 10.1111/j.1553-2712.1995.tb03123.x. [DOI] [PubMed] [Google Scholar]
- 64.Zionts LE. Fractures around the knee in children. J Am Acad Orthop Surg. 2002;10(5):345–355. doi: 10.5435/00124635-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 65.Jacobsen K. Stress radiographical measurement of the anteroposterior, medial and lateral stability of the knee joint. Acta Orthop Scand. 1976;47(3):335–344. doi: 10.3109/17453677608992002. [DOI] [PubMed] [Google Scholar]
- 66.Kennedy JC, Fowler PJ. Medial and anterior instability of the knee. An anatomical and clinical study using stress machines. J Bone Joint Surg Am. 1971;53(7):1257–70. [PubMed] [Google Scholar]
- 67.Indelicato PA. Non-operative treatment of complete tears of the medial collateral ligament of the knee. J Bone Joint Surg Am. 1983;65(3):323–329. [PubMed] [Google Scholar]
- 68.Indelicato PA. Nonoperative management of complete tears of the medial collateral ligament. Orthop Rev. 1989;18(9):947–952. [PubMed] [Google Scholar]
- 69.Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop. 1988;226:103–112. [PubMed] [Google Scholar]
- 70.Wilson TC, Satterfield WH, Johnson DL. Medial collateral ligament "tibial" injuries: indication for acute repair. Orthopedics. 2004;27(4):389–393. doi: 10.3928/0147-7447-20040401-15. [DOI] [PubMed] [Google Scholar]
- 71.Dahners LE, Mullis BH. Effects of nonsteroidal anti-inflammatory drugs on bone formation and soft-tissue healing. J Am Acad Orthop Surg. 2004;12(3):139–143. doi: 10.5435/00124635-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 72.Lobenhoffer P. [Complex instability of the anterior knee]. Orthopade. 2002;31(8):770–777. doi: 10.1007/s00132-002-0334-9. [DOI] [PubMed] [Google Scholar]
- 73.Delamarter RB, Hohl M, Hopp E., Jr Ligament injuries associated with tibial plateau fractures. Clin Orthop. 1990;250:226–233. [PubMed] [Google Scholar]
- 74.Kuroda R, et al. Avulsion fracture of the posterior oblique ligament associated with acute tear of the medial collateral ligament. Arthroscopy. 2003;19(3):E18. doi: 10.1053/jars.2003.50069. [DOI] [PubMed] [Google Scholar]
- 75.Robins AJ, Newman AP, Burks RT. Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries. The effect of medial collateral ligament rupture location. Am J Sports Med. 1993;21(1):20–25. doi: 10.1177/036354659302100104. [DOI] [PubMed] [Google Scholar]
- 76.Noyes FR, Barber-Westin SD. The treatment of acute combined ruptures of the anterior cruciate and medial ligaments of the knee. Am J Sports Med. 1995;23(4):80–89. doi: 10.1177/036354659502300402. [DOI] [PubMed] [Google Scholar]
- 77.Bosworth DM. Transplantation of the semitendinosus for repair of laceration of medial collateral ligament of the knee. J Bone Joint Surg Am. 1952;34-A(1):196–202. [PubMed] [Google Scholar]
- 78.Gorin S, Paul DD, Wilkinson EJ. An anterior cruciate ligament and medial collateral ligament tear in a skeletally immature patient: a new technique to augment primary repair of the medial collateral ligament and an allograft reconstruction of the anterior cruciate ligament. Arthroscopy. 2003;19(10):E21–E26. doi: 10.1016/j.arthro.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 79.Umansky AL. The Milch fasciodesis for the reconstruction of the tibial collateral ligament. J Bone Joint Surg Am. 1952;34-A(1):202–206. [PubMed] [Google Scholar]
- 80.O'Donoghue DH. Reconstruction for medial instability of the knee. J Bone Joint Surg Am. 1973;55(5):941–954. [PubMed] [Google Scholar]
- 81.Borden PS, Kantaras AT, Caborn DN. Medial collateral ligament reconstruction with allograft using a double-bundle technique. Arthroscopy. 2002;18(4):E19. doi: 10.1053/jars.2002.32235. [DOI] [PubMed] [Google Scholar]
- 82.Warren RF, Marshall JL. Injuries of the anterior cruciate and medial collateral ligaments of the knee. A long-term follow-up of 86 cases--part II. Clin Orthop. 1978;136:198–211. [PubMed] [Google Scholar]
- 83.Slocum DB, Larson RL, James SL. Late reconstruction procedures used to stabilize the knee. Orthop Clin North Am. 1973;4(3):679–689. [PubMed] [Google Scholar]
- 84.Paley D, et al. New procedures for tightening knee collateral ligaments in conjunction with knee realignment osteotomy. Orthop Clin North Am. 1994;25(3):533–555. [PubMed] [Google Scholar]
- 85.Toth A, Warren R. Medial side injuries of the knee: Acute and chronic Management. In: Callaghan J, Rosenberg A, Rubash H, editors. The adult knee. Philadelphia, PA: Lippincott Williams & Wilkins; 2003. pp. 801–822. [Google Scholar]
- 86.Petersen W, Laprell H. Combined injuries of the medial collateral ligament and the anterior cruciate ligament. Early ACL reconstruction versus late ACL reconstruction. Arch Orthop Trauma Surg. 1999;119(5-6):258–262. doi: 10.1007/s004020050405. [DOI] [PubMed] [Google Scholar]
- 87.Shelbourne KD, Porter DA. Anterior cruciate ligament- medial collateral ligament injury: nonoperative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am J Sports Med. 1992;20(3):283–286. doi: 10.1177/036354659202000308. [DOI] [PubMed] [Google Scholar]
- 88.Wang JC, Shapiro MS. Pellegrini-Stieda syndrome. Am J Orthop. 1995;24(6):493–497. [PubMed] [Google Scholar]