Abstract
Lamellar inclusions of the rough endoplasmic reticulum in growth plate chondrocytes, first identified (1972) in the Department of Orthopaedic Surgery, University of Iowa, has become the cytochemical hallmark for the pseudoachondroplastic dysplasia (PSACH) phenotype, linking an endoplasmic reticulum storage disorder with the osteochondrodysplasia. Since this original observation, great advances have been made, leading to the molecular understanding of this altered longitudinal bone growth anomaly. A PSACH canine model suggested that abatement of cumulative vertical growth of growth plate chondrocytes seen in PSACH results from (1) altered extracellular matrix constraints for horizontal growth and (2) uncoupling of endochondral and perichondral growth that causes metaphyseal flaring. PSACH, an autosomal dominant disease, is linked to mutation of the cartilage oligomeric matrix protein (COMP) gene. Amino acid substitutions, deletions, or additions is proposed to alter COMP structure that cause its retention in the rough endoplasmic reticulum of growth plate chondrocytes, leading to (1) compositional and structural change of the extracellular matrix, and (2) altered cellular proliferation and volume expansion. Normal growth and development occurs in COMP gene knockout mice that do not synthesis COMP, demonstrating that a mutant COMP, not absence of COMP, is required for the PSACH phenotype. The mechanism by which mutant COMP induces a PSACH phenotype remains to be elucidated.
At the University of Iowa a cell culture system has been developed whereby mutant COMP transgenes are introduced into chondrocytes and the expressed product COMP is retained in the endoplasmic reticulum. This readily manipulated system makes it possible to decipher systematically the system's cellular secretory processing pathway, in order to clarify the mechanism(s) by which the mutant COMP is retained within the endoplasmic reticulum. Concurrent with this is the development of transgenic mice expressing the mutant COMP used in the cell culture system. This will make it possible to establish that expression of a human PSACH-linked mutant COMP will produce a PSACH phenotype. A PSACH animal model will provide a means to characterize the mechanism of altered longitudinal bone growth and to test gene therapy approaches for correcting the anomaly.
INTRODUCTION
Maroteaux and Lamey in 1959 were the first to separate pseudoachondroplastic dysplasia (PSACH) from the complex group of spondylo-epiphyseal dysplasias as the pseudoachondroplastic type44. PSACH presents some features the similar to those of achondroplasia and Morquio's disease but does not match the phenotype of either disease44. A decreased longitudinal bone growth is seen in both PSACH and achondroplasia. Cranial and facial normal features are seen in PSACH, however, in contrast to achondroplasia. An onset of approximately 2 years is required to usually identify skeletal dysplasia with PSACH, while altered bone growth is seen at birth in achondroplasia. Abnormalities of the vertebrae and pelvis are present in PSACH as in Morquio's disease. Lack of (1) corneal opacities and (2) keratan sulfate in the urine distinguish PSACH phenotype from Morquio's disease40.
Mutant gene linkage studies support the clinical findings that PSACH is a separate type of osteochondrodysplasia. Autosomal dominant linkage of the extracellular matrix protein, cartilage oligomeric matrix protein (COMP), located at chromosome 19p13.18,24 is linked with PSACH9,25. Achondroplasia is linked with mutation of fibroblast growth factor receptor-3 gene located at chromosome 4p16.357 and Morquio's disease (mucopolysaccharidosis type IVA) is linked with mutation of galactosamine-6-sulfatase gene (chromosome 16q24.3)2.
CLINICAL EVALUATION
Hall and Dorst22 classified PSACH into four types, a dominant mild and severe type (formally designated types I and III) and a recessive mild and severe type (formally designated types II and IV). However, recent genetic and natural history studies have refined the demarcation between type classification. Germline/somatic mosaicism identified in apparently unaffected parents of two or more siblings with PSACH previously diagnosed with autosomal recessive inheritance21,23, demonstrates that PSACH is, in fact, an autosomal dominant disease. Mild versus severe PSACH phenotype is poorly delineated clinically, and natural history is more informative in describing the degree of musculoskeletal involvement in PSACH. Limb dwarfism is identifiable at childhood being reflected at onset of altered longitudinal bone growth. The head and facial features are normal. Lumbar lordosis, kyphosis, scoliosis, and atlantoaxial dislocation are features that can be found in the spine. Neurological chronic cervical cord compression myelopathy occurs resulting from atlantoaxial dislocation. Brachydactyly, without trident hand, telescoping fingers, and ulnar deviation of wrist are seen in the limbs. Limited elbow and hip extension and ligamentous laxity are seen in the joints accompanied with genu valgum and bowleg. Radiographic evaluation shows platyspondyly, tongue-shaped anterior vertebrae, short pedicles, short tubular bones, widened metaphyses, and fragmented irregular epiphyses. No extraskeletal medical problems are associated with PSACH46,66.
The natural history of PSACH is associated with early onset of arthritis. Weight bearing joints of the knee, hip, and foot at ~20 years of age are first in showing signs of arthritic pain46. The elbow, shoulder, and neck can be affected later in life. Windswept deformity, knock knees, bowed legs, scoliosis, and cervical spine instability are frequently present and commonly require corrective surgery intervention at adolescence. Total hip replacement is often required at an earlier age than in normal individuals. Whether the abnormal composition (extracellular matrix formation) of the femoral head / acetabulum and joint laxity or in some instances formation of shallow acetabuli or protrusio acetabuli during growth is responsible for onset of the arthritis has yet to be delineated.
HISTOMORPHOMETRIC EVALUATION
Altered longitudinal bone growth is the most apparent phenotype seen in PSACH individuals. Long bone growth entails the conversion of an expanding cartilage template into trabecular bone through the process of endochondral ossification. Growth plate chondrocytes subsequently undergo a program of matrix expansion during hypertrophy, calcification, and cell death. The calcified, hypertrophic cartilage provides a scaffold for the formation of trabecular bone. Continuous proliferation of the chondrocytes with cell and matrix expansion dictates the length of the limb through adolescence. In PSACH individuals, dramatically reduced limb lengthening appears to result from altered expansion of the extracellular matrix and longitudinal growth of the chondrocytes prior to ossification.
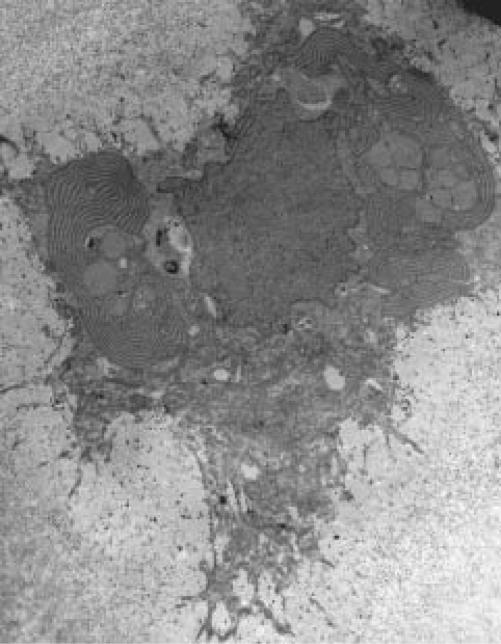
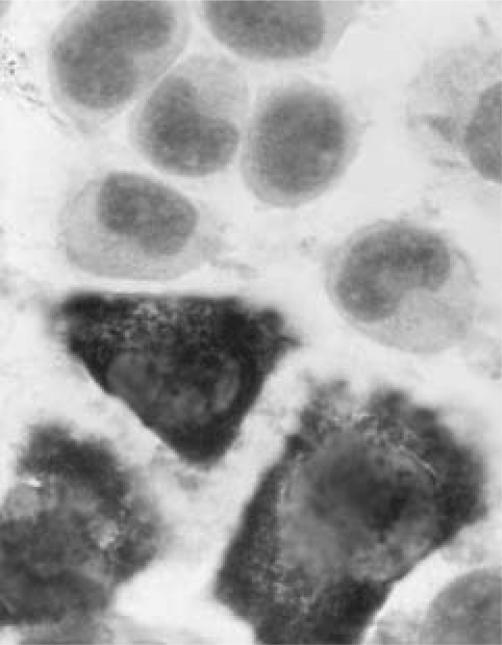
Light microscopy analyses of epiphyses and metaphyses identified an array of abnormal chondrocytes in PSACH, suggesting altered maturation and potential proliferation of chondrocytes affects longitudinal growth. In the advent of electron microscopic examination of the chondrocytes, Lindseth et al.40 observed "occasional inclusion bodies of unidentified nature within the chondrocytes" and "endoplasmic reticulum was not prominent" within the chondrocytes. Maynard et al.45 identified accumulation of alternately electron-lucent and electron-dense layers of material in the rough endoplasmic reticulum, forming extensive lamallae (Figure 1), in affected chondrocytes of the growth plate and proposed that PSACH is a rough-surfaced endoplasmic reticulum storage disorder11,45. The extracellular matrix molecules 1) aggrecan59–61, 2) COMP16,26,42, and 3) type IX collagen26,42 have since been identified in the lamellar structures, suggesting that defects in post-translational processing of the core proteins lead to their retention in the cell. It is important to note, however, that this is not a general defect in protein processing. Type II collagen secretion, for example, is unaffected60. Rather, the data imply that the defect affects a subset of extracellular matrix molecules that includes aggrecan, COMP, and type IX collagen.
