Abstract
Amputation osteoplasty is a technique modification promoted by Ertl to enhance rehabilitation after transtibial amputation. Two different techniques for creating sealing of the medullary canal and a distal bone block have been described in the literature. One technique consists of a periosteal sleeve that is sutured over the cut end of the bone. The second technique consists of hinging a segment of fibula into a slot in the cut end of the tibia. The desired goal of amputation osteoplasty is to create an end-bearing limb to enhance rehabilitation. In addition to creation of a bone bridge, Ertl also recommends myoplasty, neuroplasty, individual vessel ligation, and a special skin closure. This report is a small case series of five patients successfully treated with lower extremity amputation osteoplasty, to illustrate the techniques and report initial good results. Two patients had each of the techniques and one patient had both of the techniques. All five patients had good wound healing, accelerated rehabilitation, and the ability to use end-bearing prostheses.
INTRODUCTION
Amputations have been performed for severe disease since the beginning of recorded human history. There is probably no other orthopaedic procedure that has been performed longer or more often than amputation. Many of the important techniques and principles of amputation have remained standard for decades. However, over the past 20 years, new ideas and techniques have been developed that may improve the outcomes, recovery rates, and ultimate function of patients with amputations.1,2
One of these concepts is osteoplasty, or sealing of the medullary canal of the amputated bone. This technique is potentially applicable to all amputations, regardless of location or disease process.3,4,5 It can be utilized with amputations done for post-traumatic, diabetic, infectious, dysvascular, neoplastic, developmental, or other conditions. The technique can be used for adult or pediatric amputations.
It is useful to compare and contrast amputations and disarticulations, which have both been used for centuries. 6 A disarticulation is removal of a limb through a joint and requires resection of ligaments. Amputation is removal of a limb by cutting through bone, typically requiring a saw or other bone-cutting instruments. The primary motivation for disarticulation versus amputation in the past has been the fact that disarticulation does not require an instrument to cut the bone, but rather a knife to cut through soft tissue ligaments. In addition, disarticulation preserves length, allows for end-bearing ability, and is not complicated by overgrowth in skeletally immature patients. With a disarticulation, the medullary canal of the bone is not exposed to the surrounding tissue. In contrast, conventional amputation without osteoplasty does expose the medullary canal of the bone to the surrounding tissue. Historically, this has not been thought to present a significant problem for the patient. However, there has been growing evidence over the last 20 years that the open medullary canal may be the source of significant post-amputation problems for patients.7,8,9
Vascularity of the residual limb may be enhanced in several ways. Sealing of the end of the bone may improve medullary blood flow as it restores a more normal osseous contour to the bone end. Angiographic studies by Ertl showed sluggish flow and bulbous vessels within and distal to the cut bone of traditional amputations but a near-normal medullary vessel pattern after amputation osteoplasty. Individual ligation of vessels helps to prevent arteriovenous fistulas and pseudoaneurysms associated with traditional methods of ligation of vessel bundles. These vascular abnormalities can cause pain and interfere with residual limb function, especially with an end-bearing prosthesis. End-bearing also helps to mechanically pump blood out of the residual limb, similar to what occurs in the normal foot during walking.
Ertl has devised specific techniques to create sealing callus at the end of the cut bone of an amputation through what has been termed "amputation osteoplasty."9 He has also promoted a variety of other modifications and specific techniques for amputations.9,10 The osteoplasty concept has also been associated with an end-bearing limb for prosthetic wear. Especially for transtibial amputations (TTA's), end-loading prostheses were historically avoided because of their association with unacceptable rates of wound and residual limb breakdown. Instead, prostheses were designed to transfer weight-bearing to the knee and more proximally in order to functionally unload the end of the residual limb.5,11
Traditional amputation prostheses were designed to be suspended on the residual limb, bypassing the end of the limb and obtaining their support more proximally. For TTA's, this required weight-bearing contours around the knee. For trans-femoral amputations this meant quadrilateral sockets and ischial weight bearing. Traditionally, diabetic patients were known to have particular problems with skin breakdown with end-bearing prostheses.
