Abstract
We retrospectively analyzed the importance of factors relating to worker's compensation for 273 wrists in 211 consecutive patients who underwent primary carpal tunnel release. Patients were divided into three groups: non-work related, worker's compensation—uncontested, and worker's compensation—contested. Contested claims were those in which the worker's compensation carrier denied authorization for surgery, and in which such authorization was given following intervention by a plaintiff's attorney. Results: there were no statistically significant differences in postoperative return of grip strength and in postoperative return to work intervals in comparing groups I and II. However, the contested worker's compensation patients were much less likely (and much slower) to return to light duty and to return to full duty work. Return of grip strength was slower and less complete in this group as well. Within worker's compensation, a contested claim portends a poorer prognosis. Uncontested worker's compensation claimants have nearly as good a prognosis as non-compensation patients.
INTRODUCTION
For a variety of conditions including carpal tunnel syndrome, worker's compensation "claimants" have generally been reported to have a poorer prognosis than non-compensation patients24,7,14,10,11,15. Ergonomic factors of force, repetitive pinching and grasping, awkward postures, frequent or prolonged pressure over the volar wrist, and vibration have been implicated in the pathogenesis of carpal tunnel syndrome, whether related to work or to avocational activities20,22,3. Other personal conditions including obesity, advancing age, physical inactivity, and individual wrist dimensions have more recently been implicated17,27,21, although not without controversy18,6. Cigarette smoking has also been associated with carpal tunnel syndrome26.
In several recent reports, investigators have attempted to differentiate whether this poorer prognosis affects all worker's compensation claimants or merely a subgroup. Bonzani et al. cited administrative and psychosocial issues1, and others have suggested that involvement of a plaintiff's attorney complicates matters4,5,23,25. Some investigators have concluded that a normal or nearly normal nerve conduction test predicts a poor prognosis for worker's compensation patients11, but others have concluded that nerve tests have little predictive value8,2,12. We hypothesized that a subgroup of worker's compensation has a poorer prognosis than the overall worker's compensation population regarding carpal tunnel surgery, and we retrospectively attempted to identify one or more factors that may portend a poorer prognosis.
In a related previous unpublished study of 285 patients who underwent 347 open carpal tunnel releases, we did not prove any significant differences between the compensated versus non-compensated patients regarding subjective outcomes. Therefore, for the present study, we elected to study objectively measurable outcomes: complications, further surgery, postoperative recovery of grip strength, and return to light duty and full duty work.
MATERIALS AND METHODS
An independent reviewer retrospectively evaluated all patients in the practice of a single surgeon (DEQ) who underwent primary carpal tunnel release between January 1, 1990 and January 31, 1994. Patients were excluded from the study if they had diabetes mellitus, renal failure, a collagen vascular disease, carpal instability, or if they were pregnant when first seen or had delivered a baby within six months of the primary carpal tunnel release. Patients were also excluded if they had a history of a significant injury, e.g. Colles' fracture or crush injury, to the affected hand or wrist within 24 months of the primary carpal tunnel release. Patients were included who had other surgical procedures on an upper extremity at the time of primary carpal tunnel release, as long as the other procedures did not include surgery within the wrist joint or shoulder area. Patients were followed for six months postoperatively, at which time they were dismissed if they had reached maximum medical improvement and no further active medical or surgical treatment was planned. This review yielded 211 eligible patients who had undergone 273 primary carpal tunnel releases, all of whom were included in this study.
Preoperative evaluations always included serial thorough histories and physical examinations, and almost always included electrodiagnostic testing. The diagnosis of carpal tunnel syndrome required classic median dysesthesias of greater than three months' duration, made worse by activities and/or wrist position, and was confirmed by provocative (percussion, position, and direct pressure) and nonprovocative (sensation and strength) physical examinations.
Conservative nonsurgical treatment was exhausted in all cases prior to surgical intervention, except in cases of electrically confirmed severe neuropathies, in which dense numbness and/or thenar atrophy was present, or in which no response was demonstrated to sensory latency testing. Clinical indications for surgery included persistent pain or numbness, inability to perform activities of daily living, and obvious weakness. Candidates for surgery either had a positive electrodiagnostic test or showed temporary improvement of wrist pain and median dysesthesias following a steroid injection into the affected carpal tunnel in almost all cases.
