Abstract
New antibiotics are required to have the antibacterial activity against doxycycline-resistant Orientia tsutsugamushi. An in vitro sensitivity study showed that telithromycin was more effective than erythromycin for Rickettsia, Bartonella, and Coxiella burnetii. In this prospective, open-label, randomized trial, we enrolled patients with mild-to-moderate scrub typhus. We compared the efficacy and safety of a 5-day telithromycin therapy with those of a 5-day doxycycline therapy at Chosun University Hospital or one of its two community-based affiliated hospitals (Jangheung Hospital and Cheomdan Hospital), which are all located in southwestern Korea, between September and December 2005. A total of 92 patients were randomly assigned to either the telithromycin group (n = 47) or the doxycycline group (n = 45). After the treatment, fever control time was 20.45 ± 12.9 h in the telithromycin group and 22.60 ± 21.44 h in the doxycycline group (P > 0.05). After the treatment, the cure rate was 100% in the telithromycin group and 97.8% in the doxycycline group (P > 0.05). Furthermore, there were no significant differences in time elapsed until such symptoms as headache, myalgia, and rash disappeared. No serious adverse events or death were noted following the treatment in both groups. There were no significant differences in adverse events. In conclusion, the efficacy and safety of a 5-day once-a-day regimen of 800 mg telithromycin were equivalent to those of a 5-day twice-a-day regimen of 100 mg doxycycline in patients with mild-to-moderate scrub typhus. Telithromycin could be considered a promising new antibacterial agent for patients with scrub typhus.
A disease endemic to Asia, scrub typhus is caused by a strict intracellular, gram-negative bacterium, Orientia tsutsugamushi. It is an acute febrile illness whose symptoms and signs include fever, headache, chill, myalgia, rash, eschar, and lymphadenopathy. In most cases, recovery without sequelae is achieved with early treatment. In some cases, however, severe complications such as interstitial pneumonia, acute respiratory distress syndrome, acute renal failure, and multiple organ dysfunction occur, which may lead to death. Therefore, great care must be taken to manage patients with scrub typhus (3, 8).
Most cases of scrub typhus rapidly respond to the appropriate antibiotics; fever can be controlled within 48 h after the initiation of antibiotic treatment (19). To date, chloramphenicol has been the first effective antibiotic for the treatment of scrub typhus. Currently, however, doxycycline is regarded as a drug of choice. Quinolone has also been used experimentally, although its efficacy remains questionable. According to the U.S. Food and Drug Administration (FDA) Fetal Risk Summary, however, chloramphenicol and tetracyclines are classified as class D drugs, which are contraindicated in pregnant women. Furthermore, according to a study in Thailand, O. tsutsugamushi showed a resistance to chloramphenicol and doxycycline (22). It is therefore imperative that new antibiotics be promptly developed. According to some in vitro studies, doxycycline-resistant O. tsutsugamushi isolates from humans were sensitive to azithromycin (21, 23). Since then, it has been reported that children and pregnant women were successfully treated with macrolides, including azithromycin (4, 11). In a controlled trial comparing azithromycin with doxycycline, the efficacy of a single administration of 500 mg azithromycin was equivalent to that of a 7-day daily administration of 200 mg doxycycline (10). In our previous case report and one clinical trial, however, treatment failure occurred with symptoms of relapse after azithromycin therapy (5, 12). Therefore, azithromycin must be used with caution.
The first of the ketolide antibiotics, telithromycin has good antibacterial activity against intracellular bacteria such as Chlamydophila, Mycoplasma, Legionella spp., and other diverse ones. An in vitro sensitivity study showed that telithromycin was more effective than erythromycin for Rickettsia, Bartonella and Coxiella burnetii (17). This suggests that telithromycin could be used as an alternative drug for the treatment of rickettsiosis or Orientia infection.
In a recent preliminary study reported in Korea on comparing the clinical effectiveness of telithromycin with doxycycline on scrub typhus, it has been shown that telithromycin showed a better treatment outcome than doxycycline (13); however, to date, no English literatures have described the efficacy of telithromycin in treating patients with scrub typhus.