With Ertl osteoplasty, an end-bearing limb is the desired result to facilitate rehabilitation. This is completely different from traditional thinking. Ertl believes that the residual limb should be as normal as possible, and this includes the transmission of load along the length of the residual bone and end bearing as occurs in normal walking with a normal limb. The surgical techniques are designed to create an end-bearing "organ" that is capable of holding up to axial load. The osteoplasty is designed to provide a broad base to accept load and eliminate motion (chop-sticking) between the distal tibia and fibula. The periosteal sleeve and myoplasty help create a soft tissue "organ" capable of end-bearing load that will withstand the forces of body weight. The skin closure technique also helps.
While end-bearing on the residual limb of a traditional amputation leads to breakdown, end-bearing on the residual limb after amputation osteoplasty can be beneficial. End bearing can actually stimulate this skin and deep tissue "organ" to become stronger and tougher over time. The loaded end-bearing limb promotes tissue maintenance rather than atrophy of the residual limb attributable to disuse (penciling).
The proposed advantages to end-bearing include tissue maintenance (less atrophy), less pain, more normal sensation and blood flow, improved walking, and improved prosthetic wear. In contrast to a suspended prosthesis that gives the patient the sensation of instability, end-bearing facilitates rehabilitation by providing better proprioception. End-bearing prostheses are easier to apply and remove and some patients may even be able to get around somewhat without a prosthesis-something that is virtually impossible with traditional amputations.
Two major forms of osteoplasty have been recommended for TTA's. One is an osteoperiosteal flap over the end of the tibia. The other is a fibular bone block transversely rotated. Both of these techniques are designed to seal the medullary canal, stabilize the distal tibia and fibula, and provide the potential for end-bearing of the residual limb with use of a prosthesis.2
The Ertl osteoplasty consists of the development of a short anterior and a long posterior periosteal flap off of the tibial shaft. The posterior periosteal flap should measure approximately six centimeters distal to the level of tibial amputation. This periosteal flap is several millimeters thick and is taken with an osteotome and some flakes of bone, especially from the posterior cortex of the tibia. Muscle origin tissue, tendinous in nature, is also utilized in the development of these anterior and posterior flaps. These flaps are then sutured over the tibial osteotomy site as a pouch to help seal off the medullary canal. In addition to the bone chips adherent to the periosteum, supplemental cancellous bone slurry is placed into the pouch once it is sewn over the end of the tibia. A similar technique can be accomplished with the fibula, or the periosteum can be sutured in such a way as to cover the cut ends of both the tibia and the fibula. This osteoplasty is then combined with myoplasty and soft tissue closure under no tension to create a residual limb capable of end bearing.9,10,12
The fibular bone block technique consists of an osteotomy of the fibula, which is then hinged on a lateral periosteal sleeve transversely into a notch on the lateral aspect of the amputated distal tibia. Sutures through drill holes can be utilized to secure this bone block on both the tibia and fibula. The periosteal blood supply to this bone block is maintained through muscle attachments during the preparation. This bone block can also be covered with a periosteal sleeve as described above to further stabilize the bone block and improve sealing of the medullary canal and development of a tough tissue at the end of the bone capable of end bearing. This also helps transmit load to the distal fibula. The bone block technique also stabilizes the distal tibia and fibula, which has been postulated to improve rehabilitation and prosthetic usage.2,12
MATERIALS AND METHODS
We report five cases utilizing osteoplasty as a part of lower limb amputation (four transtibial amputations and one transfemoral amputation). The cases are shown to illustrate indications, techniques, and short-term outcome with early weight bearing.
The first two cases in the series utilized a fibular cortical bridge without a periosteal sleeve. There were two cases that utilized the periosteal sleeve without a fibular cortical bridge. The fifth case utilized a fibular cortical bridge combined with a periosteal sleeve.
