Abstract
Salvage of diffuse ankle osteomyelitis, especially in compromised hosts, is a challenging problem. The purpose of this report was to evaluate early complications and results using a standardized salvage protocol. Eight patients with diffuse ankle osteomyelitis were treated by resection of all infected tissue and hybrid-frame compression arthrodesis. At presentation, five had open wounds. According to the Cierny/Mader classification, all had diffuse anatomic involvement and six of eight were compromised hosts. Seven had central distal tibial column involvement and one had primarily talar involvement. Surgical technique involved a two-incision approach, removal of all infected material and application of a compression circumferential frame with five thin wires across the foot, two across the tibia and two half-pins in the tibia. Fusion of eight ankles and four subtalar joints was attempted. All patients received six weeks of intravenous antibiotics. Open wounds were treated with wound vacuum assisted closure (VACs) devices until closure was achieved. Frames were removed at three months and walking casts were applied for one to two more months. Ankle sepsis was eradicated in all patients. Seven of eight ankles fused at an average of 13.5 weeks (range, 10 to 16 weeks). One limb required below-knee amputation (BKA) at five weeks due to nonreconstructible vascular insufficiency. Three of four subtalar joints fused. Fixation problems included two pin-track infections cleared with oral cephalexin and one broken half-pin. Two diabetic Charcot patients required long-term ankle-foot orthosis (AFO) use due to subtalar instability. At average 3.4-year follow-up, none of the seven fused ankles has required further surgery. Use of this standardized salvage treatment protocol for these difficult problems in selected patients was effective with a relatively low associated complication rate.
INTRODUCTION
Salvage of diffuse ankle osteomyelitis, especially in compromised hosts, is a challenging problem. Although transtibial-level amputation is a treatment option, many patients would like to preserve their limb. Options for salvage surgery are several, and most involve multiple surgeries and long term treatment.3,6,10,11,13,15 The author has used a protocol utilizing some well-described techniques including complete debridement of all infected or involved tissue,11 application of a modified Ilizarov compression frame,8,9 use of vacuum-assisted wound closure7 and intravenous antibiotics. The purpose of this report is to evaluate early complications and results using a standardized salvage protocol in a selected case series.
METHODS
Between 2000 and 2002, medical records and radiographs of patients with diffuse ankle infection treated by single-stage debridement/arthrodesis were reviewed under an IRB-approved protocol. Data collected included age, gender, major co-morbidities, previous treatment, presence of open wounds, location of osteomyelitis, microbiological data, adjunct procedures and outcome from surgery. All patients were given informed consent preoperatively and understood that the surgical treatment choices were either a transtibial-level amputation or an attempted resection/arthrodesis. They were further informed of the projected period of major convalescence with each (average six weeks for amputation versus six months for resection/arthrodesis salvage) and the higher predictability of results with amputation. Patients were followed until ultimate resolution of the presenting problem.
Surgical Technique
The ankle was approached with medial and lateral J-type incisions, which are longitudinal across the malleoli and horizontal in the hindfoot. A transfibular approach to the ankle was used and the lateral malleolus was removed. If the medial malleolus was not involved, it was left intact, otherwise, it was removed. All hardware, infected bone and soft tissue were removed. The incisions were extended up the calf as needed to completely expose and debride the infection. After the wounds were completely irrigated and debrided, the ankle and subtalar joints were placed in the optimal position for fusion and two temporary smooth Steinmann pins were driven through the heel across the hindfoot into the tibia.
We applied a pre-built circular fixation frame. Three tensioned 1.8 mm wires were placed in the hindfoot. If the talus was preserved and the subtalar joint was not included in the fusion, one of these wires was placed across the talus and two were placed through the calcaneus. Two more wires were tensioned across the metatarsals. The tibia was fixated at two levels with circular rings. At each level, a tensioned thin wire and halfpin were used. The sole of the foot was placed perpendicular to the anterior crest of the tibia, with the foot externally rotated five degrees more than the opposite side. Open wounds were left open; all surgical wounds were closed in one layer with monofilament.