Under the background described above, we conducted this study to compare the efficacy and safety of telithromycin with those of doxycycline in treating patients with mild-to-moderate scrub typhus.
MATERIALS AND METHODS
Patient selection.
In this multicenter, prospective study, we enrolled patients with possible scrub typhus. Inclusion criteria were adults aged 18 years or older, a fever higher than 37.5°C, the concurrent presence of eschar or a maculopapular skin rash, and the clear presence of more than two symptoms such as headache, malaise, myalgia, coughing, nausea, and abdominal discomfort. Patients were hospitalized at Chosun University Hospital in Gwangju, Korea or one of its two community-based affiliated hospitals (Jangheung Hospital and Cheomdan Hospital), which are all located in southwestern Korea, between September and December 2005.
Exclusion criteria were an inability to take oral medications, pregnancy, hypersensitivity to the trial drugs, previous drug therapy with potential antirickettsial activity (e.g., rifampin, chloramphenicol, macrolides, fluoroquinolones, or tetracyclines) within 48 h prior to admission, severe scrub typhus (shock requiring vasopressor therapy for more than 1 h, a stuporous or comatose level of consciousness, respiratory failure requiring mechanical ventilation, or renal failure requiring immediate dialysis) (10, 14). For the differential diagnosis of scrub typhus from other diseases with similar symptoms (e.g., murine typhus, leptospirosis, hemorrhagic fever with renal syndrome, and systemic lupus erythematosus), patients underwent diagnostic tests. We thus excluded patients with concurrent infections who had the risk of causing different outcomes.
Prior to the study, patients or their guardians submitted a written informed consent (10). The protocol was approved by the Institutional Ethics Board for the Clinical Research of Chosun University Hospital.
A diagnosis of scrub typhus was made in cases in which either a single indirect immunofluorescent specific immunoglobulin M (IgM) titer against O. tsutsugamushi exceeded 1:80 or the immunofluorescent antibody assay titer increased more than four times (9). In our patients, we monitored the clinical course on a daily basis during hospitalization and then once a week for 4 weeks after discharge. Patients were contacted by telephone 1 month after discharge for a checkup of symptoms of relapse.
Number of subjects and basis of calculation.
To compare the bioequivalence between the two antibiotics based on Blackwelder's methods, we assumed the response rate of doxycycline to be 90% and defined a >20% difference in the cure rate as not being bioequivalent (2). It was assumed that the type I and type II errors were 0.05 and 0.20, respectively, and at least 33 patients per group were required to be evaluated. When assuming a 20% dropout rate, a minimum of 40 patients per group was recruited for a total of 80 experimental subjects.
Randomization and treatment assignment.
After submitting a written, informed consent, the patients with an temperature of higher than 37.5°C and who met the eligibility criteria were randomly allocated to receive one of two oral regimens in accordance with a protocol that was determined by the last digit of a resident registration number (the patients with an odd number were treated by a 5-day course of daily 200-mg doses of doxycycline, and the patients with an even number were treated by a 5-day course of daily 800-mg doses of telithromycin). Therapy was started immediately after a comprehensive clinical examination and the collection of specimens for laboratory tests.
Outcome measures.
The primary end point was the fever clearance time; this was defined as the interval between the time at which the first dose of antibiotic was administered and the time at which the oral temperature first fell below 37.3°C and then remained below this threshold without antipyretics for a minimum of 48 h.
The secondary end point was evaluated according to the following definitions. “Cure” was defined as the resolution of fever within 5 days after initiating the antimicrobial therapy. “Failure” was defined as the persistence of fever without any identifiable cause. “Relapse” was defined as the reappearance of fever and the clinical manifestations of scrub typhus, in the absence of any other identifiable cause, within 30 days after completing therapy as described previously (10). All patients were assessed for toxicity, and “adverse events” (AEs) were defined as any symptoms or signs that appeared during treatment and that had not been reported prior to the administration of the first dose of the antibiotic.
Statistical analysis.