Case 1
A 29-year-old male with chronic recalcitrant osteomyelitis was referred eight years after an open right tibial shaft fracture at the junction of the distal one-quarter and proximal three-quarters of the tibia. He had undergone 12 previous operations that succeeded in achieving bony union but had a persistent draining infection and pain that prevented him from working. Despite rotational, free flap, and split thickness skin grafting, he had unstable skin posteromedially. He was treated with a transtibial amputation with a hinged fibular cortical bone bridge that was recessed into the lateral aspect of the tibia using the technique described previously (Figures 1A, 1B). Although there was adequate fibular length, the area of chronic osteomyelitis of the tibia was too proximal to develop a good periosteal flap and maintain a margin of normal tibia between the infection and the amputation site. Therefore the periosteal flap technique was not used. The wound healed and the bone bridge consolidated by six months (Figures 1C, 1D). There was no recurrence of infection. The patient was able to walk with an end-bearing prosthesis at eight weeks, which facilitated his eventual return to work at 11 months.
Figure 1A.

(Case 1) AP radiograph of a transtibial amputation with fibular cortical bone block.
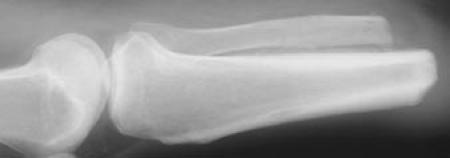
Figure 1B.

Lateral radiograph. Note the notching of the tibia to provide maximum bone surface for healing and the drill holes that were utilized for suture fixation.
Figure 1C.

AP radiograph at 6 months demonstrates healing of the bone bridge.
Figure 1D.

Lateral radiograph confirms healing. There is some ectopic bone formation posterior to the fibula.
Case 2
A 47-year-old female had a chronic recalcitrant infected nonunion of a distal metaphyseal tibia fracture that had been initially treated with a plate. After multiple operative procedures, she still had a malpositioned nonunion with Pseudomonas osteomyelitis and a very poor soft tissue envelope. She underwent transtibial amputation with a fibular cortical bone block. Again the area of infection was thought to be too proximal to safely allow the development of a periosteal flap. The wound healed and the bone bridge consolidated by eight months. The patient was able to walk with an end-bearing prosthesis at 12 weeks and eventually returned to work at 12 months.
Case 3
A 32-year-old male sustained multiple trauma (ISS 25) with injuries including left 3C open femur and tibial shaft fractures. The other extremities were successfully salvaged, but he required an acute guillotine transfemoral amputation (TFA). The patient survived and the TFA was revised with a periosteal sleeve amputation osteoplasty and wound closure 14 days after injury. The limb healed and sealing callus developed by 14 weeks. The patient was able to walk with an end-bearing prosthesis and returned to work after seven months.
Case 4
A 52-year-old male had brittle insulin-dependent diabetes and chronic recurring ulcers. In 1999, he was treated with a disarticulation at the first MTP. In 2002, he underwent a transmetatarsal amputation for new ulcers. The amputation site healed, but he developed ulcers over the heel and ankle two years later. In 2004, he underwent a TTA with a periosteal sleeve osteoplasty of the tibia. No bone block was used due to concerns about cortical bone healing. The wound healed, and sealing callus developed by 20 weeks postoperatively. The patient was able to walk with an end-bearing prosthesis and returned to work after three months. Figures 2A and 2B show the radiographic appearance after twelve months.
Figures 2A, B. (Case 4) AP (a) and lateral (b) radiograph of a TTA with periosteal sleeve osteoplasty. At one year it has the radiographic appearance of a standard TTA. There is sealing callus over the medullary canal of the distal tibia with periosteal new bone.
Figure 2A.

Figure 2B.
Case 5
A 49-year-old unemployed diabetic had chronic recurring ulcers over the heel and ankle. He sustained an open trimalleolar fracture of the distal tibia and fibula with plafond involvement. He was neuropathic with no pain and little sensation. Despite operative stabilization, he developed an infected nonunion. He underwent TTA with osteoplasty that included a hinged fibular cortical bone block covered by a periosteal sleeve with bone slurry as described previously (Figures 3A, 3B). His wound healed, and he was wearing a prosthesis by three months after surgery. An end-bearing prosthesis was allowed at that point. The bone block consolidated by six months (Figures 3C, 3D) with additional subperiosteal bone formation distal to the bone block. Unfortunately he remained unemployed.
