Abstract
Background—The pathogenesis of anorectal dysfunction, which occurs frequently in patients with diabetes mellitus, is poorly defined. Recent studies indicate that changes in the blood glucose concentration have a major reversible effect on gastrointestinal motor function. Aims—To determine the effects of physiological changes in blood glucose and hyperglycaemia on anorectal motor and sensory function in normal subjects. Subjects—In eight normal subjects measurements of anorectal motility and sensation were performed on separate days while blood glucose concentrations were stabilised at 4, 8, and 12 mmol/l. Methods—Anorectal motor and sensory function was measured using a sleeve/sidehole catheter incorporating a balloon, and electromyography. Results—The number of spontaneous anal relaxations was greater at 12 mmol/l than at 8 and 4 mmol/l glucose (p<0.05 for both). Anal squeeze pressures were less at a blood glucose of 12 mmol/l when compared with 8 and 4 mmol/l (p<0.05 for both). During rectal distension, residual anal pressures were not significantly different between the three blood glucose concentrations. Rectal compliance was greater (p<0.05) at a blood glucose of 12 mmol/l when compared with 4 mmol/l. The threshold volume for initial perception of rectal distension was less at 12 mmol/l when compared with 4 mmol/l (40 (20-100) ml versus 10 (10-150) ml, p<0.05). Conclusions—An acute elevation of blood glucose to 12 mmol/l inhibits internal and external anal sphincter function and increases rectal sensitivity in normal subjects. In contrast, physiological changes in blood glucose do not have a significant effect on anorectal motor and sensory function.
Keywords: hyperglycaemia; anorectum; motility; sensation; diabetes mellitus
Full Text
The Full Text of this article is available as a PDF (115.5 KB).
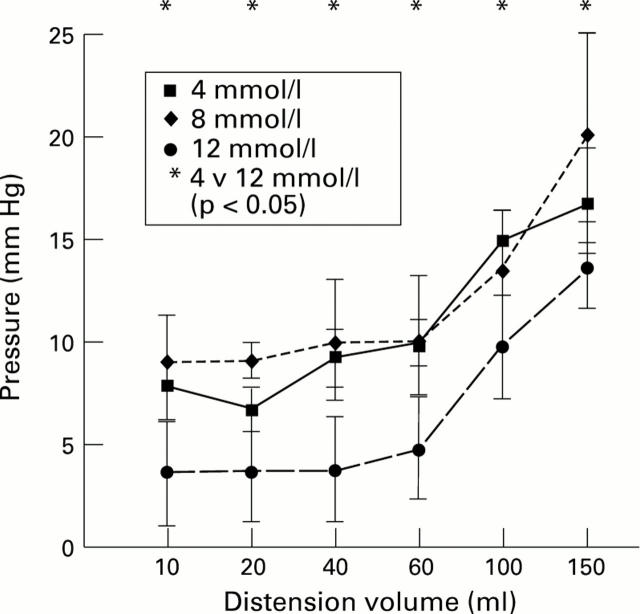
Figure 1 .
: Blood glucose concentrations (mean (SEM)) during the three experiments (4, 8, and 12 mmol/l).
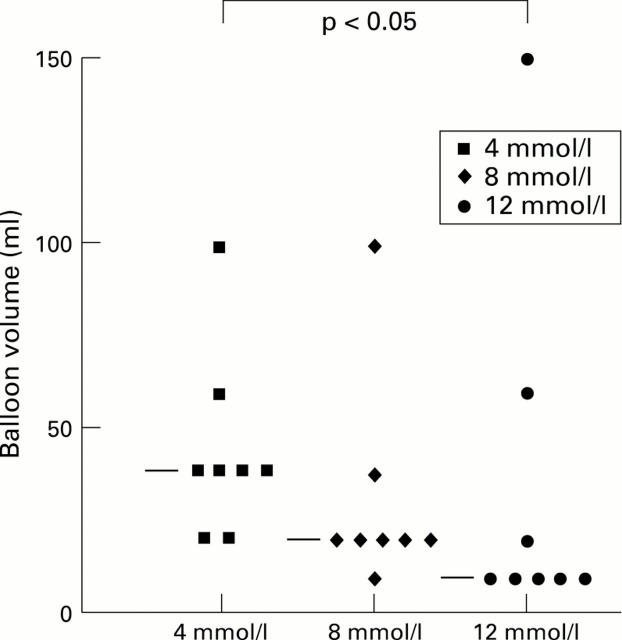
Figure 2 .