Pearson's χ2 or Fisher's exact tests were applied for comparison of rates and proportions. Mann-Whitney U tests were used to analyze continuous variables that were not normally distributed. An independent-sample t test was used to compare normally distributed variables. The Kaplan-Meier survival method was employed to compare the fever clearance time between the two groups. The log rank test was used to compare the cure rate between the two groups. An intent-to-treat analysis was used as the basic analysis for effectiveness. Additional per-protocol analysis was performed for all the effectiveness variables; thus, any deviation that could develop according to the selection method of the evaluated subjects was assessed. A P value of < 0.05 was considered statistically significant. Statistical analysis was done using SPSS version 12.0 for Windows (SPSS, Inc., Illinois, Chicago). All data were expressed as means ± standard deviations (SD).
RESULTS
Demographic characteristics.
A total of 163 patients visited Chosun University Hospital and its affiliated hospitals between September and December 2005 with a chief complaint of fever or rash.
Of them, 68 patients did not meet inclusion criteria (a previous history of drug therapy with potential antirickettsial activity in 9 patients, a temperature of lower than 37.5°C in 27 patients, severe complications associated with scrub typhus in 9 patients [4 cases of shock requiring vasopressor therapy for more than 1 h, 3 cases of stuporous or comatose-level consciousness, and 2 cases of respiratory failure requiring mechanical ventilation], 1 case of vomiting in which oral intake was impossible, and refusal of participation in 22 patients). Ninety-five patients satisfied inclusion criteria. Of these patients, however, 3 had concurrent diseases (3 cases of hemorrhagic fever with renal syndrome). Excluding these patients, we finally selected 92 patients (n = 92) and then assigned them to the telithromycin group (n = 47) and the doxycycline group (n = 45). In both groups, a 5-day daily administration was done, and intent-to-treat analyses were then performed. At baseline, there were no significant differences in the demographic and clinical data, such as age, sex, duration of symptoms, and laboratory measurements between the two groups. Baseline characteristics are represented in Table 1. Among 92 patients, 76 patients (37 [82.2%] of 45 patients in the doxycycline administration group, and 39 [83%] of 47 patients in the telithromycin administration group) had an IgM titer greater than 1:80 or an elevation of IgG greater than 4 times that which could be confirmed, so a definite diagnosis could be made. Among those in the telithromycin-administered group, 8 patients had not definitely been diagnosed with scrub typhus. Four of these patients could not be confirmed due to insufficient follow-up (but eschars were detected on all 4 patients), 2 patients were confirmed to have different diseases, 1 patient had drug fever, and for another patient, definite causality could not be determined; nonetheless, even on the follow-up serum test performed after 1 week, the IgM was less than 10 and the IgG was less than 32. Among the 8 undiagnosed patients in the doxycycline-administered group, 1 patient was confirmed to have adult-onset Still's disease and 7 patients could not be confirmed due to insufficient follow-up. However, eschars were detected on all 7 patients. All the results that are presented are based on the intent-to-treat analysis.
TABLE 1.
Demographic and clinical characteristics of patients evaluated in a comparative study of telithromycin and doxycycline for treatment of scrub typhus
| Parameter | Result for treatment groupa:
|
|
|---|---|---|
| Telithromycin (n = 47) | Doxycycline (n = 45) | |
| Demographic data | ||
| Age (mean yr ± SD) | 60.2 ± 15.9 | 61.6 ± 12.8 |
| Gender (no. of male/no. of female) | 14/33 | 18/27 |
| Duration of illness before admission (mean days ± SD) | 6.38 ± 3.9 | 6.64 ± 3.5 |
| Clinical symptoms and signs (no. [%] of patients) | ||
| Headache | 40 (85.1) | 36 (80) |
| Myalgia | 36 (76.6) | 34 (75.6) |
| Skin rash | 45 (95.7) | 42 (93.3) |
| Eschar | 42 (89.4) | 40 (88.9) |
| Laboratory measurements | ||
| White blood cell count (no. of cells × 1,000/mm3) | 6.7 ± 3.3 | 7.7 ± 3.8 |
| Hemoglobin (g/dl) | 12.5 ± 1.4 | 12.9 ± 1.6 |
| Platelet count (no. of cells × 1,000/mm3) | 141.4 ± 50.5 | 148.7 ± 47.6 |
| AST (IU/liter) | 102.3 ± 82.9 | 84.9 ± 57.7 |
| ALT (IU/liter) | 88.4 ± 94.5 | 71.8 ± 55.9 |
| Serum creatinine (mg/dl) | 1.1 ± 0.3 | 1.1 ± 0.4 |
There was no significant difference in baseline characteristics between the two groups (P > 0.05). Values are means ± SD.
