Abstract
We sought to evaluate the efficacy of daily pulsed low intensity ultrasound (LIUS) with early return to activities for the treatment of lower extremity stress fractures.
Eight patients (2 males, 6 females) with radiographic and bone scan confirmed tibial stress fractures participated in this study. Additionally, a case report of a tarsal navicular stress fracture is described. All patients except one were involved in athletics. Prior to the study, subjects completed a 5 question, 10 cm visual analog scale (VAS) regarding pain level (10 = extreme pain, 1 = no pain) and were assessed for functional performance. Subjects received 20-minute LIUS treatments 5 times a week for 4 weeks. Subjects maintained all functional activities during the treatment period. Seven patients with posterior-medial stress fractures participated without a brace. Subjects were re-tested after 4 weeks of treatment. Mann-Whitney U tests (VAS data) and paired t-tests (functional tests) assessed statistical significance (p<0.05).
Although the intensity of practice was diminished in some instances, no time off from competitive sports was prescribed for the patients with the tibial stress fractures. The patient with the anterior tibial stress fracture underwent tibial intramedullary nailing at the conclusion of a season of play.
In this uncontrolled experience, treatment of tibial stress fractures with daily pulsed LIUS was effective in pain relief and early return to vigorous activity without bracing for the patients with posterior-medial stress fractures.
INTRODUCTION
It has been estimated that up to 5% to 10% of all sports-related injuries involve stress fractures6,7,9,10. The tibia has surpassed the metatarsals to become the most common location for the development of stress fracture6,8,5. Traditional treatment has included rest, relative rest, casting and ambulatory braces and results in substantial loss of time from activities. Recently, the AIRCAST™ pneumatic tibial brace with an anterior pad hastened return to recreational activities11. Use of this brace shortened the time out of strenuous activities from 77 +/- 7 days to 21 +/- 2 days in a prospective randomized trial comparing traditional methods of stress fracture treatment 11.
Non-invasive daily pulsed LIUS (Exogen, Piscatway, New Jersey) therapy hastened tibial fracture2 and distal radius fracture healing4. Consolidation time of spine fusion improved with daily pulsed LIUS13. No research has reported success with the use of low-intensity pulsed ultrasound in the acceleration of stress fracture healing. We sought to evaluate the efficacy of daily pulsed LIUS for the treatment of tibial stress fractures with early return to activities. Our goals were to avoid losing time out of an athleteís short competitive season, and avoid brace treatment for sporting activities, as sports such as soccer make it difficult to wear a brace in competition.
MATERIALS AND METHODS
Eight patients with a positive bone scan (Figure 1) and one case of MRI documented stress fracture were treated with daily pulsed LIUS and immediate return to usual activities. There were 3 males and 6 females, 8 of the 9 patients were high school or college level athletes. Seven patients had posterior-medial tibial stress fractures and one patient, a female college level basketball player, suffered from an anterior tibial stress fracture diagnosed in the pre-season conditioning period. One patient had a tarsal navicular stress fracture diagnosed with MRI. The athletic patients participated in soccer and basketball.
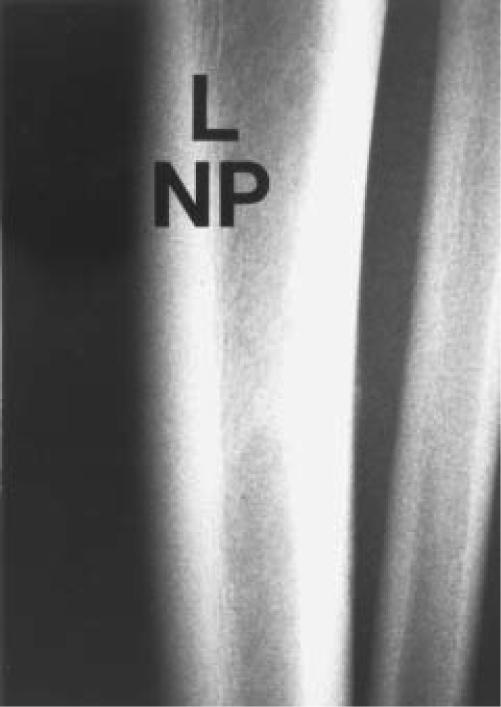
Figure 1.
