Abstract
Fifty-seven patients had arthroscopic Mumford procedures for acromioclavicular pain non-responsive to conservative treatment. Thirty-nine of these patients had concomitant rotator cuff repairs. All had significant improvement of their distal clavicular pain. Neither the amount nor the completeness of distal clavicle resection affected the results. Arthroscopic distal clavicle resection is a safe and effective method of alleviating acromioclavicular pain.
INTRODUCTION
Acromioclavicular joint symptomatology is a common finding in shoulder pathology, both as a result of direct injury to the acromioclavicular joint and rotator cuff/impingement phenomenon with acromioclavicular arthrosis. Non-operative treatments including physical therapy, anti-inflammatories, and corticosteroid injections can help resolve the symptoms. Certain cases, however are not amenable to conservative care and require operative intervention. Resection of the distal clavicle, as described by Mumford7, is a reliable method of treatment in post-traumatic degenerative disease of the AC joint, distal clavicle fractures, and shoulder impingement syndrome.
Traditionally, distal clavicle resection has been performed using an open incision over the acromioclavicular joint with detachment of the deltoid and trapezius muscle and their adjacent fascia. Symptom improvement has been satisfactory in most reported series6,7,8,9,10. However, significant morbidity can occur with these open procedures. Some of the complications with distal clavicle resections have included: residual acromioclavicular joint instability, postoperative shoulder weakness, and cosmetic complaints5. Arthroscopic subacromial decompression and resection of the distal clavicle can avoid the problems associated with traditional open procedures. Additionally, arthroscopic surgery allows adequate visualization and identification of glenohumeral joint pathology (labral tears, loose bodies, chondral injuries)11 as well as rotator cuff pathology3.
Several surgical arthroscopic approaches to the acromioclavicular joint have been proposed. One is the superior approach in which the arthroscope and instruments are inserted through the acromioclavicular joint from a superior portal8. The second approach is the subacromial technique, in which the arthroscope and burr are inserted via posterior or lateral subacromial portals7.
A variation of the subacromial technique for arthroscopic resection of the distal clavicle has been used in a number of patients, with a clinical presentation of rotator cuff/impingement pathology. In all cases a diagnostic arthroscopy was performed followed by a bursoscopy and acromioplasty and distal clavicle resection. In a number of patients, mini open procedures for rotator cuff repairs were also performed.
MATERIALS AND METHODS
From 1994-95, fifty-seven arthroscopic procedures were performed. For all patients, the indications for surgery were: impingement phenomena with pain at the acromioclavicular joint, a positive adduction sign, and tenderness of the distal clavicle to palpation9. All patients had been non-responsive to conservative care: oral anti-inflammatories, physical therapy, and injections of corticosteroid into the subacromial spaces. In all cases preoperative and postoperative x-rays were obtained to assess the amount of distal clavicle excised as well as any retained distal clavicular fragments within the superior capsule of the acromioclavicular joint.
OPERATIVE PLANNING AND TECHNIQUE
Surgical Technique
The patients were placed in a lateral decubitus position. Bucks traction was used to secure the forearm for traction. The arm was placed in approximately 30 degrees abduction, and 10-15 degrees of forward flexion. The upper extremity was then prepped with Duraprep and the forearm draped sterilely with Ioband drape. Four ccs of 1:1000 dilution of epinephrine were placed in each 3L bag of arthroscopic fluid. The Dyonics pump was used to distend the shoulder joint and subacromial space.
Glenohumeral Evaluation
The glenohumeral joint was slightly evaluated using standard anterior and posterior portals. The biceps tendon and the underside of the rotator cuff were evaluated. Any fraying or edema of the critical zone was noted. Both anterior and posterior labra were visualized as well as the articular surface of the glenoid and the humerus. Any anterior pathology was surgically addressed at this time.
Subacromial Evaluation
The arthroscope was then removed from the glenohumeral joint and placed in the subacromial bursa through the posterior portal. A third portal was made approximately 2 cc lateral to the lateral border of the acromion. Any shaving and decompressive work was done through the lateral portal. After an adequate bursectomy was done, the rotator cuff was evaluated. The humerus was maximally rotated both internally and externally while probing the rotator cuff at the critical zone. Any penetration through the rotator cuff and critical zone into the glenohumeral joint was considered to be an essential tear of the rotator cuff. If hooking or spurring of the anterior acromion was present or thickening of the bursa was noted on the undersurface of the acromion, an acromioplasty was performed using the Dyonics stone cutting burr. The anterior 7-10 mm of anterior acromion was resected, encompassing the anterior one-half to two-thirds of the acromion. Care was taken to leave a smooth underside and not to violate the anterior deltoid fascia. If the coracoacromial ligament was noted to be thickened, it was then resected using electrocautery.
The arthroscope was then placed in the lateral portal. This allowed an excellent view of the angle of resection of the acromion. This further allowed a second view of the rotator cuff from above, and any additional probing of the cuff was done at this time.