Surgical methods included either an open carpal tunnel release through a short palmar incision19 (earlier part of study) or a two-portal endoscopic carpal tunnel release by the extrasynovial modification of the method of Chow16 (later part of study). Patients were instructed to remove their bandages at any time after the second postoperative day and were allowed then to shower and wash their wounds, wearing a wrist splint as needed for comfort. In 32 cases when a flexor tenosynovectomy was indicated or a severe neuropathy existed, a longer open incision was employed and the surgical bandage was left in place for ten to fourteen days. The postoperative protocol varied somewhat when concurrent surgical procedures were performed.
Most of the worker's compensation patients in this series were referred by an occupational physician through a managed care network. The occupational physician rechecked the patients three to five days postoperatively, at which time patients were sent back to work if the clinical condition permitted and if suitable light duty was available.
Patients were followed postoperatively as necessary by the hand surgeon, and objective data were collected per protocol at two weeks, six weeks, and six months postoperatively. At each visit, grip strength was measured using the average of three tests of each hand with a Jaymar dynamometer, and work status was recorded.
Evaluation showed that the population could be divided into three samples based upon their Worker's Compensation status. The three groups were designated:
Group I—Non-Worker's Compensation cases
Group II—Worker's Compensation cases, Not Contested
Group III—Worker's Compensation cases, Contested
Contested claims were those in which the worker's compensation insurance carrier denied authorization for surgery, and in which such authorization was given after the patient retained an attorney.
Comprehensive statistical analysis of data was performed. The specific tests used are noted appropriately in the following section.
RESULTS
Demographics, diagnoses, preoperative clinical data, and surgical procedures
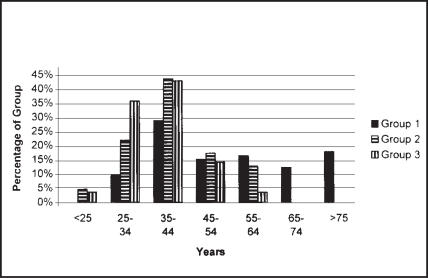
Group I (Non-Worker's Compensation) had 73 patients, including 98 affected wrists, with 87 wrists undergoing primary carpal tunnel release. Group II (Worker's Compensation, Non-Contested) comprised 110 patients, including 169 affected wrists, with 141 wrists undergoing primary carpal tunnel release. Group III (Worker's Compensation, Contested) had 28 patients, including 49 affected wrists, with 46 wrists undergoing primary carpal tunnel release. Table 1 presents demographic data regarding sex, age, hand dominance, and affected hand. Group I (Non-Worker's Compensation) included older patients (Table 1, Figure 1). The patients in Group I were significantly older than patients in either of the other groups, even when those patients over age 65 were excluded (p<.002 in each case, t-test). The two worker's compensation groups did not differ significantly in age, although Group III (Worker's Compensation, Contested) patients were younger. There were no significant differences regarding sex, hand dominance, and affected hand (chi-square analysis). Group III (Worker's Compensation, Contested) had a significantly higher incidence of bilateral carpal tunnel syndrome and underwent a significantly higher percentage of bilateral carpal tunnel releases than either of the other groups (chi-square analysis, see Table 1).
TABLE 1. MATERIALS.
| Group I Non-WC |
Group II WC Not Contested |
Group III WC Contested |
|
|---|---|---|---|
| Number of patients | 73 | 110 | 28 |
| Female | 78% | 78% | 79% |
| Mean Age, yrs | 54.2 | 40.3 | 37.7 |
| Right-handed | 88% | 94% | 93% |
| Bilateral CTS | 34% | 54% | 75%* |
| Total # wrist with CTS | 98 | 169 | 49 |
| Total CTS wrists undergoing surgery (%) | 89% | 83% | 94% |
| Total CTS wrist undergoing Bilateral Surgery | 14% | 22% | 39%** |
Note: CTS= carpal tunnel syndrome
p<.001, chi-sq. analysis
p<.01, chi-sq. analysis
Figure 1. Age at Surgery.
Age of patients at time of first carpal tunnel release. Surgery was performed upon patients of varying ages. The youngest patients were worker's compensation patients, and the oldest patients were not employed.
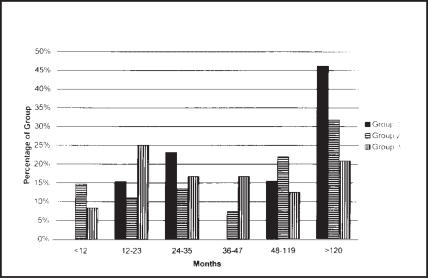
Data regarding employment are presented in Table 2 and Figure 2. The only significant differences between groups were that fewer Group I (Non-Worker's Compensation) patients were employed, and that more patients in Group III (Worker's Compensation, Contested) worked in a meat packing plant. We were unable to correlate the onset of carpal tunnel syndrome with duration of employment.