Figure 1.
Transmission electron micrograph of a pseudoachondroplastic dysplasia growth plate chondrocyte identifying alternately electron-lucent and electron-dense layers of material in the rough endoplasmic reticulum, the cytochemical hallmark pattern associated with pseudoachondroplastic dysplasia. Magnification = 3,900x.
PSACH ANIMAL MODEL
A human PSACH phenotype has been identified in a Scottish deerhound dog pedigree5,6. As seen in humans, no skeletal abnormalities were observed at birth and first evidence of chondrodysplasia was detected at four to five weeks of age. Kyphosis and limb deformities gradually developed with radiographic shorter long bones and vertebrae, irregular and delayed ossification, and metaphyseal flaring. Joint laxity was additionally noted with increase of age, suggesting ligament involvement. With closure of the proximal distal and radial growth plates, the radii were 65% shorter in length than age matched normal animals. One litter, with three animals being dwarf and two animals being phenotypically normal, was sacrificed at 17 weeks of age for histocytochemical and stereological analyses6. Chondrocytes of the proximal and distal growth plates of the radius and costochondral junctions of the sixth rib contained alternately electron-lucent and electron-dense layers of material in the rough endoplasmic reticulum within chondrocytes as seen in the human PSACH. Weightbearing load to the growth plates was not found to be a factor in inducing the lamellar inclusions of the chondrocytes since the inclusions were also present in the non-weight-bearing growth plates of the ribs. In the articular cartilage of the distal radius, lamellar inclusions were limited to chondrocytes of the deep zone, but were not present in chondrocytes of the superfical zone, indicating specificity in altered chondrocyte phenotype of growth plates.
Distal radial growth plates of dwarf Scottish deerhounds showed no difference in thickness to age matched normal littermates. However, abnormalities that included disruption of the normal columnar arrangement, apparent hypocellularity, and irregularity of the hypertrophic chondrocyte-ossification junction were seen in the metaphysis. The bone septa were thicker in the dwarf dogs, suggesting altered endochondral ossification. The identified 65% decrease in growth of longitudinal long bone was attributed, in part, to altered shape and volume of the growth plate chondrocytes. Cell shape of the growth plate chondrocytes of PSACH-like canines was statistically different from age-matched control animals. The dwarf Scottish deerhound had 50% less horizontal and 63% higher vertical diameters of proliferating chondrocyes and 65% less horizontal and 82% less vertical diameter in the hypertrophic zone. Decreased cumulative vertical growth of chondrocytes as a result of altered cellular volume, in effect, could contribute to the limb shortness. Metaphyseal flaring is reflected by uncoupling of endochondral and perichondrial growth, where a change in matrix composition alters restrained lateral expansion of the growth plate. Loss of the dwarf Scottish Deerhound dog pedigree (Dr. Gert J. Breur, Perdue University, West Lafayette, IN, personal communication) precludes thymidine labeling studies, that would measure growth plate chondrocyte proliferation relative to longitudinal growth.
GENETIC ANALYSES
The understanding of the molecular basis of PSACH was dramatically advanced with autosomal dominant gene linkage studies mapping PSACH7,8,24 and the much milder osteochondrodysplasia, multiple epiphyseal dysplasia (MED)52, to chromosome 19p13.1. Mutation of the COMP gene located at chromosome 19p13.1 is linked to PSACH and MED3,9,10,15,16,21,25,26,27,41,42,63,64. While only one chromosomal locus is linked to PSACH, at least two additional loci are identified for MED8,14 of which one is COL9A2 that encodes the (2(IX) chain of type IX collagen50. Sixty-six COMP gene mutations that have been identified in either PSACH or MED are listed inTable I. Mutations predict in-frame deletions and insertions as well as single nucleotide substitutions but do not introduce a premature stop codon. Forty-one (62%) of 66 COMP gene mutations are identified for the codons of aspartic acid (Table II). Of the two possible codons, GAC and GAT, 39 (95%) mutations involve the GAC codon for aspartic acid, suggesting a preference for mutation of the GAC. A mutational hot spot is identified at the five GAC repeat sequence located at nt1405-1419. At this site the 20 identified mutations (30% of 66 total mutations) consist of 18 trinucleotide deletions and 2 insertions. A recently identified family of diseases, triplet repeat expansion diseases, is associated with expansion of trinucleotide sequences during replication of duplex DNA47. Formation of stable hairpin loops resulting from trinucleotide repeats folding over onto themselves promotes expansion of the triplets during DNA replications. Ability of GAC repeats to form stable hairpin loops67 has prompted Délot et al.17 to explain observed GAC insertions of the nt1405-1419 (GAC)5 site identified in PSACH [(GAC)1] and MED [(GAC)2] to have resulted from trinucleotide expansion mutations47. With 18 sporadic GAC trinucleotide deletion mutations seen at this same site (nt1405-1419), the (GAC)5 repeat sequence is potentially a hot spot for replication error.
TABLE I. COMP GENE MUTATIONS.