Figures 3A, B. (Case 5) AP and lateral radiographs of patient with a TTA with both fibular bone block and ostealperiosteal sleeve.
Figures 3C, D. AP and lateral radiographs at 6 months demonstrating good healing of the fibular bone block with additional new bone formation beneath the periosteal sleeve.
Figure 3A.

Figure 3B.

Figure 3C.
Figure 3D.
RESULTS
All five patients underwent amputation osteoplasty. Five of five patients had good wound healing and function of the residual limb. All patients had radiographic evidence of sealing of the medullary canal and healing of the bone bridge by six months. All patients were able to use an end-bearing prosthesis, including the two patients with diabetes.
DISCUSSION
This small case series with short follow-up illustrates the techniques of amputation osteoplasty. Although adult tibial periosteum itself may only be a few cell layers thick, we found that it was possible to raise a soft tissue flap from the surface of the tibia that included some tendinous tissue that was 1-2 mm thick. This flap could be sutured over the cut end of bone or the fibular cortical bone block to create an osteoplasty. Similarly, it was possible to osteotomize the fibula and obtain sufficient stability of the bone block, by suture fixation through drill holes and the creation of a slot in the posterolateral aspect of the tibia, to achieve healing in these cases. All of the patients healed and had good functional use of end-bearing prostheses. For transtibial amputations with ample available length, the use of a fibular bone bridge supplemented by a periosteal sleeve is the most appealing technique. The periosteal sleeve method can be used alone for transfemoral and other amputation sites.
The Ertl website gives additional information about the technique.9,10 They emphasize that osteoplasty alone is not the only important step in the "osteomyoplastic amputation reconstruction." Five key steps are recommended: 10
Osteoplasty with periosteal sleeve.
Individual ligation of vessels.
Injection of all five nerves followed by proximal resection.
Myoplasty.
Even skin closure.
A variety of misconceptions appear in the literature. The use of a fibular cortical bone block is a form of osteoplasty but is not the technique recommended by Ertl. This cortical bone block is another way to achieve stabilization of the distal tibia and fibula, sealing of the medullary canal, and the potential for end bearing.
Although a variety of anesthetic and sclerosing medications have been advocated to prevent neuroma formation, in this series we injected the cut end of each of the nerves with 0.5cc of 0.25% marcaine to provide initial post-operative pain relief. The nerves were individually identified and put on tension before being sharply divided, injected, and allowed to retract deep within the residual limb. For TTAs, these nerves included the tibial, superficial peroneal, deep peroneal, saphenous, and sural nerves.
There are drawbacks to osteoplasty. It is more time consuming to perform than traditional amputation. There are concerns about healing problems with the more extensive dissection. The rate and reliability of the formation of the bone bridge has not been completely established. The benefits are primarily theoretical. Although there is significant data and clinical interest, Level I data to demonstrate improved outcomes is not yet available.13,14,15 There may be specific contraindications to the procedure, particularly within the zone of traumatic injury.2,16
Although end bearing has traditionally been avoided, especially in diabetic patients, there is also a different perspective developing among prosthetists. Some have observed that diabetic patients initially have significant edema, followed by severe atrophy of the residual limb. Such patients will almost always "bottom out" in their prostheses eventually. This requires multiple adjustments, and liner and socket changes over time. These same patients may also suffer from skin breakdown around the knee and fibular head. By creating a residual limb with the capacity for end loading, the diabetic patients in this series appeared to have less initial swelling, less tissue atrophy, and fewer problems with pressure sores from their prostheses. We did delay weight bearing for six weeks to allow for good soft tissue healing. Determining if the bone bridge is healed on radiographs is somewhat difficult. However, we did observe a slower rate of bone bridge consolidation in the diabetic patients, who required six months to achieve the radiographic appearance seen in non-diabetic patients after three months.
