Abstract
Background—Malnutrition and growth retardation are common complications of Crohn's disease in children. The contribution of resting energy expenditure (REE) to malnutrition is unclear. Aims—To characterise the REE and body composition in children with Crohn's disease and compare them with normal controls and patients with anorexia nervosa; to compare the effects of prednisolone and enteral nutrition on energy expenditure and body composition. Subjects—Twenty four children with Crohn's disease, 19 malnourished females with anorexia nervosa, and 22 healthy control subjects were studied. Methods—In children with Crohn's disease measurements were done when the disease was acute and repeated at one and three months after treatment with either prednisolone or enteral nutrition. Resting energy expenditure was measured by indirect calorimetry and body composition by anthropometry, bioelectrical impedance analysis, total body potassium, H218O, and bromide space studies. Results—Body weight and ideal body weight were significantly lower in patients with Crohn's disease than in healthy controls. Lean tissue was depleted and there was an increase in extracellular water. Per unit of lean body mass, there was no difference between REE in patients with Crohn's disease and controls, whereas patients with anorexia nervosa had significantly reduced REE. With enteral nutrition all body compartments and REE increased significantly (p<0.001). In a subgroup of age-matched men there was a significant increase in height after three months of enteral nutrition compared with prednisolone (p<0.01). Those treated with steroids did not show a significant change in height but did show an increase in all body compartments. However, intracellular water as well as lean body mass accretion were significantly higher in the enteral nutrition group than in the prednisolone group. Conclusions—Despite being malnourished, children with Crohn's disease fail to adapt their REE per unit of lean body mass. This might be a factor contributing to their malnutrition. Lean tissue accretion is higher in patients treated with enteral nutrition than in those treated with prednisolone.
Keywords: Crohn's disease; resting energy expenditure; body composition; anorexia nervosa; prednisolone; enteral nutrition
Full Text
The Full Text of this article is available as a PDF (132.4 KB).
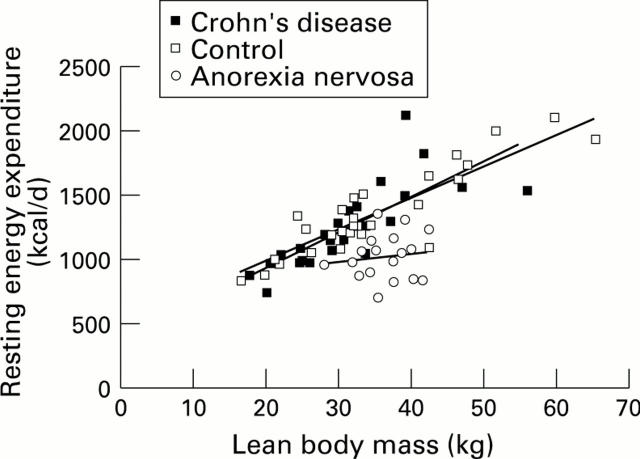
Figure 1 .