Efficacy.
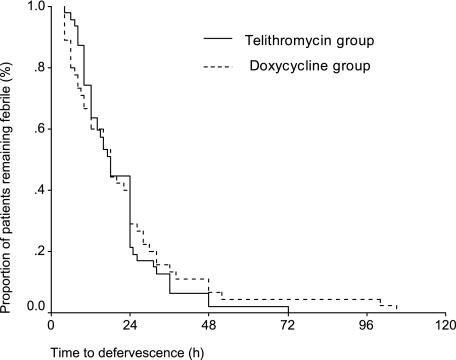
After the treatment, at the primary end point, fever clearance times were 20.45 ± 12.9 h in the telithromycin group and 22.60 ± 21.44 h in the doxycycline group (P > 0.05). However, this was not statistically significant (Table 2). To compare fever clearance time between the two groups, a log rank test was done using the Kaplan-Meier curve. This also showed no statistical significance (Fig. 1). Furthermore, there were no significant differences in time elapsed until such symptoms as headache, myalgia, and rash have disappeared (Table 2). A similar result was confirmed on the per-protocol analysis as well (data not shown).
TABLE 2.
Time elapsed until the symptoms have disappeared after the administration of antibiotics for scrub typhus in a comparative study of telithromycin and doxycycline regimens
| Symptom (unit) | Time until symptom disappeared for paitents in treatment groupa:
|
|
|---|---|---|
| Telithromycin (n = 47) | Doxycycline (n = 45) | |
| Fever (h) | 20.45 ± 12.9 | 22.60 ± 21.44 |
| Headache (days) | 3.67 ± 3.37 | 3.0 ± 2.14 |
| Myalgia (days) | 3.74 ± 3.98 | 4.12 ± 7.24 |
| Rash (days) | 6.56 ± 5.10 | 7.56 ± 4.24 |
There were no significant differences in time elapsed until symptoms disappeared between the two groups (P > 0.05). Values are means ± SD.
FIG. 1.
Kaplan-Meier curve plotting fever clearance time for patients who received telithromycin or doxycycline for the treatment of scrub typhus.
In patients in whom a diagnosis of scrub typhus was established, the elapsed times until symptoms disappeared were as follows: fever, 21.72 ± 13.50 h (telithromycin group) and 22.19 ± 22.59 h (doxycycline group); headache, 3.94 ± 3.58 days (telithromycin group) and 2.90 ± 2.22 days (doxycycline group); myalgia, 3.97 ± 4.30 days (telithromycin group) and 4.28 ± 7.80 days (doxycycline group); rash, 6.74 ± 5.46 days (telithromycin group) and 7.50 ± 4.27 days (doxycycline group). There were no significant differences in time elapsed until the symptoms disappeared between the two groups of patients in whom a diagnosis of scrub typhus was established by serology (P > 0.05).
After treatment, the cure rate was 100% in the telithromycin group and 97.8% in the doxycycline group based on the intent-to-treat analysis (Table 3). However, this was not statistically significant. In all patients with mild-to-moderate scrub typhus, fever clearance was noted following treatment. In 1 patient in the doxycycline group, however, fever clearance was noted 24 h after the treatment. This patient visited us again 2 weeks later with fever, rash, and pericarditis, in whom no causal relationship was found. Based on the assumption that the above patient had a relapse, we administered telithromycin to that patient. However, no treatment response was noted, and after treatment with a steroid, the patient's symptoms were improved. No definite causal relationship was identified, but the possibility of viral pericarditis could not be ruled out.