Postoperative Care
Open wounds were treated with vacuum assisted closure (Kinetic Concepts, Inc, San Antonio, TX) until complete epithelialization. Pin care involved removing bandages on the second day after surgery and removing heavy crusts around the half-pins with a cotton-tipped applicator. Daily showering and towel-pad drying were encouraged. Intravenous antibiotics were used for six weeks. Frames were removed around three to four months and a plaster below-knee cast was applied. Weight bearing was permitted after radiographic fusion was apparent. Casts were removed one month after apparent radiographic fusion, and patients were progressed to a removable walker and then to a shoe in another month. Patients with continued instability of the hindfoot were placed in an ankle-foot orthosis. Followup was a minimum of two years.
RESULTS
Eight patients were identified who underwent treatment of diffuse ankle osteomyelitis with this protocol during the study period. Mean age was 58.3 years (range, 51 to 72 years); three were female and five were male. Five had open wounds. Five patients had diabetes mellitus. One had rheumatoid arthritis and a history of chronic steroid use. According to the Cierny/ Mader staging system of osteomyelitis, all had type IV (diffuse permeative lesions), and six of eight were considered type B, "systemically compromised" hosts.6 Therefore, the clinical staging of this group of patients was six type IV-B, and two type IV-A. Localizing the osteomyelitis by structural column6 revealed seven patients had central column destruction, four had additional medial column involvement, four had additional lateral column involvement and one had an infected, collapsed, necrotic talus.
Most patients had had previous surgery. One patient had two attempts at an open reduction/internal fixation (ORIF) of an ankle fracture, one had talar fracture ORIF, one had an attempted ankle fusion, and one had an infected total ankle replacement component removal. Two previous soft tissue flaps failed on a single patient, and two patients had previous incision and drainage procedures. At presentation to our center, two patients had completed a six-week course of intravenous antibiotics, two had been treated over six weeks on oral antibiotics, and four were not pretreated with antibiotics.
At surgery, intraoperative specimens were sent for culture and sensitivity on all ankles. Five grew out Staphylococcus aureus, one grew out Morganella morganii and two did not grow out an organism. All patients were treated with culture-specific intravenous antibiotics, and the two patients with no identifiable organisms were treated with a first-generation cephalasporin (Cefazolin).
In these eight patients, compression arthrodesis of eight ankles and four subtalar joints was attempted. One patient required a below-knee amputation for non-reconstructible vascular insufficiency five weeks after surgery. Fixation problems included two pin track infections successfully treated with oral Cephalexin for ten days, and one broken half-pin that was treated by removing the external portion of the pin, leaving the internal portion within the tibia.
Frames were removed at an average of 12.7 weeks (range, 10 to 16 weeks). Cast or boot immobilization was used for an average of 6.9 weeks (range, 4 to 10 weeks). Seven of eight ankles radiographically fused at an average of 13.5 weeks (range, 10 to 16 weeks) (Figure 1), while the other limb required transtibial amputation at five weeks due to non-reconstructible vascular insufficiency. Three of four subtalar joints fused in the same time frame. Two diabetic Charcot patients required long-term AFO use due to clinical subtalar joint instability (Figure 2); neither had pain. No patient complained of problems with limb shortening. At average 3.4 years follow-up, none of the seven fused ankles have required further surgery.
Figure 1.
AP (a) and lateral (b) radiographs of massively swollen (closed) ankle of a 54-year-old type II diabetic male. He had received six weeks of IV nafcillin. According to the Cierny/Mader classification, he has diffuse involvement (IV) and is a systemically compromised host (B). The central and lateral columns are involved. He was treated with debridement of all infected tissue, removal of joint cartilage from the ankle and subtalar joints, and (c, d) modified Ilizarov external fixation. AP (e) and lateral (f) radiographs at two years show solid fusion of both joints.
Figure 1A.