TABLE 2. EMPLOYMENT.
| Group I Non-WC |
Group II WC Not Contested |
Group III WC Contested |
|
|---|---|---|---|
| Work Type: | |||
| Heavy (%) | 16 | 21 | 18 |
| Factory (%) | 6 | 21 | 11 |
| Meat Packing (%) | 1 | 7 | 21* |
| Clerical (%) | 29 | 49 | 50 |
| Light Or Unemp. (%) | 48** | 2 | 0 |
| Preoperative Work Status: | |||
| Full duty (%) | 39 | 48 | 39 |
| Light duty (%) | 10 | 39 | 29 |
| Not Working (%) | 51 | 13 | 32 |
p=.002, chi-sq.
p<.001, chi-sq
Figure 2. Duration of Employment Before Surgery.
Duration of Employment Before Surgery. We were unable to statistically correlate the onset of carpal tunnel syndrome with duration of employment. Some worker's compensation patients developed significant symptoms after less than one year on the job; many non-compensation patients had endured symptoms for over ten years.
Diagnostic data regarding carpal tunnel syndrome are listed in Table 3. Patients in Group III (Worker's Compensation, Contested) more commonly had pain as the major clinical finding, and less commonly had a positive confirmatory electrodiagnostic test. These values were not statistically significant.
TABLE 3. DIAGNOSIS OF CARPAL TUNNEL SYNDROME (PERCENTAGE OF SYMPTOMATIC WRISTS).
| Group I Non-WC |
Group II WC Not Contested |
Group III WC Contested |
|
|---|---|---|---|
| Nocturnal Dysesthesias, Pain | 69 | 61 | 82 |
| Positive Tinel Sign | 65 | 47 | 60 |
| Positive Phalen Test | 80 | 58 | 89 |
| Positive Direct Pressure Sign | 63 | 55 | 51 |
| Decreased Sweating | 9 | 12 | 2 |
| Abnormal Static 2 Point Discrim. | 36 | 21 | 27 |
|
Electrodiagnostic Testing Affected wrists tested (%) |
95 | 93 | 98 |
| Confirmed clinical diagnosis (%) | 95 | 90 | 69 |
Concurrent diagnoses are listed in Table 4. Obesity, defined as body weight at least 30% above recommended normal weight, was common at 25-30% in each group. For each patient, a thorough and detailed examination often disclosed one or more additional diagnoses in addition to carpal tunnel syndrome. The most common associated diagnosis was cubital tunnel syndrome. Group I (Non-Worker's Compensation) more commonly had trapeziometacarpal arthritis. Patients in Group III (Worker's Compensation, Contested) tended to have a higher number of entrapment neuropathies and to more commonly have diffuse myofascial pain, whether limited to the upper extremity and shoulder or not. Group III patients also tended to have more diagnoses than the other two groups, indicating a propensity to have both more generalized pathology and more focal pathologies than the other groups.
TABLE 4. CONCURRENT DIAGNOSES (PERCENTAGE OF SYMPTOMATIC WRISTS).
| Group I Non-WC |
Group II WC Not Contested |
Group III WC Contested |
|
|---|---|---|---|
| Obesity | 30 | 28 | 25 |
| Cubital Tunnel Syndrome | 15 | 18 | 35 |
| Myofascial Pain Syndrome | 6 | 8 | 20* |
| (Neck, Shoulder, Upper Arm) | 4 | 5 | 18 |
| (Low Back Pain Or Headaches) | 0 | 1 | 4 |
| Median Nerve Entrapment At Elbow | 5 | 5 | 12 |
| Medial or Lateral Epicondylitis | 2 | 6 | 8 |
| Thoracic Outlet Syndrome | 2 | 1 | 4 |
| Dequervain's (Extensor Tendon) | 5 | 3 | 4 |
| Arthritis Trapeziometacarpal Jt. | 13** | 4 | 4 |
| Ulnar Nerve Compression At Wrist | 0 | 2 | 4 |
| Radial Nerve Entrapment At Elbow | 2 | 4 | 2 |
| Stenosing Flexor Tenosynovitis | 4 | 4 | 2 |
| Dupuytren's Or Palmar Fibromas | 0 | 1 | 2 |
| Shoulder Impingement Syndrome | 6 | 3 | 0 |
| Other Diagnoses per extremity with CTS: | |||
| One other diagnosis | 44 | 37 | 45 |
| Two other diagnoses | 7 | 11 | 16 |
| Three other diagnoses | 4 | 0 | 8 |
p=.04, chi-sq.
p<.05, chi-sq.