TABLE 3.
Outcomes of patients who received either telithromycin or doxycycline for the treatment of scrub typhus
| Outcome | Result for treatment groupa:
|
|
|---|---|---|
| Telithromycin (n = 47) | Doxycycline (n = 45) | |
| Cure (no. [%] of patients) | 47 (100) | 44 (97.8) |
| Failure (no. of patients) | 0 | 0 |
| Relapse (no. [%] of patients) | 0 | 1 (2.2) |
| Median (range) fever clearance time (h) | 18 (4-72) | 18 (4-105) |
There were no significant differences in outcome measures between the two groups (P > 0.05).
AEs.
No serious AEs or death were noted following the treatment in both groups (Table 4). AEs were detected in 14.9% (7/47) of patients in the telithromycin group and 24.4% (11/45) of patients in the doxycycline group. Gastrointestinal AEs were also found in both groups; three cases of abdominal discomfort in the telithromycin group and six cases in the doxycycline group (two cases of nausea, one case of vomiting, one case of diarrhea, and two cases of abdominal discomfort).
TABLE 4.
AEs in patients who received either telithromycin or doxycycline for the treatment of scrub typhus
| AE | No. (%) of patients with AE in treatment groupa:
|
|
|---|---|---|
| Telithromycin (n = 47) | Doxycycline (n = 45) | |
| Nausea | 0 | 2 (4.4) |
| Vomiting | 0 | 1 (2.2) |
| Diarrhea | 0 | 1 (2.2) |
| Abdominal discomfort | 3 (6.4) | 2 (4.4) |
| Elevated serum ALT level | 4 (8.5) | 2 (4.4) |
| Skin rash | 0 | 2 (4.4) |
| Esophageal candidiasis | 0 | 1 (2.2) |
There were no significant differences in the incidences of AEs between the two groups (P > 0.05).
Clinically notable laboratory findings were seen in both groups; the hepatic parameters such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were elevated by more than two times above the baseline in 8.5% (4/47) of patients in the telithromycin group and 4.4% (2/45) of patients in the doxycycline group. In addition, two cases of skin rash and one case of esophageal candidiasis were developed in the doxycycline group. In all cases, however, the AEs were of mild-to-moderate severity. In the doxycycline group, excluding one case of skin rash, the administration schedule was not discontinued.
DISCUSSION
Scrub typhus is a disease endemic to the Pacific coast, particularly in northern Australia and East Asia, including Korea. To date, chloramphenicol, tetracycline, and doxycycline have been used as effective antibiotics for scrub typhus. However, chloramphenicol is no longer in use because of the adverse drug reactions, such as fatal aplastic anemia, bone marrow suppression, and gray baby syndrome (7, 11). Tetracycline is contraindicated in pregnant women and children aged 8 years or younger. This is because tetracycline causes permanent tooth staining in fetuses and young children, even though doxycycline itself does not cause significant tooth staining and can be used for treatment of severe, life-threatening rickettsial diseases in children. It has been reported that the new macrolide antibiotics were applied not only for in vitro assay but they were also used at clinics for pregnant women and children with scrub typhus or rickettsial infections, whose safety and efficacy have been described in published studies (4, 11, 21, 23). Among the macrolides, azithromycin could be used as the representative drug. In some cases, however, treatment failure as well as recurrence occurred after the administration of azithromycin (5, 12). According to a previous study comparing 3-day azithromycin therapy (n = 18) with doxycycline therapy (n = 12), there were two cases of treatment failure and recurrence in the azithromycin group (5). In one patient, fever persisted 24 h after a full 3-day course of azithromycin therapy. The other patient experienced symptoms of relapse 3 days after azithromycin treatment was completed. Further studies are therefore warranted to evaluate the outcome of azithromycin treatment.
