Abstract
We describe a method of dynamic assessment of patellar tracking intraoperatively during a Fulkerson osteotomy. We utilize an electrically conductive catheter intraopertively to directly stimulate the femoral nerve to cause quadriceps muscle contraction. The resultant active knee extension allows dynamic assessment of patellofemoral tracking prior to and after final Fulkerson fixation. This dynamic intraopertive technique allows us to approximate in vivo patellofemoral motion better than with passive motion assessment.
INTRODUCTION
Symptomatic recurrent patellofemoral instability that does not respond to conservative measures is often relieved by surgical intervention. While there may be numerous underlying factors that lead to clinical patellofemoral dislocation and subluxation episodes, the most common is a malalignment of the quadriceps based extensor mechanism of the thigh. Because of the slight skeletal valgus that normally exists at the knee and the slightly lateral based attachment of the patellar tendon on the tibial tubercle, there is tendency for the normal patella to displace laterally. This tendency is balanced passively by the medial patellofemoral ligaments and by the buttress effect of the lateral femoral trochlea.6 From a dynamic standpoint, it is the orientation of the distal vastus medialis portion of the quadriceps muscle that provides a medial restraint during patellar tracking. When instability episodes occur, there is a net resultant disequilibrium causing the patella to be pulled laterally out of the trochlear groove on the femur. The variety of combinations of anatomic factors contributing to patellofemoral instability necessitates that treatments are tailored specifically to the individual patient.
As a general rule, a medial transfer of the tibial tubercle with or without lateral retinacular release is the most commonly employed treatment for the unstable lateral tracking patella. Surgical procedures used include release of tight lateral structures, tightening or advancement of lax medial structures, transposition of the patellar tendon insertion, and, more rarely, derotational osteotomies and trochleoplasty. Although the senior author (J.P.A) has employed numerous techniques described for tibial tubercle osteotomy and transposition (e.g., the Hauser distal and medial transfer, the Elmslie–Trillat medialization, the Southwick sliding dovetail medialization),2,4,5 we currently use the Fulkerson osteotomy,3 which moves the tubercle into a more anterior and medial position.
Passive Intraoperative Assessment
Regardless of the technical aspects of the procedure, the intraoperative determination of the amount of medialization that is needed to produce a stable patella traditionally depends upon passive intraoperative methods of assessment. The surgeon's clinical judgment is relied upon to determine the distance that the patellar tendon attachment must be moved to allow the patella to track centrally in the femoral groove. A number of passive mechanical flexions of the knee are conducted during the operation and the tuberosity is moved a certain distance so that the surgeon is convinced that regardless of the position of the knee, the patella will remain stable within the trochlear groove.
First, with the leg in full extension, the patella is laterally displaced manually as passive knee flexion is initiated with the coupled forces of external rotation and valgus applied to the knee. Lateral subluxation is considered to be gross evidence of undercorrection. Conversely, over correction is assessed by displacing the patella medially with the knee extended, then flexing the knee and applying the opposite forces of varus and internal rotation. Gross medial displacement with this maneuver suggests overcorrection.
Unfortunately, regardless of the type of medialization procedure employed, over- and undercorrection must be avoided. It is felt that the intraoperative assessment of the appropriate amount of medialization of the tubercle remains a notable shortcoming because the anesthetized patient is unable to produce the complicated dynamic forces generated by the quadriceps.
Our technique reported here attempts to recreate those dynamic forces to allow an intraoperative assessment of approximate dynamic patellofemoral tracking. The concept that this was possible emanated from the popularization of the femoral nerve block anesthesia and the particular nerve stimulator technique employed to localize the nerve introduced by one of us (A.B.).