| Exon | Sequence changea
|
Domain | Phenotype | Frequency | Reference | |
|---|---|---|---|---|---|---|
| Nucleotide | Amino acid | |||||
| 9(14) | 868G→A | 290Asp→Asn | Hybrid | PSACH | 1 | Ikegawa (1998) |
| 9(14) | 895G→A | 299Gly→Arg | CR1 | PSACH | 1 | Ikegawa (1998) |
| 9(14) | 919G→A | 309Gly→Arg | CR1 | PSACH | 2 | Délot (1998) |
| 10(15) | 982T→C | 328Cys→Arg | CR1 | PSACH | 1 | Briggs (1995) |
| 10(15) | 1024G→T | 342Asp→Tyr | CR2 | MED (Fairbank) | 1 | Briggs (1995) |
| 10(15) | 1046A→G | 349Asp→Gly | CR2 | PSACH | 1 | Ikegawa (1998) |
| 10(15) | 1081G→T | 361Asp→Tyr | CR3 | MED (typical) | 1 | Loughlin (1998) |
| 10(15) | 1082A→T | 361Asp→Val | CR3 | MED (Fairbank) | 1 | Ikegawa (1998) |
| 10(15) | 1109delCGGGGC | 367delArgGly | CR3 | MED (typical) | 1 | Loughlin (1998) |
| 10(15) | 1111T→C | 371Cys→Ser | CR3 | MED (Fairbank) | 1 | Susic (1997) |
| 10(15) | 1111delGAC | 372delAsp | CR3 | PSACH | 1 | Briggs (1995) |
| PSACH | 1 | Briggs (1998) | ||||
| 11(16) | 1159T→G | 387Cys→Gly | CR3 | PSACH | 1 | Ikegawa (1998) |
| 11(16) | 1109delACCC- AACTCAGA |
389delArgValProAsn |
CR3 | PSACH | 1 | Loughlin (1998) |
| 1109insTGT | 389insCys | |||||
| 11(16) | 1222G→T | 408Asp→Tyr | CR4 | MED (typical) | 1 | Loughlin (1998) |
| 12(17A) | 1280G→A | 427Gly→Glu | CR5 | PSACH | 1 | Deere (1998) |
| PSACH | 1 | Délot (1998) | ||||
| 13(17B) | 1318G→A | 440Gly→Arg | CR5 | PSACH | 1 | Loughlin (1998) |
| PSACH | 1 | Briggs (1998) | ||||
| 13(17B) | 1320G→A | 440Gly→Glu | CR5 | PSACH | 2 | Briggs (1998) |
| 13(17B) | 1336G→A | 446Asp→Gln | CR5 | PSACH | 1 | Madox (1997) |
| CR5 | PSACH | 1 | Délot (1998) | |||
| 13(17B) | 1345C→A | 449Pro→Thr | CR5 | PSACH | 1 | Deere (1998) |
| 13(17B) | 1358G→A | 453Asn→Ser | CR6 | MED (Fairbank) | 1 | Briggs (1998) |
| 13(17B) | 1367delAGG | 457delGlu | CR6 | PSACH | 1 | Ferguson (1997) |
| 13(17B) | 1375delTCA | 459delSer | CR6 | PSACH | 1 | Hecht (1995) |
| 13(17B) | 1403G→A | 468Cys→Tyr | CR6 | PSACH | 1 | Hecht (1995) |
| 13(17B) | 1405delGAC | 469delAsp | CR6 | PSACH | 5 | Hecht (1995) |
| PSACH | 1 | Hecht (1998) | ||||
| PSACH | 2 | Deere (1998) | ||||
| PSACH | 7 | Briggs (1998) | ||||
| PSACH | 3 | Ikegawa (1998) | ||||
| 13(17B) | 1405insGAC | 469insAsp | CR6 | MED (unclassified) | 1 | Délot (1998) |
| 13(17B) | 1405insGACGAC | 469insAspAsp | CR6 | PSACH | 1 | Délot (1998) |
| 13(17B) | 1414G→T | 472Asp→Tyr | CR6 | PSACH | 1 | Hecht (1995) |
| 13(17B) | 1417G→A | 473Asp→Asn | CR6 | PSACH | 1 | Deere (1998) |
| 13(17B) | 1418A→G | 473Asp→Gly | CR6 | PSACH | 1 | Ikegawa (1998) |
| 13(17B) | 1423G→A | 475Asp→Asn | CR6 | PSACH | 1 | Deere (1998) |
| 13(17B) | 1445A→G | 482Asp→Gly | CR6 | PSACH | 1 | Susic (1998) |
| 14(18A) | 1520A→G | 507Asp→Gly | PSACH | 1 | Deere (1998) | |
| 14(18A) | 1526A→C | 509Asp→Ala | CR7 | PSACH | 1 | Deere (1998) |
| 14(18A) | 1526A→G | 509Asp→Gly | CR7 | PSACH | 1 | Deere (1998) |
| 14(18A) | 1531G→C | 511Asp→His | CR7 | PSACH | 1 | Deere (1998) |
| 14(18A) | 1537delGTGGT- AGACAAG |
513delValValAspLys | CR7 | PSACH | 1 | Susic (1997) |
| 14(18A) | 1552G→A | 518Asp→Asn | CR7 | PSACH | 1 | Deere (1998) |
| CR7 | PSACH | 1 | Ikegawa (1998) | |||
| 14(18A) | 1569C→G | 523Asn→Lys | CR7 | MED (Ribbing) | 1 | Ballo (1997) |
| 14(18A) | 1579A→G | 527Thr→Ala | COOH | PSACH | 1 | Hecht (1998) |
| 16(19) | 1754C→T | 585Thr-Met | COOH | PSACH | 1 | Briggs (1998) |
| 16(19) | 1754C→G | 585Thr-Arg | COOH | MED | 1 | Briggs (1998) |
| 16(19) | 1760A→G | 587His-Arg | COOH | PSACH | 1 | Deere (1998) |
nucleotides and amino acids are numbered from the start site of translation; thrombospondin1 corresponding exons are indicated in parentheses; PSACH, pseudoachondroplastic dysplasia: MED; multiple epiphyseal dysplasia; del, deletion; ins, insertion; →, substitution; Hybrid, Type-3 repeat hybrid; CR, calmodulin-like repeat; COOH, globular carboxyl domain; amino acids presented in three letter code; nucleotides presented in one letter code.
TABLE II. LOCATION OF ASPARTIC ACID MUTATIONS IN COMP.
| Domain | Number of Mutations | Aspartic Acid | Codon GAC |
|---|---|---|---|
| Total | 66 | 41(62%)a | 39 (95%)b |
| Type-3 repeats | |||
| -Hybrid | 1 | 1 | 1 |
| -Calmodulin-like | |||
| CR 1 | 4 | 0 | |
| CR 2 | 2 | 2 | 2 |
| CR 3 | 7 | 4 | 4 |
| CR 4 | 1 | 1 | 1 |
| CR 5 | 9 | 2 | 2 |
| CR 6 | 29 | 25 | 25 |
| CR 7 | 9 | 6 | 4 |
| COOH | 4 | 0 |
percentage of total mutations;
GAC percentage of total possible (GAC, GAT) codons for aspartic acid;
GAC, codon for Asp; COOH, globular carboxyl domain. See Figure 1 identifying location of aspartic acid mutations in the Type-3 repeats.
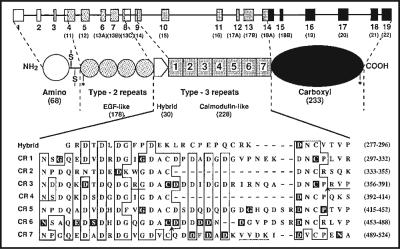
MOLECULAR STRUCTURE OF COMP
The human COMP gene consists of 19 exons9 with a coding sequence that predicts a 757 amino acid core protein51. Amino acid sequence homology with thrombospondins puts COMP in the thrombospondin family. In Table III structural and functional similarities identify COMP with the four member human thrombospodin family. Gene map, model of COMP, and amino acid mutation sites in the predicted calcium-binding Type-3 repeats are identified in Figure 2. From cDNA sequencing, the predicted 757 amino acid minus the predicted 20 amino acid leader sequence (i.e., 737 amino acids) mass of human COMP is 83,547 Da, prior to post-translational modifications51. The human COMP deduced amino acid sequence predicts: 1) 20 amino acid signal peptide (residues 1-20); 2) 68 amino acid globular amino domain (residues 21-88); 3) 178 amino acid Type-2 repeats with 4 epidermal growth factor (EGF)-like motifs (residues 89-266); 4) 258 amino acid Type-3 repeats that consist of a 30 amino acid sequence hybrid calmodulin-like (residues 267-296) followed by a 228 amino acid sequence of 7 calmodulin-like motifs (residues 297-524); and 5) 233 amino acid globular carboxyl domain (residues 525-757)37,51,53. As a glycoprotein, no O-linked oligosaccharides are attached to COMP68. Three NXT/S N-linked oligosaccharide recognition sites are identified from the deduced human COMP sequence (GenBank accession number L32137) with N121 and N741 being glycosylated and the third N-linkage site (N144) being unoccupied68. In the adult, carbohydrate compositional and estimated mass of theN-oligosaccharide at N121 is consistent with expected mass of a high mannose oligosacharride with the structure of (HexNAc)2-(Man)8-(Fuc)1. From fetal tissue, however, four composition carbohydrate ratios are linked to N121, suggesting presence of different carbohydrate moities at this site. The oligosaccharide structure attached to N741, being the same for both fetal and adult, with a calculated mass of 1723.8 +/- 225 Da, could not accurately be determined resulting from the large error value associated with its analyses68.
