Abstract
Background—Octreotide is used in many centres to prevent complications after pancreatic surgery. Delayed gastric emptying is a another complication occurring in around 30% of patients after pancreatoduodenectomy (PD) and causes prolonged hospital stay. The influence of octreotide on this complication is doubtful. Aims—To assess the effect of octreotide, at the clinical dosage used after pancreatic surgery, on gastric emptying in healthy volunteers. Subjects and methods—Eight healthy male volunteers (mean age 22.5 years) participated in this double blind, placebo controlled study. On day 1 subjects received 100 µg of octreotide or placebo subcutaneously, three times daily and on day 2, one hour after the fourth injection, gastric emptying, postprandial cholecystokinin (CCK) release, and mouth to caecum transit time (MCTT) were measured. This protocol was repeated after one week, in a crossover design. On the test day subjects received a liquid test meal (1.57 MJ/300 ml) and gastric emptying measurements were performed with applied potential tomography, a non-invasive, validated technique which measures gastric emptying through impedance differences. From the gastric emptying curves, lag time, t50, and postlag emptying rate were measured. MCTT was measured using the hydrogen breath test. Results—Lag time decreased from 29.6 (6.3) (mean (SEM)) to 12.2 (4.6) minutes (p<0.05) during octreotide treatment; t50 decreased from 87.8 (12.0) to 47.5 (8.2) minutes (p<0.02) and there was a trend towards an increased postlag emptying rate (0.8 to 1.6% per minute; p=0.07). MCTT increased from 150 (12.7) to 229 (17.9) minutes during octreotide treatment (p<0.01). Octreotide suppressed postprandial CCK release (p<0.05). Conclusions—MCTT was delayed by octreotide, suggesting impairment of small bowel transit. Octreotide administered at the clinical dosage for pancreatic surgery accelerates gastric emptying, mainly by shortening the lag time. Suppression of postprandial CCK release may be involved in this process. Octreotide administration is therefore not a contributing factor in the pathogenesis of delayed postoperative gastric emptying after PD and might even play a role in preventing this complication.
Keywords: octreotide; gastric emptying; cholecystokinin; intestinal transit; pancreatic surgery
Full Text
The Full Text of this article is available as a PDF (111.8 KB).
Figure 1 .
: Study protocol, with octreotide and placebo injections indicated by the small black arrows. On the test day gastric emptying, CCK, and MCTT measurements were performed.
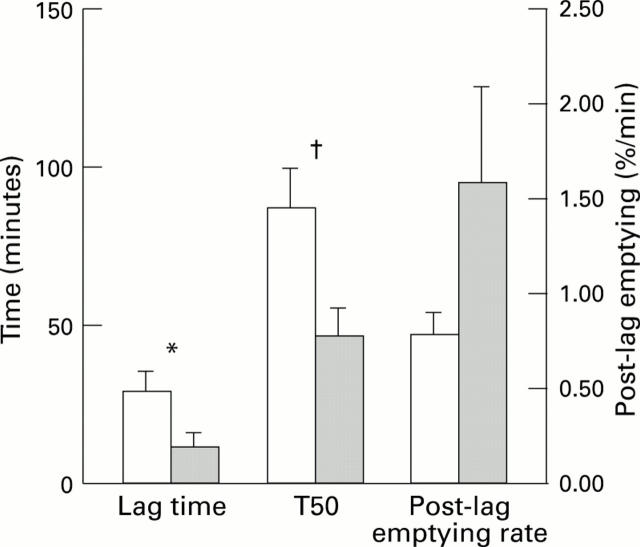
Figure 2 .
: Lag time, t50, and postlag emptying rate for placebo and octreotide treatment. *p<0.05, †p<0.02. Postlag emptying rate was not significantly different between placebo and octreotide treatment (p=0.07). White columns, placebo; shaded columns, octreotide.