Figure 1B.

Figure 1C.
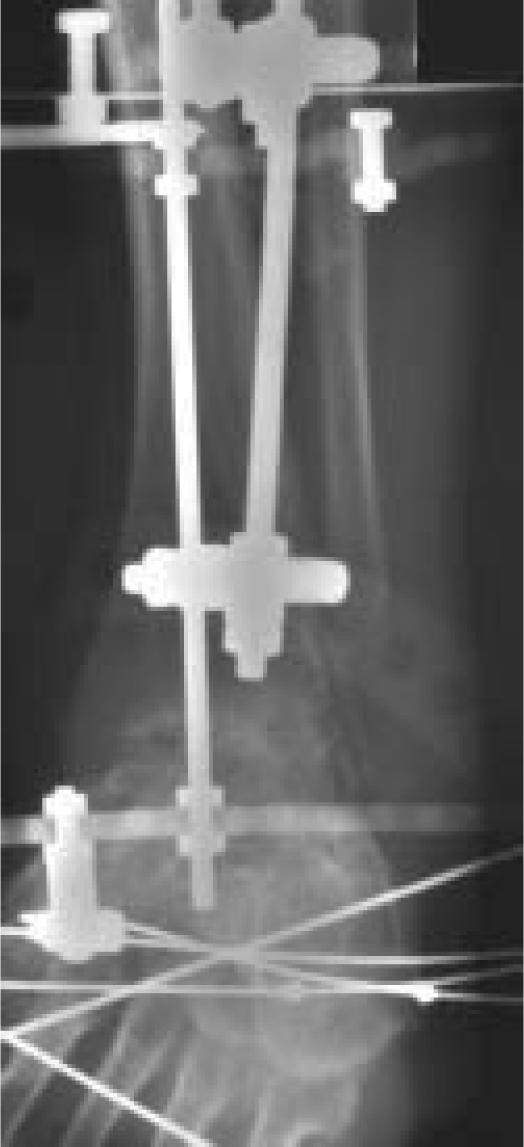
Figure 1D.

Figure 1E.

Figure 1F.

Figure 2.
AP (a) and lateral (b) radiographs of swollen (closed) ankle of a 59-year-old type I diabetic female. She had two previous open reduction and internal fixations of her ankle complicated by Staphylococcus aureus infection. She had received seven weeks of intravenous vancomycin and was advised to have an amputation. She was treated with debridement of all infected tissue, removal of hardware and joint cartilage from the ankle and subtalar joints, and circular ring compressive fixation. At two years (c, d), she has a solid ankle fusion, but requires AFO use for coronal plane subtalar joint instability.
Figure 2A.

Figure 2B.

Figure 2C.

Figure 2D.