Details of nonsurgical treatment are listed in Table 5. As previously noted, nonsurgical care was exhausted preoperatively for all patients, unless a very severe neuropathy was noted, in which case surgery was done immediately.
TABLE 5. NONSURGICAL TREATMENT, PREOPERATIVE, PERCENTAGE OF PATIENTS.
| Group I Non-WC |
Group II WC Not Contested |
Group III WC Contested |
|
|---|---|---|---|
| Wrist Splint (%) | 66 | 84 | 82 |
| Steroid Injection IM (%) | 5 | 14 | 25 |
| Oral Medications (%) | 51 | 80 | 100 |
| Physical Therapy (%) | 1 | 6 | 18 |
| Ergonomic Modifications-Job (%) | 11 | 36 | 39 |
| Steroid Inject.Carpal Tunnel (%) | 11 | 36 | 46 |
| Work Restrictions (%) | 0 | 19 | 4 |
| Time Completely Off Work (%) | 0 | 3 | 11 |
| None-Severe Neuropathy (%) | 14 | 3 | 0 |
Data regarding the index primary carpal tunnel release operation are presented in Table 6. There were no significant differences between the groups regarding the method used for the carpal tunnel release operation (chi-square analysis). Bilateral carpal tunnel releases were more commonly performed for Group III (Worker's Compensation, Contested) patients. Data regarding concurrent surgical procedures are shown in Table 7. Each of the worker's compensation groups underwent more surgical procedures than the non-compensation group (p=.0013, chi-square analysis).
TABLE 6. SURGICAL PROCEDURES (INDEX OPERATION), NUMBER OF WRISTS.
| Group I Non-WC |
Group II WC Not Contested |
Group III WC Contested |
|
|---|---|---|---|
| Short incision open CTR | 51 | 79 | 23 |
| Two-portal Endoscopic CTR | 29 | 45 | 15 |
| Standard CTR | 7 | 17 | 8 |
| Bilateral CTR (staged) | 14 | 31 | 18* |
p<.05, chi-sq.
TABLE 7. CONCURRENT SURGICAL PROCEDURES (AT INDEX OPERATION), PERCENTAGE OF PATIENTS UNDERGOING.
| Group I Non-WC |
Group II WC Not Contested |
Group III WC Contested |
|
|---|---|---|---|
| Ulnar neuroplasty at elbow | 14 | 25 | 29 |
| Median neuroplasty at elbow | 6 | 5 | 14 |
| Extens. Tendon sheath incision wrist | 5 | 2 | 2 |
| Flexor or extensor tenosynovectomy | 2 | 4 | 2 |
| Injection joint hand or wrist | 2 | 3 | 0 |
| Fasciectomy epicondyle at elbow | 1 | 2 | 2 |
| Injection shoulder | 1 | 1 | 0 |
| Opponensplasty | 1 | 0 | 0 |
| Ulnar neuroplasty at wrist | 1 | 5 | 8 |
| Excision palmar fascia | 0 | 0 | 2 |
| Incision flexor tendon sheath | 0 | 1 | 0 |
| Radial neuroplasty at elbow | 0 | 2 | 0 |
| Totals: | |||
| One concurrent procedure w/ CTR | 30 | 45 | 33 |
| Two or more concurrent procedures | 2 | 8 | 14 |
Complications of surgery
The only surgical complications were a total of four infections in this series of 277 wrists (1.4%). All resolved with wound care and oral antibiotics. However, excessive postoperative pain and dysfunction were noted in 11% (10 of 87) of the Group I (Non-Worker's Compensation) patients and in 31% of each of the two worker's compensation groups (46 of 141 and 15 of 46 patients respectively) (p<.001 in each case, chi-sq.). This problem was treated with a specific program of hand therapy and/or an intramuscular injection of a long-acting corticosteroid. There were no cases of documented reflex sympathetic dystrophy.
Further surgery
Two of 73 patients in Group I (Non-Worker's Compensation) underwent a later surgical procedure. Only one of these procedures, a median neurolysis at the elbow, was on a previously operated extremity.