: Relation between resting energy expenditure and lean body mass by bioelectric impedance analysis in children with active Crohn's disease, (regression line n=24, r=0.77, SEE=206, p<0.001), healthy controls (regression line n=22, r=0.90, SEE=149, p<0.001), and patients with anorexia nervosa (regression line n=19, r=0.14, SEE=181, p<0.12).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aiges H., Markowitz J., Rosa J., Daum F. Home nocturnal supplemental nasogastric feedings in growth-retarded adolescents with Crohn's disease. Gastroenterology. 1989 Oct;97(4):905–910. doi: 10.1016/0016-5085(89)91496-0. [DOI] [PubMed] [Google Scholar]
- Barot L. R., Rombeau J. L., Feurer I. D., Mullen J. L. Caloric requirements in patients with inflammatory bowel disease. Ann Surg. 1982 Feb;195(2):214–218. doi: 10.1097/00000658-198202000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeken W. L., Busch H. J., Sylwester D. L. Intestinal protein loss in Crohn's disease. Gastroenterology. 1972 Feb;62(2):207–215. [PubMed] [Google Scholar]
- Belli D. C., Seidman E., Bouthillier L., Weber A. M., Roy C. C., Pletincx M., Beaulieu M., Morin C. L. Chronic intermittent elemental diet improves growth failure in children with Crohn's disease. Gastroenterology. 1988 Mar;94(3):603–610. doi: 10.1016/0016-5085(88)90230-2. [DOI] [PubMed] [Google Scholar]
- Beutler B. Cachexia: a fundamental mechanism. Nutr Rev. 1988 Nov;46(11):369–373. doi: 10.1111/j.1753-4887.1988.tb05370.x. [DOI] [PubMed] [Google Scholar]
- Chan A. T., Fleming C. R., O'Fallon W. M., Huizenga K. A. Estimated versus measured basal energy requirements in patients with Crohn's disease. Gastroenterology. 1986 Jul;91(1):75–78. doi: 10.1016/0016-5085(86)90441-5. [DOI] [PubMed] [Google Scholar]
- Durnin J. V., Rahaman M. M. The assessment of the amount of fat in the human body from measurements of skinfold thickness. Br J Nutr. 1967 Aug;21(3):681–689. doi: 10.1079/bjn19670070. [DOI] [PubMed] [Google Scholar]
- Flynn M. A., Woodruff C., Clark J., Chase G. Total body potassium in normal children. Pediatr Res. 1972 Apr;6(4):239–245. doi: 10.1203/00006450-197204000-00005. [DOI] [PubMed] [Google Scholar]
- GRANDE F., ANDERSON J. T., KEYS A. Changes of basal metabolic rate in man in semistarvation and refeeding. J Appl Physiol. 1958 Mar;12(2):230–238. doi: 10.1152/jappl.1958.12.2.230. [DOI] [PubMed] [Google Scholar]
- Grunow J. E., Azcue M. P., Berall G., Pencharz P. B. Energy expenditure in cystic fibrosis during activities of daily living. J Pediatr. 1993 Feb;122(2):243–246. doi: 10.1016/s0022-3476(06)80122-8. [DOI] [PubMed] [Google Scholar]
- Heymsfield S. B., Casper K. Continuous nasoenteric feeding: bioenergetic and metabolic response during recovery from semistarvation. Am J Clin Nutr. 1988 May;47(5):900–910. doi: 10.1093/ajcn/47.5.900. [DOI] [PubMed] [Google Scholar]
- Hoshino E., Pichard C., Greenwood C. E., Kuo G. C., Cameron R. G., Kurian R., Kearns J. P., Allard J. P., Jeejeebhoy K. N. Body composition and metabolic rate in rat during a continuous infusion of cachectin. Am J Physiol. 1991 Jan;260(1 Pt 1):E27–E36. doi: 10.1152/ajpendo.1991.260.1.E27. [DOI] [PubMed] [Google Scholar]
- Isaacs K. L., Sartor R. B., Haskill S. Cytokine messenger RNA profiles in inflammatory bowel disease mucosa detected by polymerase chain reaction amplification. Gastroenterology. 1992 Nov;103(5):1587–1595. doi: 10.1016/0016-5085(92)91182-4. [DOI] [PubMed] [Google Scholar]
- Kushner R. F., Schoeller D. A. Resting and total energy expenditure in patients with inflammatory bowel disease. Am J Clin Nutr. 1991 Jan;53(1):161–165. doi: 10.1093/ajcn/53.1.161. [DOI] [PubMed] [Google Scholar]