N.P. is a 19 year old white male college level soccer play who complained of posterior-medial pain along the mid portion of the tibia.
Figure 1A.
(A) Plain radiographs of the tibia and fibula showing a small "cloud" of periosteal reaction consistent with a tibial stress fracture at the posterior-medial border of the left tibia. The accompanying bone scan confirmed the diagnosis.
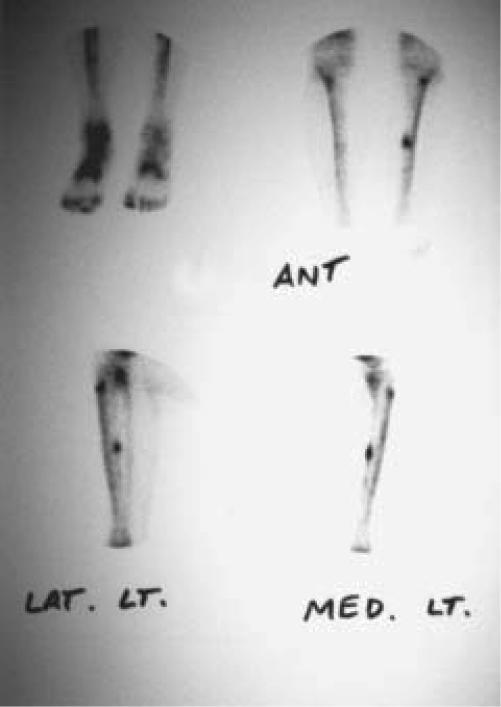
Figure 1B.
(B) The bone scan is of both tibias. Increased uptake is noted along the posterior-medial border of the left tibia in the diaphysis.
Patients were identified at the sports medicine clinic, where a history, physical exam, plain radiographs and nuclear medicine technetium bone scan were performed for the patients with tibial stress fractures. The patient with a tarsal navicular stress fracture had his diagnosis made by MRI. A pre-test and post-test of functional activities were administered in Physical Therapy. Prior to the study, subjects completed a 5 question, 10 cm visual analog scale (VAS) regarding pain level (10 = extreme pain, 1 = no pain) and were assessed for functional performance. Subjects received 20 minutes daily pulsed LIUS treatments of operating frequency = 1.5 MHz, radiating area = 3.88 cm2, pulse width = 200 microseconds and temporal average power=117 mW that were administered 5 treatments/week for 4 weeks. Patients with tibial stress fractures maintained all functional activities during the treatment period. Eight patients participated without bracing, one patient with an anterior tibial stress fracture participated with the AIRCAST™ pneumatic tibial brace with an anterior pad because of the risk for fracture during activities. The remaining patients wore an AIRCAST™ pneumatic tibial brace with an anterior pad when not participating in activities or sports. Subjects were then re-tested after 4 weeks of treatment. Mann-Whitney U tests (VAS data) and paired t-tests (functional tests) assessed statistical significance to the p<0.05 level.
Case Report
W.B. was a 20 year old African American male, Division II college level basketball player, who in early December of 1997 landed awkwardly on his foot. The foot was painful over the dorsal posterior mid-foot, in the area of the anterior tibialis tendon. He attempted to play, which he was able to do with an antalgic limp. The range of motion (ROM) was symmetric to the opposite foot. Tenderness was palpable diffusely across the dorsal mid-foot and did not localize to a discreet area. Single leg hop was similar to the opposite foot but painful. Taping, NSAIDS, ultrasound, electrical stimulation, ice and shoe modification failed to improve his pain or allow athletic participation. Pain improved immediately with an injection of local anesthetic and a cortisone compound in the area of the anterior tibialis attachment onto the tarsal navicular, but relief failed to be sustained for a significant time frame.