Further study will be required to determine healing rates, optimal techniques, indications and contraindications, and to conclusively demonstrate functional advantages of the technique of amputation osteoplasty over traditional amputation techniques.
SUMMARY
The technique of amputation osteoplasty is an intriguing modification of a common procedure, and early success with this technique warrants further investigation and consideration.
References
- 1.Ertl J. Operationstechik. Dieser abschnitt solder Veroffentlichung der von einzelnen Chirurgen geubten operativen Technik dienen. Uber Amputationsstumpfe. Chirug. 1949;20:218–224. [Google Scholar]
- 2.Dougherty PJ, Smith DG. Amputations and Prosthetics. In: Baumgaertner MR, Tornetta P, editors. Orthopaedic Knowledge Update. Trauma 3. American Academy of Orthopaedic Surgeons Publishing; 2006. pp. 78–79. [Google Scholar]
- 3.Larsen RD, O'Neal RM. The use of osteoperiosteal flaps in amputations in the hand: preliminary report. Plastic Reconstructive Surg. 1966;38(6):529. doi: 10.1097/00006534-196638060-00006. [DOI] [PubMed] [Google Scholar]
- 4.Dougherty PJ. Long-term follow-up of unilateral transfemoral amputees from the Vietnam War. J Trauma. 2003;54:718–723. doi: 10.1097/01.TA.0000046260.16866.A9. [DOI] [PubMed] [Google Scholar]
- 5.Dougherty PJ. Transtibial amputees from the Vietnam War: Twenty-eight year follow-up. J Bone Joint Surg Am. 2001;83:383–289. doi: 10.2106/00004623-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Levay D. The history of orthopaedics. Vol. 21. The Parthenon Publishing Group; 1990. Amputations and prosthetics; p. 1990. [Google Scholar]
- 7.Erikson U, Huith A. Circulation of amputation stumps. Arteriographic and skin temperature studies. Acta Orthop Scand. 1962;32:159. doi: 10.3109/17453676208989570. [DOI] [PubMed] [Google Scholar]
- 8.Hansen-Leth C. Muscle blood flow after amputation with special reference to the influence of osseous plugging of the medullary cavity. Acta Orthop Scand. 1976;47:613–618. doi: 10.3109/17453677608988747. [DOI] [PubMed] [Google Scholar]
- 9.Ertl JW, Ertl JP, Ertl WJ, Stokosa J. The Ertl osteomyoplastic transtibial amputation reconstruction. Medical papers page. Ertl reconstruction website. Available at www.ertlreconstruction.com .
- 10.Bone Bridge. Medical papers page. Available at www.bonebridge.com .
- 11.McCullough NC, Harris AR, Hampton FL. Atlas of limb prosthetics. St Louis, MO: CV Mosby; 1980. Below knee amputation; pp. 3–5. [Google Scholar]
- 12.Deffer PA, Moll JH, LaNoue AM. The Ertl osteoplastic below knee amputation. J Bone Joint Surg. 1971;53A:1028. [Google Scholar]
- 13.MacKenzie EJ, Bosse MJ, Castillo RC, et al. Functional outcomes following trauma-related lower-extremity amputation. J Bone Joint Surg. 2004;86:1636–1645. doi: 10.2106/00004623-200408000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Bosse MJ, MacKenzie EJ, Kellam JF, et al. An analysis of outcomes of reconstruction or amputation of leg-threatening injuries. N Engl J Med. 2002;347:1924–1931. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 15.Smith DG, Horn P, Malchow D, Boone DA, Reiber GE, Hansen ST., Jr Prosthetic history, prosthetic charges, and functional outcome of the isolated traumatic below-knee amputee. J Trauma. 1995;38:44–47. doi: 10.1097/00005373-199501000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Smith DG. Amputation techniques in war surgery. In Motion. 2003;13:42–43. [Google Scholar]