: Relation between intraballoon pressure (mean (SEM)) and volume during rectal balloon distension at blood glucose concentrations of 4, 8, and 12 mmol/l.
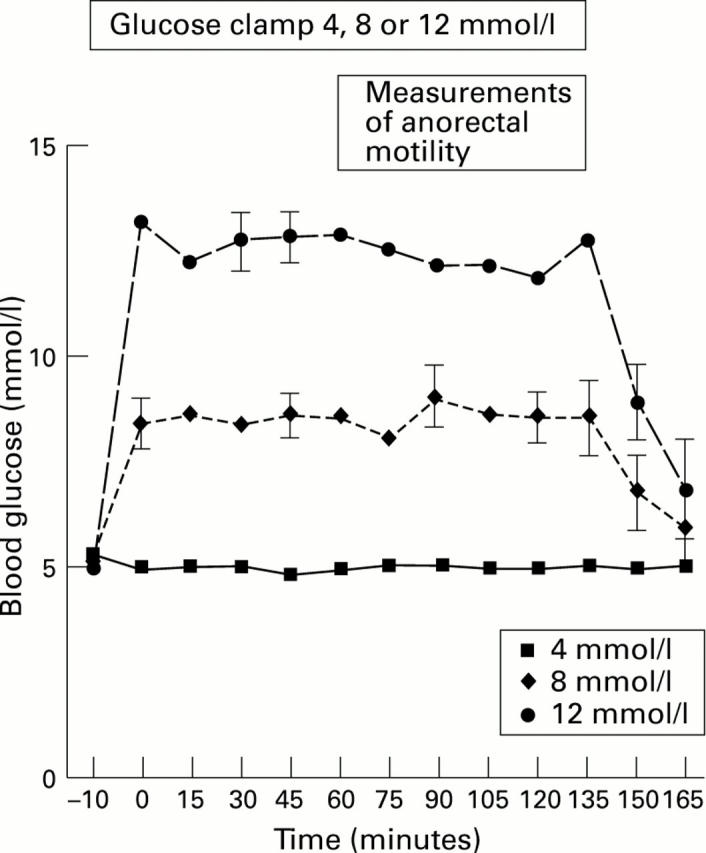
Figure 3 .
: Volume for first perception of sensation during rectal balloon distension at blood glucose concentrations of 4, 8, and 12 mmol/l. The median value is shown by the horizontal line.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Axon A. T. The transmission of Helicobacter pylori: which theory fits the facts? Eur J Gastroenterol Hepatol. 1996 Jan;8(1):1–2. doi: 10.1097/00042737-199601000-00001. [DOI] [PubMed] [Google Scholar]
- Barnett J. L., Owyang C. Serum glucose concentration as a modulator of interdigestive gastric motility. Gastroenterology. 1988 Mar;94(3):739–744. doi: 10.1016/0016-5085(88)90248-x. [DOI] [PubMed] [Google Scholar]
- Björnsson E. S., Urbanavicius V., Eliasson B., Attvall S., Smith U., Abrahamsson H. Effects of hyperglycemia on interdigestive gastrointestinal motility in humans. Scand J Gastroenterol. 1994 Dec;29(12):1096–1104. doi: 10.3109/00365529409094894. [DOI] [PubMed] [Google Scholar]
- Caruana B. J., Wald A., Hinds J. P., Eidelman B. H. Anorectal sensory and motor function in neurogenic fecal incontinence. Comparison between multiple sclerosis and diabetes mellitus. Gastroenterology. 1991 Feb;100(2):465–470. doi: 10.1016/0016-5085(91)90217-9. [DOI] [PubMed] [Google Scholar]
- Chey W. D., Kim M., Hasler W. L., Owyang C. Hyperglycemia alters perception of rectal distention and blunts the rectoanal inhibitory reflex in healthy volunteers. Gastroenterology. 1995 Jun;108(6):1700–1708. doi: 10.1016/0016-5085(95)90131-0. [DOI] [PubMed] [Google Scholar]
- De Boer S. Y., Masclee A. A., Lam W. F., Lamers C. B. Effect of acute hyperglycemia on esophageal motility and lower esophageal sphincter pressure in humans. Gastroenterology. 1992 Sep;103(3):775–780. doi: 10.1016/0016-5085(92)90005-j. [DOI] [PubMed] [Google Scholar]
- DeFronzo R. A., Tobin J. D., Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979 Sep;237(3):E214–E223. doi: 10.1152/ajpendo.1979.237.3.E214. [DOI] [PubMed] [Google Scholar]
- Feldman M., Schiller L. R. Disorders of gastrointestinal motility associated with diabetes mellitus. Ann Intern Med. 1983 Mar;98(3):378–384. doi: 10.7326/0003-4819-98-3-378. [DOI] [PubMed] [Google Scholar]
- Fraser R. J., Horowitz M., Maddox A. F., Harding P. E., Chatterton B. E., Dent J. Hyperglycaemia slows gastric emptying in type 1 (insulin-dependent) diabetes mellitus. Diabetologia. 1990 Nov;33(11):675–680. doi: 10.1007/BF00400569. [DOI] [PubMed] [Google Scholar]