METHODOLOGY
Preoperative Technique
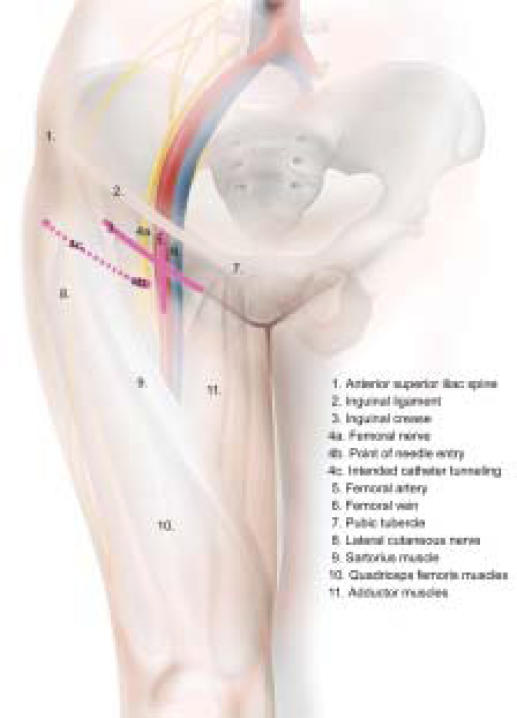
The patient has a "stimulating" femoral catheter placed in the supine position with the operative leg in the neutral position (neither externally nor internally rotated). The inguinal crease and femoral artery are identified and marked, and needle entry is one cm below the inguinal crease, and one cm lateral to the patient's femoral artery (Figure 1). Using sterile technique, local anesthetic is administered to the skin and subcutaneous tissue at the point of needle entry and the area of planned catheter tunneling. A nerve stimulator is attached to a 17-guage insulated Tuohy needle (StimuCath, Arrow International, Reading PA), and the needle is advanced in a postero-caudad direction at a 45-degree angle with the skin. The fascia lata and fascia iliaca are penetrated and a motor response is elicited of the quadriceps muscles. The current of the nerve stimulator is initially set to a current output of 1 mA, a frequency of 2 Hertz and a pulse width of 100–300 µs. Once a motor response is elicited, the stimulator is turned down and the needle position is adjusted until brisk twitches of the quadriceps muscles are still present at an output of 0.3–0.5 mA. The stimulating catheter (StimuCath, Arrow International, Reading PA) is threaded through the needle as it is held steady to maintain quadriceps stimulation. The catheter is threaded 5–10 cm past the needle tip and along the femoral nerve in a cephalad direction. Because the nerve stimulation is now via the stimulating catheter, the quadriceps twitches should remain unchanged throughout catheter advancement. It is possible to advance the catheter too far, under which circumstance the adductors of the thigh will twitch due to stimulation of the obturator nerve. The catheter would then be withdrawn slightly.
Figure 1.
Schematic of needle localization for placement of femoral nerve stimulator.
After placement, the catheter is tunneled subcutaneously for approximately 8–10 cm to secure position of the catheter during surgery. The same catheter can be used postoperatively to provide analgesia by way of a continuous femoral nerve block, though no local anesthetic agent is injected through the catheter until the operation is nearly complete.
The electrical nerve stimulator is now clipped to the catheter. After induction of general anesthesia or spinal anesthesia, but before surgery, the nerve stimulator is set to a frequency of 50 Hertz and the current is increased incrementally until the correct motor response in the quadriceps muscle is elicited. The motor response is less active if the nerve stimulator leads are changed from the usual, so the negative lead (the anode) is grounded on the patient and the positive lead (the cathode) is attached to the catheter. Careful testing and recording of the nerve stimulator settings are made, keeping in mind that a slightly higher current output would most likely be required after a tourniquet has been applied and after muscle fatigue following repeated muscle contractions.
Intraoperative Technique
Prior to the Fulkerson tibial tubercle medialization, a preliminary assessment of the dynamic tracking of the patella is made by femoral nerve stimulation. The intensity of the stimulus is refined to the point that a physiologic speed and force of quadriceps contraction is approximated. Since it is common that the J-sign is the most obvious indicator of dynamic maltracking, the knee is then supported at 10-20∞ flexion in order to observe the extrinsically induced J-sign as the knee is actively extended by the femoral nerve activated quadriceps muscle contraction. Comparisons are made to the preoperative tracking characteristics of the patella.
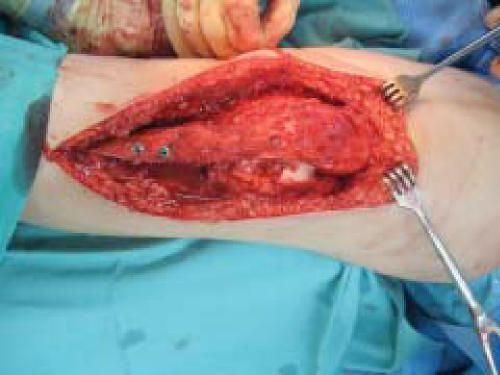
After stimulation, a medial parapatellar arthrotomy is made through a medial parapatellar skin incision. The tibial tubercle is exposed and an osteotomy is made from superficial medial to deep lateral, allowing for an anterior and medial slide. A dovetail joint is cut proximally and a periosteal hinge is left distally. Passive assessments are made of patellofemoral tracking as described above. After the tubercle is appropriately positioned, it is provisionally fixed with K-wires. The knee is then supported at 10-20° flexion in order to observe the J-sign as the knee is again actively extended. At this point, the femoral nerve stimulator is utilized to attempt to recreate the forceful contraction of the quadriceps muscles (Figures 2 & 3). Slightly higher nerve stimulator output currents may be required at this stage to achieve the desired effect. The effect of the quadriceps muscle contraction at varying levels of force is then observed and the position of the tubercle altered accordingly.