Distal Clavicle Resection
The arthroscope remained in the lateral portal for this aspect of the procedure. Through the posterior portal the underside of the acromioclavicular joint capsule was then excised using the Dyonics and synovial resector. If thickened, the inferior capsule of the acromioclavicular joint was first elevated using the electrocautery. The underside of the distal clavicle was exposed for a distance of approximately two centimeters, taking care to stay lateral to the coracoclavicular ligaments. The Dyonics stone cutter burr was then used to resect the distal clavicle, working from inferiorly to superiorly. Care was taken not to violate the superior capsule of the acromioclavicular joint.
A useful technique was to remove the clavicle from lateral to medial. This prevented floating lateral fragments of clavicle remaining within the superior acromioclavicular capsule7. Digital pressure on the distal clavicle by an assistant allowed a better view of the superior capsule of the AC joint and any retained capsular fragments. If needed, the Dyonics resector was placed in the anterior portal, which allowed better access to the posterior aspect of the AC joint.
Postoperatively, all patients were placed in an abduction pillow for 7-10 days. If a rotator cuff repair was performed, the abduction pillow was used for 4-5 weeks. Immediately postoperatively, passive motion was initiated by a physical therapist and continued on an outpatient basis. At two weeks, hydrotherapy was initiated.
RESULTS
Fifty-seven patients underwent arthroscopic distal clavicle resection arthroscopically performed. All fifty-seven had acromioplasties performed as well. Thirty-nine of these patients also underwent a rotator cuff repair. Improvement or elimination of the distal clavicle pain was reported in all subjects.
Radiographic Results
Of the 57 clavicle resections, 20 had retained clavicle fragments. Six were large fragments. Fourteen had small pieces, most visible only under hot light. All were asymptomatic. Eight patients showed radiographic evidence of a superior spike distal clavicle within the superior capsule of the AC joint (type II). Persistent symptoms of crepitus and pain occurred in one patient. These symptoms improved when the superior spike was subsequently resected.
DISCUSSION
Distal clavicle resections have been shown to be a useful adjunct in treating patients with AC pan and associated impingement who were otherwise not responsive to conservative care6,8,9,10. Cook and Tibone5 have shown the symptomatic and subject improvement of distal clavicle resections in a group of athletes. However, a loss of bench press strength was a complaint of four athletes who did not return to their previous performance level. Diligent attention to reconstruction of the deltoid and trapezius fascia was emphasized. The arthroscopic technique allows the procedure to be performed without the morbidity of detaching and reattaching the deltoids or the trapezius from the distal clavicle and the anterior acromion5,6,9. Postoperative weakness is avoided and a more rapid return to activity is expressed8.
The use of the arthroscope in the distal clavicle resection allows the thorough evaluation of both the glenohumeral joint as well as the subacromial space including partial full thickness rotator cuff tears3 and instability11. Some authors have suggested that less than optimum results can occur when shoulder laxity or other intra-articular causes of distal clavicle pain or impingement are not addressed11. Correction of the underlying instability is imperative to correct the impingement phenomena. Whether this be repair of a labral tear or capsulorrhaphy depends on the presentation. The thoroughness of this evaluation in an experienced arthroscopist and shoulder surgeon should not be underscored.
Several different techniques have been suggested for arthroscopic Mumford procedures. Synder8 recommends that all soft tissue be removed from the inferior AC joint. A pilot hole is then drilled in the center of the clavicle to a depth of 1.5 cm. With external pressure on the clavicle, the pilot hole is then enlarged in a circular fashion until only a shell of the cortical bone of the lateral clavicle remains. The remainder of the shell is then removed with the acromionizer. However, these pieces of clavicle, especially those still attached to the superior capsule, can be difficult to remove.
Flatow and Bigliani et al.8 reported on arthroscopic resections of the lateral clavicle using the superior approach. The area of arthroscopy is small and the 2.7 mm wrist arthroscope is used for this technique. With this technique they do not routinely arthroscopically examine the subacromial bursa nor the glenohumeral joint.
Our technique is a variation of the technique used by Synder7. With the Dyonics stone cutter burr and arthroscopic pump, this procedure can be quickly and safely performed. The distal clavicle does not need to be continually manually depressed, which can be technically difficult. Using the shaver from both the posterior and anterior portals, while visualizing laterally, allows the distal clavicle to be well resected and the superior capsule of the AC joint to be well visualized8.
A surprising finding was that retained clavicular fragments were not associated with residual clavicular pain. The presence of a prominent lateral spike was found to give symptoms in one patient and improved with further resection.
SUMMARY
The arthroscopic Mumford procedure is a safe, reliable method of resecting the distal clavicle. Using the lateral portal for visualization and the posterior and anterior portals for resection allows the surgeon to visualize the distal clavicle resection and is an effective method for clavicle resection.
The indication for distal clavicle resection was pain at exam either to palpation of the acromioclavicular joint or pain demonstrated at the AC joint with activity9.
Figure 1.