Eight of 110 patients in Group II (Worker's Compensation, Non-Contested) underwent a later surgical procedure. These patients underwent a total of three ulnar neuroplasties at the elbow, three median neuroplasties at the elbow, two flexor tendon sheath incisions, and two wrist flexor or extensor tenosynovectomies. Each of these procedures was done within twelve months of the index primary carpal tunnel release, and each was performed on the ipsilateral upper extremity.
One of 28 patients in Group III (Worker's Compensation, Contested) underwent a later surgical procedure, which was an ulnar neuroplasty at the elbow.
Postoperative recovery of grip strength
We excluded patients over 65 years of age in order to better study the importance of compensation. Using linear regression analysis for each operated wrist, we plotted the slope of the best fit line for data points (days since surgery, grip strength). Patients in Group III (Worker's Compensation, Contested) recovered grip strength more slowly than patients in Group I (Non-Worker's Compensation) (p=.036, Mann-Whitney rank sum test). Similarly, patients in Group III (Worker's Compensation, Contested) recovered grip strength more slowly than patients in Group II (Worker's Compensation, Non-Contested) (p=.005, Mann-Whitney rank sum test). There was no difference in recovery of grip strength in comparing Group I (Non-Worker's Compensation) and Group II (Worker's Compensation, Non-Contested) (p=.769, Mann-Whitney rank sum test). (Data regarding postoperative return of grip strength had large variances, and this data cannot be fairly or accurately extrapolated to a population. Therefore, we used the rank sum statistical test.)
Postoperative return to light duty work
Effect of compensation status: Data are presented in Figure 3. Average time completely off work was 3.26 weeks for Group I (range 0.5- 10.0 weeks), 3.89 weeks for Group II (0.5- 12.0 weeks), and 8.74 weeks for Group III (1.0- 31.0 weeks). Data were evaluated using a standard t-test and the Mann-Whitney rank sum test. Patients in Group III (Worker's Compensation, Contested) returned to light duty work less rapidly and less often than patients in Group I (Non-Worker's Compensation) (p=.005, t-test). Similarly, patients in Group III (Worker's Compensation, Contested) returned to light duty work less rapidly and less often than patients in Group II (Worker's Compensation, Non-Contested) (p<.001, t-test). There was no significant difference in time to return to light duty work in comparing Groups I and II using the t-test (p=.365). However, Mann-Whitney test results showed a significant difference between all three groups (p<.001 in each case). The return to work time for the non-worker's compensation cases is lower than that of either compensated group, but a more obvious difference is noted between Group III and Groups I and II (Figure 3).
Figure 3. Return to Light Duty.
Postoperative return to light duty work. Patients with contested worker's compensation claims returned to restricted work significantly less rapidly and less often than patients in the other two groups. The remainder of the worker's compensation patients returned to work nearly as quickly as non-compensated patients.
Postoperative return to light duty work
Effect of multiple procedures: In the entire study population as a whole, patients who underwent one surgical procedure (primary carpal tunnel release) were off work an average of 3.2 weeks (range 1-10 wks). Patients who underwent two surgical procedures (primary CTR plus one other procedure) were off work an average of 4.1 weeks (range 1-10 weeks). Patients who underwent three surgical procedures (primary CTR plus two other procedures) were off work an average of 8.0 weeks (range 2-31 weeks).
Postoperative return to full duty work
We evaluated this data using a standard t-test and the Mann-Whitney rank sum evaluation. Data are presented in Figure 4. Average time to return to full time unrestricted work was 6.4 weeks for Group I (range 1.0- 15 weeks), 8.7 weeks for Group II (1.0- 33 weeks), and 20.15 weeks for Group III (6.0- 70 weeks).
Figure 4. Return To Full Duty.
Postoperative return to full duty work. Patients with contested worker's compensation claims returned to unrestricted work significantly less rapidly and less often than patients in the other two groups. The remainder of the worker's compensation patients returned to work nearly as quickly as non-compensated patients.
Patients in Group III (Worker's Compensation, Contested) returned to full duty work less rapidly and less often than patients in Group I (Non-Worker's Compensation) (p<.005, t-test, p<.001, Mann-Whitney test ). Similarly, patients in Group III (Worker's Compensation, Contested) returned to full duty work less rapidly and less often than patients in Group II (Worker's Compensation, Non-Contested) (p<.001, t-test, p<.001, Mann-Whitney test). There was no significant difference in return to full duty work in comparing Groups I and II using the t-test (p=.10). However, Mann-Whitney test results showed a significant difference between all three groups (p<.001 in each case). The time to return to full duty for the non-worker's compensation cases is lower than that of either compensated group, but a more obvious difference is again noted between Group III and Groups I and II (Figure 4).