DISCUSSION
This retrospective case study series shows promise with the use of a simple single-stage protocol for treatment of diffuse ankle osteomyelitis in mostly compromised hosts. The approach requires meticulous care with debridement and frame application. The results reveal a high rate of limb salvage. The key elements are 1) complete resection of all infected tissue, 2) application of a circular frame with pins and wires out of the zone of infection, 3) using only tensioned thin wires in the foot, 4) six weeks of intravenous antibiotics post-operatively, and 5) use of a wound VAC to close all open wounds. With this strategy, we had a high success rate despite the poor condition of the ankles and the systemically debilitated state of six out of eight of our patients.
Cierny et al. developed important concepts for classifying ankle sepsis and reported their results in 36 patients.6 They presented two important concepts: 1) the concept of a biological classification of adult osteomyelitis, and 2) the concept of an anatomical classification of three columns of the distal tibia and ankle. The first is a generic system intended to give clinical information on prognosis and treatment. This system has been widely adopted for use to describe the results of treatment throughout the musculoskeletal system. Stage IV (diffuse) lesions fare the most poorly, especially in systemically compromised hosts (B). The second system is an anatomical classification used by Cierny et al. to guide fixation strategies.
In the present series, all eight patients had diffuse osteomyelitis: Six were systemically compromised hosts, seven had central tibial column loss, and the other had complete talar body collapse. In the original series of 36 patients studied by Cierny et. al., using aggressive reconstructive techniques for that time period, the limb salvage rate was 74 percent.6 Patients with substantial central column involvement were treated with staged reconstruction involving antibiotic bead placement, multiple bone graftings and liberal use of free muscle transfers. They reported a rate of 86 percent with major complications. All of their treatment failures occurred in type B hosts. In that series, of the 12 non-amputated ankles classified as Cierny/Mader stage IV-B, the average number of procedures per patient was 4.9, eventually eradicating infection in 83 percent and attaining union in 92 percent.6
Several different salvage strategies have been used for limited numbers of patients with these challenging problems.1,2,6,10,11,13,15 Before the Cierny/Mader classification system was developed, Lortat-Jacob et al. reported successful fusions in 18 of 24 (75 percent) ankles with external fixation and multiple Papineau graftings.11 Thordarson et al. reported their center's experience with staged reconstruction of five patients with distal tibial osteomyelitis with open wounds. The treatment protocol involved staged debridements, soft tissue transfers, unilateral external fixation and a six-week course of intravenous antibiotics. These authors had a high rate of salvage and infection eradication.15 Richter et al. reported the results of 45 ankle and/or subtalar infections treated by debridements, a combination of internal and simultaneous large-pin external fixation, and selective iliac crest grafting.13 Their patients required an average of 2.8 surgical procedures until fusion. Solid fusion was achieved in 39 of 45 patients with this protocol, six requiring further pin track surgery for continuous infectious drainage. Their cohort of patients was different from that in our present study, as only five of 45 patients in their study had diabetes mellitus. The complication rates were higher in their patients with systemic comorbidities.
Kollig et al. presented a series similar to our present study.10 In their series of 15 patients with septic ankles, 12 were treated with hybrid external fixation and three with a combination of external fixation and internal screw fixation. Open wounds were treated with dressing changes, and skin grafting as needed. Tensioned thin wires were used in the foot and distal tibia. Systemic comorbidities were present in six of 15 patients, and one other was noted to have "mental illness." In Kollig's series, one patient required revision ankle arthrodesis, and two required extension of fusion to the subtalar joint. Fourteen of 15 (93 percent) of ankles ultimately fused, but three patients had a persistently draining fistula.10
Our present study follows the lead of past studies in defining a protocol to treat these challenging problems. The importance of a complete debridement of all devitalized and potentially infected tissue was emphasized by other authors.2,4–6,10–15 In the present series, a simple circular frame was used. This frame's basic features were described by Johnson et al.,9 and has a relatively low incidence of hardware failure or bone cut-out, even in debilitated patients. The addition of a wound VAC has substantially improved our ability to obtain secondary closure without the need for free tissue transfer or skin grafting, and appears to hasten closure, thereby reducing the incidence of persistently draining sinuses.