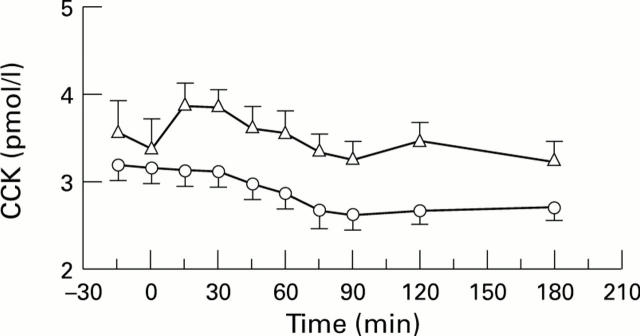
Figure 3 .
: Postprandial CCK response for placebo and octreotide administration (p<0.05). There was a significant postprandial CCK increase compared with basal levels in placebo treated subjects (p<0.05). There was no significant postprandial CCK increase in octreotide treated subjects. Open triangles, placebo; open circles, octreotide
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avill R., Mangnall Y. F., Bird N. C., Brown B. H., Barber D. C., Seagar A. D., Johnson A. G., Read N. W. Applied potential tomography. A new noninvasive technique for measuring gastric emptying. Gastroenterology. 1987 Apr;92(4):1019–1026. [PubMed] [Google Scholar]
- Baxter A. J., Mangnall Y. F., Loj E. H., Brown B., Barber D. C., Johnson A. G., Read N. W. Evaluation of applied potential tomography as a new non-invasive gastric secretion test. Gut. 1988 Dec;29(12):1730–1735. doi: 10.1136/gut.29.12.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braasch J. W., Gray B. N. Considerations that lower pancreatoduodenectomy mortality. Am J Surg. 1977 Apr;133(4):480–484. doi: 10.1016/0002-9610(77)90135-0. [DOI] [PubMed] [Google Scholar]
- Büchler M., Friess H., Klempa I., Hermanek P., Sulkowski U., Becker H., Schafmayer A., Baca I., Lorenz D., Meister R. Role of octreotide in the prevention of postoperative complications following pancreatic resection. Am J Surg. 1992 Jan;163(1):125–131. doi: 10.1016/0002-9610(92)90264-r. [DOI] [PubMed] [Google Scholar]
- Cameron J. L., Pitt H. A., Yeo C. J., Lillemoe K. D., Kaufman H. S., Coleman J. One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg. 1993 May;217(5):430–438. doi: 10.1097/00000658-199305010-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creutzfeldt W., Lembcke B., Fölsch U. R., Schleser S., Koop I. Effect of somatostatin analogue (SMS 201-995, Sandostatin) on pancreatic secretion in humans. Am J Med. 1987 May 29;82(5B):49–54. doi: 10.1016/0002-9343(87)90426-8. [DOI] [PubMed] [Google Scholar]
- Cullen J. J., Eagon J. C., Dozois E. J., Kelly K. A. Treatment of acute postoperative ileus with octreotide. Am J Surg. 1993 Jan;165(1):113–120. doi: 10.1016/s0002-9610(05)80413-1. [DOI] [PubMed] [Google Scholar]
- Debas H. T., Farooq O., Grossman M. I. Inhibition of gastric emptying is a physiological action of cholecystokinin. Gastroenterology. 1975 May;68(5 Pt 1):1211–1217. [PubMed] [Google Scholar]
- Forrest J. A., Fettes M. R., McLoughlin G. P., Heading R. C. Effect of long-term cimetidine on gastric acid secretion, serum gastrin, and gastric emptying. Gut. 1979 May;20(5):404–407. doi: 10.1136/gut.20.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraser R., Fone D., Horowitz M., Dent J. Cholecystokinin octapeptide stimulates phasic and tonic pyloric motility in healthy humans. Gut. 1993 Jan;34(1):33–37. doi: 10.1136/gut.34.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friess H., Beger H. G., Sulkowski U., Becker H., Hofbauer B., Dennler H. J., Büchler M. W. Randomized controlled multicentre study of the prevention of complications by octreotide in patients undergoing surgery for chronic pancreatitis. Br J Surg. 1995 Sep;82(9):1270–1273. doi: 10.1002/bjs.1800820938. [DOI] [PubMed] [Google Scholar]