About 90% of in Group II (Worker's Compensation, Non-Contested) patients did return to full time, full duty work at the original employer without restrictions. In Group III (Worker's Compensation, Contested), 70% did return to the work force, but only 46% returned to full time unrestricted work at the original employer.
Surgical method
We found no significant differences between populations in the rates of return of grip strength in comparing the two methods of carpal tunnel release, i.e. short open palmar incision vs. two-portal endoscopic method, although a small number of patients undergoing the endoscopic release had a remarkably rapid recovery. In this retrospective review, we did not demonstrate a more rapid return to work following endoscopic carpal tunnel release when compared with open carpal tunnel release through a short palmar incision.
DISCUSSION
Many factors influence the outcome of carpal tunnel surgery. Worker's compensation patients have been reproved because they are claimants in a legal process9. For various physical conditions, many reports associate worker's compensation with a higher chance of a poor outcome24,7,14. However, other reports identify the involvement of a plaintiff's attorney and pending litigation as the more significant factor within the population of worker's compensation claimants, and these reports associate this litigation with a prolonged recovery and less desirable outcome4,5,23,25. The present study confirms that minimally invasive surgery is generally associated with a relatively rapid return to work19,16, and also demonstrates that additional surgical procedures will predictably delay the return to work. According to our results, the vast majority of patients who undergo primary carpal tunnel release can expect to return to work regardless of their compensation status. However, there is a subgroup of worker's compensation hand surgery patients for whom the prognosis must be much less optimistic.
We retrospectively evaluated comparable populations of compensation and non-compensation patients undergoing primary carpal tunnel surgery. Within the compensation group, a subgroup existed which had the following characteristics: patients were younger, more often had bilateral carpal tunnel syndrome, more commonly complained of pain, and more commonly had negative electrodiagnostic tests. However, in the face of classic repeated history and physical examination findings, the clinicians involved concluded that the patient met the criteria for carpal tunnel syndrome. These patients more commonly had myofascial pain syndromes and also more commonly had clinical and electrodiagnostic evidence of multiple entrapment neuropathies. Like others with carpal tunnel syndrome, they were often overweight21,18. When nonsurgical treatment failed, these patients underwent carpal tunnel release in an attempt to relieve the portion of their symptoms that was due to median nerve entrapment at the wrist.
Within this subgroup, in all cases, the employer or worker's compensation insurance carrier initially denied a request for authorization to perform surgery. Following intervention by a plaintiff's attorney, this authorization was later received. These patients have a conflict with the employer or with the worker's compensation insurance carrier. (We did not attempt to identify a similar subgroup of patients who were lost to follow-up after the surgeon requested authorization for surgery and received a letter of denial.)
The occupational physician and hand surgeon are often unaware of the dynamics relating to the decision to deny authorization for surgery. The duration of employment, the employee's work record, and the employee's personal relations with co-workers, management, company health workers, insurance adjusters, and other physicians may be important. Other medical conditions affecting the employee, previous injuries, and prior worker's compensation claims can make a difference. Ergonomic considerations regarding the current or responsible employment must be considered in light of other past or current employment. Outside activities which demand repetitive pinching or grasping are relevant. We carefully evaluate these factors in all cases. If, in this setting, the surgeon recommends surgery yet the insurance carrier rejects the claim, declining to authorize surgery, the patient is likely to be dissatisfied, and may seek legal advice. In our state, once the patient retains an attorney, all communication from the insurance carrier must then be through the patient's attorney. The delays of the legal process further compound the emotional, social, and financial factors relating to the disability.
Sometimes, a part of the problem is that the diagnosis and causation are less than clear. Many patients in the practices of occupational medicine and hand surgery have the primary problem of pain. While these patients may have compressive neuropathies, they may also have other soft tissue problems which are variously labeled tendonitis, myofascial pain, repetitive strain injury, cumulative trauma, occupational cervicobrachial disorder, or one of many other names. These conditions, whether work related or not, may compromise surgical and nonsurgical outcomes9,13. Each of the worker's compensation groups in this study did have a more significant problem of disabling postoperative pain for which therapy and/or corticosteroids were necessary.