Even with a complex practice in a tertiary center, these cases are relatively rare. Patients with life-threatening limb infections or clear-cut non-reconstructible vascular insufficiency are directly treated with an amputation and are not given the option of limb salvage by this protocol. Others have limb-threatening infections with adequate vascularity, and are possible candidates for limb salvage. When I give informed consent for this procedure, I tell the patient that a transtibial-level amputation will likely restore ambulatory function more quickly and reliably. Some patients decide to have an amputation. They are usually systemically debilitated from infection, have undergone multiple previous surgeries, need or want to get back to work sooner, and financially cannot risk possible failure of the salvage protocol. Therefore, a major limitation of this study relates to the retrospective design. I have not specifically kept records of how many patients were possible candidates, but decided to have an amputation of their limb rather than undergoing an attempted salvage ankle fusion/ reconstruction with this protocol. Undoubtedly, there was inherent selection bias as patients who were unwilling or unable to consider extensive salvage surgery are likely different from those willing to have the surgery.
Another limitation relates to antibiotic coverage. All patients were given a six-week course of intravenous antibiotics after surgery. Swiontkowski et al. showed that a shorter course of intravenous antibiotics followed by culture-specific antibiotics is effectively equivalent to a six-week course of intravenous antibiotics in the treatment of chronic osteomyelitis.14 In that series, however, local antibiotic-impregnated polymethylmethacrylate bead treatment and soft tissue transfers were used liberally, and these two techniques were not used in our present series. In the present series, a six-week course of intravenous antibiotic therapy may not always have been necessary to eradicate infection. Further study of the optimal time-course and route of antibiotic treatment is clearly needed.
In conclusion, patients with severe, diffuse peri-ankle osteomyelitis may be treated effectively with a single-stage resection and circumferential frame compression arthrodesis. The tensioned thin wires in the foot confer good mechanical stability and are associated with low infection rates. The use of a wound VAC for open wounds may have been one major reason there were no persistent sinuses or need for soft tissue transfer/ grafting surgeries. The author believes this is a reasonable alternative to below-knee amputation in selected patients.
References
- 1.Anderson JG, Coetzee JC, Hansen ST. Revision ankle fusion using internal compression arthrodesis with screw fixation. Foot Ankle Int. 1997;18(5):300–309. doi: 10.1177/107110079701800511. [DOI] [PubMed] [Google Scholar]
- 2.Bibbo C, Lee S, Anderson RB, Davis WH. Limb salvage: the infected retrograde tibiotalocalcaneal intramedullary nail. Foot Ankle Int. 2003;24(5):420–5. doi: 10.1177/107110070302400508. [DOI] [PubMed] [Google Scholar]
- 3.Bishop AT, Wood MB, Sheetz KK. Arthrodesis of the ankle with a free vascularized autogenous bone graft. Reconstruction of segmental loss of bone secondary to osteomyelitis, tumor, or trauma. J Bone Joint Surg. (Am) 1995;77(12):1867–1875. doi: 10.2106/00004623-199512000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Chan YS, Ueng SW, Wang CJ, Lee SS, Chen CY, Shin CH. Antibiotic-impregnated autogenic cancellous bone grafting is an effective and safe method for the management of small infected tibial defects: a comparison study. J Trauma. 2000;48(2):246–255. doi: 10.1097/00005373-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Cierny G., III Infected tibial nonunions (1981- 1995). The evolution of change. Clin Orthop. 1999. pp. 97–105. [DOI] [PubMed]
- 6.Cierny G, III, Cook WG, Mader JT. Ankle arthrodesis in the presence of ongoing sepsis. Indications, methods, and results. Orthop Clin North Am. 1989;20(4):709–721. [PubMed] [Google Scholar]
- 7.Clare MP, Fitzgibbons TC, McMullen ST, Stice RC, Hayes DF, Henkel L. Experience with the vacuum assisted closure negative pressure technique in the treatment of non-healing diabetic and dysvascular wounds. Foot Ankle Int. 2002;23(10):896–901. doi: 10.1177/107110070202301002. [DOI] [PubMed] [Google Scholar]
- 8.Hawkins BJ, Langerman RJ, Anger DM, Calhoun JH. The Ilizarov technique in ankle fusion. Clin Orthop. 1994. pp. 217–225. [PubMed]
- 9.Johnson EE, Weltmer J, Lian GJ, Cracchiolo A., III Ilizarov ankle arthrodesis. Clin Orthop. 1992. pp. 160–9. [PubMed]
- 10.Kollig E, Esenwein SA, Muhr G, Kutscha-Lissberg F. Fusion of the septic ankle: experience with 15 cases using hybrid external fixation. J Trauma. 2003;55(4):685–691. doi: 10.1097/01.TA.0000051933.83342.E4. [DOI] [PubMed] [Google Scholar]
- 11.Lortat-Jacob A, Beaufils P, Coignard S, Elahmadi J. [Tibiotarsal arthrodesis in a septic milieu]. Rev Chir Orthop Reparatrice Appar Mot. 1984;70(6):449–456. [PubMed] [Google Scholar]
- 12.Patzakis MJ, Greene N, Holtom P, Shepherd L, Bravos P, Sherman R. Culture results in open wound treatment with muscle transfer for tibial osteomyelitis. Clin Orthop. 1999. pp. 66–70. [DOI] [PubMed]
- 13.Richter D, Hahn MP, Laun RA, Ekkernkamp A, Muhr G, Ostermann PA. Arthrodesis of the infected ankle and subtalar joint: technique, indications, and results of 45 consecutive cases. J Trauma. 1999;47(6):1072–1078. doi: 10.1097/00005373-199912000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Swiontkowski MF, Hanel DP, Vedder NB, Schwappach JR. A comparison of shortand long-term intravenous antibiotic therapy in the postoperative management of adult osteomyelitis. J Bone Joint Surg. (Br) 1999;81(6):1046–1050. doi: 10.1302/0301-620x.81b6.9794. [DOI] [PubMed] [Google Scholar]
- 15.Thordarson DB, Patzakis MJ, Holtom P, Sherman R. Salvage of the septic ankle with concomitant tibial osteomyelitis. Foot Ankle Int. 1997;18(3):151–156. doi: 10.1177/107110079701800307. [DOI] [PubMed] [Google Scholar]