Plain radiographs of the foot did not reveal an explanation for his pain. An MRI, 12/16/97, of the foot was obtained, to evaluate soft tissues. A tarsal navicular stress fracture was evident (Figure 2).
Figure 2.
W.B. is a 20 year old African American male, college level basketball player with an MRI documented tarsal navicular fracture. This image is from 12/16/97, before treatment was initiated. The stress fracture is visualized across the entire width of the tarsal navicular on the coronal view. The fracture line can be seen extending into subchondral bone.
Six weeks of NWB casting, while the standard treatment for this injury12,3, would have likely ended his competitive season. Because, we had used the daily pulsed LIUS effectively in tibial stress fractures, we proceeded to treat his injury with equally hopeful results. Fortunately, his injury coincided with almost two weeks of rest from competitive basketball because of his school's holiday break. His treatment included the Sonic Accelerated Fracture Healing System (SAFHS) (Exogen, Piscatway, New Jersey) device and three and a half weeks of non-weight bearing crutch walking in a brace, which was removed for physical therapy. On a graded basis, activities were added, and ultimately returned to competition at 5 weeks after his injury.
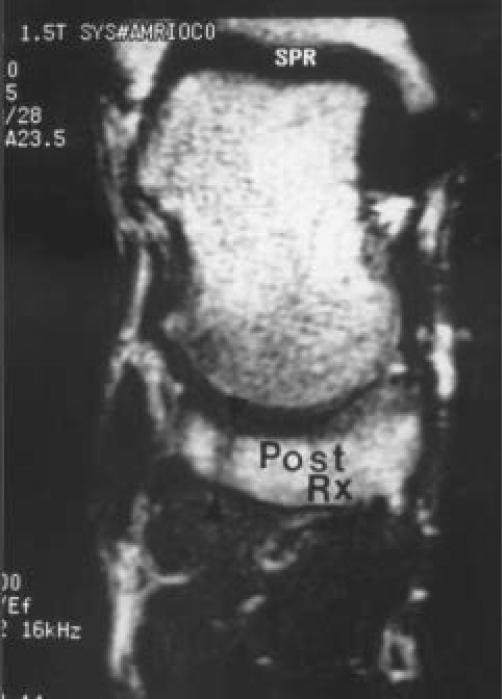
A repeat MRI, 1/27/98, demonstrated early consolidation of the stress fracture (Figure 3).
Figure 3.
This is the post treatment MRI from 1/27/98, which was obtained before he was allowed to return to competitive basketball. The fracture line appears less distinct, not as long and the articular margins appear to show consolidation of the fracture line. This is the coronal view, which is similar to the view from Figure 2.
RESULTS
All subjects resumed or maintained sporting activities at the same level as at the time of diagnosis. No adverse sequelae or recurrence of symptoms occurred in the seven patients with the posterior-medial stress fractures or in the patient with the tarsal navicular stress fracture. The patient with the anterior tibial stress fracture underwent tibial intramedullary nailing after a successful season of competition.
The results of functional testing both before and after treatment are in Table I.
TABLE I. Summary of the results of the functional testing of patients before and after treatment.
| Stepdowns/ 1 min | Pain with Palpation | |
|---|---|---|
| Pre-Treatment | 28 ± 7 repetitions | 7.5 ± 2 |
| Post-Treatment | 36 ± 5 repetitions | 3.3 ± 3 |
| Mean Difference | 8 ± 6 more repetitions | 4.3 ± 3 reduced pain |
| P | 0.02 | 0.02 |
DISCUSSION
No tibial stress fracture patients were removed from athletic activities because of their injuries. The patient with the tarsal navicular fracture missed five weeks of season, but this included two weeks Christmas vacation when his team had time off from practice and competition. This mode of treatment is remarkably different from the traditional treatment of tarsal navicular stress fractures, which is six weeks of non-weight bearing (NWB) casting3,12. Our patient was treated with a removable brace and three and one-half weeks of NWB.