- Friess H., Bordihn K., Ebert M., Malfertheiner P., Kemmer T., Dennler H. J., Büchler M. W. Inhibition of pancreatic secretion under long-term octreotide treatment in humans. Digestion. 1994;55 (Suppl 1):10–15. doi: 10.1159/000201182. [DOI] [PubMed] [Google Scholar]
- Fuessl H. S., Carolan G., Williams G., Bloom S. R. Effect of a long-acting somatostatin analogue (SMS 201-995) on postprandial gastric emptying of 99mTc-tin colloid and mouth-to-caecum transit time in man. Digestion. 1987;36(2):101–107. doi: 10.1159/000199407. [DOI] [PubMed] [Google Scholar]
- Gill R. C., Murphy P. D., Hooper H. R., Bowes K. L., Kingma Y. J. Effect of the menstrual cycle on gastric emptying. Digestion. 1987;36(3):168–174. doi: 10.1159/000199414. [DOI] [PubMed] [Google Scholar]
- Gyr K. E., Meier R. Pharmacodynamic effects of Sandostatin in the gastrointestinal tract. Digestion. 1993;54 (Suppl 1):14–19. doi: 10.1159/000201070. [DOI] [PubMed] [Google Scholar]
- Harris A. G. Somatostatin and somatostatin analogues: pharmacokinetics and pharmacodynamic effects. Gut. 1994;35(3 Suppl):S1–S4. doi: 10.1136/gut.35.3_suppl.s1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haruma K., Wiste J. A., Camilleri M. Effect of octreotide on gastrointestinal pressure profiles in health and in functional and organic gastrointestinal disorders. Gut. 1994 Aug;35(8):1064–1069. doi: 10.1136/gut.35.8.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heddle R., Collins P. J., Dent J., Horowitz M., Read N. W., Chatterton B., Houghton L. A. Motor mechanisms associated with slowing of the gastric emptying of a solid meal by an intraduodenal lipid infusion. J Gastroenterol Hepatol. 1989 Sep-Oct;4(5):437–447. doi: 10.1111/j.1440-1746.1989.tb01741.x. [DOI] [PubMed] [Google Scholar]
- Heddle R., Dent J., Read N. W., Houghton L. A., Toouli J., Horowitz M., Maddern G. J., Downton J. Antropyloroduodenal motor responses to intraduodenal lipid infusion in healthy volunteers. Am J Physiol. 1988 May;254(5 Pt 1):G671–G679. doi: 10.1152/ajpgi.1988.254.5.G671. [DOI] [PubMed] [Google Scholar]
- Hocking M. P., Harrison W. D., Sninsky C. A. Gastric dysrhythmias following pylorus-preserving pancreaticoduodenectomy. Possible mechanism for early delayed gastric emptying. Dig Dis Sci. 1990 Oct;35(10):1226–1230. doi: 10.1007/BF01536411. [DOI] [PubMed] [Google Scholar]
- Horowitz M., Maddern G. J., Chatterton B. E., Collins P. J., Petrucco O. M., Seamark R., Shearman D. J. The normal menstrual cycle has no effect on gastric emptying. Br J Obstet Gynaecol. 1985 Jul;92(7):743–746. doi: 10.1111/j.1471-0528.1985.tb01458.x. [DOI] [PubMed] [Google Scholar]
- Hunt D. R., McLean R. Pylorus-preserving pancreatectomy: functional results. Br J Surg. 1989 Feb;76(2):173–176. doi: 10.1002/bjs.1800760223. [DOI] [PubMed] [Google Scholar]
- Jansen J. B., Lamers C. B. Radioimmunoassay of cholecystokinin in human tissue and plasma. Clin Chim Acta. 1983 Jul 15;131(3):305–316. doi: 10.1016/0009-8981(83)90100-6. [DOI] [PubMed] [Google Scholar]