- Ligumsky M., Simon P. L., Karmeli F., Rachmilewitz D. Role of interleukin 1 in inflammatory bowel disease--enhanced production during active disease. Gut. 1990 Jun;31(6):686–689. doi: 10.1136/gut.31.6.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahida Y. R., Kurlac L., Gallagher A., Hawkey C. J. High circulating concentrations of interleukin-6 in active Crohn's disease but not ulcerative colitis. Gut. 1991 Dec;32(12):1531–1534. doi: 10.1136/gut.32.12.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahida Y. R., Wu K., Jewell D. P. Enhanced production of interleukin 1-beta by mononuclear cells isolated from mucosa with active ulcerative colitis of Crohn's disease. Gut. 1989 Jun;30(6):835–838. doi: 10.1136/gut.30.6.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motil K. J., Grand R. J., Maletskos C. J., Young V. R. The effect of disease, drug, and diet on whole body protein metabolism in adolescents with Crohn disease and growth failure. J Pediatr. 1982 Sep;101(3):345–351. doi: 10.1016/s0022-3476(82)80056-5. [DOI] [PubMed] [Google Scholar]
- O'Moráin C., Segal A. M., Levi A. J., Valman H. B. Elemental diet in acute Crohn's disease. Arch Dis Child. 1983 Jan;58(1):44–47. doi: 10.1136/adc.58.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigaud D., Angel L. A., Cerf M., Carduner M. J., Melchior J. C., Sautier C., René E., Apfelbaum M., Mignon M. Mechanisms of decreased food intake during weight loss in adult Crohn's disease patients without obvious malabsorption. Am J Clin Nutr. 1994 Nov;60(5):775–781. doi: 10.1093/ajcn/60.5.775. [DOI] [PubMed] [Google Scholar]
- Schoeller D. A., van Santen E., Peterson D. W., Dietz W., Jaspan J., Klein P. D. Total body water measurement in humans with 18O and 2H labeled water. Am J Clin Nutr. 1980 Dec;33(12):2686–2693. doi: 10.1093/ajcn/33.12.2686. [DOI] [PubMed] [Google Scholar]
- Seidman E. G. Nutritional management of inflammatory bowel disease. Gastroenterol Clin North Am. 1989 Mar;18(1):129–155. [PubMed] [Google Scholar]
- Seidman E., LeLeiko N., Ament M., Berman W., Caplan D., Evans J., Kocoshis S., Lake A., Motil K., Sutphen J. Nutritional issues in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1991 May;12(4):424–438. doi: 10.1097/00005176-199105000-00004. [DOI] [PubMed] [Google Scholar]
- Shetty P. S. The Nestlé Lecture. Chronic undernutrition and metabolic adaptation. Proc Nutr Soc. 1993 Aug;52(2):267–284. doi: 10.1079/pns19930063. [DOI] [PubMed] [Google Scholar]
- Strober W., James S. P. The interleukins. Pediatr Res. 1988 Nov;24(5):549–557. doi: 10.1203/00006450-198811000-00001. [DOI] [PubMed] [Google Scholar]
- Suzuki Y., Saito H., Kasanuki J., Kishimoto T., Tamura Y., Yoshida S. Significant increase of interleukin 6 production in blood mononuclear leukocytes obtained from patients with active inflammatory bowel disease. Life Sci. 1990;47(24):2193–2197. doi: 10.1016/0024-3205(90)90149-l. [DOI] [PubMed] [Google Scholar]
- Tanner J. M., Whitehouse R. H., Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. I. Arch Dis Child. 1966 Oct;41(219):454–471. doi: 10.1136/adc.41.219.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaisman N., Clarke R., Rossi M., Goldberg E., Zello G. A., Pencharz P. B. Protein turnover and resting energy expenditure in patients with undernutrition and chronic lung disease. Am J Clin Nutr. 1992 Jan;55(1):63–69. doi: 10.1093/ajcn/55.1.63. [DOI] [PubMed] [Google Scholar]
- Vaisman N., Pencharz P. B., Koren G., Johnson J. K. Comparison of oral and intravenous administration of sodium bromide for extracellular water measurements. Am J Clin Nutr. 1987 Jul;46(1):1–4. doi: 10.1093/ajcn/46.1.1. [DOI] [PubMed] [Google Scholar]
- Vaisman N., Rossi M. F., Goldberg E., Dibden L. J., Wykes L. J., Pencharz P. B. Energy expenditure and body composition in patients with anorexia nervosa. J Pediatr. 1988 Nov;113(5):919–924. doi: 10.1016/s0022-3476(88)80032-5. [DOI] [PubMed] [Google Scholar]