Preoperative x-ray: Note the spur on the inferior aspect of the clavicle as well as the hazy spur on the underside of the acromion.
Figure 2.
Postoperative x-ray. Note the extent of the distal clavicle resection. The underside of the acromion has also been thinned as compared to Figure 1.
Figure 3.
Distal clavicle resection with retained clavicular fragment within the superior capsule, Type Ia
Figure 4.
Large retained clavicular fragment within the AC space. This is a Type Ib. The patient was asymptomatic.
Figure 5.
Superior spike of the distal clavicle, Type II. The patient complained of persistent lateral clavicular pain.
Figure 6.
Status post resection of the spike of the lateral clavicle. Patient reported improved symptoms but still had residual distal clavicle pain.
Figure 7.
Lateral view of the subacromial space. Electrocautery incising the inferior capsule of the AC joint.
Figure 8.
Lateral view of the acromion, status-post acromioplasty. Anterior is at 3 0'clock.
Figure 9.
Lateral view of acromion status-post acromioplasty. Exposed underside of the distal clavicle.
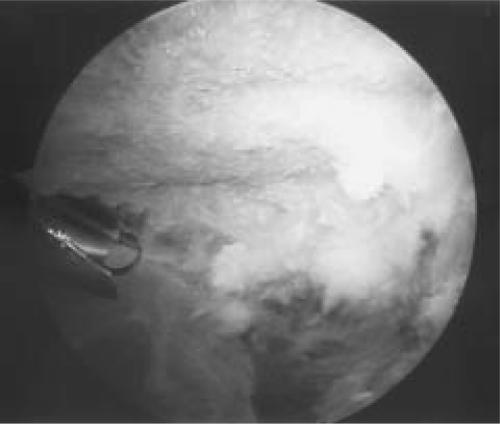
Figure 10.
Dyonics bur in place to begin distal clavicle resection.
Figure 11.
Distal clavicle resection completed. Rotator cuff is well visualized from this portal.
Table I.
| # Subjects | |
|---|---|
| Type 0 | 29 |
| Type Ia (small fragment) | 14 |
| Type IIb (large fragment) | 6 |
| Type II (lat spike) | 8 |
References
- 1.Warner J, Kann D, Maddox L. The arthroscopic impingement test. J Arthroscopic and Related Surg. 1994;10(2):224–230. doi: 10.1016/s0749-8063(05)80099-4. [DOI] [PubMed] [Google Scholar]
- 2.Caspari R, Thal R. A technique for ar throscopic subacromial decompression. J Arthroscopic and Related Surg. 1992;8(1):23–30. doi: 10.1016/0749-8063(92)90131-t. [DOI] [PubMed] [Google Scholar]
- 3.Paulos L, Franklin J. Arthroscopic shoulder decompression development and application-a five year experience. Am J Sports Med. 1990;18(4):235–244. doi: 10.1177/036354659001800303. [DOI] [PubMed] [Google Scholar]
- 4.Gartsman G. Arthroscopic acromioplasty for lesions of the rotator cuff. J Bone and Joint Surg. 1990;72(2):169–180. [PubMed] [Google Scholar]
- 5.Cook FF, Tibone JE. The Mumford procedure in athletes, an objective analysis of function. Am J Sports Med. 1988;16(2):97–100. doi: 10.1177/036354658801600202. [DOI] [PubMed] [Google Scholar]
- 6.Daluga DJ, Dobozi W. The influence of distal clavicle resection and rotator cuff repair on the effectiveness of anterior acromioplasty. Clin Orth Rel Res. 1989;247:117–123. [PubMed] [Google Scholar]
- 7.Snyder JJ, Banas MP, Karzel RP. The arthroscopic Mumford procedure: an analysis of results. J Arthroscopic Rel Surg. 1995;11(2):157–164. doi: 10.1016/0749-8063(95)90061-6. [DOI] [PubMed] [Google Scholar]
- 8.Flatow EL, Duralde XA, Nicholson GP, Pollock RG, Bigliani LU. Arthroscopic resection of the distal clavicle with a superior approach. J Shoulder-Elbow Surg. 1998;4(1):41–50. doi: 10.1016/s1058-2746(10)80007-2. [DOI] [PubMed] [Google Scholar]
- 9.Novak PJ, Bach BR, Jr, Romeo AA, Hager CA. Surgical resection of the distal clavicle. J Shoulder-Elbow Surg. 1998;4(1):35–40. doi: 10.1016/s1058-2746(10)80006-0. [DOI] [PubMed] [Google Scholar]
- 10.Petchell JF, Sonnabend DH, Hughes JS. Distal clavicular excision: a detailed functional assessment. Australia-New Zealand J Surg. 1995;65:262–266. doi: 10.1111/j.1445-2197.1995.tb00625.x. [DOI] [PubMed] [Google Scholar]
- 11.Jobe FW. Shoulder instability in the overhand or throwing athlete. Clin J Sports Med. 1995;14(4):917–935. [PubMed] [Google Scholar]