Objective improvement in the tibial stress fractures was documented using reported scales1. Our mode of treatment was successful in compression, posterior-medial, stress fractures. The one patient with an anterior or tension side fracture didnít respond to low intensity pulsed ultrasound treatment and required intramedullary nailing of her stress fracture at the end of the competitive season. So, this method of treatment may not be useful in this type of tibial stress fracture.
This is the first reported use of this technique to accelerate healing for lower extremity stress fractures. Daily pulsed Low-Intensity Pulsed Ultrasound significantly minimized time off from normal activities. This is a comparatively expensive form of treatment and medical reimbursement may be an issue. Thus, further review would be advised. A prospective, controlled randomized trial is the obvious next step, if not here perhaps another center. This treatment method may be useful in the select instance of a high demand athlete who cannot afford time away from competition to rehabilitate this injury. Until efficacy is documented with a randomized prospective trial, reimbursement by insurance carriers may not be forthcoming.
ACKNOWLEGMENTS
Thank you to Paula Hurley, M.S. Ed. for her editorial assistance.
References
- 1.Flandr y F, Hunt JP, Terr y GC, Hughston JC. Analysis of subjective knee complaints using visual analog scales. Am J Sports Med. 1991;19:112–118. doi: 10.1177/036354659101900204. [DOI] [PubMed] [Google Scholar]
- 2.Heckman JD, Ryaby JP, McCabe J, Frey JJ, Kilcoyne RF. Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. J Bone and Joint Surg. 1994 Jan;76-A:26–34. doi: 10.2106/00004623-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Khan KM, Fuller PJ, Brukner PD, Kearney C, Burry HC. Outcome of conservative and surgical management of navicular stress fracture in athletes. Eight-six cases proven with computerized tomography. Am J of Sports Med. 1992;20:657–666. doi: 10.1177/036354659202000606. [DOI] [PubMed] [Google Scholar]
- 4.Kristiansen TK, Ryaby JP, McCabe J, Frey JJ, Roe LR. Accelerated healing of distal radius fractures with the use of specific, low-intensity ultrasound. A multicenter, prospective, randomized, double-blind, placebo-controlled study. J Bone and Joint Surg. 1997 Jul;79-A:961–973. doi: 10.2106/00004623-199707000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Maitra RS, Johnson DL. Stress fractures: Clinical History and Physical Examination. Clin Sports Medicine. 1997 Apr;16:259–274. doi: 10.1016/s0278-5919(05)70021-1. [DOI] [PubMed] [Google Scholar]
- 6.Meyer S. Stress fractures of the foot and leg. Clin Sports Med. 1993;12:395. [PubMed] [Google Scholar]
- 7.Monteleone G. Stress fractures in the athlete. Orthop Clin North Am. 1995;26:423. [PubMed] [Google Scholar]
- 8.Renstrom P. Mechanism, diagnosis, and treatment of running injuries. Instr Course Lect. 1993;42:225–234. [PubMed] [Google Scholar]
- 9.Smrcina C. Stress fractures in athletes. Nurs Clin North Am. 1991;26:159. [PubMed] [Google Scholar]
- 10.Sterling J, et al. Stress fractures in the athlete: Diagnosis and management. Sports Med. 1992;14:336. doi: 10.2165/00007256-199214050-00005. [DOI] [PubMed] [Google Scholar]
- 11.Swenson EJ, DeHaven KE, Sebastianelli WJ, Hanks G, Kakenak A, Lynch JM. The effect of a pneumatic leg brace on return to play in athletes with tibial stress fractures. Am J of Sports Med. 1997 May–June;25:322–328. doi: 10.1177/036354659702500309. [DOI] [PubMed] [Google Scholar]
- 12.Torg JS, Pavlov H, Cooley LH. Stress fracture of the tarsal navicular. J Bone and Joint Surg. 1982 Jun;64A:700–712. [PubMed] [Google Scholar]
- 13.Whitecloud TS. Spine fusions heal more quickly with ultrasound in animal model. Orthopedics Today. 1997 Dec;17(1 & 36) [Google Scholar]