The first ketolide antibiotic, telithromycin, was produced by the structural modification of macrolides. In comparison with macrolides, the affinity of ketolides to the binding sites in domains II and V of the 50S ribosomal subunit has improved (15, 24). Owing to this, ketolides showed antibacterial activity against not only macrolide-resistant bacteria but also various strains including Chlamydophila and Legionella (16, 18, 20). According to in vitro experiments, telithromycin showed good antibacterial activity against Rickettsia spp., Bartonella spp., and Coxiella burnetii, and its MIC was lower than that of erythromycin (17). These results suggest that telithromycin is an effective antibiotic in treating patients with rickettsiosis and scrub typhus.
In Korea, a preliminary study compared the efficacy of telithromycin with that of doxycycline regarding fever clearance time in patients with scrub typhus (5). According to this study, the fever clearance time was shorter in the telithromycin group than the doxycycline group. In our series, however, there was no significant difference in fever clearance time between the two groups. The above-mentioned, preliminary study was conducted with 23 Korean patients with scrub typhus at two centers. These patients were divided into the telithromycin group (n = 12) and the doxycycline group (n = 11). This study showed that fever clearance time was 17.7 h in the telithromycin group and 30.7 h in the doxycycline group, which was statistically significant. In one center, however, patients were all given telithromycin. In these patients, 800 mg telithromycin was administered twice on the first day and then administered once daily from the next day on. From then on, 800 mg telithromycin was administered for 2 to 3 days after fever disappeared. In the other center, patients were all given 100 mg doxycycline twice daily and then administered for 2 to 3 days after fever disappeared. In other words, the weakness of the above study is the lack of randomization and that the loading dose was given to the telithromycin group only. In our series, however, both the intent-to-treat analysis and analysis of patients in whom a diagnosis of scrub typhus was established showed no significant differences in two outcome measures for the efficacy of telithromycin (primary and secondary end points) between the two groups (P > 0.05).
We enrolled not only patients who were hospitalized at one university hospital (the tertiary hospital) but also those who were hospitalized at the primary medical institutions such as the two affiliated community hospitals. This is somewhat different from the previous studies enrolling patients who were hospitalized at only tertiary hospitals. In other words, among those who visited the tertiary hospitals, many patients had already been treated at the primary medical institutions and had a relatively severe disease. Therefore, their clinical manifestations and treatment response could be different from those of patients who were treated at the primary medical institutions. In this regard, compared with the previous studies of patients who were admitted at the tertiary hospitals only, our patients consisted of not only moderate but also mild cases. Therefore, our enrolled patients are considered to better represent the actual clinical manifestations and treatment responses of O. tsutsugamushi-infected patients. This might explain why the fever clearance time was shorter in our study than other recent Korean reports (10, 13).
Of interest, there was a significant difference in fever clearance time following doxycycline treatment between the tertiary hospital and the primary medical institutions, (28.12 ± 26.67 h in 25 cases versus 15.70 ± 8.69 h in 20 cases). On the other hand, there was no significant difference in fever clearance time following telithromycin treatment between the tertiary hospital and the primary medical institutions (21.04 ± 11.87 h in 28 cases versus 19.58 ± 14.58 h in 19 cases). These differences can be attributed to the severity of scrub typhus or the involvement of doxycycline-resistant strains, which deserves further studies.
Gastrointestinal AEs were more frequent in the doxycycline group. The temporary elevation of serum AST and ALT was more frequent in the telithromycin group. However, these differences did not reach statistical significance. No serious events or death were noted following the treatment in our series. Our results showed that there were no significant differences in the incidences of AEs between the two groups. However, cautious use of telithromycin is required because potential fatal hepatotoxicity of telithromycin has been reported (1, 6). In addition, doxycycline is more cost effective than telithromycin. Therefore, the lack of cost effectiveness and AEs could be a limiting factor for the use of telithromycin. Furthermore, the FDA did not approve the use of telithromycin in children. The FDA classified telithromycin as a class C drug, whereas azithromycin is a class B one. According to the FDA, telithromycin must be cautiously used in pregnant women.