Figure 2.
Patellar position just prior to quadriceps stimulation.
Figure 3.
Quadriceps stimulated with central patellar tracking.
DISCUSSION
We have found this technique useful. In one case, the information from the dynamic assessment resulted in us shifting the tubercle further laterally than we would have otherwise done, because we feared subsequent medial instability. In two other cases, the tubercle was shifted more medially because the force of the quad was insufficient to normalize the lateral maltracking.
Prior to the institution of this novel technique of dynamic assessment, we had two patients who developed medial patellar instability around one year post operatively. We feel this phenomenon may have been due to the fact that their quadriceps strength continued to improve after surgery and eventually the stronger VMO pulled the patella medially. It is uncertain that intraoperative femoral nerve stimulation would have changed the outcome, but it remains a possibility.
In terms of problems utilizing this technique, we have had one patient whose quadriceps contracted forcefully enough to dislodge the fixation intraoperatively. In this instance, the distal bone bridge had been inadvertently disrupted. Interestingly, the two screw, bi-cortical fixation was simply felt to have been inadequate to prevent this pullout. This does raise the concern that provisional or final fixation must be secure prior to a dynamic assessment of quadriceps function than it would otherwise need to be during passive assessment. Assurance against detachment of the transferred tibial tubercle is maximized by several maneuvers: 1) maintenance of a sturdy bone bridge distally; 2) creating a dovetail undercut of the proximal part of the osteotomy that locks the transferred tubercle under the proximal tibial cortex; 3) temporary fixation of the bone block with pins; 4) active counter pressure with the surgeons thumb, compressing the bone block in its bed and; 5) determining the most effective level of electrical stimulus to avoid the more violent muscle contractions.
We are encouraged that the use of intra-operative femoral nerve stimulation may help address some of the problems of passive assessment of patellofemoral tracking and improve the success rate of patellofemoral realignment procedures. A similar technique has previously been described for intraoperative stimulation of the suprascapular nerve in rotator cuff repairs,1 but to our knowledge, no such technique has been described for intraoperative femoral nerve stimulation. We believe that utilization of the described technique for dynamic patellofemoral assessment helps more accurately realign the extensor mechanism intraoperatively. Further prospective analysis will be required to assess its long-term benefit in the outcome of patellofemoral realignment procedures.
References
- 1.Boezaart AP, de Beer JF, van Rooyen K. Rotator Cuff Tear: Intraoperative Electrical Stimulation of the Suprascapular Nerve. Arthroscopy. 2000;16(7) doi: 10.1053/jars.2000.16288. [DOI] [PubMed] [Google Scholar]
- 2.Cox JS. An evaluation of the Elmslie-Trillat procedure for management of the patellar dislocations and subluxations. Am J Sports Med. 1976;4:72. doi: 10.1177/036354657600400204. [DOI] [PubMed] [Google Scholar]
- 3.Fulkerson JP. Anteromedialization of the Tibial Tuberosity for Patellofemoral Malalignment. Clin Orthop. 1983;177:176–181. [PubMed] [Google Scholar]
- 4.Hauser ED. Total tendon transplant for slipping patella. Surg Gnecol Obstet. 1938;66:199. doi: 10.1097/01.blo.0000238831.50186.87. [DOI] [PubMed] [Google Scholar]
- 5.Southwick WO, Becker GE, Albright JA. Dovetail patellar tendon transfer for recurrent dislocating patella. JAMA. 1968;204:665. [PubMed] [Google Scholar]
- 6.Walsh MW. Recurrent Dislocation of the Knee in the Adult. In: DeLee JC, Drez D, editors. Orthopaedic Sports Medicine. 2nd ed. Philadelphia: Saunders; 2003. pp. 1710–1749. [Google Scholar]