Abstract
We report a patient who presented with three months of foot pain, lytic bone lesions in the foot, and a painless ipsilateral leg skin ulcer. Bone and skin biopsies revealed organisms compatible with Blastomyces. Systemic blastomycosis is rare, especially with bone involvement in the foot.
CASE REPORT
The patient is a 27-year-old woman who presented to our foot outpatient clinic with three months of worsening right midfoot pain, worst with weight-bearing. Non-steroidal anti-inflammatory agents and tramadol did not help. There was no history of trauma. A few weeks after the foot pain onset, she also noticed a quarter-sized painful nodular skin lesion in the popliteal fossa that subsequently started to drain clear fluid.
Several weeks before the foot pain onset, she was diagnosed with a "pneumonia" for which she was treated locally as an outpatient with two weeks of amoxicillin, with resolution of her respiratory symptoms. A microbiologic diagnosis was not attempted. Past medical history was otherwise significant for depression and childhood asthma. She had no fevers, chills, weight loss or change in appetite. She was a 1.5 pack-per-day smoker for 15 years. She denied a history of sexually transmitted diseases, cancer, immunocompromise, drug abuse or frequent or recurrent infections. She had multiple tooth caries in the past, with multiple extractions. She lived in a farm house. She had a monogamous partner. She was not pregnant.
On examination, she was obese, in no acute distress, and with normal vital signs. Lung examination revealed clear breath sounds. Left foot examination revealed exquisite tenderness throughout the medial midfoot. She could not tolerate any midfoot passive or active motion due to pain. The skin was normal in the foot with minimal swelling. A left popliteal fossa examination revealed a 4 x 2 cm beefy red granulomatous plaque with mild creamy exudate (Figure 1). There was no inguinal or popliteal adenopathy.
Figure 1.
Left leg popliteal fossa skin plaque (top), and closeup (bottom).
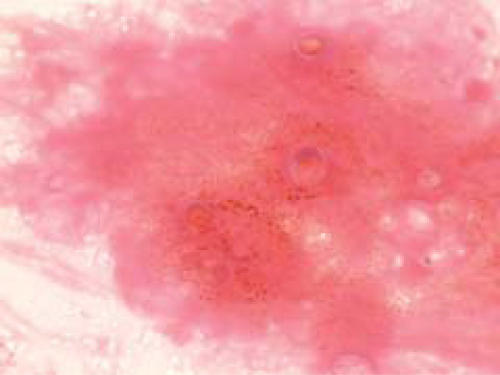
Plain radiographs (Figure 2) of the foot, performed at an outside institution two months prior to her evaluation at our clinic, were normal. MRI (Figure 3) at that time revealed signal changes throughout the navicular bone with surrounding edema in the soft tissue. The MRI would have been consistent with possible infection, malignancy, stress fracture, or avascular necrosis of the navicular.
Figure 2.

Normal foot lateral radiograph one month after onset of pain.
Figure 3.
Sagittal MRI one month after onset of pain, revealing diffuse signal change in navicular with associated soft tissue edema.
At our evaluation, plain radiographs revealed a proximal navicular well-demarcated cyst that had eroded into the talonavicular joint (Figure 4). There was osteopenia throughout the foot. Foot computerized tomography (CT) scan revealed multiple lytic lesions throughout the foot, and a large focal cyst of the proximal navicular with intra-articular involvement (Figure 5).
Figure 4.
Lateral foot radiograph at presentation in our clinic, three months after onset of pain, revealing destructive lytic lesion in proximal navicular.
Figure 5.


CT scans revealing diffuse foot and ankle lytic lesions with the largest erosive lesion in the proximal navicular on coronal and sagittal images.
Laboratory data revealed a CRP of 2.0 (normal < 0.5), an ESR of 30, and a normal CBC.
The most likely etiology on our differential was chronic multi-focal infectious process, more likely of fungal or tubercular etiology, rather than bacterial etiology.
She underwent small open incisional biopsy of the navicular bone. The navicular cyst was filled with white gelatinous material; cultures and pathology were obtained. Cultures were also obtained from the talonavicular joint synovial fluid. Intraoperative frozen pathology revealed granulomatous chronic and acute inflammation. The wound was irrigated and closed. She was casted and remained non-weight-bearing.
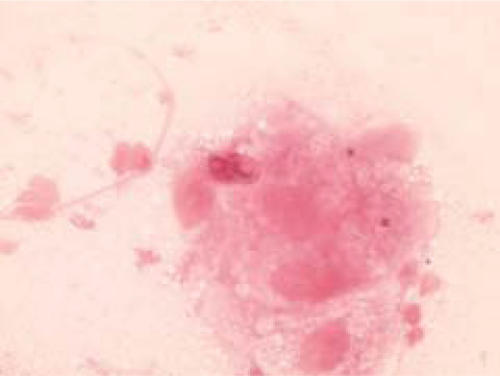
Blastomyces dermatitidis (Figure 6) was seen on gram stain and Calcoflor stain, and later grew from cultures of the navicular cyst material, and the talonavicular synovial fluid. Histology of bone revealed abundant acute inflammatory cells with multiple necrotizing granulomas, and spherical yeast forms were present with thick walls and broad-based budding, compatible with Blastomyces.
