Abstract
We are reporting a practical technique for the production of antibiotic beads for use in combating musculoskeletal infections. The technique utilizes bead molds with tobramycin powder mixed with polymethylmethacr ylate on twisted wire strands to produce strands of 25 beads of various sizes. These beads are gas sterilized and available for use "off the shelf" in a manner that is much more efficient than traditional production by hand on the back table in the operating room. Our technique was also utilized at a second institution to demonstrate its efficacy at another site.
INTRODUCTION
Antibiotic beads have gained wide acceptance in orthopedics in the treatment of a variety of skeletal infections due to their ability to provide high concentrations of antibiotic at the site of infection while avoiding the complications associated with systemic toxicity.8,11 Traditionally, beads have been made by hand in the operating room on the back table during the case. This is a time consuming and cumbersome process, and is an inefficient use of resources. The antibiotic is not uniformly distributed, the bead size and shape is inconsistent and the beads are not well attached to the wire. In addition, the methylmethacrylate monomer, known to be toxic to musculoskeletal tissue, is still present for the first two hours after mixing the beads.12,13 Prefabricated beads are less expensive and easier to use. They allow for more uniform delivery of the antibiotic and are of better quality and consistency than hand made beads (Figure 1). Although the FDA has approved the use of antibiotics in beads, these beads are not commercially available because no company has been approved to sell the combined product. The purpose of this article is to outline and illustrate our technique, and provide practitioners with all the information required for the production of these beads using molds. We report the evaluation of our technique at the University of New Mexico in terms of improvements in quality, efficiency and cost of bead production with molds compared to traditional methods. We also report experience using these techniques at another institution.
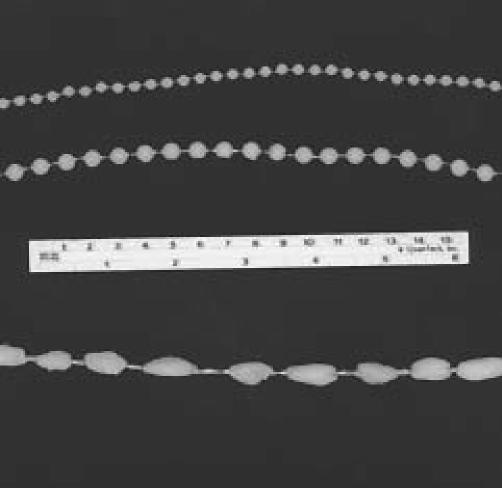
Figure 1.
The 6.4 mm diameter and 5.0 mm diameter mold produced beads are compared to the typical hand made beads.
MATERIALS AND METHODS
The first step in the prefabrication of antibiotic beads is obtaining bead molds. We utilized the metal casted teflon coated molds commercially available from the University of Vermont (Figure 2).3 Each mold will make two chains of 25 beads that are 6.4 mm in diameter. The materials are then assembled (Table I). Beads are made in a clean vacuum hooded environment by the formula described in Table 2. Two strands of 26 gauge wire are twisted together fifty turns using a hand drill and placed in the slots of the mold. One 40 gram packet of sterile methacrylate monomer powder is mixed with two vials of tobramycin powder (1.2 grams each), and then divided into five equal, eight gram portions utilizing a laboratory scale, and placed into specimen cups. The monomer is aspirated into a 20cc syringe using an 18 gauge filter needle. Four milliliters of monomer is mixed with the eight grams of powder mixture for 30 seconds and placed in two 10cc syringes. The liquid is then sequentially injected into each hole in the bead mold with gentle pressure. Excess cement is removed by scraping the tongue depressor along the top of the mold, and the molds are allowed to set for twenty minutes. The beads are subsequently taken from the molds and flashing is removed. When the process is complete, each bead chain is placed in a sterile peal pack and gas sterilized using ethylene oxide gas. The sterile packets are opened in the operating room for use as they are needed.
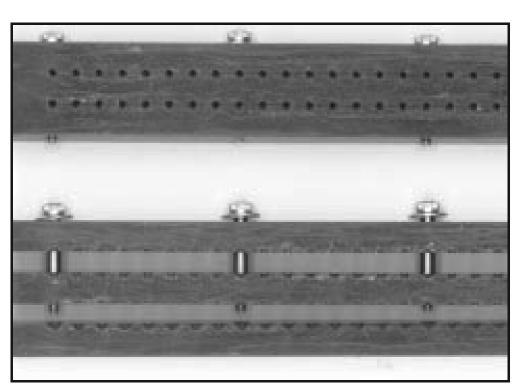
Figure 2.
The black, forged metal, teflon-coated bead molds for the 6.4mm diameter beads are shown. This mold produces two chains of 25 beads.
TABLE 1. MATERIAL FOR BEAD PRODUCTION.