- Fraser R., Horowitz M., Dent J. Hyperglycaemia stimulates pyloric motility in normal subjects. Gut. 1991 May;32(5):475–478. doi: 10.1136/gut.32.5.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene D. A. A sodium-pump defect in diabetic peripheral nerve corrected by sorbinil administration: relationship to myo-inositol metabolism and nerve conduction slowing. Metabolism. 1986 Apr;35(4 Suppl 1):60–65. doi: 10.1016/0026-0495(86)90189-7. [DOI] [PubMed] [Google Scholar]
- Groop L. C., Luzi L., DeFronzo R. A., Melander A. Hyperglycaemia and absorption of sulphonylurea drugs. Lancet. 1989 Jul 15;2(8655):129–130. doi: 10.1016/s0140-6736(89)90184-0. [DOI] [PubMed] [Google Scholar]
- Hasler W. L., Soudah H. C., Dulai G., Owyang C. Mediation of hyperglycemia-evoked gastric slow-wave dysrhythmias by endogenous prostaglandins. Gastroenterology. 1995 Mar;108(3):727–736. doi: 10.1016/0016-5085(95)90445-x. [DOI] [PubMed] [Google Scholar]
- Hebbard G. S., Samson M., Andrews J. M., Carman D., Tansell B., Sun W. M., Dent J., Horowitz M. Hyperglycemia affects gastric electrical rhythm and nausea during intraduodenal triglyceride infusion. Dig Dis Sci. 1997 Mar;42(3):568–575. doi: 10.1023/a:1018851227051. [DOI] [PubMed] [Google Scholar]
- Orkin B. A., Hanson R. B., Kelly K. A., Phillips S. F., Dent J. Human anal motility while fasting, after feeding, and during sleep. Gastroenterology. 1991 Apr;100(4):1016–1023. doi: 10.1016/0016-5085(91)90277-r. [DOI] [PubMed] [Google Scholar]
- Rogers J., Levy D. M., Henry M. M., Misiewicz J. J. Pelvic floor neuropathy: a comparative study of diabetes mellitus and idiopathic faecal incontinence. Gut. 1988 Jun;29(6):756–761. doi: 10.1136/gut.29.6.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo A., Fraser R., Horowitz M. The effect of acute hyperglycaemia on small intestinal motility in normal subjects. Diabetologia. 1996 Aug;39(8):984–989. doi: 10.1007/BF00403919. [DOI] [PubMed] [Google Scholar]
- Schiller L. R., Santa Ana C. A., Schmulen A. C., Hendler R. S., Harford W. V., Fordtran J. S. Pathogenesis of fecal incontinence in diabetes mellitus: evidence for internal-anal-sphincter dysfunction. N Engl J Med. 1982 Dec 30;307(27):1666–1671. doi: 10.1056/NEJM198212303072702. [DOI] [PubMed] [Google Scholar]
- Schvarcz E., Palmér M., Aman J., Horowitz M., Stridsberg M., Berne C. Physiological hyperglycemia slows gastric emptying in normal subjects and patients with insulin-dependent diabetes mellitus. Gastroenterology. 1997 Jul;113(1):60–66. doi: 10.1016/s0016-5085(97)70080-5. [DOI] [PubMed] [Google Scholar]
