In December 2006 the Government of Canada announced the coming into force of the new Quarantine Act.1 This new act modernizes legislation dating back to 1872. According to Dr. David Butler-Jones, Canada's Chief Public Health Officer, “the new Quarantine Act represents a huge step forward in … preparing for an influenza pandemic.”2
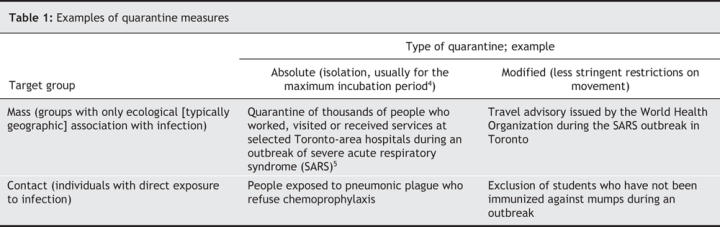
Quarantine, broadly defined, means the “restrictions placed on the entrance to and the exit from the place or premises where a case of communicable disease exists.”3 In practice, there is an important distinction between quarantine and case-specific measures. Quarantine describes the actions directed at healthy people thought to have been exposed to a communicable disease and who may be incubating the infection. Case-specific measures, including case isolation, are directed at people known or suspected, on clinical or laboratory grounds, to be actually infected. Quarantine targets the incubation period and case isolation targets the period of clinical illness. A quarantine matrix with examples is presented in Table 1.
Table 1
Quarantine is an ancient concept. It can be traced back to the efforts to control the Black Death in 14th century Italy. Initially, the period of detention was 30 days — the trentino. This was later modified to 40 days — the quarantino — perhaps because this matched the 40 days of Lent.6 Quarantine measures were “harsh and stupid” and were based on “gross ignorance” and “fear.”7 The unmarked graves on Grosse-Île in the St. Lawrence River bear stark witness to the folly of quarantine.
When I trained in public health, some 25 years ago, quarantine had fallen into disrepute because of the widespread perception that it did not work. The term quarantine came back into prominence in the mid-1980s to describe an (inappropriate) strategy for controlling the spread of HIV (really case isolation, not quarantine). In recent years, quarantine has become respectable again. This began in the context of post-9/11 concerns about bioterrorism, although it has never been clear against which bioterror threats quarantine would be useful. Mass quarantine gained further currency when it was adopted as a control strategy against severe acute respiratory syndrome (SARS) in 2003. Now, quarantine is re-entrenched in the mainstream of public health theory such that it is being proposed as a measure to fight pandemic influenza.
Quarantine has a very limited role in modern public health practice. The Control of Communicable Disease Manual4 provides an authoritative summary of control measures for more than 150 infectious diseases of public health concern. For the vast majority of these diseases, the manual dismisses quarantine with the curt phrase “not applicable” and recommends modified quarantine for only 6 diseases. For example, it recommends that children who have not been immunized against mumps be excluded from school during an outbreak. The manual recommends absolute quarantine in only 2 circumstances: people exposed to pneumonic plague who refuse chemoprophylaxis and people who are louse infested and have been exposed to typhus fever. The manual does not recommend any quarantine measures for influenza, smallpox or SARS, and it does not recommend mass quarantine for any disease in any circumstances.
For quarantine to be effective, 3 conditions must be met. First, the disease must be efficiently transmissible in its incubation period or very early in its symptomatic stage. Case isolation, not quarantine, is appropriate for diseases that are spread only during symptomatic illness. Quarantine will be ineffective for diseases that can be spread by people with only asymptomatic illness. Second, it must be possible and practical to identify all, or virtually all, people incubating the infection. Third, infected people must comply with the conditions of the quarantine.
Quarantine has substantial costs. These can include diversion of scarce resources, augmentation of public fears and intolerances, provocation of civil disobedience and infringement of human rights.8
Mass absolute quarantine was used as a control measure by public health authorities in the outbreak of SARS in Toronto in 2003. Quarantine was adopted early in the outbreak, when little was known about the disease, and was unnecessary because SARS was not highly infectious during its incubation period or its early symptomatic stage.9 SARS quarantine was ineffective because compliance was poor — no higher than 57%10 and possibly much lower. The costs, in terms of wasted resources and public anxiety and intolerance, were substantial. Travel advisories for SARS, a form of modified quarantine, were also unnecessary. SARS was, in fact, rapidly eradicated by effective isolation of cases in hospitals.11
The name Quarantine Act is misleading because the act actually addresses the use of both quarantine and case-specific measures at our international borders. The new legislation reflects the change of focus from marine travel to air travel. The act does not give emergency public health powers to the federal government within Canada, because constitutionally these responsibilities fall to the provincial governments.12
The Quarantine Act is administered by the Public Health Agency of Canada, which employs about 30 quarantine officers (graduate nurses backed up by 2 medical officers) working at 6 airport quarantine centres (Vancouver, Calgary, Toronto, Ottawa, Montréal and Halifax). The act gives these officers substantial powers for case-specific measures and quarantine and the authority to deal with potentially infected cargo, conveyances and human remains. If a mass absolute quarantine is contemplated, the federal minister of health has the authority to requisition any premises for use as a quarantine facility (e.g., an airport hotel).
An individual of concern is identified, almost always, on the basis of being clinically ill and is referred to the quarantine officer by airplane staff (an obligation under international law) or by a customs officer. The quarantine officer does an initial medical assessment and, if necessary, refers the person to a local hospital with which the Public Health Agency of Canada has a service agreement. The person's disposition is then determined. The hospital provides isolation facilities, if required.