Figure 6.
Microscopic blastomycosis from foot navicular biopsy: spherical yeast forms with budding apparent.
Further workup included a chest radiograph showing right upper-lobe linear opacities, and a chest CT with right upper-lobe scarring. Pathology of the left leg skin popliteal lesion shave specimens revealed chronic suppurative inflammatory infiltrate with giant cells, scattered plasma cells, and scattered broad-based budding yeast forms, again compatible with Blastomyces. Peripheral blood immunopathology revealed normal T-lymphocytes and B-lymphocytes. Electrolytes and liver enzymes were normal. HIV testing was negative.
Clinical diagnosis was North American blastomycosis involving lung, bone, and skin. She most likely had respiratory inoculation resulting in the pneumonia that was diagnosed prior to the onset of foot pain, with subsequent hematogenous involvement of bone and skin. Primary bone or skin inoculations are not likely. Treatment with oral itraconazole was initiated at 200 milligrams orally, twice daily.
DISCUSSION
Blastomyces dermatitidis is a dimorphic fungus. In its natural soil habitat, it exists as a mold in multi-cellular colonies composed of branching hyphae. The mold releases spores (conidia) into the air. At body temperature, the fungus grows in a yeast unicellular form, appearing spherical or elliptical, and reproduces by budding. The yeast cell has a thick refractile cell wall. Pulmonary infection occurs after the spores are inhaled. The respiratory infection could be asymptomatic, or result in self-limited acute pneumonia, or chronic pneumonia. Systemic involvement infrequently occurs overall, but when it does, it can manifest in any organ, most commonly the bone and joints, skin and central nervous system. In North America, Blastomyces is endemic in Southeastern and Southcentral states, especially those bordering the Mississippi and Ohio river basins.
Our patient demonstrated several uncommon manifestations of this infection. She had multi-organ involvement: lung, skin, and bone. A large series of 326 blastomycosis cases revealed that a single organ was involved in 82.8% of cases (lung 91.4%; skin 18.1%; bone 4.3%; genitourinary 1.8%; nervous system 1.8%).1 Bone involvement has been reported in the literature from 19502 to recently.3 However, bone involvement in many cases has been at the distal ends of long bones.3 It is unusual for foot involvement to occur, as in this patient.
The pneumonia that occurred prior to her foot symptoms likely represented blastomycosis, resulting from pulmonary inoculation. Her pulmonary symptoms were self-limited. However, the chest CT showing chronic scarring could be compatible with chronic pulmonary infection. She then likely proceeded to disseminate to involve the skin and bones of the foot. Eventually, diagnosis required pathology examination of the foot navicular cyst. The skin lesion was not appreciated initially to be fungal, nor was it related to the foot bone lesion, but its realization may have initially made us more suspicious for Bastomycosis.
The diagnosis of skeletal blastomycosis is frequently delayed. In our patient, she had three months of symptoms before a bone biopsy was obtained. This is similar to the reported literature, where diagnosis of blastomycosis is delayed due to low suspicion, and greater consideration given to malignancy or tuberculosis. In a study from the University of Mississippi, only 18% of 123 patients with blastomycosis were correctly diagnosed early.4 In our patient, once the bone diagnosis was made, the skin lesion was confirmed to be fungal.
The plan for therapy of this patient will involve oral itraconazole for at least one year. Amphotericin B is only indicated in cases of either life-threatening disease, or central nervous system involvement.5
References
- 1.Chapman SW, Lin AC, Hendricks KA, Nolan RL, Currier MM, Morris KR, Turner HR. Endemic blastomycosis in Mississippi: epidemiological and clinical studies. Semin Respir Infect. 1997 Sep;12(3):219–228. [PubMed] [Google Scholar]
- 2.Alfred KS, Harbin M. Blastomycosis of bone; report of a case. J Bone Joint Surg. (Am) 1950 Oct;32(A:4):887–889. [PubMed] [Google Scholar]
- 3.Saiz P, Gitelis S, Virkus W, Piasecki P, Bengana C, Templeton A. Blastomycosis of long bones. Clin Orthop Relat Res. 2004 Apr;421:255–259. doi: 10.1097/01.blo.0000126305.87452.82. [DOI] [PubMed] [Google Scholar]
- 4.Lemos LB, Guo M, Baglia M. Blastomycosis: organ involvement and etiologic diagnosis. A review of 123 patients from Mississippi. Ann Diagn Pathol. 2000 Dec;4(6):391–406. doi: 10.1053/adpa.2000.20755. [DOI] [PubMed] [Google Scholar]
- 5.Chapman SW, Bradsher RW, Jr, Campbell GD., Jr Practice guidelines for the management of patients with blastomycosis. Clin Inf Dis. 2000;30:679–683. doi: 10.1086/313750. [DOI] [PubMed] [Google Scholar]