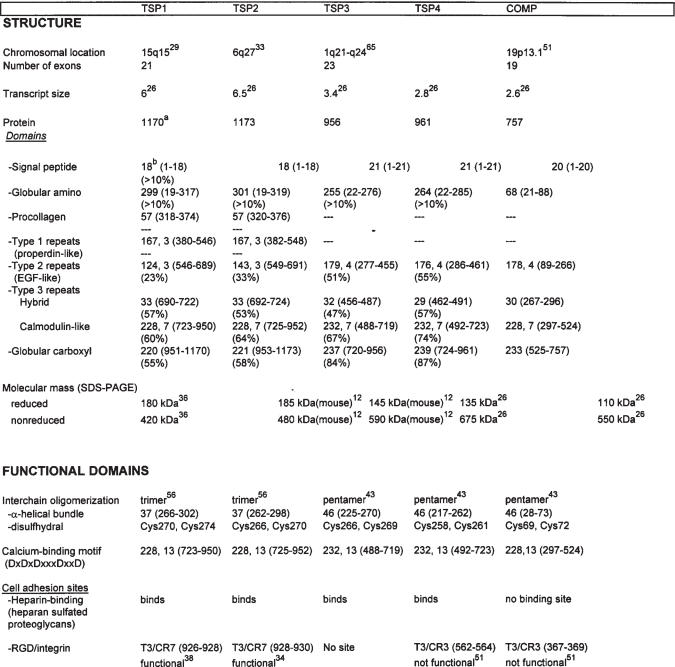
TABLE III. HUMAN THROMBOSPONDIN FAMILY.
number of amino acids from GenBank Accession numbers: TSP1, X14787; TSP2, L12350; TSP3, L38969; TSP4, Z19585; COMP, L32137;
quantity of amino acids within domain, amino acid location identified in parentheses (number from start site translation). Transcript size expressed in kilobase pairs. RGD, arginine-glycine-aspartic acid tripeptide - cell surface recognition sequence. T3, Type 3 repeats; CR7, calmodulin-like 7 repeat. Repeats: number of repeats or calcium binding sites are indicated following identification of amino acid number within the domain.
Figure 2.
Diagrammatic representation of the COMP gene, protein domains, and mutation sites within the Type-3 repeats. The COMP gene consists of 19 exons, to which corresponding protein domains are indicated [ (1) circle, globular Amino; (2) stippled circles, Type-2 repeats, EGF-like; (3) Type-3 repeats: (i) pentamer box, Hybrid; (ii) square boxes, Calmodulin-like; (4) oval, globular Carboxyl]. Corresponding thrombospondin1 exons are indicated in parentheses. Asterisks identify N-linked high oligosaccharides at N121 and N741. Two cysteines (C69, C72) identified in the Amino domain are involved in interchain pentamer oligomerization. CR, calmodulin-like repeats; Amino acids are shown in one letter code and numbered (parentheses) from the start site in translation. Amino acids homology: boxed area, identical sequence; underlined, deletion; dark background, substitution; ↑, insertion. Sequence alignment (277-524), with gaps (- - -) to optimize sequence homologies.
Sequence homology with the family of four thrombospondins has placed COMP as the fifth member (TSP5) of the family. All with unique chromosomal locations, the COMP gene produces the smallest (2.6 kb) transcript26 with an open reading frame of 2274 nt. The globular Amino domain of COMP has the least sequence homology with thrombospondins, with 200 amino acids fewer than thrombospondins. COMP's inability to bind to heparin18 is attributed to the lack of these amino acids. However, in COMP as in thrombospondins, an identical disulfhydral site is involved in interchain interactions that result in formation of multimeric structures. As with TSP3 and TSP4, COMP is a pentamer resulting from interchain disulfyhdral cross-linking and formation of a 5 α-helical bundle from a 46 amino acid sequence within the globular Amino domain of COMP19,43,49. PSACH growth plate chondrocytes express COMP retained in the rough endoplasmic reticulum as a pentamer16,26,42 suggesting PSACH-linked COMP mutations do not alter interchain formation. In the Type-2 repeats four EGF-like sequences (44-55 amino acid units), based on positions of the six cysteine residues4, are identified in COMP with 51% and 55% identical sequence homology with human TSP3 and TSP4, respectively. Proteins containing EGF-like motifs have been documented in forming ligand-receptor interactions at cell surfaces, initiating signal transduction cascades that alter metabolic parameters of the cell such as growth regulation. Functional significance of the EGF-like repeats in COMP remains to be identified.
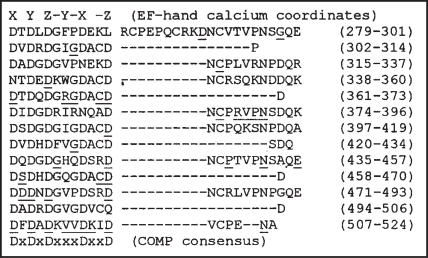
Of the 66 mutations, 62 (94%) are located in the 228 amino acid continuous sequence that make up the Type-3 repeats to which calcium binding sites have been ascribed. Utilizing amino acid sequence homologies of COMP with thrombospondins, a seven repeat consensus sequence of 23-38 amino acids is identified with the alignment of two cysteines and eleven aspartic acids. An eighth hybrid sequence with one cysteine and four aspartic acids is additionally identified within the domain.Figure 2 combines alignment of the 8 homologous peptide sequence motifs and identifies of COMP and MED associated mutations within these sequences. Further amino acid alignments in the Type-3 repeats with a consensus sequence of DxDxDxxxDxxD (D, aspartic acid; x, any amino acid) identifies 13 sequences, also seen in TSP148, with similar EF-hand calcium coordinates that have been established in calmodulin-like proteins32. Proteins with EF-hands bind calcium within a helix-loop-helix structure having 6 amino acids whose vertices approximate an octahedron with the positions designated X,Y,Z,-X,-Y,-Z. Oxygen containing side chains of the amino acids at these coordinates, such as that seen in COMP with aspartic acid are involved in calcium coordination. Figure 3 identifies EF-hand consensus sequences in the Type-3 repeats of COMP. Removal of calcium from TSP1 results in (1) accessibility to otherwise unavailable proteolytic cleavage sites within the Type-3 repeats35 and (2) decrease in size of the Type-3 repeats containing globular structures36,55, establishing calcium's ability to effect structural conformation of TSP1 potentially through the EF-hand calcium binding coordinates. Mutations within the EF-hand consensus sequences [53 (85%) of Type-3 repeats domain 62] potentially could alter normal conformational structure of COMP by changing the ability of calcium to interact with COMP, which as a result could cause formation of the lamallar structures in the rough endoplasmic reticulum growth plate chondrocytes25. Other mutations located within the Type-3 repeats, not in the EF-hand calcium coordinates, potentially change the structure of COMP, indirectly altering ability of the calcium-binding pocket to interact with calcium. For example, in the COMP mutation of Ser371 is substitution for Cys371 it is expected that loss of the disulfhydral linkage occurs that would cause alteration in the tertiary structure of COMP, indirectly, changing a calcium binding site. Mutation in the COMP gene predicts 97% of COMP molecules, as a pentamer, would have at least one monomeric unit containing a mutation.