The powers of the Quarantine Act are reasonable if used appropriately. If, for example, an airplane passenger develops pneumonic plague en route to Canada, that individual should be isolated and close contacts detained until appropriate control measures (i.e., chemoprophlyaxis and public health observation) are put in place. As a practical measure, someone needs to be available to deal with sick passengers, if only to support the airport staff. The act should be used almost exclusively for case-specific measures and rarely, if ever, for true quarantine.
Could border quarantine protect Canada against an influenza pandemic? No. It would be impossible to identify all people potentially exposed to a disease infecting hundreds of millions of people worldwide. In addition, people with asymptomatic infections would still slip through a quarantine net.
The costs of attempting quarantine for pandemic influenza control would be enormous. Consider the implications. All people — visitors and returning Canadians — arriving from any affected country would have to be put in absolute quarantine for 3 days (the maximum incubation period of influenza). In addition, any person arriving here from an unaffected country not observing similarly strict precautions would also need to be quarantined. (Recall that the woman who brought SARS to Toronto arrived asymptomatic in Canada on a plane from the United States.) Very quickly, tens of thousands of people would be in quarantine in and around Canada's airports. The whole system would soon collapse in chaos, and international travel would grind to halt. How long would it go on … weeks, months, years?
Could border quarantine delay the arrival of an influenza pandemic? Perhaps, but this is entirely speculative. Ironically, border quarantine may not even be necessary. Influenza marches to its own epidemiologic drummer, for reasons we do not truly understand. The 1968 pandemic, for example, took several months to reach North America notwithstanding extensive trans-Pacific air travel.
Our national borders are not, and probably never were, an important line of defence against infectious diseases. Our real defences — and they are very robust — lie in sanitation and hygiene, in our excellent overall health and general medical care, and in immunization, antibiotics and antiviral drugs. We should focus on strengthening global surveillance and our ability to acquire and quickly apply new knowledge.
The Public Health Agency of Canada should seriously address the appropriate application of quarantine (both at our borders and more generally) now, before we face an influenza pandemic or other crisis. The powers of the Quarantine Act will be useful in appropriate but very limited circumstances. The current perception that quarantine has a larger role in infectious disease control is questionable and needs to be better defined. Does quarantine really have a viable role in the 21st century, or should it be sent back to the dustbin of history?
@ See related article page 1827
Key points about quarantine and case-specific measures
Quarantine
• Directed at people thought to have been exposed to a communicable disease and who may be incubating the infection (targets incubation period)
• Appropriate for diseases that are spread during incubation period or very early in symptomatic stage
• Ineffective for diseases that can be spread by people with asymptomatic illness
• It must be possible and practical to identify all, or virtually all, people incubating the disease
• Infected people must comply with the conditions of the quarantine
• Border quarantine would not protect Canada against an influenza pandemic
Case-specific measures (case isolation)
• Directed at people known or suspected, on clinical or laboratory grounds, to be actually infected (targets clinical illness)
• Appropriate for diseases that are spread only during symptomatic illness
Comments
• Our real defence lies in sanitation and hygiene, overall health and general medical care, and in immunization, antibiotics and antiviral drugs
• The focus should be on strengthening global surveillance and our ability to acquire and quickly apply new knowledge about infectious diseases
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Richard Schabas, Hastings and Prince Edward Counties Health Unit, 179 North Park St., Belleville ON K8P 4P1; fax 613 966-9418; rschabas@hpechu.on.ca
REFERENCES
- 1.Quarantine Act, RSC 2005, c20, s82. Repeals RSC 1985, cQ-1. Available: http://lois.justice.gc.ca/en/Q-1/258445.html (accessed 2007 May 18).
- 2.Public Health Agency of Canada. New Quarantine Act to further protect the health of Canadians [news release]. Ottawa: The Agency; 2006 Dec 12. Available: www.phac-aspc.gc.ca/media/nr-rp/2006/2006_10_e.html (accessed 2007 May 1).
- 3.Dorland's illustrated medical dictionary. 24th ed. Philadelphia: Saunders; 1965. p. 1260.
- 4.Heymann DL, editor. Control of communicable diseases manual. 18th ed. Washington (DC): American Public Health Association; 2004. p. 621.
- 5.Dwosh H, Hong HHL, Austgarden D, et al. Identification and containment of an outbreak of SARS in a community hospital. CMAJ 2003;168:1415-20. [PMC free article] [PubMed]
- 6.Sehdev PS. The origin of quarantine. Clin infect dis 2002;35:1071-2. [DOI] [PubMed]
- 7.Whittingham HE. What has happened to quarantine. Med Serv J Can 1958;14:327-31. [PubMed]
- 8.Barbera J, Macintyre A, Gostin L, et al. Large-scale quarantine following biological terrorism in the United States: scientific examination, logistic and legal limits, and possible consequences. JAMA 2001;286:2711-7. [DOI] [PubMed]
- 9.World Health Organization. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). Geneva: The Organization; 2003. p. 8. Available: www.who.int/csr/sars/en/WHOconsensus.pdf (accessed 2007 May 1).
- 10.Svoboda T, Henry B, Shulman L, et al. Public health measures to control the spread of severe acute respiratory syndrome during the outbreak in Toronto. N Engl J Med 2004;350:2352-61. [DOI] [PubMed]
- 11.Schabas R. Severe acute respiratory syndrome: Did quarantine help? Can J Infect Dis 2004;15:204. Available: www.pulsus.com/Infdis/15_04/shab_ed.htm (accessed 2007 May 1). [DOI] [PMC free article] [PubMed]
- 12.Wilson K. Pandemic threats and the need for new emergency public health legislation in Canada. Healthcare Policy 2006;2:35-42. [PMC free article] [PubMed]