- Kleibeuker J. H., Beekhuis H., Jansen J. B., Piers D. A., Lamers C. B. Cholecystokinin is a physiological hormonal mediator of fat-induced inhibition of gastric emptying in man. Eur J Clin Invest. 1988 Apr;18(2):173–177. doi: 10.1111/j.1365-2362.1988.tb02409.x. [DOI] [PubMed] [Google Scholar]
- Klinkenbijl J. H., van der Schelling G. P., Hop W. C., van Pel R., Bruining H. A., Jeekel J. The advantages of pylorus-preserving pancreatoduodenectomy in malignant disease of the pancreas and periampullary region. Ann Surg. 1992 Aug;216(2):142–145. doi: 10.1097/00000658-199208000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konturek J. W., Thor P., Maczka M., Stoll R., Domschke W., Konturek S. J. Role of cholecystokinin in the control of gastric emptying and secretory response to a fatty meal in normal subjects and duodenal ulcer patients. Scand J Gastroenterol. 1994 Jul;29(7):583–590. doi: 10.3109/00365529409092476. [DOI] [PubMed] [Google Scholar]
- Kutz K., Nüesch E., Rosenthaler J. Pharmacokinetics of SMS 201-995 in healthy subjects. Scand J Gastroenterol Suppl. 1986;119:65–72. doi: 10.3109/00365528609087433. [DOI] [PubMed] [Google Scholar]
- Lembcke B., Creutzfeldt W., Schleser S., Ebert R., Shaw C., Koop I. Effect of the somatostatin analogue sandostatin (SMS 201-995) on gastrointestinal, pancreatic and biliary function and hormone release in normal men. Digestion. 1987;36(2):108–124. doi: 10.1159/000199408. [DOI] [PubMed] [Google Scholar]
- Liberski S. M., Koch K. L., Atnip R. G., Stern R. M. Ischemic gastroparesis: resolution after revascularization. Gastroenterology. 1990 Jul;99(1):252–257. doi: 10.1016/0016-5085(90)91255-5. [DOI] [PubMed] [Google Scholar]
- Mangnall Y. F., Kerrigan D. D., Johnson A. G., Read N. W. Applied potential tomography. Noninvasive method for measuring gastric emptying of a solid test meal. Dig Dis Sci. 1991 Dec;36(12):1680–1684. doi: 10.1007/BF01296609. [DOI] [PubMed] [Google Scholar]
- Miedema B. W., Sarr M. G., van Heerden J. A., Nagorney D. M., McIlrath D. C., Ilstrup D. Complications following pancreaticoduodenectomy. Current management. Arch Surg. 1992 Aug;127(8):945–950. doi: 10.1001/archsurg.1992.01420080079012. [DOI] [PubMed] [Google Scholar]
- Montorsi M., Zago M., Mosca F., Capussotti L., Zotti E., Ribotta G., Fegiz G., Fissi S., Roviaro G., Peracchia A. Efficacy of octreotide in the prevention of pancreatic fistula after elective pancreatic resections: a prospective, controlled, randomized clinical trial. Surgery. 1995 Jan;117(1):26–31. doi: 10.1016/s0039-6060(05)80225-9. [DOI] [PubMed] [Google Scholar]
- Mushambi M. C., Trotter T. N., Barker P., Rowbotham D. J. A comparison of gastric emptying rate after cimetidine and ranitidine measured by applied potential tomography. Br J Clin Pharmacol. 1992 Sep;34(3):278–280. doi: 10.1111/j.1365-2125.1992.tb04139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson-Piercy C., Hammond P. J., Gwilliam M. E., Khandan-Nia N., Myers M. J., Ghatei M. A., Bloom S. R. Effect of a new oral somatostatin analog (SDZ CO 611) on gastric emptying, mouth to cecum transit time, and pancreatic and gut hormone release in normal male subjects. J Clin Endocrinol Metab. 1994 Feb;78(2):329–336. doi: 10.1210/jcem.78.2.7906279. [DOI] [PubMed] [Google Scholar]