Figure 3.
Calcium-binding sequence homologies in the Type-3 repeats of human COMP. Thirteen amino acid sequences are numbered (parentheses) from the start site in translation. Sequence alignment (residues 279-524), with gaps (- - -) to optimize sequence homologies. Amino acid, one letter code; underline, mutation site.
FUNCTION OF COMP MOLECULE
COMP is normally localized in the extracellular matrix of connective tissues with an unknown function. Thrombospondins, glycoprotein homologs of COMP, as extracellular matrix molecules, are identified with growth, cellular/tissue differentiation, cell motility, and cell adhesions through either cell surface interactions or interactions with extracellular matrix molecules. Cell surface heparin-binding and Arg-Gly-Asp (RGD) sites have been mapped to sequences within the thrombospondins. COMP, however, does not have the heparin-binding site sequence (minus 200 amino acid within the globular Amino domain), nor does it have a functional RGD site51, therefore, this eliminates these sequences as potential functional sites within COMP.
Difference in COMP extracellular matrix location and carbohydrate composition identified between fetal and adult suggests altered function of COMP in cartilage. Prior to longitudinal bone growth, COMP, synthesized by the chondrocytes, is found localized in the interterritoral compartment of the extracellular matrix20,58. During longitudinal bone growth COMP becomes localized to the pericellular and territorial compartments of the extracellular matrix18,58 with the highest level of mRNA detected in chondrocytes in the proliferative zone58. COMP, within the growth plate, may be involved in regulating cell growth and proliferation58. Differences in N-linked glycosylation structure patterns of COMP isolated from fetal and adult cartilage68 may contribute to differences in molecular interactions within the matrix.
COMP is selectively expressed in cells of cartilage, tendon, ligament, and synovium. In the growth plate of PSACH individuals, COMP is localized to the electron-lucent lamellae of the rough endoplasmic reticulum, but the rough endoplasmic reticulums of tendon and ligament tissues are unaltered45. Radiolabel metabolic studies demonstrate COMP is retained as a pentamer intracellularly and not processed for secretion in chondrocytes isolated from PSACH individuals. COMP secretion from cultured cells isolated from tendon, ligament16,26,42, and chondrocytes differentiated to a fibroblastic phenotype26 demonstrate that COMP retention in PSACH individuals is specific to chondrocytes. Normal development of a COMP gene knockout mouse (personal communication Dr. JT Hecht, Department of Pediatrics, University of Texas-Houston Medical Center, Houston, TX) demonstrates that it is the mutation, not the absence of COMP, that affects cartilage extracellular matrix deposition. Eliminating expression of COMP is not sufficient to alter cartilage extracellular matrix, a mutant COMP molecule must be expressed.
FUTURE DIRECTION OF RESEARCH ON PSACH
The mechanism(s) linking COMP gene mutations with the PSACH phenotype has yet to be elucidated. Several questions are proposed in order to characterize mutant COMP's role in generation of a PSACH phenotype. With the presence of a COMP gene mutation it is predicted that 97% of expressed pentameric COMP will contain at least one monomeric unit. The actual amount of mutated monomeric units within the pentameric species is not known. It would be anticipated that with an increase in percentage of mutated monomeric units that a greater altered structure of the pentameric species would occur, that could influence severity of the phenotype. Identifying a correlation between quantity of mutant COMP monomeric units and a PSACH phenotype would be beneficial in attempts to correct the anomaly through a gene therapy approach.
A PSACH phenotype is not clinically identified at birth, even though COMP is being synthesized. Potentially a required amount of mutated monomeric units are needed for the PSACH phenotype to be evident. Alternatively, during growth, mutant COMP alters COMP normal interaction with molecules that are expressed during growth that are not present during development. Potentially, this altered molecular interaction leads to generation of PSACH phenotype.
Altered function of tissues normally expressing COMP is observed in PSACH, suggesting expression of the mutant COMP is occurring universally. However, tendon and ligament cells do not present with extended rough endoplasmic reticulum as seen in growth plate chondrocytes, suggesting difference in molecular interactions of mutant COMP in these tissues. Hecht et al.26, identified co-precipitation of COMP and TSP4 with antibodies either specific for COMP or TSP4 from PSACH tendon cells, but not with chondrocytes, suggesting difference in interactions with COMP. One explanation for observed molecular co-precipitation is that COMP and TSP4 are found as heteropentamers, similarly seen with TSP1 and TSP254. As well as differences in synthesis observed between tendon and ligaments compared to chondrocytes, molecular interactions of mutant COMP with TSP4 could attribute to a difference in cellular phenotype.
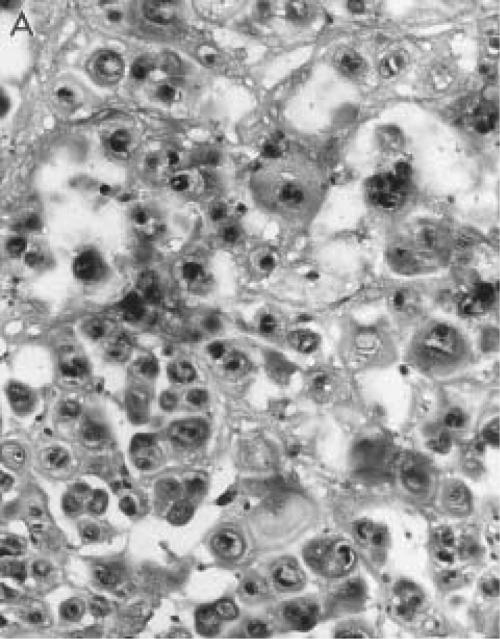
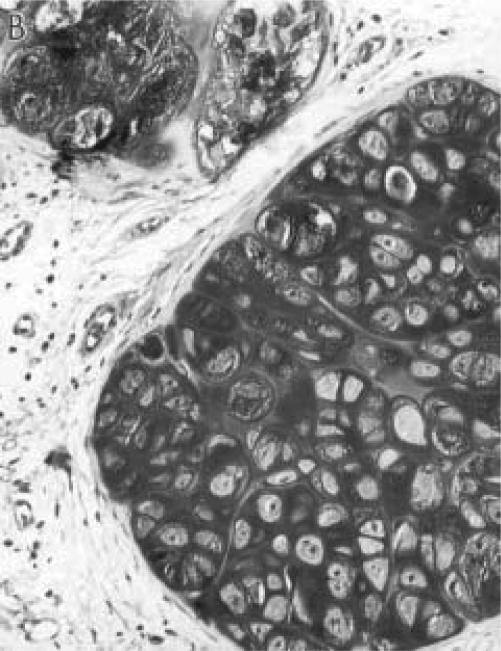
A cell culture system has been developed at the University of Iowa, whereby a PSACH-linked mutant COMP transgene is expressed in a cell line having a chondrocyte phenotype13,30,62. Coupling an amino acid codon sequence to COMP cDNA, for immunological monitoring of the expressed human COMP transgenes, retention of expressed transgene was observed in the rough endoplasmic reticulum (Figure 4). Proteoglycan metabolism was altered in the cell culture system when mutant COMP was expressed by the chondrocyte-like cells (Figure 5). Establishing a PSACH-like cell culture system, with unlimited amounts of cells, permits us to perform manipulative experiments, which are impossible using human tissue or isolated cells. Concurrent studies have been initiated at the University of Iowa in developing mouse transgenics, expressing the same human mutant COMP transgene developed in our cell culture system. Development of a PSACH animal model will permit studies to be performed that are not ethically feasible in humans and impossible in the cell culture system.