- Schvarcz E., Palmér M., Aman J., Lindkvist B., Beckman K. W. Hypoglycaemia increases the gastric emptying rate in patients with type 1 diabetes mellitus. Diabet Med. 1993 Aug-Sep;10(7):660–663. doi: 10.1111/j.1464-5491.1993.tb00141.x. [DOI] [PubMed] [Google Scholar]
- Sims M. A., Hasler W. L., Chey W. D., Kim M. S., Owyang C. Hyperglycemia inhibits mechanoreceptor-mediated gastrocolonic responses and colonic peristaltic reflexes in healthy humans. Gastroenterology. 1995 Feb;108(2):350–359. doi: 10.1016/0016-5085(95)90060-8. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Katsinelos P., Horowitz M., Read N. W. Disturbances in anorectal function in patients with diabetes mellitus and faecal incontinence. Eur J Gastroenterol Hepatol. 1996 Oct;8(10):1007–1012. doi: 10.1097/00042737-199610000-00014. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Donnelly T. C. Impaired internal anal sphincter in a subgroup of patients with idiopathic fecal incontinence. Gastroenterology. 1989 Jul;97(1):130–135. doi: 10.1016/0016-5085(89)91425-x. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Miner P. B., Kerrigan D. D., Donnelly T. C. The role of transient internal sphincter relaxation in faecal incontinence? Int J Colorectal Dis. 1990 Feb;5(1):31–36. doi: 10.1007/BF00496147. [DOI] [PubMed] [Google Scholar]
- Sun W. M., Read N. W., Prior A., Daly J. A., Cheah S. K., Grundy D. Sensory and motor responses to rectal distention vary according to rate and pattern of balloon inflation. Gastroenterology. 1990 Oct;99(4):1008–1015. doi: 10.1016/0016-5085(90)90620-g. [DOI] [PubMed] [Google Scholar]
- Wald A. Colonic and anorectal motility testing in clinical practice. Am J Gastroenterol. 1994 Dec;89(12):2109–2115. [PubMed] [Google Scholar]
- Yeap B. B., Russo A., Fraser R. J., Wittert G. A., Horowitz M. Hyperglycemia affects cardiovascular autonomic nerve function in normal subjects. Diabetes Care. 1996 Aug;19(8):880–882. doi: 10.2337/diacare.19.8.880. [DOI] [PubMed] [Google Scholar]
- Yeoh E., Sun W. M., Russo A., Ibanez L., Horowitz M. A retrospective study of the effects of pelvic irradiation for gynecological cancer on anorectal function. Int J Radiat Oncol Biol Phys. 1996 Jul 15;35(5):1003–1010. doi: 10.1016/0360-3016(96)00147-2. [DOI] [PubMed] [Google Scholar]
- de Boer S. Y., Masclee A. A., lam W. F., Schipper J., Jansen J. B., Lamers C. B. Hyperglycemia modulates gallbladder motility and small intestinal transit time in man. Dig Dis Sci. 1993 Dec;38(12):2228–2235. doi: 10.1007/BF01299901. [DOI] [PubMed] [Google Scholar]