Our cohorts had mild-to-moderate scrub typhus because we excluded patients with severe scrub typhus. Therefore, we do not know whether telithromycin would be effective in treating severe scrub typhus. Further studies are required including the optimum antibiotics therapy of severe scrub typhus.
In conclusion, we first reported, in English, that the efficacy and safety of a 5-day once-a-day regimen of 800 mg telithromycin were equivalent to those of a 5-day twice-a-day regimen of 100 mg doxycycline in patients with scrub typhus. Telithromycin could be considered a promising new antibacterial agent for patients with scrub typhus.
Acknowledgments
This study was financially supported by Sanofi-Aventis Korea Co., Ltd.
The present study was supported by grants from the Clinical Medicine Research Institute at Chosun University Hospital.
The authors have no conflicts of interest.
Footnotes
Published ahead of print on 2 April 2007.
REFERENCES
- 1.Bertino, J. S. 2006. Severe hepatotoxicity of telithromycin. Ann. Intern. Med. 145:472. [DOI] [PubMed] [Google Scholar]
- 2.Blackwelder, W. C. 1982. “Proving the null hypothesis” in clinical trials. Control Clin. Trials 3:345-353. [DOI] [PubMed] [Google Scholar]
- 3.Chi, W. C., J. J. Huang, J. M. Sung, R. R. Lan, W. C. Ko, and F. F. Chen. 1997. Scrub typhus associated with multiorgan failure: a case report. Scand. J. Infect. Dis. 29:634-635. [DOI] [PubMed] [Google Scholar]
- 4.Choi, E. K., and H. Pai. 1998. Azithromycin therapy for scrub typhus during pregnancy. Clin. Infect. Dis. 27:1538-1539. [DOI] [PubMed] [Google Scholar]
- 5.Chung, M. H., S. W. Han, M. G. Choi, W. H. Chang, H. J. Pai, H. S. Shin, H. J. Jung, M. H. Kang, and J. Y. Jung. 2000. Comparison of a 3-day course of azithromycin with doxycycline for the treatment of scrub typhus. Korean J. Infect. Dis. 23:433-438. [Google Scholar]
- 6.Clay, K. D., J. S. Hanson, S. D. Pope, R. W. Rissmiller, P. P. Purdum III, and P. M. Banks. 2006. Brief communication: severe hepatotoxicity of telithromycin: three case reports and literature review. Ann. Intern. Med. 144:415-420. [DOI] [PubMed] [Google Scholar]
- 7.Feder H. M., Jr., C. Osier, and E. G. Maderazo. 1981. Chloramphenicol: a review of its use in clinical practice. Rev. Infect. Dis. 3:479-491. [DOI] [PubMed] [Google Scholar]
- 8.Hsu, G. J., T. Young, M. Y. Peng, F. Y. Chang, M. Y. Chou, and L. F. Sheu. 1993. Acute renal failure associated with scrub typhus: report of a case. J. Formos. Med. Assoc. 92:475-477. [PubMed] [Google Scholar]
- 9.Kim, D. M., N. R. Yun, T. Y. Yang, J. H. Lee, J. T. Yang, S. K. Shim, E. N. Choi, M. Y. Park, and S. H. Lee. 2006. Usefulness of nested PCR for the diagnosis of scrub typhus in clinical practice: a prospective study. Am. J. Trop. Med. Hyg. 75:542-545. [PubMed] [Google Scholar]
- 10.Kim, Y. S., H. J. Yun, S. K. Shim, S. H. Koo, S. Y. Kim, and S. Kim. 2004. A comparative trial of a single dose of azithromycin versus doxycycline for the treatment of mild scrub typhus. Clin. Infect. Dis. 39:1329-1335. [DOI] [PubMed] [Google Scholar]
- 11.Lee, K. Y., H. S. Lee, J. H. Hong, J. K. Hur, and K. T. Whang. 2003. Roxithromycin treatment of scrub typhus (tsutsugamushi disease) in children. Pediatr. Infect. Dis. J. 22:130-133. [DOI] [PubMed] [Google Scholar]