Figure 4.
Immunohistochemical identification of human PSACH-linked mutant COMP tagged with a selective immunoreactive sequence distinct from rat COMP in Swarm rat chondrosarcoma cells cultured for 4 days. Brown staining identifies retention of expressed mutant COMP within the cells. Magnification = 1,500x.
Figures 5A-B (next column).
Histochemical staining of sulfated proteoglycans with safranin O of the Swarm rat chondrosarcoma tumor expressing a human PSACH-linked mutant COMP (panel A), grown subcutaneously in rat for 59 days. Less proteoglycans are incorporated into the extracellular matrix of the chondrosarcoma containing the mutant COMP transgene, suggesting expression of the mutant COMP is altering deposition of aggrecan in the extracellular matrix as similarly seen in PSACH. Control tumor is presented in panel B. Magnification = 95x.
Figure 5A.
Figure 5B.
ACKNOWLEDGMENT
I thank Dr. JA Maynard for supplying the transmission electron micrograph of a PSACH growth plate chondrocyte from a patient in 1971. The PSACH-like cell culture system and a mutant COMP transgenic mouse system are from unpublished data collected in the course of studies performed in collaboration with Drs. JT Hecht (University of Texas Medical Center, Houston, TX), BM Vertel (The Chicago Medical School, North Chicago, IL), TT Glant (Rush-Presb-St Luke's Med Ctr, Chicago IL), JA Martin, JA Maynard, BP Bosch, TB Rapp, HW Kim and with the technical support of GL Kurriger, AS Carter, AC Schroeder. Thanks to LA Lembke for her editorial help with this manuscript. Financial assistance was provided by the Human Growth Foundation, Children's Miracle Network and Central Investment Fund Research Enhancement award from the University of Iowa.
Footnotes
Dedicated to Dr. Reginald R. Cooper for his years as the Head of the Department of Orthopaedic Surgery in the University of Iowa and his insight with Drs. Jerry A. Maynard and Ignacio V. Ponseti as the first in recognizing pseudoachondroplastic dysplasia as a rough endoplasmic reticulum processing disorder.
References
- 1.Adolph KW, Long GL, Winfield S, Ginns EI, Bornstein P. Structure and organization of the human thrombospondin 3 gene (THBS3) Genomics. 1995;27:329–336. doi: 10.1006/geno.1995.1050. [DOI] [PubMed] [Google Scholar]
- 2.Baker E, Guo X-H, Orsborn AM, Sutherland GR, Callen DF, Hopewood JJ, Morris CP. The Morquio A syndrome (mucopolysaccharidosis IVA) gene maps to 16q24.3. Am J Hum Gene. 1993;52:96–98. [PMC free article] [PubMed] [Google Scholar]
- 3.Ballo R, Briggs MD, Cohn DH, Knowlton RG, Beighton PH, Ramesar RS. Multiple epiphyseal dysplasia, Ribbing type: A novel point mutation in the COMP gene in a South African family. Amer J Med Genet. 1997;68:396–400. [PubMed] [Google Scholar]
- 4.Bender W. Homeotic gene products as growth factors. Cell. 1985;43:559–560. doi: 10.1016/0092-8674(85)90224-7. [DOI] [PubMed] [Google Scholar]
- 5.Breur GJ, Zebre CA, Slocombe RF, Padgett GA, Braden TD. Clinical, radiographic, pathologic, and genetic features of osteochondrodysplasia in Scottish deerhounds. J Am Veter Med Assn. 1989;195:606–612. [PubMed] [Google Scholar]
- 6.Breur GJ, Farnum CE, Padgett GA, Wilsman NJ. Cellular basis of decreased rate of longitudinal growth of bone in pseudoachondroplastic dogs. J Bone and Joint Surg. 1992;74-A:516–528. [PubMed] [Google Scholar]
- 7.Briggs MD, Rasmussen IM, Weber JL, Yuen J, Reinker K, Garber AP, Rimoin DL, Cohn DH. Genetic linkage of mild pseudoachondroplasia (PSACH) to markers in the pericentromeric region of chromosome 19. Genomics. 1993;18:656–660. doi: 10.1016/s0888-7543(05)80369-6. [DOI] [PubMed] [Google Scholar]
- 8.Briggs MD, Choi H, Warman ML, Loughlin JA, Wordsworth P, Sykes BC, Irven CM, Smith M, Wynne-Davies R, Lipson MH, Biesecher LC, Garber AP, Lachman R, Olsen BR, Rimoin DL, Cohn DH. Genetic mapping of a locus for multiple epiphyseal dysplasia (EDM2) to a region of chromosome 1 containing a type IX collagen gene. Am J Hum Genet. 1994;55:678–684. [PMC free article] [PubMed] [Google Scholar]
- 9.Briggs MD, Hoffman SMG, King LM, Olsen AS, Mohrenweiser H, Leroy JG, Mortier GR, Rimoin DL, Lachman RS, Gaines ES, Cekleniak JA, Knowlton RG, Cohn DH. Pseudoachondroplasia and multiple epiphyseal dysplasia due to mutations in the cartilage oligomeric matrix protein gene. Nature Genet. 1995;10:330–336. doi: 10.1038/ng0795-330. [DOI] [PubMed] [Google Scholar]
- 10.Briggs MD, Mortier GR, Cole WG, King LM, Golik SS, Bonaventure J, Nuytinck L, De Paepe A, Leroy JG, Biesecker L, Lipson M, Wilcox WR, Lachman RS, Rimoin DL, Knowlton RG, Cohn DH. Diverse mutations in the gene for cartilage oligomeric matrix protein in the pseudoachondroplasia-multiple epiphyseal dysplasia disease spectrum. Am J Hum Genet. 1998;62:311–319. doi: 10.1086/301713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper RR, Ponseti IV, Maynard JA. Pseudoachondroplastic dwarfism. A rough-surfaced endoplasmic reticulum storage disorder. J Bone and Joint Surg. 1973;55-A:475–484. [PubMed] [Google Scholar]
- 12.Chen H, Aeschlimann D, Nowlen J, Mosher DF. Expression and initial characterization of recombinant mouse thrombospondin 1 and thrombospondin 3. FEBS Lett. 1996;387:36–41. doi: 10.1016/0014-5793(96)00460-7. [DOI] [PubMed] [Google Scholar]
- 13.Chen LL, Stevens JW, Martin JA, Hecht JT, Ver tel BM. A cell model for pseudoachondroplasia and COMP. Mol Biol Cell. 1998.