However, we have shown very satisfactory outcomes from carpal tunnel surgery in our worker's compensation patients in whom the diagnosis was not contested. Indeed, the results are very comparable to those of noncompensation patients. Objective measurements of postoperative return of grip strength, postoperative return to light duty work, and postoperative return to full duty work correlated very well with each other. After surgery, the contested worker's compensation claimants were slower and less likely to regain preoperative grip strength, and the results regarding return to work paralleled this finding.
Before performing surgery, we discuss the anticipated postoperative rehabilitation with each patient. Our experience is that patients will do much better if they are promptly returned to light duty after surgery. This requires cooperation from the patient and the employer. Through our managed care network, we have educated employers and representatives of insurance carriers regarding the need to create suitable light duty work in order to return the employee to work as soon as possible. We instruct patients to elevate their hands for three days. After that time, patients rarely need narcotic pain medication and are usually able to drive an automobile with care. Therefore, we expect that our patients will be able to return to light duty work three to seven days following carpal tunnel surgery via either of the methods discussed in this article, although this decision may be influenced by a variety of other factors.
This study is limited in that we were unable to exactly determine the earliest date of return to work in many cases. Rather, work status was noted in the chart at each follow-up visit, and was retrospectively assessed. We expect to be able to document, in a new prospective study, the more rapid return to work (usually three days postoperatively) that we generally prescribe. We continue to believe that elucidation of factors which influence outcomes can help to clarify the prognosis in worker's compensation cases.
ACKNOWLEDGMENT
The authors wish to thank the following occupational physicians for allowing the inclusion of their patients in this study: Drs. David Berg, Wesley Brown, Paul Fowler, Camilla Frederick, Gerald Looney, Richard McCaughey, Maurice Minervini, N. John Prevo, Ronald Rossing, Anthony Sciorrotta, Dennis Swena, and Robert Tobias.
Footnotes
Supported by a grant from: Iowa Methodist Medical Center, Des Moines, Iowa 50309
References
- 1.Bonzani PJ, Millender L, Keelan B, Mangieri MG. Factors prolonging disability in work-related cumulative trauma disorders. J Hand Surg. 1997;22-A:30–34. doi: 10.1016/S0363-5023(05)80176-5. [DOI] [PubMed] [Google Scholar]
- 2.Braun RM, Jackson WJ. Electrical studies as a prognostic factor in the surgical treatment of carpal tunnel syndrome. J Hand Surg. 1994;19-A:893–900. doi: 10.1016/0363-5023(94)90086-8. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control, committee. Occupational disease surveillance: carpal tunnel syndrome. Morbidity Mortality Weekly Report. 1989 Jul 21;38(28):485–489. [PubMed] [Google Scholar]
- 4.Dichraff RM. When the injured worker retains an attorney. AAOHN J. 1993;41(10):491–498. [PubMed] [Google Scholar]
- 5.Dworkin RH, Handlin DS, Richlin DM, Brand L, Vannucci C. Unraveling the effects of compensation, litigation, and employment on treatment response in chronic pain. Pain. 1985;23(1):49–59. doi: 10.1016/0304-3959(85)90229-5. [DOI] [PubMed] [Google Scholar]
- 6.Gerr F, Letz R. Letter re: Nathan et al: Obesity as a risk factor. J Occup Med. 1992;34:1117–1118. doi: 10.1097/00043764-199211000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Greenough CG, Taylor LJ, Fraser RD. Anterior lumbar fusion. A comparison of noncompensation patients with compensation patients. Clin Orthop. 1994;300:30–37. [PubMed] [Google Scholar]
- 8.Grundberg AB. Carpal tunnel decompression in spite of normal electromyography. J Hand Surg. 1983;8-A:348–349. doi: 10.1016/s0363-5023(83)80179-8. [DOI] [PubMed] [Google Scholar]