The materials for bead production
Antibiotic bead mold:
Sizes:
|
TABLE 2. METHOD FOR BEAD PRODUCTION.
The method of bead production
|
Steps 6 through 8 should take no longer than 5 minutes.
Makes 10 bead strands total.
To determine the efficiency of this bead production method we compared the cost and time of our bead production method with traditional hand methods. We compared the total cost of the components of each technique and the amount of time to use each technique. The bead production method described was the end result of attempting over twenty different techniques for antibiotic bead production using molds. The cost of production included the mold, antibiotic powder, polymethylmethacrylate, wire, syringes and gas sterilization. The time included time to assemble the materials, production of the beads and sterilization time. The costs of the traditional method included the antibiotic powder, polymethylmethacrylate, wire, and cost of the operating room. The time included time to assemble the materials, and production of the beads. We also investigated the potential for this technique to be used at another institution.
RESULTS
This method was successful at the routine production of tobramycin impregnated polymethylmethacrylate bead chains. The cost of bead production with molds was eighty dollars per chain. The cost of bead production by traditional methods was two hundred and seven dollars per chain. The cost savings were the result of improved efficiency through marked reduction in wasted material. Eight chains were produced per batch of cement with prefabrication while hand-made technique averaged 1.5 chains/batch. Prefabricated beads were made in batches in a laboratory setting with economies of scale in set-up costs and marked reduction in cost compared to the operating room production of hand made beads. This cost efficiency was ten times greater than the increased cost of packaging, sterilization and storage of prefabricated beads. The time to make one chain with molds averaged twelve minutes. The time to make one chain by traditional methods was twenty-eight minutes. This represents a thirty percent improvement in cost, and a thirty-five percent reduction in time. When sterile unused cement was scavenged from arthroplasty cases and utilized in bead production, cost savings were increased to fifty-five percent. In addition to the quantitative advantages of bead production with molds, there were also distinctive qualitative advantages. The beads were vastly more uniform and more firmly attached to the wire. The antibiotic appeared to be more evenly distributed within the beads, and there also appeared to be less debris. The bead size was more appropriate for the majority of wounds than the hand made beads, which tended to be too large. Using the molds we were able to produce ten bead chains from one batch of cement. The hand made method produced only two bead chains.
This antibiotic bead production technique was utilized at a second institution to investigate its general potential applicability. Texas Tech University in El Paso, Texas had previously used hand made antibiotic bead technique. The second site purchased the bead molds and after two demonstrations of the technique were able to effectively produce the beads and incorporate them into clinical practice. This required cooperation among the Department of Orthopedics, the operating room, pharmacy and sterile processing.
DISCUSSION
At the University of New Mexico, the most common indications for the use of antibiotic beads are for open fractures, large infected wounds, chronic osteomyelitis, infected nonunions and secondary nailing after external fixation.1,2,6,9 They have also been successfully used in the treatment of traumatic gun shot wounds and contaminated bowel wounds.10 One example of the use of antibiotic beads is that of the antibiotic bead pouch technique in the initial treatment of an open fracture.4,7 In this technique, the wound is irrigated and debrided, and skeletal fixation is achieved by standard orthopedic procedures. A chain of antibiotic beads is placed in the wound, especially in the dead space of bone loss. The wound is covered with a semi-permeable opsite, which prevents fluid leaking and desiccation while allowing oxygen to pass. An overflow drain to gravity only is placed to prevent the opsite from detaching from the skin and is removed after 36 hours. Beads are removed once a nice vascular bed develops typically at four days. At that point, assessment is made to determine the need for a bone graft or soft tissue coverage.5
Because antibiotic beads have historically been produced by the orthopedic surgeons themselves, pharmacy involvement has been minimal. With the new methods available for bead production, pharmacy intervention could help to further minimize the obstacles associated with antibiotic bead production.3
Molds are available to make beads in three sizes: 6.4 mm, 4.0 mm, and 3.2 mm.3 It was very difficult to inject the cement into the small opening for the 3.2 mm beads, so we abandoned this technique. The 6.4mm beads are the most appropriate for the vast majority of indications, although the 4.0mm beads were useful in the hand and selected small wounds elsewhere in the body. The molds can be re-coated with teflon if wear occurs. We have used molds more than two hundred times and have not yet needed re-coating.
The shelf life of prefabricated antibiotic beads has been reported to be in excess of one year in pharmacokinetic studies by Walenkamp14 and in Septopal beads sold commercially in Europe. Based upon the method of sterile processing and packaging that we utilized, we identify a six month shelf life on the peal pack. We did not perform a comparison of the elution characteristics of prefabricated beads to those made in the operating room, nor is this a comparison of clinical efficacy of these two techniques.