- Notivol R., Carrio I., Cano L., Estorch M., Vilardell F. Gastric emptying of solid and liquid meals in healthy young subjects. Scand J Gastroenterol. 1984 Nov;19(8):1107–1113. [PubMed] [Google Scholar]
- Pederzoli P., Bassi C., Falconi M., Camboni M. G. Efficacy of octreotide in the prevention of complications of elective pancreatic surgery. Italian Study Group. Br J Surg. 1994 Feb;81(2):265–269. doi: 10.1002/bjs.1800810237. [DOI] [PubMed] [Google Scholar]
- Petring O. U., Flachs H. Inter- and intrasubject variability of gastric emptying in healthy volunteers measured by scintigraphy and paracetamol absorption. Br J Clin Pharmacol. 1990 Jun;29(6):703–708. doi: 10.1111/j.1365-2125.1990.tb03691.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichlin S. Somatostatin (second of two parts). N Engl J Med. 1983 Dec 22;309(25):1556–1563. doi: 10.1056/NEJM198312223092506. [DOI] [PubMed] [Google Scholar]
- Stolk M. F., van Erpecum K. J., Koppeschaar H. P., de Bruin W. I., Jansen J. B., Lamers C. B., van Berge Henegouwen G. P. Postprandial gall bladder motility and hormone release during intermittent and continuous subcutaneous octreotide treatment in acromegaly. Gut. 1993 Jun;34(6):808–813. doi: 10.1136/gut.34.6.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka M., Sarr M. G. Effects of exogenous motilin and morphine on interdigestive gastrointestinal motor activity after total duodenectomy in dogs. Surgery. 1988 Aug;104(2):317–325. [PubMed] [Google Scholar]
- Tanaka M., Sarr M. G. Role of the duodenum in the control of canine gastrointestinal motility. Gastroenterology. 1988 Mar;94(3):622–629. doi: 10.1016/0016-5085(88)90232-6. [DOI] [PubMed] [Google Scholar]
- Tanaka M., Sarr M. G. Total duodenectomy: effect on canine gastrointestinal motility. J Surg Res. 1987 May;42(5):483–493. doi: 10.1016/0022-4804(87)90022-9. [DOI] [PubMed] [Google Scholar]
- Tjeerdsma H. C., Smout A. J., Akkermans L. M. Voluntary suppression of defecation delays gastric emptying. Dig Dis Sci. 1993 May;38(5):832–836. doi: 10.1007/BF01295908. [DOI] [PubMed] [Google Scholar]
- Trede M., Schwall G. The complications of pancreatectomy. Ann Surg. 1988 Jan;207(1):39–47. doi: 10.1097/00000658-198801000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wald A., Van Thiel D. H., Hoechstetter L., Gavaler J. S., Egler K. M., Verm R., Scott L., Lester R. Gastrointestinal transit: the effect of the menstrual cycle. Gastroenterology. 1981 Jun;80(6):1497–1500. [PubMed] [Google Scholar]
- Yeo C. J., Cameron J. L., Maher M. M., Sauter P. K., Zahurak M. L., Talamini M. A., Lillemoe K. D., Pitt H. A. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995 Oct;222(4):580–592. doi: 10.1097/00000658-199510000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerbi A., Balzano G., Patuzzo R., Calori G., Braga M., Di Carlo V. Comparison between pylorus-preserving and Whipple pancreatoduodenectomy. Br J Surg. 1995 Jul;82(7):975–979. doi: 10.1002/bjs.1800820738. [DOI] [PubMed] [Google Scholar]
- von der Ohe M. R., Camilleri M., Thomforde G. M., Klee G. G. Differential regional effects of octreotide on human gastrointestinal motor function. Gut. 1995 May;36(5):743–748. doi: 10.1136/gut.36.5.743. [DOI] [PMC free article] [PubMed] [Google Scholar]