- 9.Hadler NM. Repetitive upper-extremity motions in the workplace are not hazardous. J Hand Surg. 1997;22-A:19–29. doi: 10.1016/S0363-5023(05)80175-3. [DOI] [PubMed] [Google Scholar]
- 10.Higgs PE, Edwards DF, Martin DS, Weeks PM. Carpal tunnel surgery outcomes in workers: effect of worker's compensation status. J Hand Surg. 1995;20-A:354–359. doi: 10.1016/S0363-5023(05)80086-3. [DOI] [PubMed] [Google Scholar]
- 11.Higgs PE, Edwards DF, Martin DS, Weeks PM. Relation of preoperative nerve-conduction values to outcome in workers with surgically treated carpal tunnel syndrome. J Hand Surg. 1997;22-A:216–221. doi: 10.1016/s0363-5023(97)80154-2. [DOI] [PubMed] [Google Scholar]
- 12.Louis DS, Hankin FM. Symptomatic relief following carpal tunnel decompression with normal electroneuromyographic studies [Retracted by Hankin, FM; and Louis, DS in Orthopaedics, 11:532, 1988 and 11:1244, 1988] Orthopaedics. 1987;10:434–436. doi: 10.3928/0147-7447-19870301-06. [DOI] [PubMed] [Google Scholar]
- 13.McKinnon SE, Novak CB. Repetitive strain in the workplace. J Hand Surg. 1997;22-A:2–18. doi: 10.1016/S0363-5023(05)80174-1. [DOI] [PubMed] [Google Scholar]
- 14.Misamore GW, Ziegler DW, Rushton JL., II Repair of the rotator cuff. A comparison of results in two populations of patients. J Bone Jt Surg. 1995;77-A:1335–1339. doi: 10.2106/00004623-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Mont MA, Mayerson JA, Krackow KA, Hungerford DS. Total knee arthroplasty in patients receiving worker's compensation. J Bone Jt Surg. 1998;80-A:1285–1290. doi: 10.2106/00004623-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Nagle DJ. Endoscopic carpal tunnel release: Chow dual-portal technique. AAOS Instr Course Lect. 1995;44:155–160. [PubMed] [Google Scholar]
- 17.Nathan PA, Keniston RC. Carpal tunnel syndrome and its relation to general physical condition. Hand Clinics. 1993;9:253–261. [PubMed] [Google Scholar]
- 18.Nathan PA, Keniston RC, Myers LD, Meadows KD. Obesity as a risk factor for slowing of sensory conduction of the median nerve in industry. J Occup Med. 1992;34:379–383. [PubMed] [Google Scholar]
- 19.Nathan PA, Meadows KD, Keniston RC. Rehabilitation of carpal tunnel surgery patients using a short surgical incision and an early program of physical therapy. J Hand Surg. 1993;18-A:1044–1050. doi: 10.1016/0363-5023(93)90401-N. [DOI] [PubMed] [Google Scholar]
- 20.Silverstein BA, Fine LJ, Armstrong TJ. Occupational factors and carpal tunnel syndrome. Am J Industrial Med. 1987;11:343–358. doi: 10.1002/ajim.4700110310. [DOI] [PubMed] [Google Scholar]
- 21.Stallings SP, Kasdan ML, Soergel TM, Corwin HM. A case-control study of obesity as a risk factor for carpal tunnel syndrome in a population of 600 patients presenting for independent medical examination. J Hand Surg. 1997;22-A:211–215. doi: 10.1016/S0363-5023(97)80153-0. [DOI] [PubMed] [Google Scholar]
- 22.Stock SR. Workplace ergonomic factors and the development of musculoskeletal disorders of the neck and upper limbs: a meta-analysis. Am J Industrial Med. 1991;19:87–107. doi: 10.1002/ajim.4700190111. [DOI] [PubMed] [Google Scholar]
- 23.Talo S, Hendler N, Brodie J. Effects of active and completed litigation on treatment result. J Occup Med. 1989;31(3):265–269. doi: 10.1097/00043764-198903000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Tollison CD. Compensation status as a predictor of outcome in nonsurgically treated low back injury. Southern Med J. 1993;86(11):1206–1209. doi: 10.1097/00007611-199311000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Trief P, Stein N. Pending litigation and rehabilitation outcome of chronic back pain. Arch Phys Med Rehabil. 1985;66:95–99. [PubMed] [Google Scholar]
- 26.Vessey MP, Villard-Mackintosh L, Yeates D. Epidemiology of carpal tunnel syndrome in women of childbearing age. Int J Epidemiol. 1990;19(3):655–659. doi: 10.1093/ije/19.3.655. [DOI] [PubMed] [Google Scholar]
- 27.Werner RA, Albers JW, Franzblau A, Armstrong TJ. The relationship between body mass index and the diagnosis of carpal tunnel syndrome. Muscle Nerve. 1994;17:632–636. doi: 10.1002/mus.880170610. [DOI] [PubMed] [Google Scholar]