There are a variety of other techniques across the country for using molds. Another type of mold that is available is the plastic, disposable bead mold which can be purchased from the University of Minnesota. These molds consist of two plastic molded half domes which clamshell together and are secured by stainless steel sliding channels. A longitudinal slot accepts 0-prolene suture or 20-gauge stainless steel wire. Three chains of 25 beads are produced with each mold. Although these are less expensive molds ($55/mold), we encountered a variety of insurmountable problems when using them. It was very difficult to get the cement into the molds at just the right consistency, which often resulted in the premature consolidation of the cement. Often the two half domes were not well attached to each other or to the wire. Significantly more cement was required for each mold due to the excess amount of flashing and the large increase in wasted material. It was difficult to keep, or insure that the wire was in the track, which resulted in beads that were not centered or were not even attached to the wire.
Molds could also be used in the operating room. We found this technique less reliable and less efficient in both cost and time. We also attempted to make our own molds using a variety of designs. None of them were as good or efficient as the molds purchased and described in our technique.
SUMMARY
Antibiotic beads can be produced by acquiring commercially available, forged metal teflon coated molds with the materials and methods described in this article. This bead chain production method resulted in significant savings of cost and time with improvement in bead quality. This method is recommended to the orthopedic surgeon currently using the traditional hand-made technique in the operating room.
References
- 1.Behrens F. Fracture with soft tissue injuries. In: Browner BD, Levine AM, Jupiter JB, Trafton PG, editors. Skeletal Trauma. I. Philadelphia: WB Saunders Co; 1992. pp. 321–323. [Google Scholar]
- 2.Fears RL, Gleis GE, Seligson D. Skeletal Trauma. 2. Vol. 1. Philadelphia: WB Saunders Co; 1998. Diagnosis and Treatment of Complications; pp. 568–575. [Google Scholar]
- 3.Goodell JA, Flick AB, Hebert JC, Howe JG. Preparation and release characteristics of tobramycin impregnated polymethylmethacrylate beads. Am J Hosp Pharm. 1986;43:1454–1460. [PubMed] [Google Scholar]
- 4.Henry SL, Ostermann PAW, Seligson D. The antibiotic bead pouch technique: The management of severe compound fractures. Clin Orthop. 1993;295:54–62. [PubMed] [Google Scholar]
- 5.Henry SL, Ostermann PAW, Seligson D. The prophylactic use of antibiotic impregnated beads in open fractures. J Trauma. 1990;30:1231–1238. doi: 10.1097/00005373-199010000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Laurencin C, Gerhart T, Witschger P, Satcher R, Domb A, Rosenburg AF, Hanff P, Edsberg L, Hayes W, Langer R. Bioerodible polyanhydrides for antibiotic drug delivery in vivo osteomyelitis treatment in a rat model system. J Ortho Res. 1993;11(2):256–262. doi: 10.1002/jor.1100110213. [DOI] [PubMed] [Google Scholar]
- 7.Llowe DW, Hansen ST. Immediate nailing of open fractures of the femoral shaft. J Bone Joint Surg. (A) 1988;70:812–819. [PubMed] [Google Scholar]
- 8.Klemm KW. Antibiotic bead chains. Clin Orthop. 1993;295:63–76. [PubMed] [Google Scholar]
- 9.Rosen H. Nonunion and Malunion. In: Browner BD, Levine AM, Jupiter JB, Trafton PG, editors. Skeletal Trauma. 2. Vol. 1. Philadelphia: WB Saunders Co; 1998. pp. 631–633. [Google Scholar]
- 10.Rosen HR, Marczell AP, Czerwanka E, Stierer MO, Spoula H, Wasl H. Local gentamicin application for perineal wound healing following abdomino-perineal recutum excision. Am J Surg. 1991;162:438–441. doi: 10.1016/0002-9610(91)90256-d. [DOI] [PubMed] [Google Scholar]
- 11.Seligson D, Popham J, Voos K, Henry SL, Paguri M. Antibiotic leaching from polymethylmethacrylate beads. J Bone Joint Surg. (A) 1993;75(5):714–720. doi: 10.2106/00004623-199305000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Von Faunhofer JA, Polk HC, Jr, Seligson D. Leaching of tobramycin from PMMA bone cement beads. J Biomed Mater Res. 1985;19:751–756. doi: 10.1002/jbm.820190703. [DOI] [PubMed] [Google Scholar]
- 13.Wahlig H, Dingeldein E, Bergmann R, Reuss K. The release of gentamicin from polymethylmethacrylate beads. J Bone Joint Surg. (B) 1978;60:270–275. doi: 10.1302/0301-620X.60B2.659478. [DOI] [PubMed] [Google Scholar]
- 14.Walenkamp GHIM. Gentamicin-PMMA beads. A clinical, pharmacokinetic and toxicological study. Darmstadt, FR Germany: E Merck; 1983. [Google Scholar]