- 14.Deere M, Blantin SH, Scott CI, Langer LO, Pauli RM, Hecht JT. Genetic heterogeneity in multiple epiphyseal dysplasia. Am J Hum Genet. 1995;56:698–704. [PMC free article] [PubMed] [Google Scholar]
- 15.Deere M, Sanford T, Ferguson HL, Daniels K, Hecht JT. Identification of twelve mutations in cartilage oligomeric matrix protein (COMP) in patients with pseudoachondroplasia. Am J Med Genet. 1998;80:510–513. doi: 10.1002/(sici)1096-8628(19981228)80:5<510::aid-ajmg14>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 16.Délot E, Brodie SG, King LM, Wilcox WR, Cohn DH. Physiological and pathological secretion of cartilage oligomeric matrix protein by cells in culture. J Biol Chem. 1998;273:26692–26697. doi: 10.1074/jbc.273.41.26692. [DOI] [PubMed] [Google Scholar]
- 17.Délot E, King LM, Briggs MD, Wilcox WR, Cohn DH. Trinucleotide expansion mutations in the cartilage oligomeric matrix protein (COMP) gene. Hum Mol Genet. 1999;8:123–128. doi: 10.1093/hmg/8.1.123. [DOI] [PubMed] [Google Scholar]
- 18.Di Cesare PE, Möglin M, Carlson CS, Pasumarti S, Paulsson M. Cartilage oligomeric matrix protein: Isolation and characterization from human articular cartilage. J Orthop Res. 1995;13:422–428. doi: 10.1002/jor.1100130316. [DOI] [PubMed] [Google Scholar]
- 19.Efimov VP, Lustig A, Engel J. The thrombospondin-like chains of cartilage oligomeric matrix protein are assembled by a five-strand (-helical bundle between residues 20 and 83. FEBS Letters. 1994;341:54–58. doi: 10.1016/0014-5793(94)80239-4. [DOI] [PubMed] [Google Scholar]
- 20.Ekman S, Reinholt FP, Hultenby K, Heinegård D. Ultrastructural immunolocalization of cartilage oligomeric matrix protein (COMP) in porcine growth cartilage. Calci Tissue Int. 1997;60:547–553. doi: 10.1007/s002239900278. [DOI] [PubMed] [Google Scholar]
- 21.Ferguson HL, Deere M, Evans R, Rotta J, Hal JG, Hecht JT. Mosaicism in pseudoachondroplasia. Am J Med Genet. 1997;70:287–291. [PubMed] [Google Scholar]
- 22.Hall JG, Dorst JP. Pseudoachondroplastic SED, recessive Maroteaux-Lamy type. Birth Defects Orig Art Ser. 1969;V(4):254–259. [Google Scholar]
- 23.Hall JG, Dorst JP, Rotta J, McKusick VA. Gonadal mosaicism in pseudoachondroplasia. Am J Med Genet. 1987;28:143–151. doi: 10.1002/ajmg.1320280121. [DOI] [PubMed] [Google Scholar]
- 24.Hecht JT, Francomano CA, Briggs MD, Deere M, Conner B, Horton WA, Warman M, Cohn DH, Blanton SH. Linkage of typical pseudoachondroplasia to chromosome 19. Genomics. 1993;18:661–666. doi: 10.1016/s0888-7543(05)80370-2. [DOI] [PubMed] [Google Scholar]
- 25.Hech JT, Nelson LD, Crowder E, Wang Y, Elder FFB, Harrison WR, Francomano CA, Prange CK, Lennon GG, Deere M, Lawler J. Mutations in exon 17B of cartilage oligomeric matrix protein (COMP) cause pseudoachondroplasia. Nature Genet. 1995;10:325–329. doi: 10.1038/ng0795-325. [DOI] [PubMed] [Google Scholar]
- 26.Hecht JT, Deere M, Putnam E, Cole W, Vertel B, Chen H, Lawler J. Characterization of cartilage oligomeric matrix protein (COMP) in human normal and pseudoachondroplasia musculoskeletal tissues. Matrix Biol. 1998;17:269–278. doi: 10.1016/s0945-053x(98)90080-4. [DOI] [PubMed] [Google Scholar]
- 27.Ikegawa S, Ohashi H, Nishmura G, Kim KC, Sannohe A, Kimizuka M, Fukushima Y, Nagai T, Nakamura Y. Novel and recurrent COMP (cartilage oligomeric matrix protein) mutations in pseudoachondroplasia and multiple epiphyseal dysplasia. Hum Genet. 1998;103:633–638. doi: 10.1007/s004390050883. [DOI] [PubMed] [Google Scholar]
- 28.Incardona F, Lawler J, Cataldo D, Panet A, Legrand Y, Foidart JM, Legrand C. Heparin-binding domain, type 1 and type 2 repeats of thrombospondin mediate its interaction with human breast cancer cells. J Cell Biochem. 1996;15:431–442. doi: 10.1002/(sici)1097-4644(19960915)62:4<431::aid-jcb1>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 29.Jaffe E, Bornstein P, Disteche CM. Mapping the thrombospondin gene to human chromosome 15 and mouse chromosome 2 by in situ hybridization. Genomics. 1990;7:123–126. doi: 10.1016/0888-7543(90)90528-3. [DOI] [PubMed] [Google Scholar]
- 30.Kim HW, Martin JA, Schroeder AC, Kurriger GL, Maynard JA, Stevens JW. PSACH-linked COMP mutation alters chondrosarcoma ECM formation. Trans Orthop Res Soc. 1999;24:430. [Google Scholar]
- 31.Knowlton RG, Cekleniak JA, Cohn DH, Briggs MD, Hoffman SM, Brandriff BF, Olsen AS. High-resolution genetic and physical mapping of multiple epiphyseal dysplasia and pseudoachondroplasia mutations at chromosome 19p13.1-p12. Genomics. 1995;28:513–519. doi: 10.1006/geno.1995.1183. [DOI] [PubMed] [Google Scholar]
- 32.Kretsinger RH. Crystallographic studies of calmodulin and homologs. Ann NY Acad Sci. 1980;356:1–19. doi: 10.1111/j.1749-6632.1980.tb29594.x. [DOI] [PubMed] [Google Scholar]
- 33.LaBell TL, McGookey-Milewicz DJ, Disteche CM, Byers PH. Thrombospondin II: Partial cDNA sequence, chromosome location, and expression of a second member of the thrombospodin gene family in humans. Genomics. 1992;12:421–429. doi: 10.1016/0888-7543(92)90430-z. [DOI] [PubMed] [Google Scholar]
- 34.Laherty CD, O'Rourke K, Wolf FW. Thrombospondin 1 and thrombospondin 2 are expressed as both homo- and heterotrimers. J Biol Chem. 1992;267:24921–24924. [PubMed] [Google Scholar]
- 35.Lawler J, Simons ER. Cooperative binding of calcium to thrombospondin. The effect of calcium on the circular dichroism and limited tryptic digestion of thrombospondin. J Biol Chem. 1983;258:12098–12101. [PubMed] [Google Scholar]
- 36.Lawler J, Derick LH, Connolly JE, Chen JH, Chao FC. The structure of human platelet thrombospondin. J Biol Chem. 1985;260:3762–3772. [PubMed] [Google Scholar]
- 37.Lawler J, Hynes RO. The structure of human thrombospondin, an adhesion glycoprotein with multiple calcium-binding sites and homologies with several proteins. J Cell Biol. 1986;103:1635–1648. doi: 10.1083/jcb.103.5.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lawler J, Weinstein R, Hynes RO. Cell attachment to thrombospondin: the role of ARG-GLY-ASP, calcium, and integrin receptors. J Cell Biol. 1988;107:2351–2361. doi: 10.1083/jcb.107.6.2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lawler J, McHenry K, Duquette M, Derick L. Characterization of human thrombospondin- 4. J Biol Chem. 1995;270:2809–2814. doi: 10.1074/jbc.270.6.2809. [DOI] [PubMed] [Google Scholar]
- 40.Lindseth RE, Danigelis JA, Murray DG, Wray JB. Spondylo-epiphyseal dysplasia (Pseudoachondroplastic type) Amer J Dis Child. 1967;13:721–726. doi: 10.1001/archpedi.1967.02090210135017. [DOI] [PubMed] [Google Scholar]