- 12.Lee, S. H., D. M. Kim, Y. S. Cho, S. H. Yoon, and S. K. Shim. 2006. Usefulness of eschar PCR for diagnosis of scrub typhus. J. Clin. Microbiol. 44:1169-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim, J. H., S. Y. Lee, J. S. Lee, S. Chil, E. S. Kim, M. H. Chung, J. S. Kang, J. H. Lee, Y. K. Cho, and S. O. Lee. 2006. A preliminary report on the clinical efficacy of telithromycin for the treatment of scrub typhus. Korean J. Infect. Dis. 38:39-44. [Google Scholar]
- 14.McClain, J. B., B. Joshi, and R. Rice. 1988. Chloramphenicol, gentamicin, and ciprofloxacin against murine scrub typhus. Antimicrob. Agents Chemother. 32:285-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Namour, F., D. H. Wessels, M. H. Pascual, D. Reynolds, E. Sultan, and B. Lenfant. 2001. Pharmacokinetics of the new ketolide telithromycin (HMR 3647) administered in ascending single and multiple doses. Antimicrob. Agents Chemother. 45:170-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roblin, P. M., and M. R. Hammerschlag. 1998. In vitro activity of a new ketolide antibiotic, HMR 3647, against Chlamydia pneumoniae. Antimicrob. Agents Chemother. 42:1515-1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rolain, J. M., M. Maurin, A. Bryskier, and D. Raoult. 2000. In vitro activities of telithromycin (HMR 3647) against Rickettsia rickettsii, Rickettsia conorii, Rickettsia africae, Rickettsia typhi, Rickettsia prowazekii, Coxiella burnetii, Bartonella henselae, Bartonella quintana, Bartonella bacilliformis, and Ehrlichia chaffeensis. Antimicrob. Agents Chemother. 44:1391-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schulin, T., C. B. Wennersten, M. J. Ferraro, R. C. J. Moellering, and G. M. Eliopoulos. 1998. Susceptibilities of Legionella spp. to newer antimicrobials in vitro. Antimicrob. Agents Chemother. 42:1520-1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheehy, T. W., D. Hazlett, and R. E. Turk. 1973. Scrub typhus. A comparison of chloramphenicol and tetracycline in its treatment. Arch. Intern. Med. 132:77-80. [DOI] [PubMed] [Google Scholar]
- 20.Soriano, F., R. Fernandez-Roblas, R. Calvo, and G. Garcia-Calvo. 1998. In vitro susceptibilities of aerobic and facultative non-spore-forming gram-positive bacilli to HMR 3647 (RU 66647) and 14 other antimicrobials. Antimicrob. Agents Chemother. 42:1028-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strickman, D., T. Sheer, K. Salata, J. Hershey, G. Dasch, D. Kelly, and R. Kuschner. 1995. In vitro effectiveness of azithromycin against doxycycline-resistant and -susceptible strains of Rickettsia tsutsugamushi, etiologic agent of scrub typhus. Antimicrob. Agents Chemother. 39:2406-2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watt, G., C. Chouriyagune, R. Ruangweerayud, P. Watcharapichat, D. Phulsuksombati, K. Jongsakul, P. Teja-Isavadharm, D. Bhodhidatta, K. D. Corcoran, G. A. Dasch, and D. Strickman. 1996. Scrub typhus infections poorly responsive to antibiotics in northern Thailand. Lancet 348:86-89. [DOI] [PubMed] [Google Scholar]
- 23.Watt, G., P. Kantipong, K. Jongsakul, P. Watcharapichat, and D. Phulsuksombati. 1999. Azithromycin activities against Orientia tsutsugamushi strains isolated in cases of scrub typhus in Northern Thailand. Antimicrob. Agents Chemother. 43:2817-2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zuckerman, J. M. 2004. Macrolides and ketolides: azithromycin, clarithromycin, telithromycin. Infect. Dis. Clin. N. Am. 18:621-649, xi. [DOI] [PubMed] [Google Scholar]