- 41.Loughlin J, Irven C, Mustafa Z, Briggs MD, Carr A, Lynch A-A, Knowlton RG, Cohn DH, Sykes B. Identification of five novel mutations in cartilage oligomeric matrix protein gene in pseudoachondroplasia and multiple epiphyseal dysplasia. Human Mutat Suppl. 1998;1:S10–S17. doi: 10.1002/humu.1380110105. [DOI] [PubMed] [Google Scholar]
- 42.Maddox BK, Keene DR, Sakai LY, Charbonneau NL, Morris NP, Ridgway CC, Boswell BA, Sussman MD, Horton WA, Bachinger HP, Hecht JT. The fate of cartilage oligomeric matrix protein is determined by the cell type in the case of a novel mutation in pseudoachondroplasia. J Biol Chem. 1997;272:30993–30997. doi: 10.1074/jbc.272.49.30993. [DOI] [PubMed] [Google Scholar]
- 43.Malashkevich VN, Kammerer RA, Efmov VP, Schulthess T, Engel J. The crystal structure of a five-stranded coiled coil in COMP: A proteotype in channel. Science. 1996;274:761–765. doi: 10.1126/science.274.5288.761. [DOI] [PubMed] [Google Scholar]
- 44.Maroteaux P, Lamy M. Les formes pseudoachondroplastiques des dysplasies spondyloepiphysaires. Presse Med. 1959;67:383–386. [PubMed] [Google Scholar]
- 45.Maynard JA, Cooper RR, Ponseti IV. A unique rough surface endoplasmic reticulum inclusion in pseudoachondroplasia. Lab Invest. 1972;26:40–44. [PubMed] [Google Scholar]
- 46.McKeand J, Rotta J, Hecht JT. Natural history study of pseudoachondroplasia. Am J Med Genet. 1996;63:406–410. doi: 10.1002/(SICI)1096-8628(19960517)63:2<406::AID-AJMG16>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 47.Mitas M. Trinucleotide repeats associated with human diseases. Nucleic Acids Res. 1997;12:2245–2253. doi: 10.1093/nar/25.12.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Misenheimer TM, Mosher DF. Calcium ion binding to thrombospondin 1. J Biol Chem. 1995;270:1729–1733. doi: 10.1074/jbc.270.4.1729. [DOI] [PubMed] [Google Scholar]
- 49.Mörgelin M, Heinegård D, Enge J, Paulsson M. Electron microscopy of native cartilage oligomeric matrix protein purified from the Swarm rat chondrosarcoma reveals a five-arm structure. J Biol Chem. 1992;267:6137–6141. [PubMed] [Google Scholar]
- 50.Muragaki Y, Mariman ECM, van Berrsum SEC, Perala M, van Mourik JBA, Warman ML, Olsen BR, Hamel BCJ. A mutation in the gene encoding the alpha-2 chain of the fibril-associated collagen IX, COL9A2, causes multiple epiphyseal dysplasia (EDM2) Nat Genet. 1996;12:103–105. doi: 10.1038/ng0196-103. [DOI] [PubMed] [Google Scholar]
- 51.Newton G, Weremowicz S, Morton CC, Copeland NG, Gilbert DJ, Jenkins NA, Lawler J. Characterization of human and mouse cartilage oligomeric matrix protein. Genomics. 1994;24:435–439. doi: 10.1006/geno.1994.1649. [DOI] [PubMed] [Google Scholar]
- 52.Oehlmann R, Summerville GP, Yeh G, Weaver EJ, Jimenez SA, Knowlton RG. Genetic linkage mapping of multiple epiphyseal dysplasia to the pericentromeric region of chromosome 19. Am J Hum Genet. 1994;54:3–10. [PMC free article] [PubMed] [Google Scholar]
- 53.Oldberg Å, Antonsson P, Lindbloom K, Heinegård D. COMP (cartilage oligomeric matrix protein) is structurally related to the thrombospondins. J Biol Chem. 1992;267:22346–22350. [PubMed] [Google Scholar]
- 54.O'Rourke KM, Laherty CD, Dixit VM. Thrombospondin 1 and thrombospondin 2 are expressed as both homo- and heterotrimers. J Biol Chem. 1992;267:24921–24924. [PubMed] [Google Scholar]
- 55.Qabar A, Derick L, Lawler J, Dixit V. Thrombospondin 3 is a pentameric molecule held together by interchain disulfide linkage involving two cysteine residues. J Biol Chem. 1995;270:12725–12729. doi: 10.1074/jbc.270.21.12725. [DOI] [PubMed] [Google Scholar]
- 56.Sottile J, Seleue J, Mosher DF. Synthesis of truncated amino-terminal trimers of thrombospondin. Biochemistry. 1991;30:6556–6562. doi: 10.1021/bi00240a028. [DOI] [PubMed] [Google Scholar]
- 57.Shiang R, Thompson LM, Zhu Y-Z, Church DM, Fielder TJ, Bocian M, Winokur ST, Wasmuth JJ. Mutations in the transmebrane domain of FGFR3 cause the most common genetic from of dwarfism, achondroplasia. Cell. 1994;78:335–342. doi: 10.1016/0092-8674(94)90302-6. [DOI] [PubMed] [Google Scholar]
- 58.Shen Z, Heinegård D, Sommarin Y. Distribution and expression of cartilage oligomeric matrix protein and bone sialoprotein show marked changes during rat femoral head development. Matrix Biology. 1995;14:773–781. doi: 10.1016/s0945-053x(05)80020-4. [DOI] [PubMed] [Google Scholar]
- 59.Stanescu V, Maroteaux P, Stanescu R. The biochemical defect of pseudoachondroplasia. Europ J Pediat. 1982;138:221–225. doi: 10.1007/BF00441206. [DOI] [PubMed] [Google Scholar]
- 60.Stanescu V, Stanescu R, Marteaux P. Pathogenic mechanisms in osteochondro-dysplasias. J Bone and Joint Surg. 1984;66-A:817–836. doi: 10.2106/00004623-198466060-00002. [DOI] [PubMed] [Google Scholar]
- 61.Stanescu R, Stanescu V, Muriel M-P, Maroteaux P. Multiple epiphyseal dysplasia, Fairbank type: Morphologic and biochemical study of cartilage. Am J Med Genet. 1993;45:501–507. doi: 10.1002/ajmg.1320450420. [DOI] [PubMed] [Google Scholar]
- 62.Stevens JW, Rapp TB, Martin JA, Maynard JA, Vertel BA, Hecht JT. Stable transfection of chondrocytes with mutant human COMP. Trans Orthop Res Soc. 1998;23:103. [Google Scholar]
- 63.Susic S, McGrory J, Ahier J, Cole WG. Multiple epiphyseal dysplasia and pseudoachondroplasia due to novel mutation in the calmodulin-like repeats of cartilage oligomeric matrix protein. Clin Genet. 1997;51:219–224. doi: 10.1111/j.1399-0004.1997.tb02458.x. [DOI] [PubMed] [Google Scholar]
- 64.Susic S, Ahier J, Cole WG. Pseudoachondroplasia due to the substitution of the highly conserved Asp482 by Gly in the seventh calmodulin-like repeat of cartilage oligomeric matrix protein. Hum Mutat Suppl. 1998;1:S125–S127. doi: 10.1002/humu.1380110142. [DOI] [PubMed] [Google Scholar]
- 65.Vos HL, Devarayalu S, de Vries Y, Bornstein P. Thrombospondin 3 (Thbs3), a new member of the thrombospondin gene family. J Biol Chem. 1992;267:12192–12196. [PubMed] [Google Scholar]
- 66.Wynne-Davies R, Hall CM, Young ID. Pseudoachondroplasia: Clinical diagnosis at different ages and comparison of autosomal dominant and recessive types. A review of 32 patients (26 kindred) J Med Genet. 1986;23:425–434. doi: 10.1136/jmg.23.5.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yu A, Dill J, Mitas M. The purine-rich trinucleotide repeat sequences d(CAG)15 and d(GAC)15 form hairpins. Nucleic Acids Res. 1995;23:4055–4057. doi: 10.1093/nar/23.20.4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zaia J, Boynton RE, McIntosh A, Marshak DR, Olsson H, Heinegård D, Barry FP. Post-translational modifications in cartilage oligomeric matrix protein. Characterization of the N-linked oligosaccharides by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. J Biol Chem. 1997;272:14120–14126. doi: 10.1074/jbc.272.22.14120. [DOI] [PubMed] [Google Scholar]